Diabetic eye screening: cohort management
Updated 27 September 2024
Applies to England
1. Introduction
1.1 Purpose and definitions
This guidance describes the management of people on the programme register of their local diabetic eye screening programme (DESP), known as the screening ‘cohort’. It defines the eligible population and which people should be invited for screening, excluded and suspended. It also provides guidance in special circumstances and rarer forms of diabetes that will require screening.
Here is a diagrammatic representation.
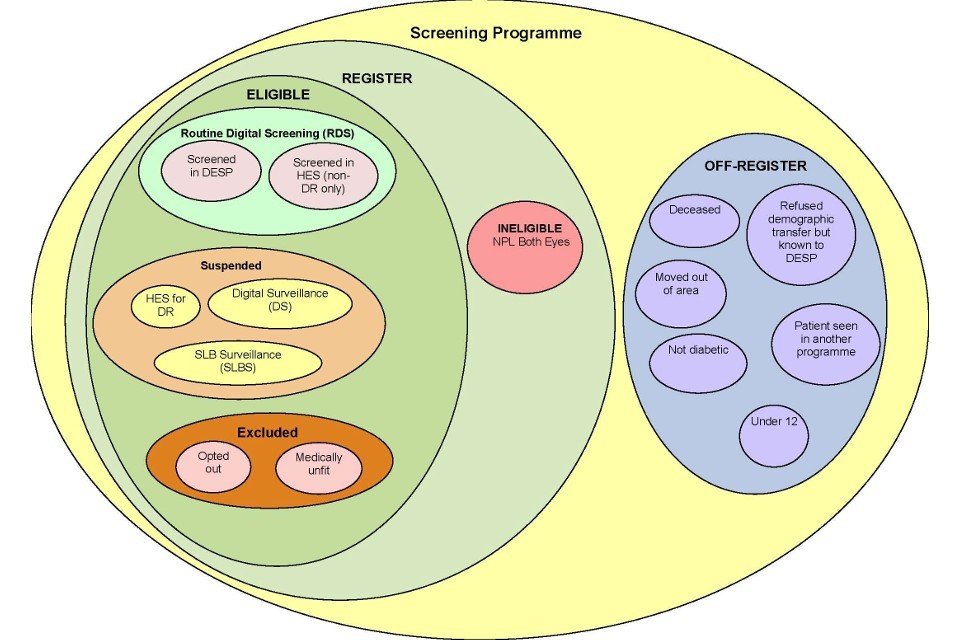
Diagram representing the cohort for the diabetic eye screening programme.
1.2 Eligible
The population that is entitled to an offer of screening from the NHS DESP. All people with diabetes over the age of 12 are eligible except those with no perception of light in both eyes.
The local screening programme should separate eligible people who are not invited into one of 2 categories: exclusions and suspensions. People who are suspended are under surveillance, assessment and/or treatment of their diabetic retinopathy by a clinician who has taken clinical responsibility for their care. People who are excluded are not invited for screening and are not screened or assessed for diabetic retinopathy.
1.3 Suspended
Suspended individuals are defined as eligible people who are not invited for annual digital screening and continue to have their retinae checked for diabetic retinopathy (DR). An eligible person who is suspended can be:
- under the care of the hospital eye service (HES) for management or treatment of DR
- under surveillance in a slit lamp biomicroscopy (SLB) clinic
- under surveillance in digital surveillance for DR
All people who are suspended are not invited for routine digital screening by the DESP and should be monitored through the failsafe system.
1.4 Excluded
Excluded individuals are defined as eligible population on the programme list who are not invited for routine digital screening and do not have their retinae checked for DR in another part of the screening pathway. This includes:
- those who have made a written informed choice to opt out of NDESP - referred to as ‘opt outs’
- those who could never be able to receive and/or benefit from treatment due to another existing condition - referred to as ‘medically unfit’
2. Suspensions
People with diabetes are suspended from screening when they are:
- under the care of hospital eye services (HES) for management of their DR
- under surveillance in a SLB clinic
- under surveillance for DR in a digital surveillance clinic
Those with non-DR lesions under the care of HES are not suspended.
GPs cannot suspend individuals as ‘under-care’ of ophthalmology. Not all assessments in the hospital eye clinic will involve a regular examination of the retina and the ophthalmologist may not know that the person has diabetes.
Only individuals who have been screened by the screening programme can be suspended. Those who are under the care of ophthalmology, but have not yet been imaged by the screening programme, should either be screened once by the screening programme or have documented evidence from the HES that they are being managed or treated for DR. If appropriate, the screening programme can then suspend the person. People who are suspended should be monitored through the failsafe system.
