National norovirus and rotavirus bulletin week 32: data to week 30 (31 July 2022)
Updated 10 August 2023
Applies to England
Main messages
This monthly bulletin covers the 4 week period between 4 July and 31 July 2022 (reporting weeks 27 to 30, 2022) and is the first bulletin of the 2022/2023 season. The main messages of this bulletin are:
- Norovirus laboratory reports during the first 4 weeks of the 2022/2023 season (weeks 27 to 30) were 11% higher than the 5-season average of the same period prior to the emergence of coronavirus (COVID-19), from 2014/2015 to 2018/2019.
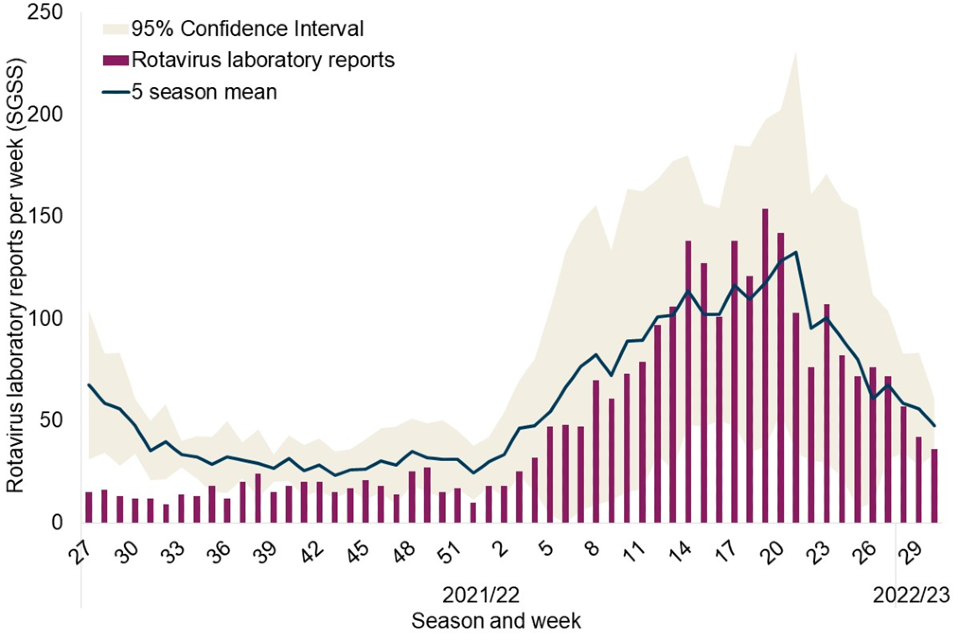
- During weeks 27 to 30, 2022, laboratory reports of rotavirus were 10% lower than the 5-season average (2014/2015 to 2018/2019) for the same 4 week period pre-COVID-19.
- Reported enteric virus (EV) outbreaks have exceeded the 5-season average of the same period pre-COVID-19 in recent weeks (27 to 30), reports were 16% higher than the 5-season average of the same period.
- So far this season, reports of outbreaks in hospital settings remain notably lower than during the same period in the 5 seasons pre-COVID-19.
- During the 2022/2023 season to date the majority (71%) of samples characterised were norovirus Genogroup 2 (GII) of which the most frequently identified strain was genotype GII.6 (21%), however due to low numbers of samples submitted for molecular surveillance in the early part of the season, these data should be interpreted with caution.
Background
The UK Health Security Agency (UKHSA) first launched this National Norovirus and Rotavirus Bulletin in December 2020 to provide an overview of activity in England and temporarily replace the suspended Official Statistics national norovirus and rotavirus report.
The coronavirus (COVID-19) pandemic impacted activity across all gastrointestinal pathogen surveillance indicators for England in 2020 and 2021, but for some pathogens including norovirus this continued in to 2022. The reasons for the reduction in norovirus reporting are considered to be multifactorial. The pandemic led to many changes which have likely had a negative impact on surveillance indicators, but which have likely also resulted in reduced norovirus and rotavirus (and other enteric virus) transmission.
Following a period of very low activity throughout the 2020/2021 season norovirus reporting began to increase from week 25 of 2021, although not returning to the seasonal trend observed pre-pandemic during the 2021/2022 season. It is likely that unusual norovirus activity will continue into the 2022/2023 season.
Reported rotavirus activity remained low throughout the 2020/2021 season and into the first half of the 2021/2022 season, but returned to expected levels in 2022, generally following the historical seasonal trend from week 13 onwards.
