HPR volume 15 issue 17: news (1 November)
Updated 19 January 2022
Tuberculosis in England: 2021 report
The United Kingdom Health Security Agency (UKHSA) has published ‘Tuberculosis in England: 2021 annual report’ containing data to the end of 2020. The report also presents data on the UK pre-entry screening programme as well as latent TB infection (LTBI) testing and treatment.
The TB report will support timely actions to achieve the aims set out by the Tuberculosis (TB) Action Plan for England, 2021 to 2026.
Epidemiology
There were 4,125 people diagnosed with TB in England in 2020, a 12.7% decline from the previous year. The rate of TB reached an all-time low of 7.3 per 100,000 population and has now been below the 10 per 100,000 World Health Organization (WHO) definition of a low incidence country (set out in its End TB Strategy) since 2017 (see figure).
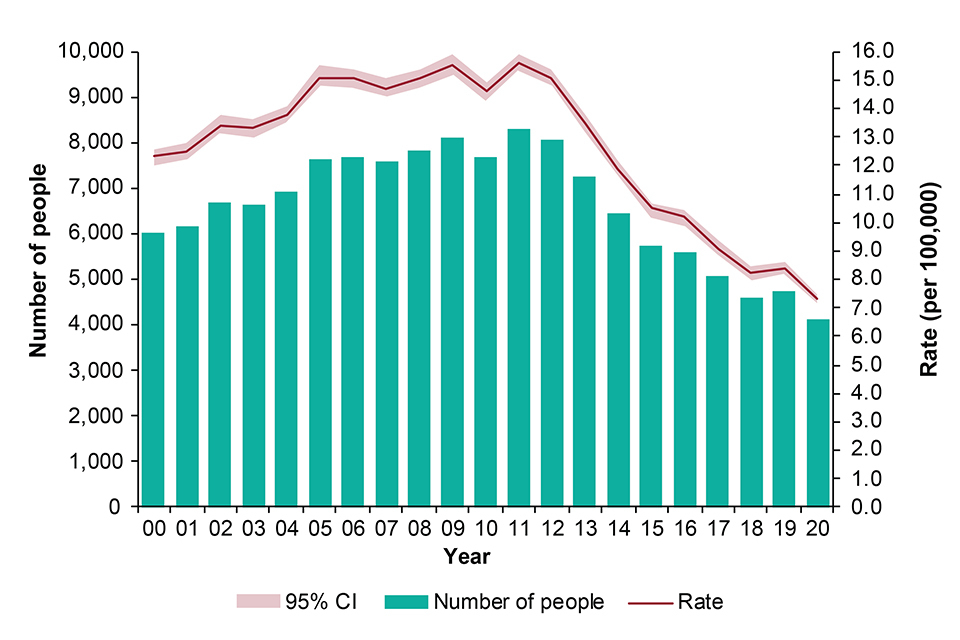
Number of TB notifications and rates, England, 2000 to 2020
People born outside the UK continued to account for most of the TB notifications in 2020 (72.8%) and, with a TB incidence rate of 36.3 per 100,000, remained 15 times greater than the rate among people born in the UK (2.3 per 100,000). Between 2019 and 2020 there has been a decline in the number and rates of TB among both people born outside the UK (number: -13.8%, rate: -8.6%) and in the UK (number: -10.3%, rate -11.5%).
Treatment outcomes in drug sensitive cohort
The overall proportion of people with drug sensitive TB (with an expected treatment duration of less than 12 months) who completed treatment by 12 months remained unchanged in 2019 (82.0%) compared to 2018 (84.8%). The overall proportion of people who died (4.2%) or were lost to follow-up (3.4%) at the last reported outcome was comparable to previous years.
Antimicrobial resistance
The proportion of people with initial isoniazid resistance without multi-drug resistant TB (MDR-TB) in 2020 remained high at 6.5%, after remaining relatively consistent at an average of 5.4% over the past 10 years before 2017. The number of people with rifampicin- or multi-drug resistant (RR-MDR) TB increased between 2019 (n=53) and 2020 (n=58).
TB in under-served populations
In 2020, 12.7% of people diagnosed with TB who were aged 15 years or older had a social risk factor (SRF) – current alcohol misuse, current or history of drug misuse, homelessness or imprisonment. The 2020 proportion of people with an SRF was slightly lower than 2019 (13.9%). This proportion was highest among people born in the UK (22.6%) compared to those born outside the UK (9.1%). People with an SRF were more likely to have pulmonary disease and worse treatment outcomes
Conclusions
In 2020, there were 4,125 people notified with TB, a fall of 12.6% from 2019 in the number of notifications. In 2019 the rate had risen for the first time since 2011 and that rise has not been fully explained. The rate of TB in England was 7.3 per 100,000 in 2020. However, the period covered by this report was heavily affected by the coronavirus (COVID-19) pandemic, which has had complex impacts on healthcare access and delivery, migration and social behaviours, all of which may have influenced TB transmission, diagnoses and notifications.
