Health matters: combating high blood pressure
Published 24 January 2017
Summary
This professional resource outlines how providers and commissioners can reduce the population average blood pressure through improved prevention, detection and management.
Scale of the problem
Defining high blood pressure
Blood pressure is measured in millimetres of mercury (mmHg) and is recorded as 2 numbers usually written one above the other. The top number is the systolic blood pressure - the highest pressure in blood vessels and happens when the heart contracts, or beats. The bottom number is the diastolic blood pressure - the lowest pressure in blood vessels in between heartbeats when the heart muscle relaxes.
The normal or ideal adult blood pressure is considered to be between 90/60mmHg and 120/80mmHg.
The National Institute for Health and Care Excellence (NICE) defines high blood pressure, also known as hypertension, as a clinic blood pressure of 140/90 mmHg or higher and either a subsequent ambulatory blood pressure monitoring daytime average or home blood pressure monitoring average of 135/85 mmHg or higher.
Blood pressure readings between 120/80mmHg and 140/90mmHg are defined as high normal blood pressure. High blood pressure doesn’t just happen to older adults. Over 2.1 million people under the age of 45 had high blood pressure in England in 2015.
Why focus on high blood pressure
The Global Burden of Disease 2015 highlights that high blood pressure is the second biggest known global risk factor for disease after poor diet. In the UK, high blood pressure is the third biggest risk factor for disease after tobacco smoking and poor diet.
High blood pressure is, however, the largest single known risk factor for cardiovascular disease and related disability.
High blood pressure increases the risk of:
- heart failure
- coronary artery disease
- stroke
It can also increase the risk of chronic kidney disease, peripheral arterial disease, and vascular dementia.
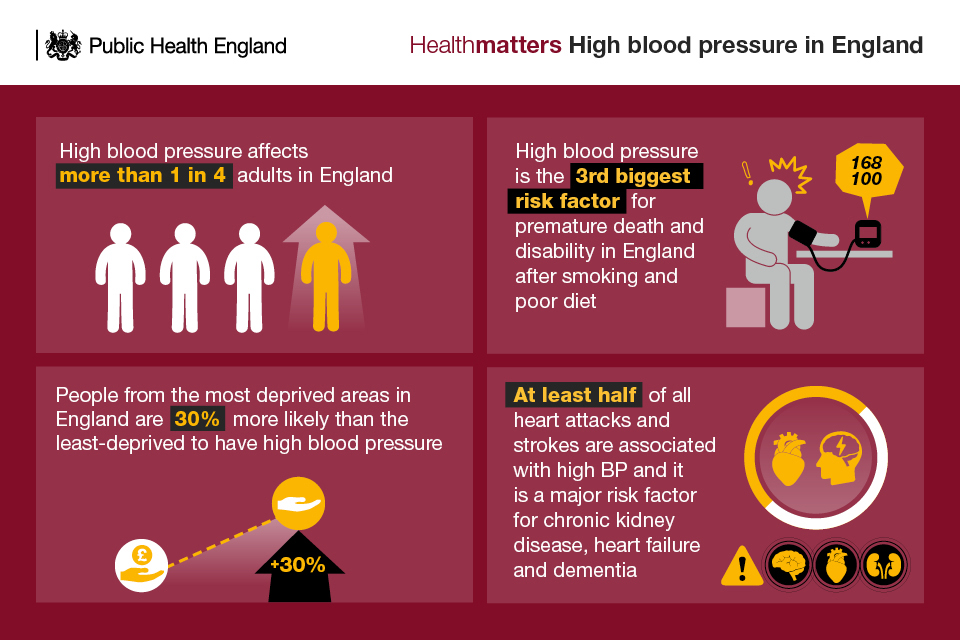
Approximately 1 in 4 adults worldwide have high blood pressure. It is projected to affect more than 1.5 billion people around the world by 2025.
The Global Burden of Disease 2015 report estimated that high blood pressure was responsible for 10.7 million deaths worldwide.
