Work exposures to HIV, hepatitis B, and hepatitis C still rising
New PHE report warns of healthcare workers’ continued risk of exposure to bloodborne viruses through occupational sharps injuries.
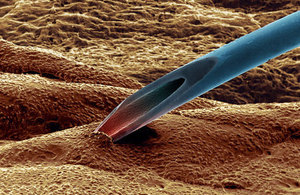
SPL injection
A new report launched today (11 December 2014) by Public Health England (PHE) warns that healthcare workers continue to be at risk of exposure to bloodborne viruses through occupational sharps injuries, despite the fact that safety-engineered devices to prevent these injuries are now available.
Occupational exposures to a bloodborne virus (BBV) that were reported to PHE increased among healthcare workers from 373 in 2004 to 496 in 2013. Over this 10-year period, approximately 30% of exposures involved a source patient infected with HIV; 54% involved hepatitis C (HCV), and 9%, hepatitis B (HBV). Of these exposures 81% were sustained by doctors, nurses and healthcare assistants and 65% occurred during clinical procedures. Seventy-eight percent of exposures involved a percutaneous needlestick injury, the majority of which were sharps injuries involving a hollow-bore needle.
The report, presented at the 5th Prevention of Occupational Infections, Treatment and Reporting Strategies (POINTERS) Conference in Cardiff City Hall, comes after the EU Sharps Directive in 2010 and the UK Sharps Regulations in 2013, which state that safe working conditions must be created for healthcare workers to help reduce the risk of sharps injury. ‘Safe working conditions’ can range from working hours that reduce tiredness among healthcare workers, to the provision of safety devices to reduce the risk of a needlestick injury before, during or after use, and appropriate training to staff performing clinical procedures.
Between 2004 and 2013, 9 healthcare workers were infected with HCV following occupational exposure in England, Wales and Northern Ireland. Eight of the nine healthcare workers received antiviral therapy, of whom 7 are known to have achieved viral clearance.
The report also finds that HBV immunisation programmes across England, Wales and Northern Ireland are effectively protecting healthcare workers from HBV infection, with no new cases reported. Furthermore, 97% of healthcare workers exposed to HIV who commenced post-exposure prophylaxis (PEP) did so within 72 hours of exposure, and no HIV infections to healthcare workers have been reported.
Dr Fortune Ncube, Head of the BBV Department at PHE said:
It is a disappointment that we still continue to see injuries to healthcare workers occurring after the procedure, in the period prior to and during disposal. These injuries are entirely preventable.
Despite this, we are encouraged that there have been no new HIV infections in healthcare workers and that the immunisation programme for HBV is effective in preventing HBV infections in healthcare workers. We want to remind all healthcare employers to comply with the regulations regarding safer working conditions and to provide safety devices to healthcare workers in an effort to reduce sharps injuries and protect them from infection.
Jill Holmes, Infection Prevention Control Nurse Specialist and Infection Control Society representative on the Safer Needles Network said:
Safety-engineered devices are not fool proof. Unless they are used correctly, these devices will not be effective or prevent sharps injuries. It is vital that healthcare providers train new and existing staff in their correct use.
It is also essential for all staff to remember the importance of basic sharps safety, such as never, ever re-sheathing a used needle, always taking the sharps bin to the point of use, and never filling above the fill line. Safe use and handling of sharps must be embedded into everyday practice.
Notes to Editors
The eye of the needle is a report on healthcare workers’ exposures to bloodborne viruses such as hepatitis B, hepatitis C and HIV while at work. Read the full 2014 report.
Additional key findings from data submitted to the significant occupational exposures surveillance system between 2004 and 2013 indicate that:
- 4830 significant occupational exposures to a BBV were reported among healthcare workers; the annual number of exposures increased from 373 in 2004 to 496 in 2013
- of healthcare workers reporting a significant occupational exposure, 1 in 2 was exposed to HCV, 1 in 3 to HIV, and 1 in 10 to HBV
- seven in ten (71%, 3396/4766) exposures involved a percutaneous needlestick injury, the majority of which were sharps injuries involving a hollowbore needle; the annual number of percutaneous injuries increased by 22% over the 10-year period from 283 to 344, whereas mucocutaneous exposures increased by 61%, from 90 to 145
- two-thirds (65%, 2490/3816) of exposures occurred in wards, operating theatres and Accident and Emergency (A&E) departments; the annual number of exposures increased over time both in operating theatres and A&E but declined in wards
- four in five (81%, 3926/4830) exposures were sustained by doctors, nurses and healthcare assistants; among all occupational groups, two-thirds (65%, 2288/3494) of exposures occurred during clinical procedures
- of healthcare workers exposed to HBV for whom immunisation status was known (data limited to the period from 2009 to 2013), 96% (300/313) were known responders to the HBV vaccine; no HBV seroconversions have been reported
- occupational exposures to HIV are well managed; 97% (580/598) of healthcare workers exposed to HIV who commenced post-exposure prophylaxis (PEP) did so within 72 hours of exposure; 89% (535) commenced PEP within 24 hours; no HIV seroconversions have been reported
- between 2004 and 2013, there have been 9 reported HCV seroconversions
More information on the 5th POINTERS conference.
Public Health England exists to protect and improve the nation’s health and wellbeing, and reduce health inequalities. It does this through advocacy, partnerships, world-class science, knowledge and intelligence, and the delivery of specialist public health services. PHE is an operationally autonomous executive agency of the Department of Health. www.gov.uk/phe Follow us on Twitter @PHE_uk.
UKHSA press office: National Infection Service
UKHSA press office, infectious diseases
61 Colindale Avenue
London
NW9 5EQ