A decline in the reported number and rate of people notified with TB in 2020, after the small rise in 2019, should be viewed with caution in the light of the significant impact of the COVID-19 pandemic. There are still significant hurdles to be overcome to reach the end TB pre-elimination goal of 1.0 per 100,000 by 2035. These include a continuing high proportion of cases with social risk factors and ongoing delays between symptom onset and start of treatment.
In England, nearly 60% of local authorities have now achieved a 3-year average TB incidence of less than 5.0 per 100,000 and 12 of these have reached the WHO End TB pre-elimination target rate of less than 1.0 per 100,000.
National Poisons Information Service (NPIS) annual report
UK healthcare professionals made more than 780,000 visits (‘user sessions’) to the NPIS’s online TOXBASE database in 2020 to 2021, and more than 2,300 telephone enquiries were referred to an NPIS consultant toxicologist, according to the recently published ‘NPIS annual report for financial year 2020 to 2021’.
Hospital departments are principal users of the service – more than 150,000 poisoning-related hospital presentations occur in the UK each year. Other users are NHS telephone advice services – such as NHS 111, NHS 24 and NHS Direct – and individual professionals in the field, such as ambulance service personnel.
A high proportion of all enquiries relate to patients presenting to hospitals following suspected self-inflicted poisonings or the effects of substance misuse; also following accidental ingestions of potentially toxic substances, errors in dosing of medicines, or environmental or occupational exposures. Classical drugs of misuse such as diazepam, cocaine, cannabis, MDMA and heroin continue to dominate NPIS activity.
The NPIS is uniquely placed to collate poisoning surveillance data and identify national trends and these are presented in the annual report. Particular topics selected for review are: drugs of misuse; pesticides; carbon monoxide; dinitrophenol; and toxicovigilance during the COVID-19 pandemic.
Update on lead exposure in children in England: 2020 cases
UKHSA has published the fourth annual report on lead exposure in children in England. The report summarises the surveillance of cases reported to UKHSA from 1 January to 31 December 2020. Children under 16 years old with an elevated blood lead concentration ≥0.48μmol/L (equivalent to ≥10μg/dl) require case management by Health Protection Teams to receive public health interventions to identify and remove the source of lead.
Thirty-five cases of lead exposure in children were notified to Public Health England (PHE) in 2020. The main epidemiology findings are:
- most cases (60%) were directly notified by surveillance by participating laboratories; substantially more cases (40%) were notified through other routes compared to previous years (normally around 20%)
- the number of cases detected was lower than the expected incidence of lead exposure based on international population survey data
- the average detection rate for England between 2015 and 2020 was 4.62 cases per million children aged 0 to15 years, although there was large regional variation
- cases were typically 1 to 4 years of age, male, and resident in more deprived areas
The key messages and recommendations include:
- lead is a persistent environmental contaminant that has toxic effects in humans even at low blood lead concentrations, although risk is reduced as levels drop
- children exhibiting pica – or other hand-to-mouth behaviour – in environments with lead hazards are likely at highest risk of exposure
- clinicians should be aware of important sources of lead exposure, children most at risk, and presenting symptoms or signs of exposure
- cases with a blood lead concentration above the public health intervention level for lead should be notified to health protection teams for active public health case management
UKHSA lowered the public health intervention concentration for lead from ≥10μg/dL (≥0.48μmol/L) to ≥5μg/dL (≥0.24μmol/L) for children under 16 years and for pregnant women, with effect from 5 July 2021. UKHSA is working with stakeholders to support this change and has produced updated guidance and advice to support this change including a series of stakeholder events.
Annual review of infections in UK blood, tissue and organ donors
The joint NHS Blood and Transplant and UKHSA Epidemiology Unit has published its annual review entitled ‘Safe supplies 2020: progress in a pandemic’. The unit is responsible for the surveillance systems which report on infections in blood, tissue, cell and organ donations across the UK.
This year’s report presents data up to 2020 that demonstrates the continued low risk of infection from blood transfusion in the UK. UKHSA and NHSBT use the data to ensure the best safety measures are applied and to provide evidence for ongoing reviews of donor selection and testing policies. The new review, for example, includes the findings and recommendations of the FAIR project (For the Assessment of Individualised Risk) – see below.
In 2020, over 1.7 million blood donations were screened across the UK of which 176 (0.01%) were confirmed positive for either hepatitis B virus, hepatitis C virus, HIV, human T-cell lymphotropic virus (HTLV) or treponemal antibody (syphilis) and were discarded. The majority of these were detected in donations from new donors (129, 73%) and these were mostly either past or chronic infections in the donor. A further 409 donations tested positive for hepatitis E virus and were discarded.
The chance of not detecting and releasing an infectious donation made by a donor who has very recently acquired hepatitis B, hepatis C or HIV is estimated over a 3-year period each year. The current estimate for 2018 to 2020 remains at less than one in a million. Of these 3 viruses, hepatitis B carries the highest risk of not being detected and released with potential for being transfusion-transmitted. Since 2012 the HIV and hepatitis C virus risk has declined, and the hepatitis B virus risk remained relatively stable.