Often described as a ‘silent killer’ because it rarely causes symptoms, high blood pressure was responsible for around 75,000 deaths in 2015, according to the Global Burden of Disease report.
High blood pressure affects more than 1 in 4 adults in England, around 12.5 million people in 2015. The prevalence of high blood pressure for adults in England in 2015 was 31% among men and 26% among women, with little change over the last few years.
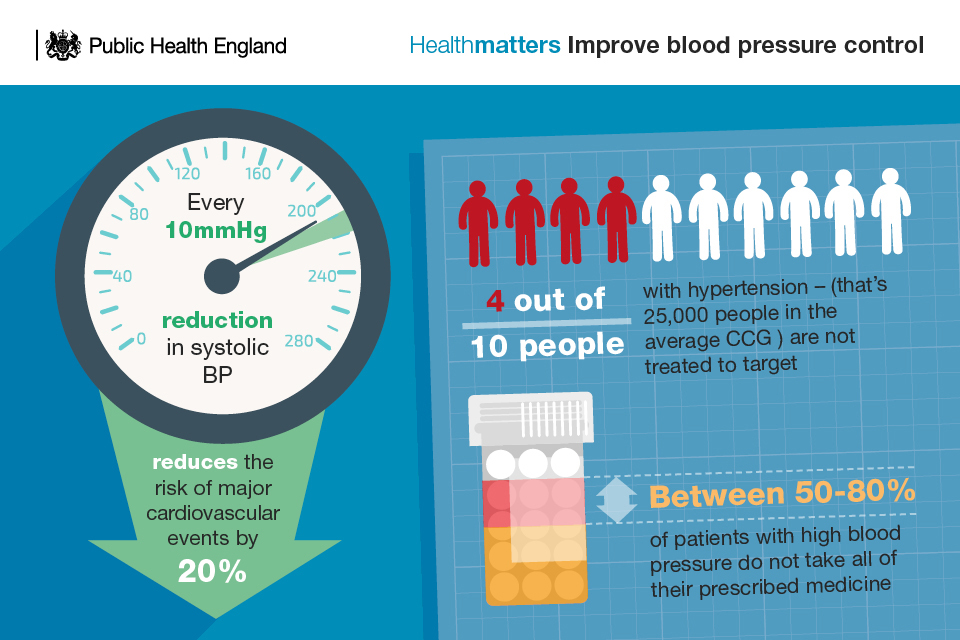
There is robust evidence that action to lower blood pressure does reduce the risk to health. For example, a major systematic review in the Lancet found that in the populations studied, every 10mmHg reduction in blood pressure resulted in:
- a 17% reduction for coronary heart disease
- a 27% reduction for stroke
- a 28% reduction for heart failure
- a significant 13% reduction in all-cause mortality
Some progress has already been made in reducing the population’s levels of high blood pressure. The Health Survey for England shows that the population average blood pressure in England has fallen over the last decade by almost 3mmHg systolic, though very little has changed over the last 3 years.
The proportion of adults with untreated high blood pressure has decreased from 2003 to 2015 for both sexes (from 20% to 15% among men and from 16% to 10% among women).
However, England’s performance in terms of diagnosing and treating high blood pressure is still a long way off compared to what has been achieved in countries such as Canada and the US.
In Canada, 65% of adults with high blood pressure are both diagnosed and managed to recommended levels, compared to only 35% in England.
Costs to the NHS
High blood pressure places a considerable strain on the NHS.