3. Exclusions
People with diabetes aged 12 and over should be sent an invitation for diabetic eye screening (DES) and given the opportunity to make their own informed choice about whether to accept the invitation. In cases where there is doubt over whether the person with diabetes should be invited or not, they should be sent an invitation. The decision to exclude a person with diabetes should only be done after careful assessment of the individual and their circumstances.
Exclusions from DES should form a very low proportion of the programme register; a national acceptable range will be determined as a baseline in the future.
An annual audit of exclusions should be carried out by the screening programme. This audit will include a review of:
- exclusions by GP practice, and an investigation where practice(s) are reporting unusual levels of exclusions
- the exclusion process, ensuring all exclusions have adequate supporting documentation
- the re-invitation process for people wishing to opt out
- those who have been assessed by the clinical lead as never being able to be screened by digital photography or SLB
3.1 Ineligible people
Ineligible individuals are defined as people with no perception of light in both eyes.
All people who are registered with severe sight impairment should be assessed by an ophthalmologist as some may still have some residual vision and therefore qualify for continued DES. People should continue to have DES unless there is no perception of light in both eyes.
4. Excluded categories
This category includes opted out and medically unfit people.
4.1 Informed opt-out and postponement of screening
An individual may choose not to attend or be invited for diabetic eye screening for a period of time. There can be several reasons why someone may wish to opt-out of screening. Local services must discuss the options available to the individual. They should also talk about the risks of not attending, ensuring the implications of this decision are clearly explained.
If a person with diabetes has concerns about screening, these should be addressed where possible and alternatives to opting out should be discussed. Local services should make sure there is a full explanation of the conversation and an audit history documented on their record.
Before an opt-out request can be actioned:
- the individual must be provided with sufficient information to enable them to make an informed decision about opting out of the DES programme, in a format which is accessible to them, including information on diabetic retinopathy, the screening process (including risks and benefits) and the consequences of attending or not attending
- the individual must be informed that opting out of the DES programme will stop them getting any future invitations or reminders about diabetic eye screening for the specified time period
- it must be made clear to the individual that they can return to the DES programme at any time
- the individual should put their request to withdraw from the DES programme in writing to confirm that they have made an informed decision
- if a person is unable to sign a standard form, for example because of a severe physical or learning disability, then alternative methods of communication are acceptable according to individual circumstances and the reasons should be documented
The returned opt-out form should be retained by the DES service. A copy of a confirmation letter stating that the person has opted out of the DES programme should be sent to both the person and their GP.
The DES service should automatically re-invite the person at the period of time indicated on the signed opt-out form asking if they would like to re-consider their decision to opt-out of screening. The individual’s status will revert to eligible for routine digital screening unless the person completes and returns a new opt-out form.
Individuals can choose to opt-out of the screening programme in this way for a maximum of 3 years.
Postponement of DES screening appointments
If an individual is invited for screening but does not wish to attend temporarily, they should be encouraged to postpone their appointment for a maximum of 6 months at a time. Services should not use the opt-out process for this purpose. Individuals should still be made aware of the risks associated with postponing their appointment and informed that they will automatically be re-invited for screening following the period of time that they have chosen to postpone their appointment for.
Individuals can postpone their appointments for a specific amount of time and then repeat with another postponement if requested.
If an individual postpones their appointment they will still be classed as active within the screening programme and the associated performance reports.
Consent withheld for demographic transfer
If a person with diabetes wants to permanently opt-out of the DES programme, they can withhold or withdraw their consent for data sharing between their GP and local DES service. In such cases, an individual would no longer be invited for screening and would not receive any communication from the local service.
The individual must request that their data is not shared with the DES service and their GP must record this on the individual’s record.
If this happens at the time of diabetes diagnosis, the individual would remain unknown to the DES service. If the DES service already has a record of this person then they would change the individual’s status to off-register ‘refused demographic transfer, but known to programme’.
It is the responsibility of the GP to make sure that individuals with diabetes who want to permanently opt-out of the DES programme and refuse transfer of their personal information are aware of the risk to their eyesight and are offered the opportunity to change this decision and be referred back into the DES programme if they want to.
4.2 Medically unfit
Medically unfit covers the following categories of people:
Terminally ill
Terminally ill is defined within NDESP as a person with diabetes who is suffering from a progressive disease, and where their death can be reasonably expected within 6 months.
The least restrictive option is for the person to remain in call or recall and receive screening invitations. The invitations can be considered and accepted or declined on each occasion. Alternatively, the GP or other caring physician can discuss whether or not the person wishes to continue to attend screening and the patient can, if they wish, make an informed decision to opt out.
In some circumstances, where the GP or care team believe that receiving invitations or completing an informed opt-out will cause distress to the person or their carer they can decide that it is in the person’s best interest to exclude them as medically unfit in order to stop invitations being sent, further detail is available below.
