[Withdrawn] Health matters: improving the prevention and diagnosis of bowel cancer
Published 27 June 2016
Summary
Public Health England (PHE) wants to see fewer people develop bowel cancer and encourage more eligible people to come forward for screening, to achieve an uptake target of 75%.
This resource highlights what we know about how bowel cancer affects people, with an aim to help achieve these goals.
The scale of the problem
Bowel cancer, also known as colorectal cancer, is one of the most common cancers, accounting for over 10% of all cancers in England. Every 15 minutes someone is diagnosed with bowel cancer in the UK.
In 2014, it was the third most common cancer in men and women but the second biggest killer after lung cancer. It killed 13,036 (7,049 men and 5,987 women) in England in 2014 which is equivalent to 35 people every day.

Bowel cancer who it affects infographic
Prevention
Just over half (54%) of bowel cancer cases in the UK are linked to lifestyle risk factors.
Diet plays a major role in bowel cancer risk. The evidence has been steadily growing around the risks of eating large amounts of red meat and processed meats, such as sausages, bacon, ham and salami.
The International Agency for Research on Cancer (IARC) has classified processed meats as Group 1 which means that they cause cancer, and red meat as Group 2A which means that they probably can cause cancer.
It is estimated that around 1 in 5 bowel cancers in the UK are linked to eating these meats. Limiting the amount of red meat consumed to 500 grams or less (cooked weight) per week and limiting the amount of processed meats eaten can help lower the risk.
The World Cancer Research Fund classifies dietary fibre as probably protective against bowel cancer. About 12% of bowel cancer cases in the UK are linked to eating less than 23g of fibre a day.

Reducing your risk of bowel cancer infogarphic
Early detection
Overall, bowel cancer survival is relatively good; 78% of male and 76% of female bowel cancer patients survive for 1 year following diagnosis.
Early detection is fundamental to short and long-term survival. The earlier bowel cancer is diagnosed the better.
One year survival for those diagnosed with a stage 1 (earliest) cancer is 98% for men and women. When detected at stage 4 (the most advanced stage), 1 year survival is much lower: 44% for men and 35% for women.
Cancers can be diagnosed from a number of different routes. Often this is through screening or when a GP refers someone when they present with symptoms. Sometimes, however, cancer is diagnosed as a result of an emergency presentation.

Early detection of bowel cancer
Cancer is more likely to be detected at an early stage via screening or via a 2 week wait GP referral. It is more likely to be diagnosed late when it’s diagnosed as an emergency presentation.
One year survival for bowel cancer detected through screening is 97%, but through emergency presentation it is only 49%, likely reflecting the later stage at diagnosis.
Patients from more deprived areas are more likely to be diagnosed after an emergency presentation, and less likely to be diagnosed via screening.
Warning signs
Most patients with bowel cancer present with one or more of the following symptoms:
- a persistent change in bowel habit, especially going to the toilet more often or diarrhoea for several weeks, usually with blood on or in the stools
- blood in the stools without other haemorrhoid symptoms, such as soreness, discomfort, pain
- abdominal pain, discomfort or bloating always provoked by eating, sometimes resulting in a reduction in the amount of food eaten and weight loss
- a lump in the abdomen
The symptoms of bowel cancer can be subtle and don’t necessarily make you feel ill. Anyone with symptoms is encouraged to speak with their GP as soon as possible.
The NHS Bowel Cancer Screening Programme
Screening aims to lower the burden of cancer in the population by discovering disease before it develops into cancer or in its early stages. Bowel polyps are common but only around 1 in 10 will progress to potentially cancer. This progression is a slow process, generally taking about 10 years. This means there is a good window of opportunity for screening, prevention and early detection.
The earlier bowel cancer is diagnosed the more effective treatment will be. More than 9 in 10 bowel cancer patients will survive for more than 5 years if diagnosed at the earliest stage. Early stage cancer treatment is also significantly less expensive to the NHS than treatment for advanced disease.
In England, screening is offered every 2 years for men and women aged 60 to 74. Screening is also available every 2 years for older individuals on request.
The national programme currently uses the guaiac-based faecal occult blood test (gFOBt), which is used to collect samples from 3 bowel motions. These samples are sent to a lab and examined for hidden traces of blood in the stool. If positive, the person is invited to a screening practitioner consultation, to discuss the need for further investigations by way of a colonoscopy.
Meta-data analysis from 3 randomised controlled trials found that bowel cancer mortality was reduced by 16% in populations offered gFOBt screening compared with populations not offered screening.
Bowel scope screening
Bowel scope screening is currently being rolled out in England as part of the NHS Bowel Cancer Screening Programme. This is a one-off test that complements gFOBt and is designed to prevent bowel cancer.
It is offered at the age of 55 and involves the use of flexible sigmoidoscopy to look for the presence of adenomas and polyps in the sigmoid colon, rectum and anus.
The UK Flexible Sigmoidoscopy Screening trial found that cumulative incidence, including prevalent cancers detected at screening, was reduced by 50% for cancers in the rectum and sigmoid colon, and by 33% for bowel cancer overall. Bowel cancer mortality was reduced by 43%.
The trial concluded that bowel screening using flexible sigmoidoscopy is safe and confers a substantial and long-lasting benefit when offered once between the ages of 55 to 64.
The aim is for all bowel screening centres in England to start bowel scope screening using flexible sigmoidoscopy by the end of December 2016.

