Cervical screening: support for people who feel anxious about attending
Updated 24 September 2025
Applies to England
This information is for women and people with a cervix who find it difficult to attend cervical screening.
You may feel understandably anxious or worried about attending, this could be for many reasons and may include:
- a mental health condition
- previous cervical screening experience(s)
- previous traumatic experience(s)
- sexual and/or domestic violence
- dysphoria
This information talks about what support is available if you are worried, feel anxious or think it may be painful when attending your cervical screening. You can use this information to help decide whether to attend and to find support to make it easier for you if you would like it.
Cervical screening
Cervical screening tests for human papillomavirus (HPV).
HPV is very common. Most people will get the virus at some point in their life. It is spread through close skin to skin contact during any type of sexual contact. There are many different types of HPV, some types can cause abnormal cell changes, but only some types can lead to cancer, these types do not cause any symptoms. In most cases, your immune system can get rid of the virus without you ever knowing you had it.
Sometimes HPV can stay in the body for many years at undetectable levels without causing any problems. This is called ‘dormant’ HPV. Dormant HPV can become active and is then found at screening. This means the HPV infection can become active again years after you have it. HPV can cause abnormal cell changes in your cervix.
Your cervix is the lowest part of your uterus (or womb), and it is found at the top of your vagina.
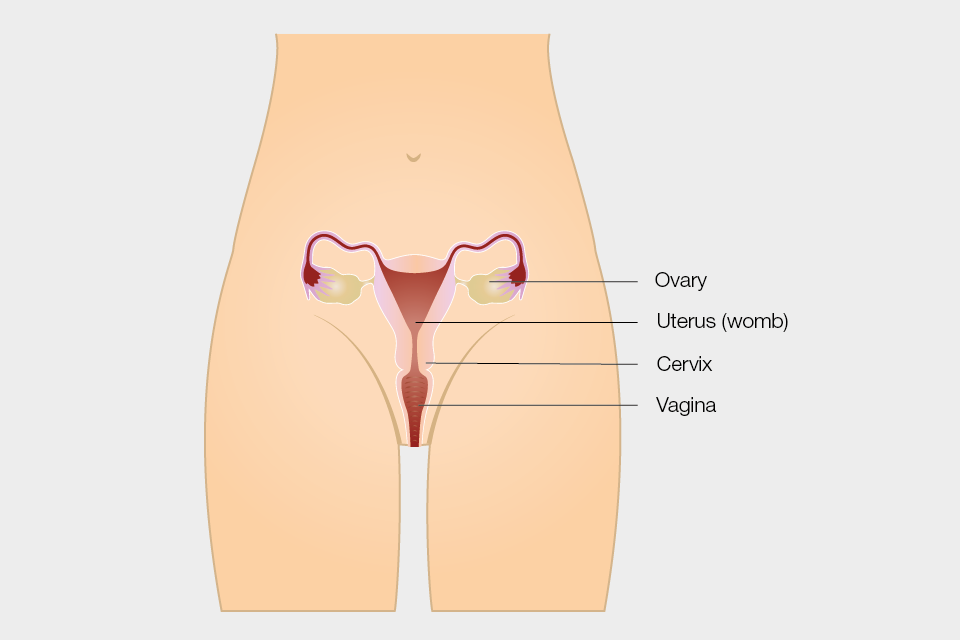
Diagram showing the location of the cervix.
Your body can usually get rid of the abnormal cells and your cervix returns to normal. But sometimes this doesn’t happen, and the abnormal cells can go on to develop into cancer. This is usually a slow process taking over 10 years.
Going for cervical screening when invited is the best way to protect yourself against cervical cancer. It is your choice whether to have a cervical screening test or not. Please read the leaflet about cervical screening available at: Cervical screening: leaflet for women considering screening - GOV.UK (www.gov.uk). This leaflet will help you decide whether to have the test and provide more information about HPV and cervical cancer.