In 2020, 1 hepatitis B investigation was reported to Serious Hazards of Transfusion (SHOT) as a probable transfusion-transmission. A suspected HEV investigation from 2019 was closed in 2020, also assigned as probable. In 2020, there were no proven bacterial transmissions were reported. More information is available in the SHOT report.
More individualised risk assessment
FAIR is the project name given to the work that reviewed the blood donor selection policy affecting men who have sex with men (MSM) led by the UK blood services, UKHSA, Nottingham University and a range of stakeholders including LGBT+ groups. FAIR assessed whether the UK blood service could move to a more individualised blood donor selection policy while maintaining safety. Also included are the updated residual risk estimates among blood donations, a summary of markers of infections detected in blood, tissue and organ donors and reported transfusion transmitted infections.
In December 2020, following the FAIR review, UK ministers agreed to change to a more individualised blood donor selection policy to allow some MSM to donate without a deferral. This was a change from the 3-month deferral for MSM, and others with sexual partners who are at increased risk of infections. The FAIR review refined the behaviours and circumstances that are higher risk by triangulating evidence on from the general population, blood donors and acceptable and effective questions from socio-behavioural work.
A policy based on an individual’s sexual activity was perceived as fair, more inclusive and unlikely to deter people from donating. The same questions are now asked of all donors and can allow anyone who has not had a new sexual partner in the last 3 months to give blood if all the donation safety criteria are met. FAIR was implemented by the UK blood services in 2021 and active post implementation monitoring is in place.
Convalescent plasma donations
In April 2020 the UK blood services began collection of convalescent plasma (CVP) to assess its effectiveness in clinical trials. Potential donors who had who had recovered from SARS-CoV-2 infection were targeted, with male and hospitalised patients prioritised for the best chance of obtaining a donation with high antibody levels. Between April and December 2020 in England, 33,301 CVP donations and 11,234 samples were collected with 46 confirmed positive (0.1%). Higher, but not significantly different, rates of hepatitis B and C in CVP donations from new donors were recorded, compared with new whole blood donations. These appeared to be longstanding infections. Syphilis total rates were significantly higher in CVP donors but only 3 of 25 donors had a recent infection.
New and emerging infections
Another role of the unit is in horizon-scanning for infectious diseases that could potentially affect the safety of the UK blood supply, particularly new and emerging infections. This work is carried out in conjunction with colleagues across UKHSA and with blood services around the world. The year 2020 was of course dominated by the COVID-19 pandemic but the year also saw Usutu virus identified in birds in the UK: the public health risk was low but this indicated the potential for West Nile virus transmission. Tick-borne infections were also notable, with the first locally acquired babesia and the second locally acquired tick-borne encephalitis human cases recorded in the UK.
In 2020 the blood services risk assessed COVID-19 infection with donor deferrals for any symptomatic individuals, and after having a vaccine put in place, as a precautionary measure since there was no evidence for transfusion transmission. Donations were able to continue during the pandemic restrictions with extra safety precautions in place including social distancing and face coverings to protect staff and donors at session, recognised as COVID-secure by PHE.
Bone and tissue donations
In recent years there has been a planned reduction in the collection of bone from living surgical bone donors. In 2020, no donors tested positive. Deceased tissue donors have the highest rates of positivity which may reflect their age: 5 donors had chronic hepatis B, 3 hepatis E, 1 for HTLV and 2 for past syphilis. During 2020, no cord blood donors tested positive for markers of infection – antenatal screening will generally select out women positive for hepatis B, HIV and syphilis.
NHSBT is also responsible for deceased organ donation across the UK. Some deaths in the UK are in circumstances where organ donation is possible, but donors or families must agree. Deaths increased in the UK during 2020 due to the impact of the pandemic, but the number of donors decreased by almost a third as patients who tested positive for the virus were unable to donate. During 2020, 1,644 people became consented potential donors with family consenting to donation. Around three quarters became actual donors with at least one organ retrieved for transplantation, and 95% became utilised with at least one organ transplanted.
Organ donation can save and transform lives, and markers of infection are not necessarily barriers for transplantation. Of the 1107 utilised donors, 11 were reactive for viral infections, 5 of which were hepatitis C. Hepatitis C is the most common virus among deceased organ donors, NAT testing for increased risk donors such as people who have injected drugs can reduce hepatitis risk for recipients.
Full details of data sources used by NHSBT and UKHSA, and of methods used in compiling the report, together with infographics, are available on the NHSBT website under Latest annual report.
For further information email: epidemiology@nhsbt.nhs.uk
If you are interested in donating blood see the NHS Blood and Transplant Give Blood website or call 0300 123 2323 for more information. To join the organ donor register see the NHS Blood and Transplant Organ Donation website.
Surveillance reports in this issue
Lead Exposure in Children Surveillance System (LEICSS) annual report (data for 2020)
Enterococcus spp. bacteraemia in England: annual report 2020