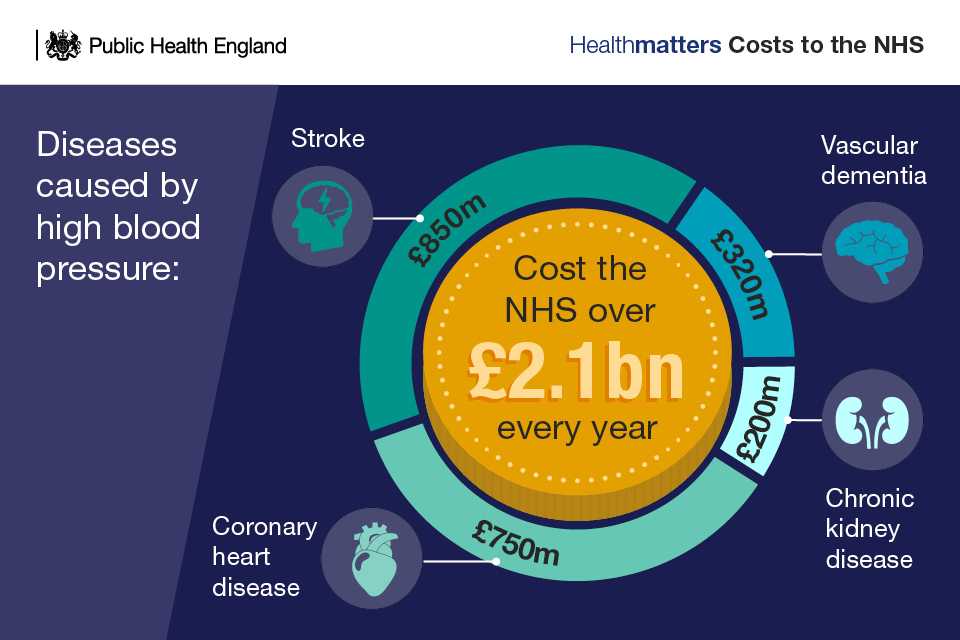
The Blood Pressure Action Plan published by Public Health England (PHE), and its partners in England’s Blood Pressure System Leadership Board, has called for action to reduce the population average blood pressure by 5mmHg through improved prevention, detection and management. Over 10 years, this reduction could save an estimated 45,000 quality adjusted life years (QALYS), and save £850m on related health and social care costs.
Sustainability Transformation Plans (STPs) offer a real opportunity for broad place-based partnerships to drive improvement in the prevention, detection and management of high blood pressure. This opportunity is highlighted in the STP aide-mémoires on prevention and primary care.
Preventing high blood pressure
It is estimated that up to 80% of premature deaths from cardiovascular disease, can be prevented through better public health. All blood pressure guidelines agree that support for behaviour change to address modifiable risk factors should be the first step in preventing high blood pressure.
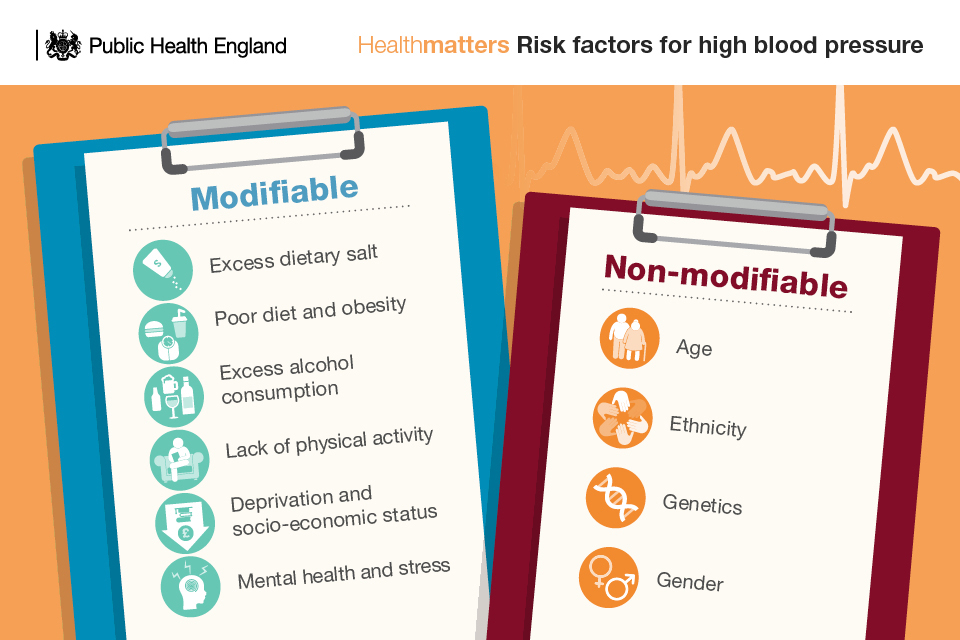
Who is at risk of high blood pressure
There are a number of modifiable and non-modifiable factors that can increase the risk of developing high blood pressure.