What happens after screening infographics
FIT testing
Public Health minister Jane Ellison confirmed this month (June 2016) that the Faecal Immunochemical Test (FIT) will replace gFOBt as the primary test for bowel cancer. The age range for screening will remain the same.
FIT is a better, simpler version of the screening test. It doesn’t just detect whether blood is present or not in stool samples, but detects the amount of blood present. It is also specific to human blood unlike gFOBt which detects animal blood ingested via diet. This makes it a more sensitive test, and it also requires only a single sample.
It has been estimated that the new test will increase screening uptake by around 10%; meaning an additional 200,000 people could be tested each year.
Results of a 6-month FIT pilot involving 39,460 patients showed almost double the uptake with FIT than with gFOBt for previous non-responders (up from 14.5% to 26.6%).
There was an increase in participation for those invited for the first time, from 50.2% to 61.5% and also for those who had participated previously (from 86.6% to 91.1%).
Of particular note is the increase in uptake in the traditionally ‘hard to reach’ deprived population, which was up from 46.9% to 55.1%.
Other advantages of moving to the use of FIT include:
- an easier to use kit
- FIT can be measured more reliably using a machine rather than the human eye
- FIT is more sensitive than gFOBt and therefore can help detect cancers more reliably and at an earlier stage
- increased test sensitivity enables FIT to detect more polyps and adenomas, which may have gone on to develop into bowel cancer in the future
Tenth anniversary of the NHS Bowel Cancer Screening Programme
The NHS Bowel Cancer Screening Programme, based on gFOBt, is now in its 10th year. More than 30 million invitations were sent out and more than 18.4 million kits were returned.