You will get an invitation for cervical screening through the post if:
- your contact details are up to date
- you are between 25 and 64 years old
- you are registered as female on your NHS records
In some areas, you may be able to arrange your appointment at a sexual health clinic instead of your GP practice.
If you are not registered at a GP practice and would like to have screening at a GP practice, you will need to register first; more information about registering is available at: How to register with a GP surgery - NHS (www.nhs.uk)
In some areas, local sexual health clinics may also offer screening. More information about finding a sexual health clinic local to you is available at: Find a sexual health clinic - NHS (www.nhs.uk).
If you are not sure if you are due for cervical screening, you can ask your GP or health professional.
Trans men and non-binary people with a cervix are eligible for cervical screening. How you’re invited will depend on how your gender is recorded in your GP patient record.
• If you’re listed as female, you’ll receive invitations automatically.
• If not, you can “opt in” to receive routine invitations. You can do this by contacting a cervical screening provider, such as your GP, a sexual health clinic, or a transgender health clinic.
If you’re unsure, contact your GP and you can read NHS population screening: information for trans and non-binary people.
Booking your appointment
Before you book your appointment, it might help to think about what would make screening easier for you. You might already know what can help or you may want to discuss this with a nurse or health professional who can make some suggestions. Here are some tips that might help:
- If you get anxious sitting in waiting rooms, let the receptionist know. You can ask to book the first appointment of the day, so that you do not have to wait long.
- If you would prefer to be seen by a woman, ask for a female health professional.
- Tell the receptionist if you would like a chaperone. This is a usually another health professional. You might also want a friend, relative, partner or carer present.
- You may feel you need more time for your cervical screening appointment. Ask the receptionist if you can book a longer appointment to give you more time during and after.
You may also wish to consider asking for an appointment just to talk about what happens during the screening first (you do not have to have the test at this appointment).
If you find screening painful a doctor may be able to prescribe creams or medications to help you feel more relaxed.
Before your appointment
You may find it helpful to:
- plan your journey
- listen to music or watch something on your phone to help you relax, or bring something to read
- consider what to wear to your appointment; if you feel more comfortable, you can wear a skirt, dress, long top, or any clothing that helps you feel more covered. You can keep these on during your test, removing only your underwear when necessary
- speak to the health professional beforehand to discuss your concerns if you think the test may be uncomfortable as they can offer support
- ask someone you trust to go with you, such as a friend, relative or carer/mental health worker, who can also be with you after your appointment
Questions to ask the health professional
It might be helpful to think of any questions you want to ask the health professional before your appointment.
We want to make you feel at ease so you have the best possible experience - you can ask for extra support for any reason, including if you:
- have a mental health condition
- take medication that makes you shake
- find it hard to leave your house
- sometimes find it hard to process information
- do not like to feel exposed by removing your clothes
- are embarrassed by showing your body
- have scars
- feel like you might be judged
- feel like a burden
- are afraid it will hurt
- may start to cry or freeze up
- may pass out or faint
- may have a panic attack
- get distressed during a physical examination
- have had a negative cervical screening experience in the past
- have experienced trauma
- are a survivor of sexual violence
- are a survivor of female genital mutilation or cutting (FGM/C)
- want to be warned before the health professional touches you
- find that waiting rooms make your symptoms worse
- find that certain words, actions or positions trigger anxiety attacks or flashbacks
- feel a disconnection with some parts of your body
You may want to print out and fill in the extra support checklist to take with you to your screening test.
During your appointment
The cervical screening test takes a few minutes – here’s what to expect at your appointment:
The health professional will explain the test at the start of your appointment.
- You will have a private space to undress from the waist down and you will have a modesty sheet to cover you – remember you can wear a long top or dress/skirt to help you feel less exposed.
- There may be different positions that could make the test more comfortable for you, like lying on your side. Your healthcare professional will work with you to make sure you are in the most comfortable position.