Non-modifiable risk factors
1. Age
In the UK, as in other developed nations, blood pressure tends to rise with age. In England, the increase in average systolic pressure between ages 16 to 24 years and 75 years and above is just under 20mmHg. This is thought to reflect the length of time that people are exposed to modifiable lifestyle risk factors.
2. Gender
Health Survey for England figures show that for any given age up to about 65 years, women tend to have a lower blood pressure than men. Between 65 to 74 years of age, women tend to have a higher blood pressure. In terms of prevalence, in England the proportion of the population with hypertension increases from 5% of men and 1% of women aged 16 to 24 years, to 58% in men and women aged 65 to 74 years.
3. Ethnicity
In England, people from Black African and Black Caribbean ethnic groups have a higher risk of hypertension than the general population, although any differences in hypertension between other ethnic groups is not always apparent.
Ethnic groups, such as South Asian, Black African and Black Caribbean communities, are more prone to developing type 2 diabetes which also increases the risk of having high blood pressure.
4. Genetics
Genetic factors play some role in high blood pressure, heart disease, and other related conditions. Research on twins suggest that up to 40% of variability in blood pressure may be explained by genetic factors.
Modifiable risk factors
There are a number of environmental risk factors that are driving the epidemic of cardiovascular disease. Health professionals and local authorities should raise awareness of these factors and encourage people to make healthy lifestyle changes.
1. Excess dietary salt
Excess dietary salt is one of the most important modifiable risk factors for high blood pressure. A high salt diet disrupts the natural sodium balance in the body. This causes fluid retention which increases the pressure exerted by the blood against blood vessel walls.
The Department of Health report ‘Salt reduction – onwards and downwards’ estimated that for every one gram of salt we cut from our average daily intake, there would be an estimated 4,147 fewer premature deaths. This will save the NHS £288 million each year.
In England, the salt reduction programme started in 2004 and continues today. It has focused on reducing levels of salt in a wide range of everyday foods as this is where most salt in the diet comes from. Salt that is added during cooking and at the table only accounts for around one-quarter of the salt we eat. Some significant reductions of up to 50% have already been achieved in some foods, such as bread.
The latest PHE National Diet and Nutrition Survey also found that adults’ average salt consumption has reduced in the decade from 2005 to 2014.
Average salt consumption for adults in England in 2014 (based on 24-hour urinary sodium excretion) was 8.0 grams per day. This has decreased from 8.5 grams in 2011 and 8.8 grams in 2005 to 2006. Overall salt intake has fallen by 11% since the 2005 to 2006 survey.
But average salt consumption remains too high as adults and children over 11 should have no more than 6g per day, younger children should have even less.
In parallel with work to remove 20% of the sugar from foods that contribute most to children’s sugar intakes, PHE expects all food businesses – retailers, manufacturers and the eating out of home sector – to continue to work to meet the existing salt reduction targets which are to be achieved by 2017 and cover 76 categories of foods.
2. Obesity
It is not just a diet high in salt that can increase the risk of high blood pressure. Eating a diet high in calories and fat, especially saturated fat which we are consuming too much of, and low in fruit and vegetables increases the risk of becoming overweight or obese. Obese men are more than twice as likely to develop high blood pressure and obese women 3 times more likely.
There is a strong and direct relationship between excess weight and high blood pressure.
