Your guide to NHS cervical screening
Updated 12 November 2025
Applies to England
You can choose if you take part in cervical screening. This leaflet aims to help you decide. Cervical screening used to be called a ‘smear test’.
Why the NHS offers cervical screening
We offer cervical screening to check the health of your cervix and help prevent cervical cancer. We look for high-risk human papillomavirus (HPV). This is because it can cause abnormal changes that may lead to cervical cancer.
Finding and treating any changes early can prevent most cases of cervical cancer. Cervical cancer mostly affects women and people who have a cervix under the age of 45, but abnormal changes can happen at any age.
Cervical screening saves thousands of lives each year in the UK.
Regular cervical screening is important. You’re still at risk of cervical cancer even if you:
- have had the HPV vaccine
- have only had 1 sexual partner
- haven’t had penetrative sex
- have had the same partner, or have not had sex, for a long time
- are a lesbian or bisexual
- are a trans man or a non-binary person with a cervix
- have had a subtotal (partial) hysterectomy that did not remove your cervix
If you’ve had a total hysterectomy, you do not have a womb or cervix. This means you do not need cervical screening.
Cervical screening is not a check for other cancers of the reproductive system, such as ovary, womb, vulval or vaginal cancer. Do not wait to contact a GP if you have any concerns.
Who we invite for cervical screening
We routinely invite women aged 25 to 64 every 5 years. Most cervical cancers develop between these ages.
Your GP surgery gives us your contact information. Please make sure they have the correct details, including your:
- name
- date of birth
- address
- mobile number
- email address
Your invitation will give you information about booking cervical screening. You can book as soon as you’re invited.
Trans men and non-binary people with a cervix are also eligible for cervical screening. How you’re invited will depend on how your gender is recorded in your GP patient record:
- If you’re listed as female, you’ll receive invitations automatically.
- If not, you can “opt in” to receive routine invitations. You can do this by contacting a cervical screening provider, such as your GP, a sexual health clinic or a transgender health clinic.
If you’re unsure, contact your GP. Find more information on screening for transgender and non-binary people.
Cervical cancer and HPV
Cervical cancer is a cancer found anywhere in the cervix.
The cervix is the opening to your womb from your vagina. It’s part of the reproductive system and is sometimes called the neck of the womb.
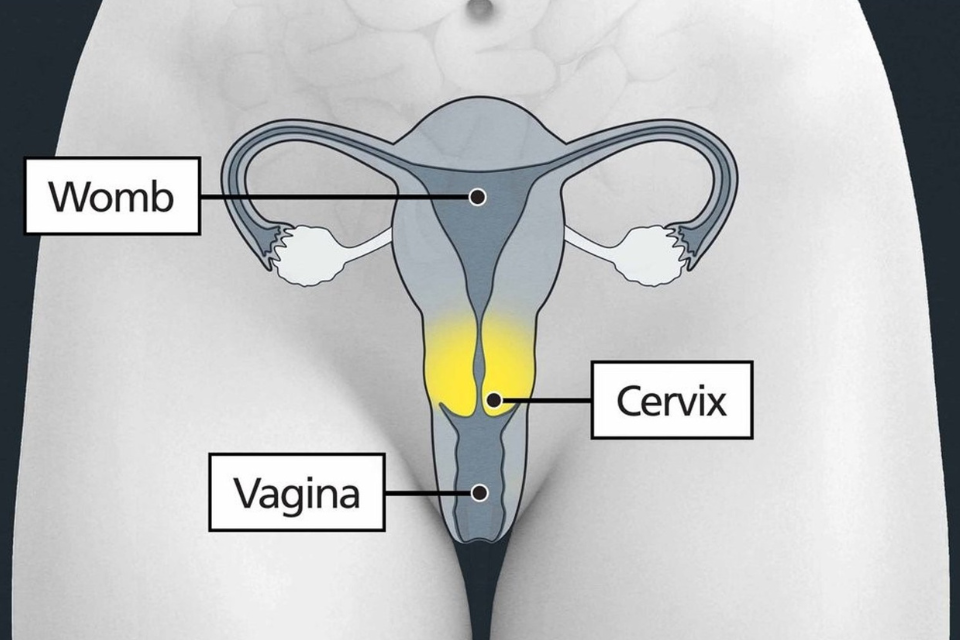
Diagram showing the position of the cervix
Nearly all cervical cancers are caused by an infection with certain high-risk types of human papillomavirus (HPV).