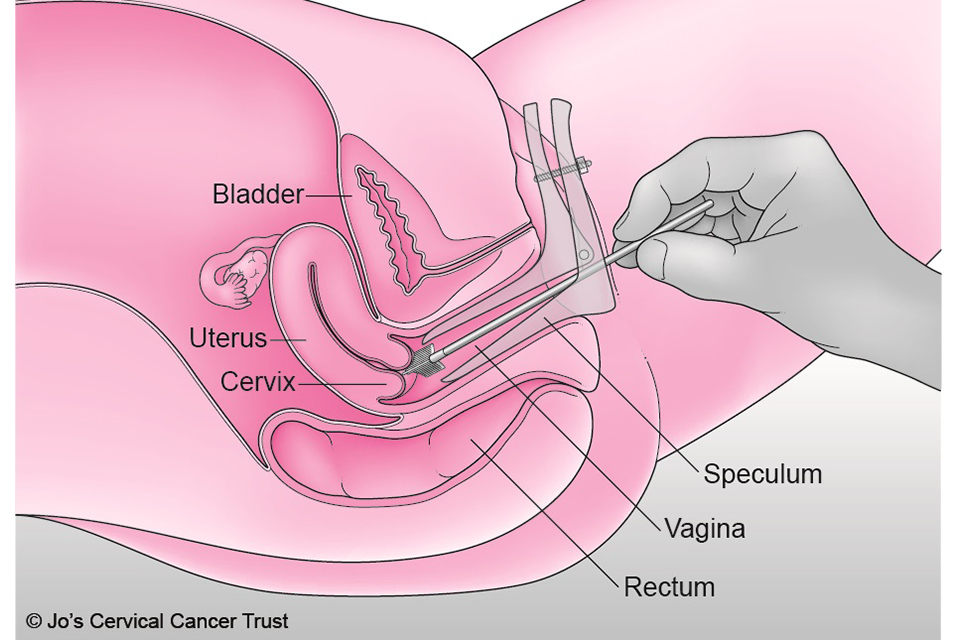
- A speculum (usually plastic) will be gently put into your vagina. It opens so the health professional can see your cervix. Speculums come in a range of sizes. Talk to your health professional to discuss the size that is most appropriate for you. You can also ask to place the speculum yourself.
- The health professional will use a small, soft brush to take a sample of cells from your cervix.
- Your test could feel uncomfortable but remember, you are in control during the test. It may help to agree a word or hand signal, so the health professional knows to stop immediately if you want them to.
After the test
The sample of cells is sent to the laboratory for testing.
We will send your screening result to you by post. The nurse or doctor who does your screening test will tell you when you can expect to get your result letter, and they will also get a copy. Please make sure you tell your GP practice or healthcare professional about any changes to your address.
You may feel anxious while waiting for your results. It may help to speak with someone you trust about how you are feeling.
Cervical screening results
HPV negative
Most people get an HPV negative result. This means no further tests are needed and you will be called back for screening when your next test is due.
HPV positive, no abnormal cells
If your sample is HPV positive, we also test it for abnormal cells. If none are found, your result will say you have HPV, but no abnormal cells. We will ask you to come for screening again sooner than usual. Your result letter will explain when.
HPV positive, abnormal cells
There are several ‘grades’ of abnormal cells as some are more serious than others. Your result letter will explain what your results mean. If you have HPV and any grade of abnormal cervical cells we will refer you for colposcopy (see information below).
Further information about having a colposcopy is available at: NHS cervical screening – having a colposcopy.
Unavailable or inadequate
Occasionally a sample may be called ‘unavailable’ or ‘inadequate’. This means that we were not able to get a result from your screening sample. This sometimes happens when there are not enough cells in the sample to get a result or due to a technical problem at the laboratory.
We will send you a letter inviting you for a repeat test in 3 months. Waiting 3 months gives your body enough time to make new cells, meaning it is less likely to happen again.
Looking after your health
You will get another invitation through the post when you are due for cervical screening again.