According to the Health Survey for England, in 2015 over a quarter of adults (27% of men and women) were obese. A further 41% of men and 31% of women were classed as being overweight.
People should be encouraged to eat a healthier diet, including more fruit and vegetables (at least 5 portions a variety of fruit and vegetables a day), fibre (in the form of starchy carbohydrates) and oily fish, choosing lower salt, fat and sugar options in line with the Eatwell Guide.
3. Excess alcohol consumption
Alcohol has been identified as a causal factor in more than 60 medical conditions, including high blood pressure. Heavy habitual consumption of alcohol links to raised blood pressure. Blood pressure rises, in some cases to dangerous levels, when large amounts of alcohol are consumed – particularly when binge drinking.
Health Survey for England figures show that in 2015, using the CMO 2016 revised guidelines, 31% of men and 16% of women drank more than the recommended number of units per week, including 16% of men and 13% of women who drank at increasing risk levels, and 4% of men and 3% of women who drank at higher risk levels (more than 50 units a week for men, more than 35 units for women).
4. Lack of physical activity
People who do not take enough aerobic exercise are more likely to have or to develop high blood pressure. People in the UK are around 20% less active now than in the 1960s. If current trends continue, we will be 35% less active by 2030.
Figures from the Health Survey for England show that 67% of men and 55% of women aged 16 and over do at least 150 minutes of moderate physical activity per week.
Adults aged 19 to 64 should aim for 150 minutes of moderate intensity activity, in bouts of 10 minutes or more, each week. This can also be achieved by 75 minutes of vigorous activity across a week or a mixture of moderate or vigorous. Find out more in the Health matters edition on physical activity.
5. Impact of deprivation and socio-economic status
The burden of high blood pressure is greatest among individuals from low-income households and those living in deprived areas.
The PHE report ‘Tackling high blood pressure - from evidence into action’ estimated that people from the most deprived areas in England are 30% more likely than the least-deprived to have high blood pressure. These inequalities are wider still for outcomes of high blood pressure such as stroke and coronary heart disease.
6. Mental health
Many forms of mental health issues can affect heart disease. Anxiety and stress can increase hormones like adrenaline and cortisol which impact on blood pressure and heart rate.
It is also thought that people who are stressed deal with that stress by engaging in unhealthy eating habits, as well as smoking and drinking, and this increases their risk of having a high blood pressure.
Improving the detection and management of high blood pressure
Raise awareness
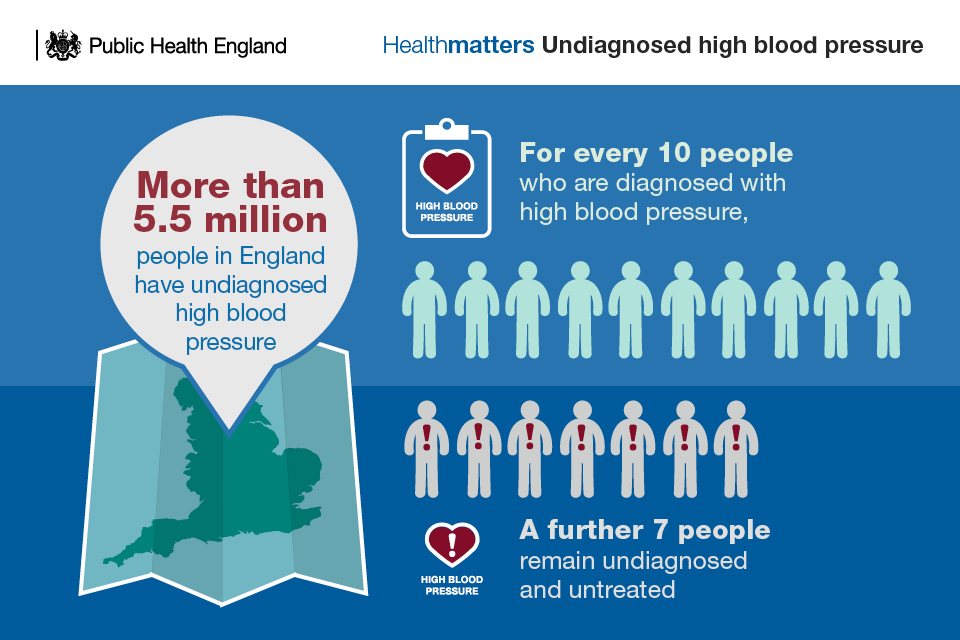
Over 10 years, an estimated 7,000 quality adjusted life years could be saved, and £120m not spent on related health and social care costs, if England achieved a 15% increase in the proportion of adults who have had their high blood pressure diagnosed .