HPV is the name for a very common group of viruses. Most HPV viruses are low-risk and do not cause any problems.
HPV viruses spread easily. You can get HPV from any kind of sexual contact, including:
- any skin-to-skin contact of the genital area
- vaginal, anal or oral sex
- sharing sex toys
You can catch HPV even if you have not had penetrative sex. Most people get some type of HPV during their lives. It’s nothing to feel ashamed or embarrassed about.
You can have HPV for many years even if you have not been sexually active or had a new partner. HPV does not always cause symptoms, so you may not know if you have it.
Your body will usually get rid of HPV, but if high-risk HPV stays in your body, it can cause changes to the cells in your cervix. These changes may become cervical cancer if untreated.
If you do not have a high-risk type of HPV, it’s very unlikely you’ll get cervical cancer. This includes if you’ve had abnormal cell changes in your cervix before.
How cervical screening works
Cervical screening is usually done by a female nurse or doctor. You can ask for this when you make your appointment, and your GP surgery or sexual health clinic will make sure a female healthcare professional is available.
They’ll take a sample of cells from your cervix with a soft brush for testing at a lab. After this, most people will not need any further tests.
If we find high-risk HPV in your sample, we also check for any abnormal changes in the cells. This helps to make cervical screening results more accurate.
If we find changes, you may need a different test called a colposcopy to look at your cervix more closely. We’ll offer you an appointment to discuss this if you need it.
At your appointment
The nurse or doctor will explain to you what to expect at each step of your screening:
- You will have privacy to get undressed from the waist down. You may want to wear something you can leave on, like a long jumper, dress or skirt.
- You will be given a paper sheet or towel to put over your waist area during your screening.
- You’ll usually lie back with your legs bent, feet together and knees apart. You can ask to be in a different position, such as on your side. Sometimes, you may need to change position during the test.
- The nurse or doctor will gently put a smooth, tube-shaped tool called a speculum into your vagina. They may use a small amount of lubricant to help reduce any discomfort. You can ask for a smaller speculum. You can also ask to insert the speculum yourself at first.
- They’ll open the speculum to see your cervix. Using a soft brush, they’ll take a small sample of cells from your cervix. You may feel some discomfort. You can try breathing exercises to help you relax.
- They’ll close and remove the speculum and leave you to get dressed. They can give you tissues to wipe away any lubricant.
The cervical screening test itself should take less than 5 minutes. The whole appointment should take about 10 minutes.
The nurse or doctor will be trained to support you. You can also bring someone with you, such as a friend, relative, partner or support worker. They can be in the room with you during your appointment.
If you need to empty your bladder before your screening, let the nurse or doctor know. You can ask for adjustments to help you feel more comfortable and you should say if you feel any pain.
You can watch a video of a cervical screening on NHS.UK. It shows an illustrated view of inside the body, and explains what happens during the test.
Practical hints and support
You may need support to attend your cervical screening. When you book, tell your GP surgery or sexual health clinic if you need any reasonable adjustments, such as:
- a longer or double appointment
- information in other languages or formats or an interpreter
- a chaperone in the room with you (another trained member of staff)
- an appointment with a trusted doctor or nurse who you already have a good relationship with
You should:
- book your screening for when you’re not having a period – this includes the 2 days before or after you bleed
- wait until after any treatment for unusual vaginal discharge or a pelvic infection
- let them know if you are or could be pregnant, as you may need to delay your screening
Most people should avoid vaginal medicines, lubricants and creams for 2 days before cervical screening. However, if you think your appointment may be more difficult because of vaginal dryness, they may prescribe a vaginal oestrogen cream or pessary before your screening.