Pre-existing conditions
People who will never be able to benefit from and/or receive treatment due to a pre-existing condition should be assessed by either their GP or the clinical lead. If their clinician confirms that this is the case, the person can be excluded under ‘medically unfit’ category.
Digital photography inappropriate
People who will never be able to have a digital image taken or graded in both eyes due to a pre-existing condition that cannot be treated, should be assessed by the clinical lead, or an ophthalmologist nominated by the clinical lead.
If the clinical lead, in discussion with the individual (and if relevant, their carer), considers they could benefit from regular review using SLB and could benefit from treatment for DR if required, then the individual should be referred to the SLB surveillance clinic. These individuals should be suspended from the screening programme and monitored through the failsafe system.
If the clinical lead, in discussion with the individual (and if relevant their carer), considers they would not benefit from regular review using SLB or could not benefit from treatment if required, then the clinical lead can exclude the individual from the screening programme as medically unfit.
5. Situations that require special consideration
5.1 People with ungradable images
Separate guidance regarding management of people with ungradable images is available.
5.2 People who have a disability
In most cases a person with a disability should be able to access their local screening programme. Local programmes should ensure they provide a service that is accessible to them in accordance with appropriate disability discrimination legislation.
In a small number of cases a person may have a disability that prevents them from being screened by digital photography. In these circumstances the clinical lead should discuss their situation and options with them (and if appropriate with their carer and GP) on an individual basis.
It is not appropriate for either the GP or screening programme staff to exclude a person with a disability from screening when they have capacity to make their own decisions.
5.3 Excluding a person in their best interests
A person who lacks the mental capacity to consent to screening should not be excluded or removed from a screening recall programme unless a ‘best interest decision’ to do so has been taken on their behalf. In most cases, the least restrictive option is for that person to remain in call or recall and receive screening invitations at routine intervals. The invitations can be considered and accepted or declined on each occasion.
Screening programmes will need to ensure there is evidence that any best interest decision has adhered to the principles of the Mental Capacity Act and that all relevant factors, reasonable adjustments and alternatives have been considered.
In exceptional circumstances, a care team may decide it is in the best interests of a person who lacks mental capacity to withdraw from a screening programme. Screening staff should be satisfied that the best interest decision has been reached in accordance with their local code of practice. The person making the best interest decision to exclude a person from screening should be aware that the person can be re-invited at any time if circumstances change and screening is then considered to be in the person’s best interests.
5.4 Housebound patients
DES and laser photocoagulation treatment require special equipment which is not portable and cannot be provided in people’s homes.
People in institutional or residential care or who are housebound and able to benefit from screening and treatment should continue to be invited for screening. There should be provision for a service that is accessible to them in accordance with disability discrimination legislation.
Local programmes should ensure housebound people have reasonable access to screening. The GP and, if appropriate, care home staff will have a role in making sure patients are encouraged to attend for screening and subsequent treatment if necessary.
People who are unable to travel outside their home or who have a disability that would preclude treatment should be assessed in line with the medically unfit process as outlined within this document. Domiciliary assessment or home visits are not part of the screening service and if provided should be commissioned, funded and managed separately from NDESP.
5.5 Referable incidental findings
The management of incidental findings (non-diabetic retinopathy) is not within the scope of the screening programme. Incidental findings that may require a referral are the responsibility of the general practitioner (GP). The referral of these cases from the screening provider may be managed or commissioned according to an agreed local protocol.
People who are referred and followed for an incidental finding will continue to require routine digital screening.
People referred for non-DR eye conditions must remain on the active register ie not suspended from the programme. However, while these patients are in the care of HES, routine diabetic retinopathy screening can be carried out in one of 2 ways:
- Individuals will continue to be recalled to the DESP for regular DES, and the incidental finding referral made to HES will have no impact on their participation in screening.
- Individuals who are referred to HES for a condition other than DR can be screened within the HES for DR by a medical retinal specialist. This must include an RxMx grade.
5.6 Private patients
Patients who attend private ophthalmologists should not be excluded from invitations to the screening programme. They can be excluded if they wish by completing and returning a completed opt out form.
5.7 Postponement
A postponement is an extension added to a person’s next due appointment date, made as a manual change by DESP administrative staff at the request of the patient or the patient’s GP. In all cases, the patient will remain eligible for screening and will not be counted as suspended or excluded.
Postponement should be used only when a patient is unable to attend for screening for limited time (up to a maximum of 12 months), for example due to holiday, scheduled surgery or limited illness.
This category should be failsafed and audited to ensure this category is being used appropriately.
5.8 People in institutional organisations
All eligible people in prison, other places of prescribed detention and secure institutions should have access to DES. Local programmes should have policy that describes how they access these institutions for screening and the appropriate pathways of care for these people.