However, half the adult population in England do not know what their blood pressure reading is.
Since its launch in February 2015, over a million people (1.18 million) have completed the Heart Age tool. Just over half (52%) knew their blood pressure.
NICE recommends that people get their blood pressure checked at least once every 5 years, and more frequently for people with high-normal blood pressure.
PHE supports the annual Know Your Numbers! campaign run by the charity Blood Pressure UK, which enables over 100,000 tests per year. Know your Numbers! Week involves hundreds of nationwide organisations signing up to provide free blood pressure tests and information at venues known as Pressure Stations.
Pressure Stations are located throughout the community including pharmacies, workplaces, GP surgeries, hospitals, health clubs, leisure centres, shopping centres and supermarkets.
The British Heart Foundation (BHF) is supporting a blood pressure programme aimed at implementing and evaluating community based early detection and management interventions, reaching high risk groups and those least likely to take up invitations for blood pressure testing through traditional routes.
Understand local need
PHE has a range of tools to help assess local need, plan services and undertake effective commissioning of healthcare services to detect high blood pressure.
Blood Pressure: How can we do better? local resources, designed by PHE and the BHF, are available for each clinical commissioning group (CCG). These reports show each CCG how they are doing in detecting and treating blood pressure, gains that can be made by lowering blood pressure, alongside practical tips from healthcare professionals on how you can improve detection and management of blood pressure.
The Healthier lives: high blood pressure interactive variation atlas presents performance data on blood pressure risk factors, prevalence, detection and care.
This data is available at local authority, CCG and general practice level, bringing together existing public data.
Detection
The majority of blood pressure testing is carried out in primary care. However, GP practices have, on average, no blood pressure reading in the last five years on file for 10% of their patients aged 45 or over. This represents a huge opportunity to pick up more cases of high blood pressure.
The PHE and BHF Blood Pressure – How can we do better? resource highlights a number of ways in which GPs, nurses and pharmacists can improve the detection of high blood pressure without adding significantly to GP workload. These include better use of audit and routine integration of blood pressure measurement into protocols for nurse-led management of multiple long term conditions.
NHS Health Check
The NHS Health Check, for adults in England aged 40 to 74, is an ideal opportunity for GPs and other healthcare professionals to offer patients regular blood pressure measures and give advice to promote a healthier lifestyle. Those who are eligible are invited once every 5 years.
