[Withdrawn] Management of non-visualised aortas
Updated 1 October 2024
1. Non-visualised aortas
The main aim of the NHS Abdominal Aortic Aneurysm (AAA) Screening Programme is to reduce aneurysm-related mortality through the early detection, appropriate monitoring and treatment of aortic aneurysms. Screening services invite men for an abdominal ultrasound scan during the year they turn 65. The screening scans are performed by qualified screening technicians who follow a standard scanning protocol. This requires measurement of the aorta in transverse and longitudinal plane.
In some situations, the screening technicians may not be able to clearly visualise the aorta, for instance when scanning men with a high body mass index. In these circumstances, the man will be invited to return for a repeat scan at the clinic or to the medical imaging unit at the hospital/vascular laboratory associated with the local screening programme.
If the result of a second scan at a screening clinic is also non-visualised then the man must be referred to the imaging unit/vascular laboratory. They should then notify the screening office of the outcome. It is the screening provider’s responsibility to send the screening result to the GP and action in line with standard operating procedures. If the aorta still cannot be visualised by the imaging unit/vascular laboratory then the individual case must be discussed with the local programme director.
Following receipt of positive screening results, local providers should book future screening appointments for surveillance men within routine clinics unless otherwise advised.
Local providers are expected to fund any imaging required following non-visualised results from their local screening provider budget.
It is expected that imaging units/vascular laboratories have clear governance and oversight arrangements in place between screening providers and vascular units together with defined patient pathways.
Reasons for non-visualisation include:
- high body mass index, resulting in the screening technician being unable to identify all, or large segments of, the abdominal aorta
- excessive bowel gas resulting in two or more failed examinations
- ambiguity regarding caliper placement and aortic diameter measurement
- unusual anatomy or pathology or previous abdominal wall surgery
The local AAA screening provider should indicate the reason for requesting the confirmation scan on the man’s referral form.
2. Test procedure and reporting
The man should be scanned, in accordance with protocols of the local imaging unit or vascular laboratory for imaging of the abdominal aorta. In line with screening guidelines, you should check and clearly record:
- individual’s identification
- NHS number
You should measure and document:
- the maximum transverse (internal wall to internal wall) anterior-posterior (A/P) diameter of the aorta
- the maximum longitudinal (internal wall to internal wall) A/P diameter of the aorta
These measurements should be clearly documented in the scan report as they need to be entered onto the national AAA database, SMaRT.
Images should:
- include the lumbar spine as a landmark
- be annotated to demonstrate the scan orientation, for example, ‘TS’ or ‘transverse’
Generic log-ins are not permitted since identification of the person performing the scan must be recorded on SMaRT.
Imaging reports should be sent to the local screening office ensuring the name of clinician performing the scan is recorded.
If the abdominal aorta is found to measure 5.5cm or more in diameter, the report should be sent urgently, within one working day, to the local screening provider office. Local multi-disciplinary team arrangements may apply with routes for urgent referral to vascular surgery.
The imaging unit/vascular laboratory should follow their local protocol for dealing with any incidental findings. Again, a copy of the report should be sent to the local screening provider for reference, ensuring the name of clinician performing the scan is recorded.
It is essential that the local screening provider should be informed if a man does not attend his imaging unit/vascular laboratory appointment.
3. Technical problems and non-visualisation of the abdominal aorta
Both the transverse and longitudinal measurements of the aorta are required in order for the screening test to be classed as successful. Occasionally it is impossible to obtain an adequate image of the aorta that enables the diameter to be measured in either, or both, of these planes. The reason for non-visualisation should be stated in the report and sent to the local AAA screening provider.
There will also be cases when a section of the aorta cannot be visualised. The national screening programme has issued guidance to local screening providers and the same advice should be followed by imaging departments. The guidance is summarised as follows.
3.1 Guidance for non-visualisation of the suprarenal aorta
Approximately 95% of all abdominal aortic aneurysms are found in the infrarenal aorta; isolated dilated segments of the suprarenal aorta are rarely encountered during routine scanning. However, wherever possible the suprarenal aorta should be imaged in addition to the infrarenal aorta (figure1).