If you have any unusual symptoms, please tell your GP as soon as possible. These might include:
- vaginal bleeding that is unusual for you; bleeding between your periods, during or after sex, after the menopause or having heavier periods than usual
- pain during sex
- changes to vaginal discharge
- pain in your lower back, between your hip bones (pelvis), or in your lower tummy (abdomen)
These symptoms are often caused by other things, but it is important to get them checked. In rare cases cervical cancer can develop in between screening tests. But if you are found to have cancer, getting it diagnosed and treated early can mean you are more likely to survive.
Screening is not a test for investigating symptoms. If you have any of these changes, don’t wait for your next cervical screening appointment. See your GP as soon as possible. Your GP can examine you and refer you to a gynaecology clinic if necessary.
Getting support
If you need support, you:
- can talk to a trusted friend, relative or health professional
- may find it helpful to seek spiritual support from a religious or spiritual leader
- may want to talk to someone at an available charity
CliniQ
CliniQ has a skilled team of advice workers, offering mentoring, peer support and advice around a range of issues. Their team consists of trans mentors and advisers from a variety of backgrounds, who can support you online or in-person on either a one-off or regular basis.
Email: mentoring@cliniq.org.uk
Eve Appeal
Through their Ask Eve nurse service, the Eve Appeal answers people’s questions about their gynae health, gynae cancers and provide vital reassurance. This free, confidential and expert support is available over the phone, via email, and through their website.
To contact Ask Eve, call them on 0808 802 0019 – free to call from landlines and mobile phones – or email nurse@eveappeal.org.uk, or you can fill in our contact form and they will get back to you.
The Havens
The Havens are specialist centres in London for people who have been raped or sexually abused. Telephone 020 3299 6900 for urgent advice or an appointment.
LGBT Foundation
The LGBT Foundation is a national charity with LGBTQ+ health and wellbeing at the heart of everything they do.
Helpline: 0345 3 30 30 30
Lines are open between 9am and 9pm on a weekday and between 10am and 6pm on Saturday and Sunday (excluding bank holidays and religious festivals).
My Body Back (London and Glasgow)
My Body Back offers support to people to reclaim control of their body after sexual violence. It runs specialist clinics offering cervical screening and sexually transmitted infection (STI) testing in London and Glasgow for women, transgender and non-binary people who have experienced sexual violence.
Email: info@mybodybackproject.com
OUTPatients
OUTPatients is the UK’s only LGBTIQ+ cancer charity. It is proudly led by and for LGBTIQ+ people affected by cancer, and work hard to support and advocate for its community.
To contact OUTPatients please fill out their online form.
Samaritans
Samaritans is available round the clock, every single day of the year. You can talk to them any time you like, in your own way, about whatever’s getting to you.
Call free, any time: 116 123
Email: jo@samaritans.org
SANE
SANE is a national mental health helpline offering specialist emotional support to anyone affected by mental illness.
SANEline: 0300 304 7000 (every day, 4.30 to 10pm).
Support for victims of sexual violence and abuse
Advice and support for those who are experiencing or feel at risk of sexual violence and abuse is available at: Support for victims of sexual violence and abuse - GOV.UK (www.gov.uk)
Trans clinics offering cervical screening
Some sexual health clinics offer specialist trans and non-binary services which includes the option to attend for cervical screening.
National FGM Support Clinics
National FGM Support Clinics (NFGMSCs) are community-based clinics that offer a range of support services for women with female genital mutilation (FGM)
More information and clinic locations can be found at: National FGM Support Clinics - NHS - NHS (www.nhs.uk)
Acknowledgement
This information is adapted from a leaflet developed by Dr Frederique Lamontagne-Godwin, which was based on research with users of mental health services and was supported by:
- Jo’s Cervical Cancer Trust
- NHS Dorset Healthcare University Foundation Trust
- Public Health England
- University of Surrey
- University of West London
- West London NHS Trust
We are grateful to all the patients, service user groups, professionals and frontline staff who helped in the making of that leaflet, and in adapting it for this current version.