6. Rarer forms of diabetes
There are a number of rarer forms of diabetes that carry differing risks of developing diabetic retinopathy. NDESP is not intended to provide highly specialised care for very small groups of people. Therefore, it is suggested that all patient with rarer forms of diabetes are invited for routine screening, irrespective of the type of diabetes they have. People may opt-out of screening once they have made an informed decision as detailed above.
6.1 Maturity onset diabetes of the young (MODY)
When a person is diagnosed with MODY they should be referred to the DESP and be invited for routine digital screening irrespective of the type of MODY they have.
6.2 Steroid induced diabetes
When a person is diagnosed with diabetes due to steroid treatment they should be referred to the DESP and receive routine digital screening.
They should continue to have routine digital screening until the discontinuation of steroid treatment or referral to hospital eye services or digital surveillance.
Following discontinuation of steroid treatment:
- if the individual shows continued signs of diabetes they will need ongoing routine digital screening
- if there are no clinical signs or symptoms of diabetes following discontinuation of steroids they do not need screening or ongoing screening, they should be categorised as ‘not having diabetes’ or ’not diabetic’ and removed from the cohort
This decision should be made by the person’s medical team and the appropriate coding or category applied to them at their GP practice.
Local programmes do not have to audit or monitor this process or an individual’s category until the individual has their steroid induced diabetes code removed by their GP and are no longer on the electronic extract as part of ongoing validation.
6.3 Gestational diabetes
When a woman is diagnosed with diabetes during pregnancy the clinicians involved with the woman’s care must decide whether they diagnose this as type 2 diabetes or gestational diabetes.
If the clinicians diagnose gestational diabetes, no screening is required during pregnancy.
If the clinicians diagnose type 2 diabetes during pregnancy, the woman should be coded as having diabetes by their GP practice and will be issued an invitation to attend DES screening as outlined in the recommendations for screening during pregnancy.
7. Early worsening phenomenon
The early worsening phenomenon can occur when a person with diabetes has a sudden improvement in their diabetic control for a number of reasons which can lead to an increased risk of diabetic retinopathy. This could be:
- a diabetic patient becoming pregnant following a history of poor control and their control improves dramatically
- transition from poor control on tablet therapy to commencement of insulin therapy
- transition from poor control on insulin therapy to commencement of insulin pump treatment
- people with undiagnosed diabetes for a number of years, following diagnosis their and their blood pressure diabetic control improves quickly following diagnosis
These individuals should be entered onto the appropriate screening interval for their pathway within the screening programme; they do not require an increased frequency of screening or surveillance. Where clinically appropriate, an individual’s diabetes clinical team can discuss with the diabetic eye screening service Clinical Lead, whether the ‘Clinical Lead 24-month override option’ can be utilised.
No evidence currently exists about the effects on diabetic retinopathy when starting on hybrid closed loop (HCL) systems,
Services can utilise the ‘Clinical Lead 24-month override option’ available within the diabetic eye screening software to enable an additional 12-month screen following initiation of HCL system. This should only be used where the diabetes clinical team has notified the screening service clinical lead that an individual is at higher risk.
If the screening result is R0M0 following this additional 12-month screening appointment they will be eligible for 24-month screening once again and will be automatically assigned the most appropriate screening interval by the software.
Reference: Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Arch Ophthalmol. 1998 Jul;116(7):874-86. PubMed PMID: 9682700.
8. Diabetes in remission or diabetes resolved
All people who have had a definitive diagnosis of diabetes should be screened for diabetic retinopathy for life. This is because there is still an increased risk of sight loss even if diabetes is deemed in remission (with the exceptions outlined in this document). It is essential that the correct GP codes are attached to the records of these individuals. An incorrect code could lead to a person with a previous definitive diagnosis not having their eyes screened.
The GP code for ‘diabetes in remission’ should be used for people previously diagnosed with type 1 or type 2 diabetes who no longer meet the classification of having diabetes due to a reduction in blood sugar (HbA1c) levels. Interventions can include bariatic surgery, pancreatic transplant and significant weight loss.
‘Diabetes resolved’ codes should not be used for individuals whose diabetes is in remission or whose blood sugar levels are within normal limits due to an intervention. GPs should be encouraged to review patients who have a ‘diabetes resolved’ code to make sure that code is appropriate.
If an individual is removed from the local service cohort by an electronic extraction method such as GP2DRS, local services should check with the GP that ‘diabetes resolved’ is the correct code and has not been added in error.
9. Off-register individuals
This category includes people who:
- are deceased
- moved out of area
- refused demographic transfer but known to DESP
- are seen in another programme
- are not diabetic
- are under 12
These people will not receive an invitation for screening. Local programmes should have standard operating procedures that cover off-register patients and ensure that the appropriate checks have been undertaken. The decision or evidence should be documented within the screening software to provide assurance to the local programme that this person is in the correct status.
Programmes should be able to assure the commissioners and programme board that this category is being used appropriately.