If the suprarenal section cannot be fully visualised but the rest of the aorta is clearly seen, then this is acceptable and the aortic diameter can be recorded (figure 2).
The suprarenal section is the part of the abdominal aorta above the renal arteries. These are not normally visible and the superior mesenteric artery (SMA) can be used as an alternative landmark. Colour flow imaging, to aid the location of the renal arteries or SMA, can only be used by medical imaging departments.
If the SMA is also not visible, the suprarenal section approximates to the first 3cm of the abdominal aorta just below the xiphisternum or diaphragm.
If any part of the infrarenal aorta cannot be visualised (figure 3) then it should be recorded as a non-visualised scan and the appropriate pathway followed.
The following diagrams are for illustrative purposes:
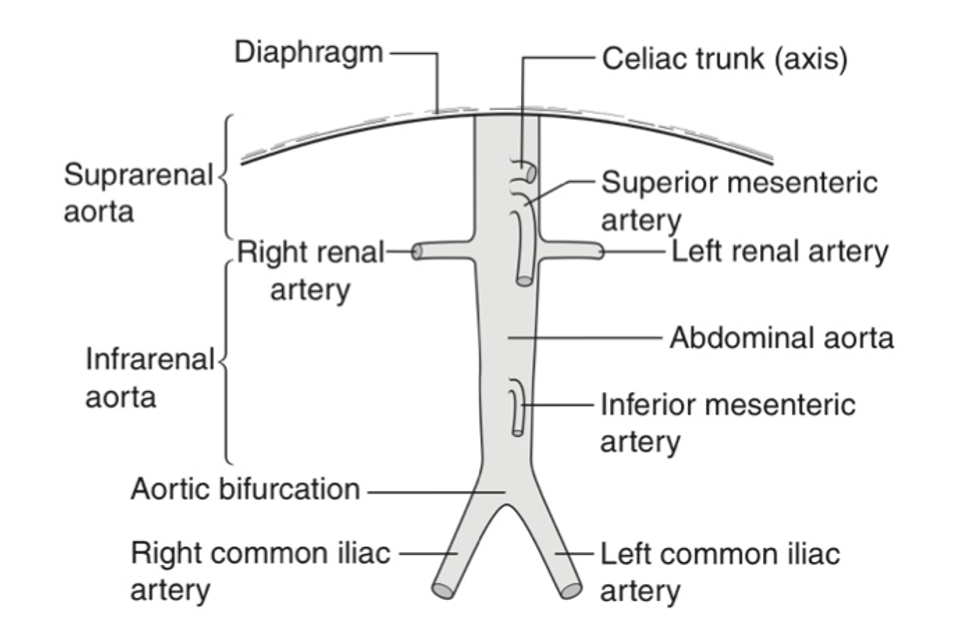
Figure 1. Anatomy of the abdominal aorta
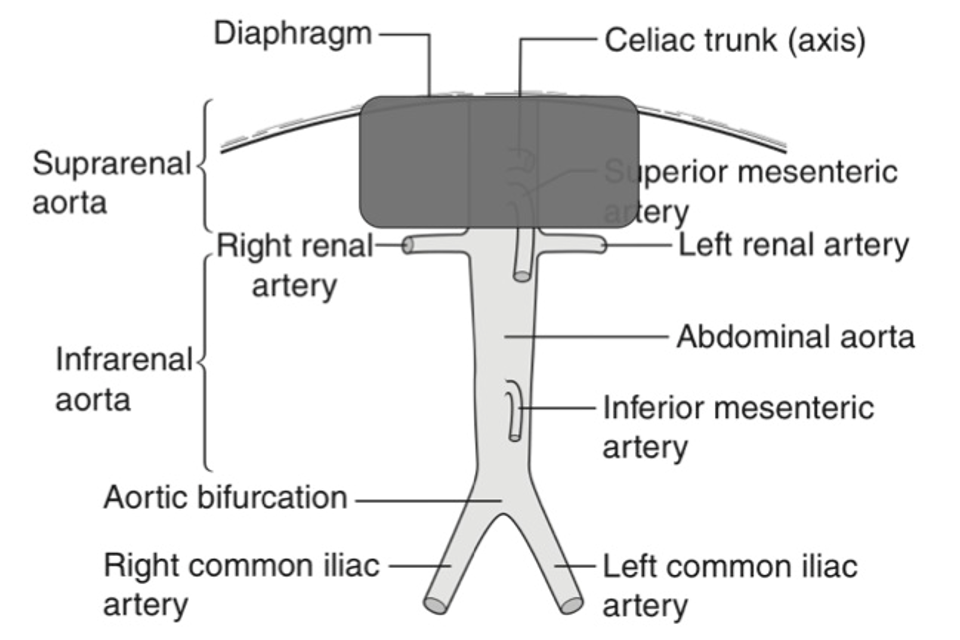
Figure 2. Non-visualisation of supra-renal aorta
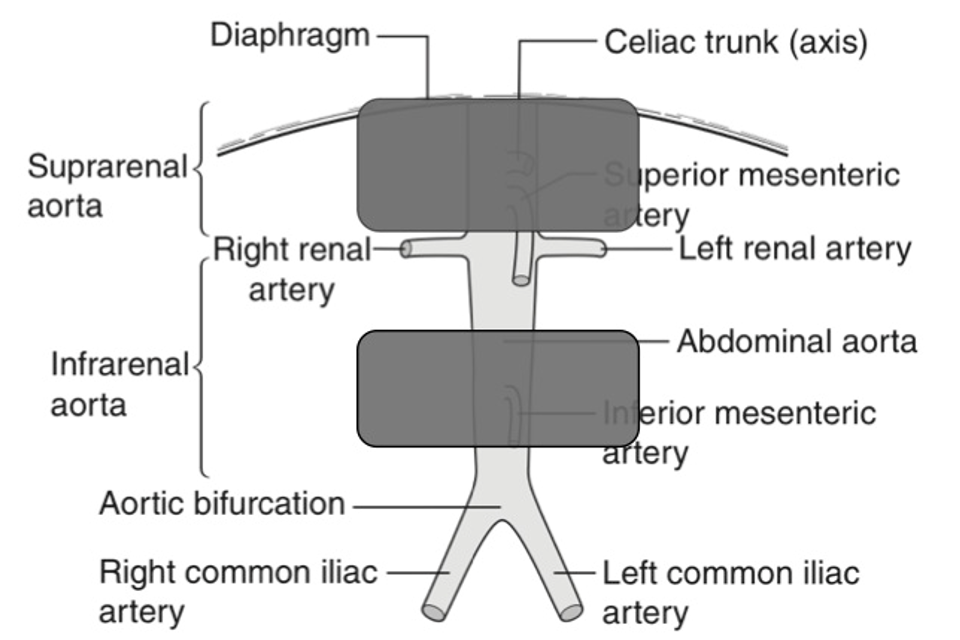
Figure 3. Non-visualisation of the supra and infrarenal abdominal aorta
To ensure that a consistent policy is applied across local screening providers, screening technicians should also discuss the issue of non-visualisation with their local clinical skills trainer and quality assurance lead.
4. Governance and oversight arrangements with local screening providers
In most cases, the clinical skills trainer and quality assurance lead for the local screening provider will be a member of the imaging unit or vascular laboratory providing the additional imaging. Regular, direct contact between screening providers and imaging units/vascular laboratories is essential. As part of this process, formal arrangements should include:
- attendance of an imaging unit or vascular laboratory representative at local AAA screening provider team meetings
- audit of images and reports
- discussion and feedback regarding interesting cases or imaging problems
5. External quality assurance review
Imaging units and vascular laboratories should be aware that local screening providers are subject to external quality assurance (QA) reviews and should, therefore, work with the local screening provider to ensure that relevant information and documentation is available regarding the process for additional imaging. Regular meetings should be organised between the local screening provider and the imaging unit or vascular laboratory to discuss such arrangements and any potential problems with internal or external QA processes.
