HPR volume 15 issue 18: news (22 November 2021)
Updated 19 January 2022
ESPAUR annual report in summary
The annual English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) report, published by the UK Health Security Agency (UKHSA) on 17 November, provides data on antibiotic use and resistance in the financial year 2020 to 2021.
The main findings of the eighth report are summarised below.
Antibiotic resistance
In line with reductions in social mixing, enhanced hand hygiene and fewer people in hospital, the number of key-pathogens bloodstream infections fell in England between 2019 and 2020 (from 88,195 to 77,310).
Importantly however, the proportion of bloodstream infections (BSI) that were resistant to one or more antibiotics increased (from 14,829 to 15,549), suggesting we are likely to see a rise in antibiotic-resistant infections as pandemic-related restrictions are discontinued.

For full text explanation of the above infographic, see Infographic 3 at ‘The burden of bloodstream infections (BSI) and resistant BSI’.
A requirement for the notification of the results of antimicrobial susceptibility tests – and, specifically, any identified carbapenemase-producing Gram-negative bacteria (CPGNB) – was added to the Health Protection (Notification) Regulations on the 1 October 2020. There were 586 notifications of CPGNB between October and December 2020, 6% of which were from sterile sites.
Antibiotic usage
With the changes in healthcare delivery and in healthcare-seeking behaviour, one of the most pronounced changes was the reduction in antibiotic prescribing, especially in primary care, where the reduction observed between 2019 and 2020 – from 18.0 defined daily doses (DDDs) per 1,000 inhabitants per day to 16.0 DDDs per 1,000 inhabitants per day – was greater than the reductions seen between 2016 and 2019 (from 19.3 DDDs to 18.0).
When secondary care consumption rates were assessed as DDDs per 1,000 hospital admissions, a greater increase compared to previous years was seen between 2019 and 2020, driven by an increase in inpatient prescribing (6%). Changes in prescribing during the coronavirus (COVID-19) pandemic had been expected. These increases in hospital inpatient consumption are thought to be largely related to changes in hospital populations (with cancellations of elective procedures) and reductions in hospital admissions during the COVID-19 pandemic. Antimicrobial stewardship (AMS) teams will need to work tirelessly with prescribers in the coming 12 months to reverse this trend.
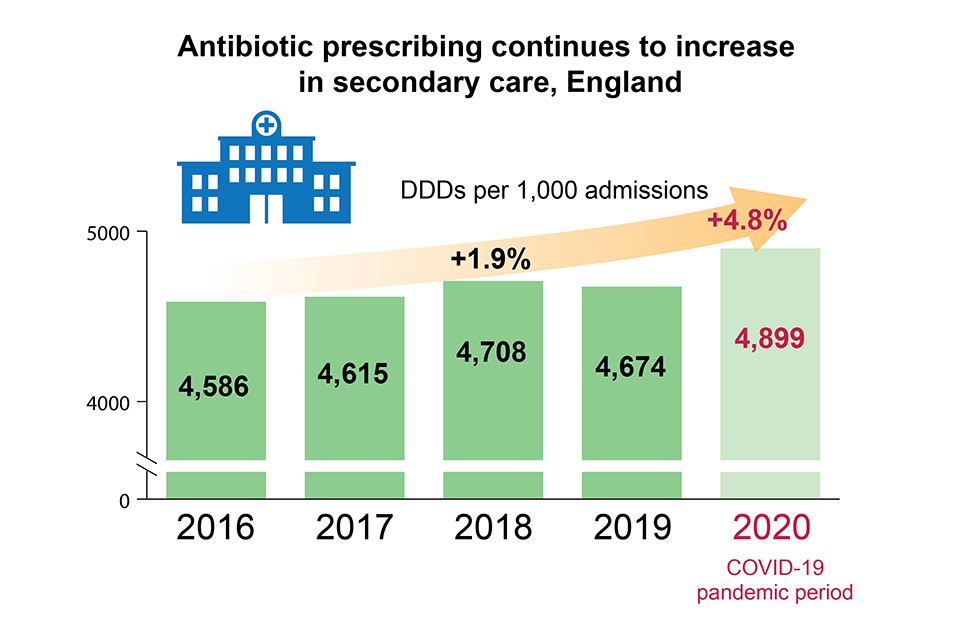
Each of the 5 data bars in the above infographic represents 5 years of secondary care antibiotic prescribing from 2016 to 2020. The bars show an increased prescribing between 2016 to 2018, reflecting the increase in consumption from 4,586 DDDs per 1,000 admissions in 2016 to 4,615 in 2017 and 4,708 in 2018. This represents a 3% increase across the 3 years. This is further indicated by a diagonal arrow which points upwards from left to right across the top of the bars. There is a slight decrease in trend in 2019 to 4,674 DDDs per 1,000 admissions, followed by an increase in 2020 (the COVID-19 pandemic period) to 4,899 DDDs per 1,000 admissions.