There was also a substantial and sustained drop in the number of EV outbreaks reported to national surveillance following the emergence of COVID-19 in March 2020, with an 83% decrease in total reported EV outbreaks across the entire 2020/2021 season compared to the pre-pandemic 5-season average (2014/2015 to 2018/2019). Prior to the emergence of COVID-19 the majority of reported EV outbreaks occurred in hospital and care home settings, however during the 2020/2021 and 2021/2022 seasons the most frequently reported setting was educational settings.
UKHSA’s Enteric Virus Unit (EVU) provides a norovirus characterisation service to support national surveillance and monitor the diversity of circulating strains. The drop in norovirus reporting during the 2019/2020 and 2020/2021 seasons lead to a period of low referral for characterisation, therefore these data are not presented. During the 2021/2022 season, 572 norovirus positive samples were characterised of which 90% were genogroup 2 (GII), 8% were genogroup one (GI) and 2% were mixed. The 3 most frequent norovirus GII genotypes identified were GII.4 (48%), GII.3 (13%) and GII.2 (10%) and the most frequently identified norovirus GI genotypes were GI.3 (3%) and GI.6 (3%). To enable effective molecular surveillance, it is crucial that samples are obtained from suspected norovirus cases or outbreaks for laboratory confirmation and then norovirus-positive samples are referred on to EVU for characterisation.
Data summary
Data reported here provide a summary of norovirus and rotavirus activity (including EV outbreaks) in England up to reporting week 30 of the 2022/2023 season.
Unusual reported norovirus activity continued throughout the 2021/2022 season (Figure 1). Norovirus laboratory reports increased during the early part of the 2021/2022 season and until week 40 of 2021 were generally comparable or higher than the same period in the 5 seasons prior to the emergence of COVID-19 (2014/2015 to 2018/2019). This was followed by a period of activity consistently lower than the 5-season average until week 20 of 2022, after which weekly reports have remained comparable to or higher than the 5-season average. Total norovirus laboratory reports in weeks 27 to 30 (228 laboratory reports) were 8% higher than the 5-season average (210 laboratory reports) for the same 4 week period.
Throughout the first half of the 2021/2022 season rotavirus laboratory reports remained lower than the 5-season average of the same period pre-COVID-19 (Figure 2). Since week 13, 2022 reports have mostly remained higher than or comparable to the 5-season average. Overall activity for the 4 week period of weeks 27 to 30, 2022 (207 laboratory reports) was 10% lower than the 5 season average (229 laboratory reports) for the same period.
Across the 2021/2022 season the number of reported EV outbreaks have varied in comparison with the 5 season average calculated from 2014/2015 to 2018/2019. However, reports were 18% lower over the entire 2021/2022 season, (Figure 3). The total number of reported EV outbreaks during weeks 27 to 30 of the 2022/2023 season (148 outbreaks) was 16% lower than the 5-season average for the same 4 week period (177 outbreaks).
During the 2021/2022 season there was a shift in reported outbreak settings. Historically the majority of outbreaks were reported in hospital and care home settings, however in the 2021/2022 season outbreaks were most frequently reported in educational settings. The 4 week period of weeks 27 to 30, 2022 the majority of reported EV outbreaks (all but one suspected or confirmed as norovirus) have occurred in care home and educational settings, 53% and 41% respectively (Figure 4).
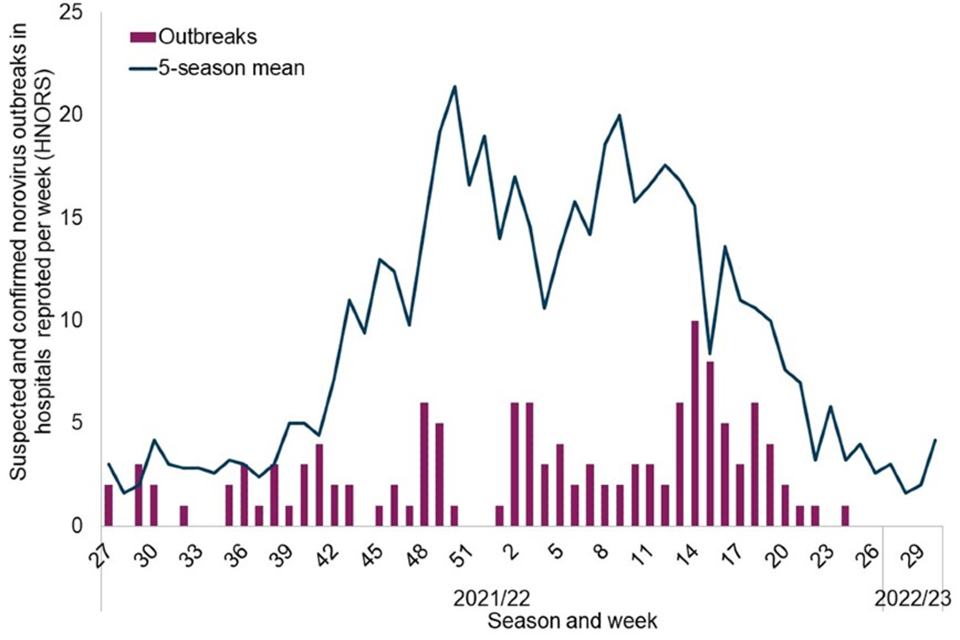
Throughout the 2021/2022 and 2022/2023 seasons to date, reports of suspected and confirmed norovirus outbreaks in hospitals have been substantially lower than the 5-season average (up to week 30 of the 2022/2023 season no outbreaks have been reported to the Hospital Norovirus Outbreak Reporting System (HNORS), (Figure 5).