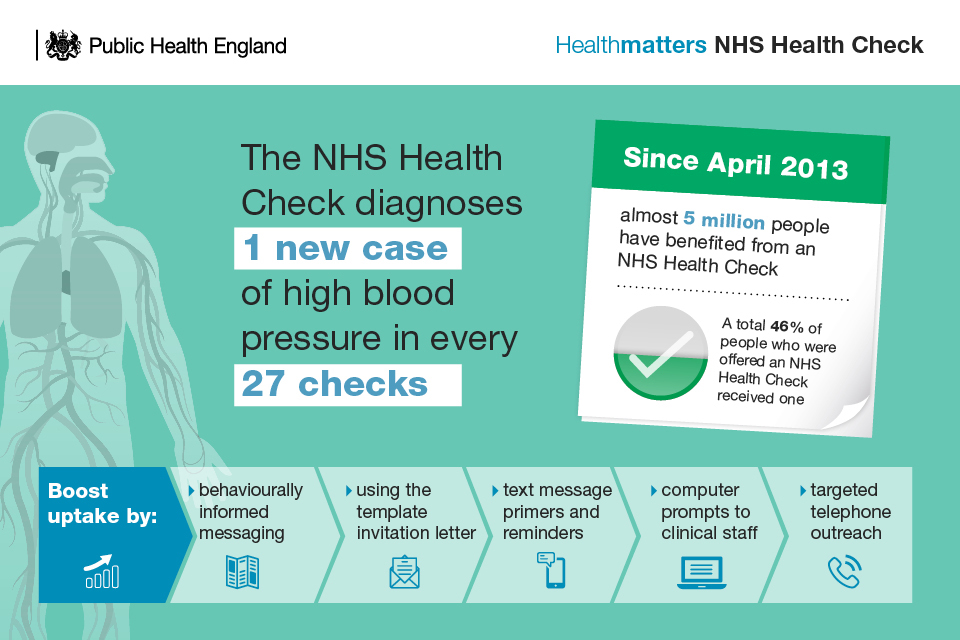
A large scale national evaluation of the NHS Health Check published in the Lancet found that it picked up 1 new case of high blood pressure in every 27 checks.
A study published in the British Journal of General Practice, looking at the first 5 years of the NHS Health Check programme in 3 London areas (City and Hackney, Tower Hamlets and Newham) found that 50% more new cases of hypertension were diagnosed in NHS Health Check attendees compared to non-attendees.
Since April 2013, just under 5 million (4.90 million) people have had an NHS Health Check. For 2016 to 2017, the number of people who were offered an NHS Health Check was 1.37 million. A total 48.3% of people who were offered an NHS Health Check received one.
PHE has published guidance on ways to increase the uptake of the NHS Health Check, which includes advice on:
- using the template invitation letter
- text message primers and reminders
- computer prompts to clinical staff
- behaviourally informed messaging
- targeted telephone outreach
Self-monitoring
Patients should be encouraged to self-monitor their blood pressure. Research suggests that self-monitoring of blood pressure is associated with moderate net reductions in both systolic and diastolic blood pressure of around 2.5 mmHg.
The British and Irish Hypertension Society has listed a number of validated monitors that are suitable for use at home and available at low cost. NHS Choices offers videos that can help patients to use blood pressure monitors.
Management
NICE recommendations guide healthcare professionals in the treatment of high blood pressure. Blood pressure treatment targets should be agreed with patients as part of a shared management plan, and should take account of co-morbidity, adverse effects and patient preference.
1 in 3 people with diagnosed high blood pressure are not treated to target, according to the BHF. This figure varies greatly between demographically similar CCGs and between neighbouring practices, suggesting significant scope for improvement.
For example, CCGs in England report between 73% and 86% of diagnosed hypertensive patients meeting the less stringent target of 150/90 for blood pressure control that is included in the Quality and Outcomes Framework– a 13% difference between lowest and highest control.
Roll out of the new NHS RightCare CVD prevention optimal value pathway will support improved detection and management in CCGs though the use of new approaches that mobilise the wider primary care team. Examples range from systematic use of pharmacists in diagnosis and treatment in Dudley to cooperation between local practices to deliver at scale optimisation of treatment for patients in Bradford.
Improve medication adherence
It is estimated that between 50 to 80% of patients with high blood pressure do not take all of their prescribed medicine.
Healthcare professionals can use shared decision making resources to help the individual make informed decisions about behaviour change and drug treatment. In addition, community and practice pharmacists can be mobilised to support patients in their use of medication, for example by integrating this into routine medicines use reviews.
Call to action
Health Matters - Combating High Blood Pressure
A video of a conversation between opinion leaders about how to prevent, diagnose and treat high blood pressure in England.