Antibiotic prescribing continued to be greatest within the general practice setting (72.7%).
Between 2019 and 2020, community prescribing of antifungals decreased by 24% and hospital prescribing increased by 21%.
Antibiotic stewardship
The COVID-19 pandemic had a significant impact on the AMS activities undertaken across the UK. Of the AMS leads that responded to a UK-wide survey, most reported a reduction in AMS activity with 64% (61 out of 95) reporting that COVID-19 had a negative impact on routine AMS activities. However, despite this, for primary care, the Treat Antibiotics Responsibly, Guidance, Education and Tools (TARGET) hosted on the Royal College of General Practitioners website remained the most accessed section of that website.
The Keep Antibiotics Working (KAW) social marketing campaign 2017 to 2019 supported a range of actions across the healthcare system. The percentage of GPs reporting that “the advertising makes me more confident to say no to patients asking for antibiotics” was high at launch in 2017 and has been maintained. Campaign recognition among the general public also improved over the 3 years, rising from 56% (n=1,201) of participants recognising the campaign in 2017 to 71% (n=1,350) in 2019.
For World Antimicrobial Awareness Week (WAAW) 2020, UKHSA developed an Antibiotic awareness toolkit for healthcare professionals in England: a collection of digital resources for healthcare workers, designed to standardise and de-duplicate efforts in disseminating AMR messages and mitigate challenges in running local campaigns due to the COVID-19 pandemic.
GRASP annual report in summary
UKHSA has published the annual Gonococcal Resistance to Antimicrobials Surveillance Programme (GRASP) report, presenting the latest data on antimicrobial resistance in Neisseria gonorrhoeae in England and Wales.
Between 2019 and 2020, Neisseria gonorrhoeae isolates collected through GRASP showed:
- a decrease in reduced susceptibility (minimum inhibitory concentration (MIC) >0.03 mg/L) to ceftriaxone, the current first-line therapy, from 2.9% in 2019 to 1.4% in 2020
- the modal ceftriaxone resistance MIC remained stable at 0.008 mg/L in 2020
- the modal MIC for isolates from gay, bisexual, and other men who have sex with men (MSM) remained higher (0.015 mg/L) than those from both women and heterosexual men (0.008 mg/L)
- no cases of ceftriaxone resistance (MIC >0.125 mg/L) were confirmed by the UKHSA Antimicrobial Resistance in STIs (AMRSTI) national reference laboratory on direct referral in 2020 – however only 18.2% of isolates with suspected ceftriaxone resistance were referred to UKHSA
Between 2019 and 2020, testing of gonococcal isolates collected through the GRASP sentinel surveillance system also showed:
- azithromycin resistance remained stable with a marginal reduction from 9.3% to 8.7%
- cefixime resistance remained stable with a marginal reduction from 0.8% to 0.6%
- ciprofloxacin resistance increased from 42.7% to 44.3%
- penicillin resistance decreased from 17.9% to 9.6%
- tetracycline resistance increased from 62.9% to 65.1%
The stabilisation of azithromycin (MIC >0.5 mg/L), cefixime (MIC >0.125 mg/L), ciprofloxacin (MIC >0.06 mg/L) and tetracycline (MIC >1 mg/L) resistance and, most notably, the substantial decline in the proportion of isolates resistant to penicillin (MIC >1 mg/L) in 2020 represents a change in the trend in antimicrobial resistance observed from 2016 to 2019. As in previous years, no spectinomycin resistance (MIC >64 mg/L) was detected in 2020 and the modal gentamicin MIC remained low (4 mg/L).
Prescribing data demonstrated excellent adherence to the British Association for Sexual Health and HIV (BASHH) national (UK) guideline for managing infection with N. gonorrhoeae, with 97.6% of individuals receiving the recommended first-line of ceftriaxone 1 g intramuscular (IM) monotherapy in 2020.
The effectiveness of first-line treatment for gonorrhoea continues to be threatened by the development of antimicrobial resistance. However, the ongoing decline in reduced ceftriaxone susceptibility, together with the decreasing penicillin resistance and stable rates of azithromycin, cefixime, ciprofloxacin and tetracycline resistance, are encouraging developments
Sexual health services should report cases of suspected treatment failure to UKHSA via the online HIV and STI web portal.
Infection report
Laboratory surveillance of Acinetobacter spp. bacteraemia in England: 2020.