Of the 24 norovirus positive samples characterised during the 2022/2023 season to date, 71% (17 out of 24) were genogroup 2 (GII) and 29% (7 out of 24) were genogroup one (GI). The 3 most frequent norovirus GII genotypes identified were GII.6 (21%), GII.3 (17%) and GII.17 (13%) and the most frequently identified norovirus GI genotypes were GI.3 (21%) and GI.2 (8%).
Laboratory data
Please see data sources and caveats section for more information and for guidance on interpretation of trends and the impact of COVID-19.
Figure 1. Norovirus laboratory reports in England by week during 2021/2022 and 2022/2023 seasons, compared to 5-season average
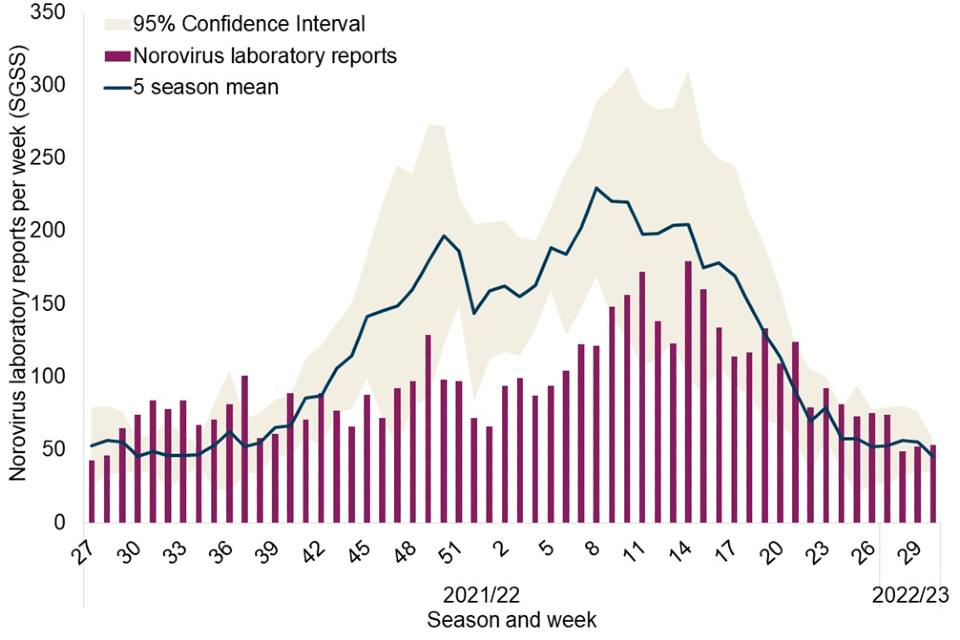
Figure 2. Rotavirus laboratory reports in England by week during 2021/2022 and 2022/2023 seasons, compared to 5-season average
Outbreak data
Please see data sources and caveats section for more information and for guidance on interpretation of trends and the impact of COVID-19.