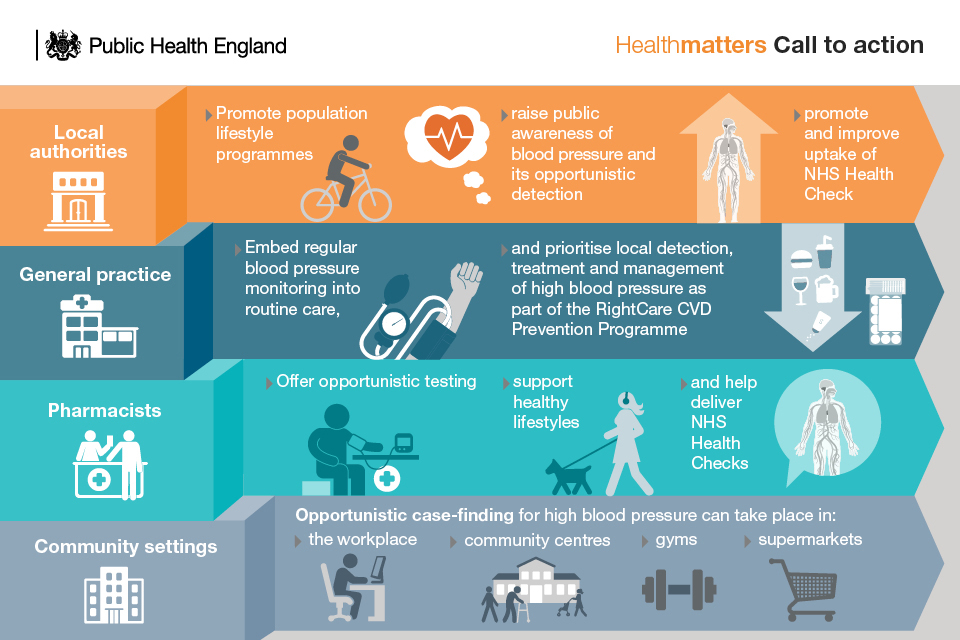
Local authorities
Local authorities have an essential role to play in promoting population lifestyle programmes that encourage physical activity, healthy eating, tackling overweight and obesity and reducing alcohol misuse.
PHE’s One You campaign, aimed at people aged 40 to 60, can help to motivate people to take steps to improve their health, through action on the main risk factors such as smoking, inactivity, obesity, alcohol consumption, all of which are relevant to reducing the risk of high blood pressure. It also includes advice on checking your blood pressure and the NHS Health Check.
Local authorities have a crucial role to play in making sure One You meets the needs of communities across the whole of England. A whole host of free assets and materials are available to use in your local area.
Local authorities should look to:
- develop and support initiatives to promote public awareness of blood pressure and its opportunistic detection
- work collaboratively with partners across the health and social care system to maximise the benefits of blood pressure prevention, detection and management
- promote and improve the uptake of the NHS Health Check
General practice
Teams should increase opportunistic blood pressure testing in the practice and make blood pressure testing routine in all nurse-led clinics such as asthma, COPD, diabetes, weight management, smoking cessation, as well as in other local enhanced service clinics.
Practices should prioritise blood pressure detection, treatment and management, embedded and implemented as part of local CVD prevention strategies, including:
- STPs
- Health and Wellbeing Boards’ Strategies
- RightCare CVD Prevention Optimal Value Pathway
Primary care should look to develop and support high quality training opportunities for relevant staff engaging in blood pressure detection and management.
Pharmacists
With 1.2 million people visiting a community pharmacy every day, pharmacy teams have an enormous opportunity to promote health at a local level. For some people, the local pharmacy will be their first point of contact, or their only contact, with a health care professional.
Healthy living pharmacy teams can increase opportunistic testing in pharmacies and help deliver brief advice for NHS Health Checks, and the prevention, early detection and management of high blood pressure.
Community care
Opportunistic case-finding for high blood pressure can take place in a range of community settings including:
- workplaces
- community centres
- gyms
- supermarkets (particularly those with on-site pharmacies)