Some people feel understandably anxious about cervical screening. This may be because of a mental health condition, past traumatic experiences, sexual abuse or domestic violence. You are in control of your cervical screening and can ask to stop at any time. You can read our guidance for people who find it difficult to attend on GOV.UK.
Cervical screening results
The nurse or doctor will tell you when you can expect your results. There are 3 possible results:
- HPV negative
- HPV positive, no abnormal cells
- HPV positive and abnormal cells
Sometimes we cannot get a result from your sample. If this happens, we’ll invite you for another cervical screening in 3 months. It does not mean anything is wrong.
HPV negative
Most people (around 87 in 100) have this result.
It means we did not find high-risk HPV in your sample.
Your risk of getting cervical cancer is very low. We do not need to check your sample for abnormal cell changes in your cervix.
We’ll usually invite you for screening again in 5 years. Some people may be invited sooner depending on previous test results. Your results will confirm this.
HPV positive, no abnormal cells
Around 9 in 100 people have this result.
It means we found high-risk HPV in your sample, but there were no abnormal cell changes.
We’ll invite you for screening again in 1 year. We ask you to come sooner than usual so we can check if your body has got rid of the high-risk HPV, which happens in most cases.
If you still have high-risk HPV but no abnormal cell changes, we’ll invite you for screening again 1 year later. If you still have high-risk HPV after 2 years, we’ll invite you for a colposcopy to look at your cervix more closely.
HPV positive and abnormal cells
Around 4 in 100 people have this result.
It means we found high-risk HPV in your sample and abnormal changes to the cells of your cervix. Your results letter will explain this in more detail.
We’ll refer you for a colposcopy. It’s like cervical screening, but it’s done in hospital. A specialist nurse or doctor will look at your cervix using a magnifying lens. This is called a colposcope and it stays outside of the body. If needed, they may take a small tissue sample called a biopsy. You can read more about having a colposcopy on NHS.UK.
Most people who have a colposcopy do not have cervical cancer.
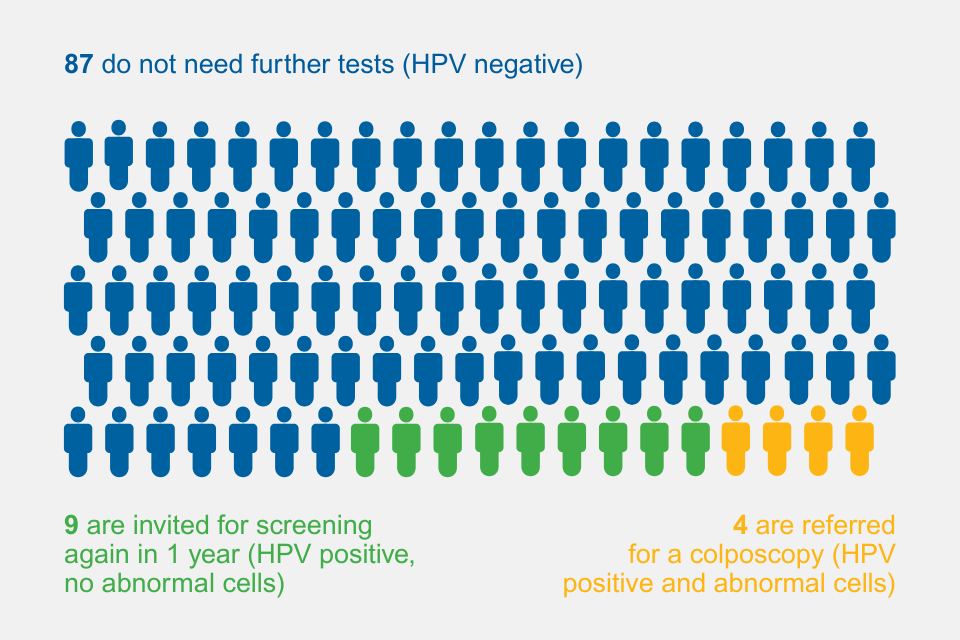
Results for every 100 people who have cervical screening
The NHS records your result on a national database. This means we can compare your regular screening results. We will keep your sample for 10 years.