Figure 3. Gastroenteritis outbreak reports by causative agent and week of declaration in England, 2021/2022 and 2022/2023 seasons compared to the 5-season average of total reported outbreaks
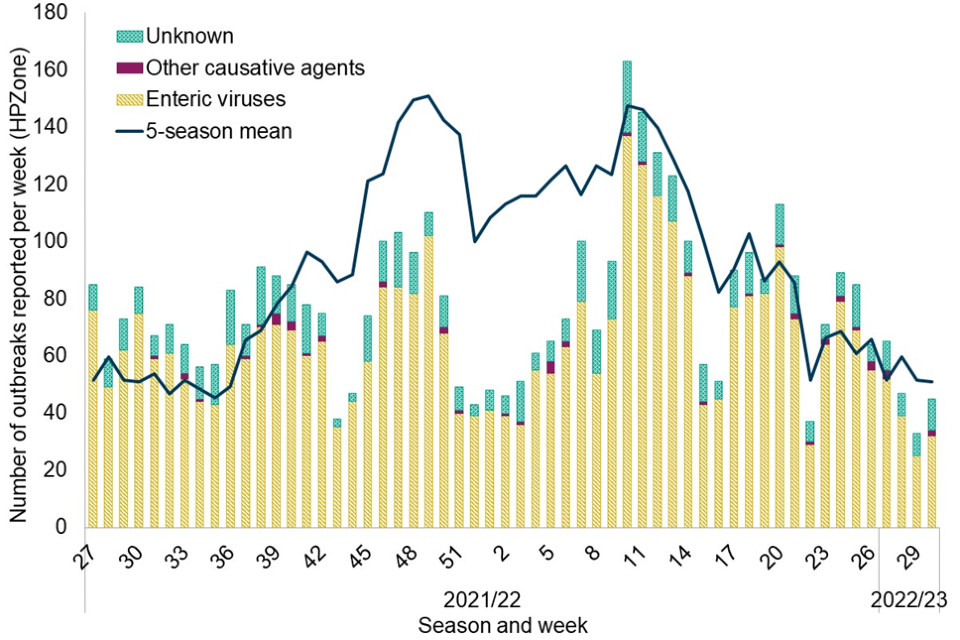
Figure 4. Enteric virus outbreaks reported to HPZone in England by setting during the 2021/2022 and 2022/2023 seasons (to week 30, 2022)
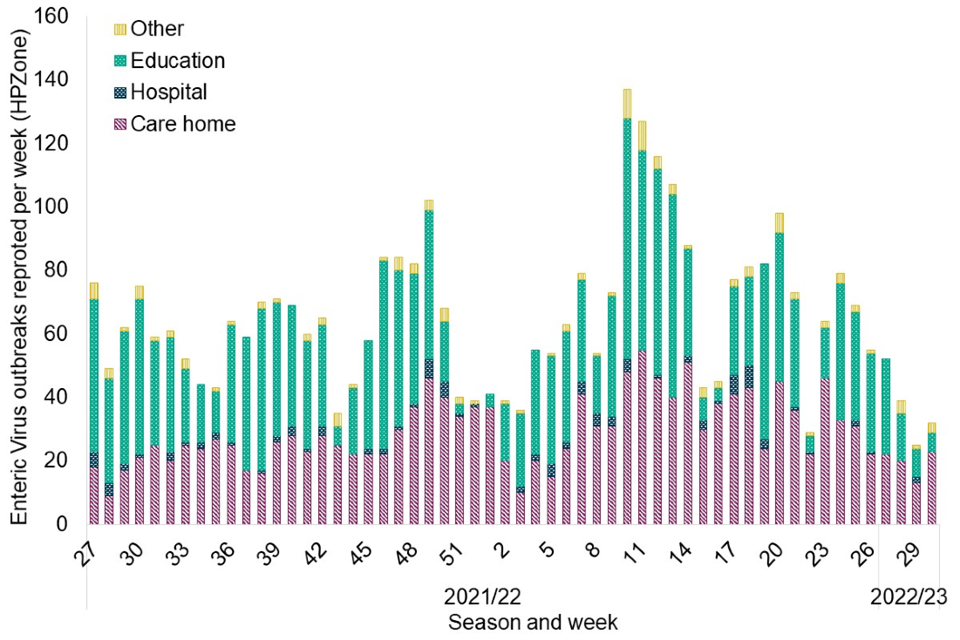
Figure 5. Suspected and confirmed norovirus outbreaks reported to HNORS in England by week of occurrence during the 2021/2022 and 2022/2023 seasons compared to the 5-season average*
Data sources, notes and caveats
Data sources
- The Second-Generation Surveillance System (SGSS) is the national laboratory reporting system, recording positive reports of norovirus and rotavirus.
- The Hospital Norovirus Outbreak Reporting System (HNORS) is a web-based scheme for reporting suspected and confirmed norovirus outbreaks in Acute NHS Trust hospitals, and captures information on the disruptive impact these outbreaks have in hospital settings.
- HPZone is a web-based case and outbreak management system used by health protection teams (HPTs) to record outbreaks they are notified of and investigate. In England, suspected and confirmed EV outbreaks (norovirus, rotavirus, astrovirus and sapovirus) are reported as ‘Gastroenteritis’ outbreaks.