Bowel screening 10th anniversary infographics
Understanding the pros and cons of screening
It is important that health professionals explain to patients the risks and benefits of bowel screening. These are outlined in leaflets that accompany all screening invitations, and all abnormal result letters (which include a referral to discuss colonoscopy).
Benefits of taking part in bowel cancer screening include:
- regular bowel cancer screening reduces the risk of dying from bowel cancer by 16% in the population invited
- detecting polyps that may develop into cancer over time; removing polyps during a colonoscopy can reduce your future chances of developing bowel cancer
- the gFOBt or FIT test can be done in the privacy of your own home
Risks of taking part in bowel cancer screening include:
- the chance that a cancer is missed if it was not bleeding when the screening test was taken
- not all bowel cancers detected by screening can be successfully treated
- although rare, there are risks associated with having a colonoscopy, including bleeding and bowel perforation
It is important that people still act on symptoms even if they’ve taken part in bowel screening because screening won’t pick up all anomalies and polyps can develop in the 2 years between screening tests.
Increasing uptake of bowel cancer screening
Bowel screening uptake across the UK is not as high as seen in the other cancer screening programmes, and there are considerable inequalities between areas and demographics. Since the start of the screening programme over 30 million people have been invited or invited again to participate in screening. The most recent uptake figure from PHE stands at 56%.
In some parts of the country, uptake is as low as 33% according to figures from Bowel Cancer UK, Seven out of 10 of the worst areas in the country are in London and 44% of clinical commissioning groups (CCGs) in England are below the national average.
Bowel cancer screening uptake in England is lowest in the youngest screening age groups. Uptake is higher in females than males in every age group, though the gap narrows with increasing age.
PHE targets 75% of eligible people taking up invitations for bowel cancer screening. In order to reach this, PHE is working to address a range of barriers to increasing uptake, including:
- cultural taboos around collecting and storing samples
- perception of a home-based test as less important than one delivered by a health professional
- preferring not to know rather than deal with the implications of an abnormal result
- a misconception that the test is not applicable if you don’t have any apparent symptoms of bowel cancer
- working with CRUK on developing a Be Clear on Cancer-branded bowel screening campaign pilot
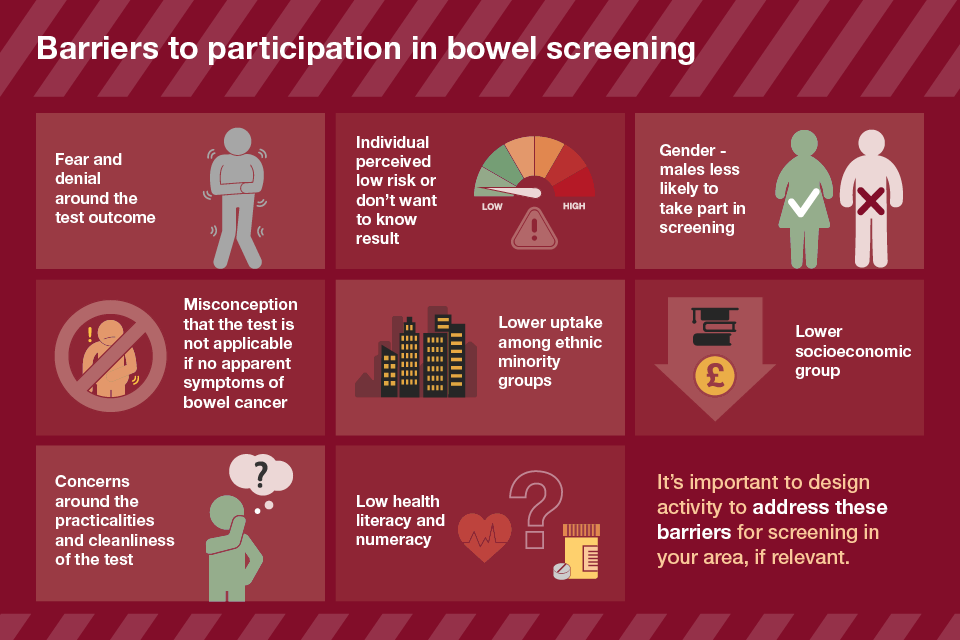
Barriers to participation in bowel screening infographics
Men are less likely to take up screening (55% compared with 60% of women) but are more likely to get an abnormal gFOBt result and more likely to be diagnosed with cancer or have polyps found.
Ethnicity and social deprivation are major determinants of bowel cancer screening uptake in the UK, as with many other cancer screening programmes. Gender is also a determinant in bowel cancer screening in England, with women more likely to take part.
The biggest boost to screening uptake could be achieved by the national roll out of the FIT test, but there are a number of other interventions that could be used to increase uptake of gFOBt bowel cancer screening, while still enabling people to make an informed choice.
GP endorsement
UK research shows that when an individual is made aware that their GP supports the screening programme, bowel screening uptake is increased by up to 6%.
Combining this with an enhanced patient information leaflet can increase uptake by up to 12%. An enhanced information leaflet includes information on how to use the kit and explicitly addresses perceived barriers.
Telephone advice
Phoning potential participants to offer information and answer questions, in combination with a GP endorsement letter, has been found to increase screening uptake by around 8%.
This approach was trialled in areas of low socio-economic status and high ethnic diversity, demonstrating that telephone advice could help to address inequalities in screening uptake.
PHE and Cancer Research UK (CRUK) London campaign
A kit enhancement pack, containing a stool catcher and gloves, combined with outdoor advertising and a CRUK endorsement flyer inserted inside an NHS test kit mailing has been found in a London pilot study to be effective in increasing bowel cancer screening uptake by 6.1% in ages 60 to 69 and 7.3% in ages 70 to 74.
Face to face promotion
A study found that providing face-to-face health promotion sessions at an individual’s own GP practice, alongside pictorial and multi-lingual guides and non-latex gloves, increases bowel screening uptake by around 5%.
The sessions took place after people had received a GP endorsement letter 2 weeks after they were due to return their screening kit.