Possible risks of cervical screening
No screening test is 100% reliable.
In cervical screening, this is because:
- an HPV infection or abnormal cells can sometimes be missed (a ‘false negative’ result)
- there is a small chance that a result says abnormal cells are found when the cervix is normal (a ‘false positive’ result)
- there is a small risk of abnormal cells developing and turning into cancer in between screening tests
Possible risks of having a colposcopy
Most people will not need a referral for a colposcopy and will not need to have abnormal cells removed. If you do need cells removed, there’s a small risk of bleeding and infection. You’ll get more information to help you decide if you need a colposcopy.
Cervical cancer symptoms
Symptoms of cervical cancer may include:
- vaginal bleeding that’s unusual for you
- bleeding during or after sex, between your periods or after the menopause (when your periods have stopped for 12 months or more)
- having heavier periods than usual
- changes to your vaginal discharge
- pain during sex
- pain in your lower back, between your hip bones (pelvis), or in your lower tummy
These symptoms are very common and can have many causes, but it’s important to get them checked by a GP. If cancer is the cause, finding it early means treatment is more likely to be effective.
If you have another condition, like fibroids or endometriosis, see a GP if your symptoms change, get worse or do not feel normal for you.
Who is more likely to get cervical cancer
Cervical cancer mostly affects women and people with a cervix under the age of 45, but it can happen at any age.
You may be more likely to get cervical cancer if:
- you’re under 45 – cervical cancer is more common in younger people
- you have a weakened immune system, for example if you have HIV or AIDS
- you have given birth to many children or had children at an early age (under 17 years old)
- your mother took the hormonal medicine diethylstilbestrol while pregnant with you
- you’ve had vaginal, vulval, kidney or bladder cancer in the past
- you smoke
- you’ve taken the contraceptive pill for more than 5 years – this only slightly increases your risk
You can lower your chance of getting cervical cancer by using condoms, stopping smoking and eating a balanced diet.
You cannot get cervical cancer if you’ve had surgery to remove your womb and cervix.
Cervical cancer and the HPV vaccine
The HPV vaccine helps protect against the HPV virus, which causes most cervical cancers.
It’s recommended for children aged 12 to 13 years old and people at higher risk from HPV. If you were eligible but missed getting vaccinated when you were 12 or 13, contact your GP surgery.
It’s still important to attend cervical screening appointments, even if you’ve been vaccinated against HPV. It does not protect you from all types of HPV, so there’s still a small chance you could get cervical cancer.
Cervical screening and HPV vaccination give the best protection from cervical cancer.
Clinical trials
You may be asked if you want to take part in a clinical trial. These are medical research studies. Any trial you are offered will gather information about the best types of screening tests or treatments so we can improve services in the future. You can choose whether to take part or not.
More information and support
For advice on cervical screening, you can contact your GP surgery or sexual health clinic.
This information is available in alternative formats, including other languages. It is also available in easy read.
To request another format, you can phone 0300 311 22 33 or email england.contactus@nhs.net.
You can also:
- find more information on cervical screening
- read our guidance for people who find it difficult to attend
- read information for transgender and non-binary people about NHS screening programmes
The Eve Appeal are a gynaecological cancer charity. They offer free and confidential advice on cervical screening. You can email nurse@eveappeal.org.uk or phone 0808 802 0019.
We use personal information from your NHS records to invite you for screening at the right time. NHS England also uses your information to ensure you receive high quality care and to improve the screening programmes. Read more about how we use and protect your information.
Find out how to opt out of screening.