- Norovirus characterisation data is produced by the Enteric Virus Unit and is used to monitor the diversity of circulating strains of norovirus in England.
Data notes and caveats
In order to capture the winter peak of activity in the reporting period the norovirus and rotavirus season runs from week 27 in year 1 to week 26 in year 2, that is, week 27 2021 to week 26 2022, July to June. The 2021/2022 and 2022/2023 seasons are compared to the 5-season average calculated from the 5-season period of 2014/2015 to 2018/2019. The 2019/2020 and 2020/2021 seasons are not included in this calculation due to the adverse impact of the emergence of COVID-19 on surveillance part way through the 2019/2020 season and the continued impact into the 2021/2022 season. In years with a week 53 (2015 and 2020) data is combined with week 52 data to avoid distortion of the figure.
Trends for the 2019/20, 2020/2021 and 2021/22 seasons should be interpreted with caution. It is likely that the interventions implemented to control COVID-19 have led to a reduction in enteric virus transmission. However, when considering the surveillance data reported here, the magnitude of the reduction is unlikely to be wholly attributable to these control measures alone. It will include other factors such as, but not limited to, changes in ascertainment, access to health care services and capacity for testing.
Under-ascertainment is a recognised challenge in enteric virus surveillance with sampling, testing and reporting criteria known to vary by region. In addition, samples for microbiological confirmation are collected in a small proportion of community outbreaks. Therefore, this report provides an overview of enteric virus activity across England and data should be interpreted with caution.
All surveillance data included in this report is extracted from live reporting systems, is subject to a reporting delay, and the number reported in the most recent weeks may rise further as more reports are received. Therefore, data pertaining to the most recent 2 weeks is not included.
For SGSS data, week number is calculated from specimen date and location is based on laboratory geography. Norovirus data include faecal and lower GI tract specimen types only. Following the introduction of the rotavirus vaccine into the routine childhood immunisation schedule in July 2013, the total number of laboratory-confirmed rotavirus infections each season has remained low compared to the pre-vaccine period.
HPZone data utilises week of date of outbreak declaration for analyses due to mandatory completion of the field. While this usually reflects the date of notification, batch reporting of outbreaks can occur.
Over the 5 seasons prior to the emergence of COVID-19 (2014/2015 to 2018/2019) an average of 86.1% of gastroenteritis outbreaks reported to HPZone were attributed to EVs (norovirus, rotavirus, sapovirus and astrovirus), 1.8% to other causative agents and 12.0% were of unknown cause. Of the outbreaks attributed to EVs, 98.4% were reported as suspected and confirmed norovirus outbreaks.
During the previous 5 seasons prior to the emergence of COVID-19 (2014/2015 to 2018/2019) 62.7% of all reported outbreaks attributed to EVs (norovirus, rotavirus, sapovirus and astrovirus), occurred in care home settings, 18.7% in educational settings, 13.0% in hospital settings and 5.6% in ‘other’ settings. Of the outbreaks attributed to EVs, 98.4% were reported as suspected and confirmed norovirus outbreaks. Only 13.7% of reported EV outbreaks were laboratory confirmed as norovirus during the previous 5 seasons.
HNORS reporting is voluntary and variations may reflect differences in ascertainment or reporting criteria by region. National guidance recommends closure of the smallest possible unit in hospitals. Therefore, not all outbreaks reported to HNORS result in whole ward closure (some closures are restricted to bays only) and not all suspected cases are tested. Week number is calculated from date of first case onset for HNORS data. During the 5 seasons prior to the emergence of COVID-19 (2014/2015 to 2018/2019) 73.6% of outbreaks reported to HNORS were laboratory confirmed as norovirus.
From May to October 2019 and during February 2020 the HNORS website was temporarily offline. The reliance on manual data collation during this period may have negatively impacted ascertainment so trends should be interpreted with caution.
Further information
Official Statistics ‘National norovirus and rotavirus reports’ can be found at Norovirus and rotavirus: summary of surveillance reports.
Further information about norovirus surveillance can be found at Norovirus: guidance, data and analysis.
Further information about rotavirus surveillance can be found at Rotavirus: guidance, data and analysis.
Acknowledgements
We are grateful to all who provided data used in this report, including NHS Infection Control and Prevention staff (HNORS users), UKHSA local (HPTs) and UKHSA regional teams (Field Services) and UKHSA Regional Public Health and Collaborating Laboratories.
This report was produced by the Gastrointestinal Infections and Food Safety (One Health) Division, UKHSA.
Please direct any queries or comments to NoroOBK@ukhsa.gov.uk