How to increase uptake pf bowel cancer screening infographic
Cancer Research UK’s online hub contains information on the evidence on the impact of different initiatives, as well as useful resources for people looking to take action in their area.
How to improve the prevention and detection of bowel cancer
The role for commissioners of services
Local authorities have responsibility for commissioning behavioural and lifestyle campaigns to prevent cancer. They are best-placed to determine which combination of initiatives, across education, housing, planning and healthcare, would deliver the most impact, and which should be led through workplace health and wellbeing initiatives.
About a third of cancers are caused by smoking, diet, alcohol and obesity. To help reduce people’s risk of getting cancer, PHE has produced advice on:
Resources are available for local authorities to promote PHE’s Be Clear on Cancer campaign which was developed to raise awareness of the symptoms of bowel cancer, and to encourage people who have the key symptoms to go to their doctor without delay.
Research of the campaign has shown increased attendances for symptoms directly linked to the campaign, with the largest percentage increase seen in people aged 50 to 59. The increase was significantly greater for men and in people attending practices in the most-deprived quintile.
PHE’s One You campaign supports adults to improve lifestyle behaviours and reduce their risk of developing diseases like bowel cancer. A range of personalised tools are available via the How Are You online quiz, which has been completed by over 1 million people since it launched in March 2016.
Working with hard to reach groups
Screening should be delivered in a way which addresses local health inequalities, tailoring and targeting interventions when necessary.
Local authorities should work in collaboration with CCGs and screening partners to identify any barriers to accessing screening in their local area and to encourage more people from hard to reach groups to participate in screening.
Hard to reach groups include:
- individuals who have hearing problems or are deaf
- individuals who are partially sighted or blind
- individuals with a physical disability
- individuals with a learning disability
- people from ethnic minority backgrounds who have no or poor understanding of the English language
- travelling communities
- lesbian, gay, bisexual and transgender individuals
PHE guidance sets out tips for overcoming general barriers to accessing screening.
PHE’s Fingertips tool provides cancer services data at GP and CCG level to inform commissioning decisions including data on:
- cancer screening
- 2 week wait referrals
- diagnostic services
- emergency presentations and admissions

The role of local authorities and GPs
The role of the GP
Encouraging patients to attend for screening
GPs are not routinely involved in the bowel cancer screening programme because the test is done at home. This lack of involvement can discourage some people from taking part.
GPs have a key role to play in providing details about the screening programme and discussing the pros and cons of screening with patients so that they are able to make an informed choice about whether or not to participate.
Addressing patient-specific factors such as poor knowledge of the benefits of bowel screening, using the gFOBt, and perceived difficulties of completing the bowel cancer screening procedure could help to increase screening participation.
The Royal College of General Practitioners has developed a 30-minute online bowel cancer screening course which highlights the importance of the GP’s role in the NHS Bowel Cancer Screening Programme.
Studies on GP endorsement have shown that the public value the opinion of their GP and this can help to reduce screening variations.
CRUK has developed a GP letter template to promote bowel screening that can be customised by practices to send to their patients. It has been found that it is better if the endorsement letter is signed by the patient’s own GP rather than by the more impersonal ‘on behalf of the practice’.
Practices in London are due to implement their own endorsement letters and reminders in June 2016.
Practices can raise awareness of the bowel screening programme by:
- placing promotional posters in the waiting area and other appropriate areas such as toilets
- using health screens to display bowel screening awareness DVDs, where these are available
- setting up bowel cancer screening promotion display stands
- organising an awareness event at the practice
- conducting an outreach event in conjunction with local community or religious groups
Making an early diagnosis of bowel cancer
The updated NICE suspected cancer referral guideline aims to support GPs to recognise the signs and symptoms of 37 different cancers, including bowel cancer, and refer people for the right tests faster.
The guideline focuses on the symptoms that a patient might experience and go to their doctor with.
NICE recommends referring people using the suspected cancer pathway referral (for an appointment within 2 weeks) for bowel cancer if:
- they are aged 40 or over with unexplained weight loss and abdominal pain or
- they are aged 50 or over with unexplained rectal bleeding or
- they are aged 60 or over with iron‑deficiency anaemia or changes in their bowel habit
- or tests show occult blood in their faeces
- they have a rectal or abdominal mass
Read the full NICE guideline for more details on when to refer.
Investing in workforce and training
Supporting the rollout of FIT
The National Cancer Taskforce Strategy published in 2015 highlighted the need to address current workforce deficits in endoscopy services. The introduction of the FIT test is likely to increase demand on already stretched endoscopy services due to improved uptake and also because FIT is a more sensitive test.
CRUK scoping the future report predicts that more than 750,000 additional endoscopy procedures a year will be undertaken by 2020 – a 44% increase on current activity.
PHE is working to:
- design and develop an implementation strategy for FIT screening
- ensure all bowel screening centres have started offering bowel scope screening by the end of December 2016
- provide quality assurance support to the implementation of bowel scope screening
- procure IT systems to support the implementation and monitoring of FIT
