SPI-B: Return to campus for Spring term: risk of increased transmission from student migration, 13 January 2021
Updated 13 May 2022
Since the announcement of national lockdown on 4 January 2021, DfE has updated guidance for the return of university students to campus.
If university students currently engaging in purely online learning are to return to campus in the spring, additional information is needed to encourage and support the uptake of testing and increased health-protective behaviours, and to identify the impact of student behaviours on the wider community.
If universities are to remain closed to most face-to-face teaching beyond the spring, consideration must be given to the short, medium, and long-term risks to and impacts on students.
Executive summary
- University student interaction in highly-connected environments makes students susceptible to higher rates of transmission (High Confidence).
- Studies indicate that large scale randomised testing, contact tracing, and quarantine underpin successful infection control strategies for containing campus outbreaks (Medium to High Confidence).
- Quantitative and qualitative work are needed urgently to identify the most common approaches to and requirements for testing and other interventions in universities.
- Additional work is needed to understand the costs, feasibility and acceptability of universal, asymptomatic testing in universities, including more diverse student and staff populations.
- Maximising uptake of testing and protective behaviours among those who need to be on campus for in-person courses must be underpinned by support packages that are tailored to specific needs if testing indicates the need to self-isolate (High Confidence).
- Following a positive test, information about the principles underlying self-isolation should help people understand why and how to adhere. Multiple studies in the current pandemic and in previous outbreaks have shown that low levels of knowledge, not believing the illness to pose a serious risk and not perceiving a benefit to self-isolation are associated with lower adherence (High Confidence).
- Long term planning beyond the end of the spring term is required to provide the certainty that the HE sector needs, minimise uncertainty for students and staff, and to help minimise risk of national transmission (High Confidence).
Future considerations
As previously seen, current national restrictions won’t all be lifted at the same time and student returns can significantly affect community transmission, though the extent of impact will vary between locations (Medium Confidence). When sequencing the lifting of restrictions, university returns could feasibly be one of the last restrictions to be removed; relative to other restrictions, non-returns are likely to create fewer harms (Low Confidence).
Universities have been delivering online education throughout the pandemic. There is a low barrier to continuity of delivery online and once provision is set up it can be continued easily (Low Confidence). Universities have already demonstrated that many exams can be delivered online.
Ultimately, there may be a need to work with training providers (and other practice related training courses) about how competencies are evidenced, especially when these can’t be evaluated in person due to closures, amongst other factors.
1. Testing and Student Behaviour
DfE advises HE providers should set a clear expectation that all students should access coronavirus (COVID-19) testing on their return to university, including those returning to face-to-face teaching in January and those returning later. How can as many students as possible be encouraged to participate in mass testing on return to university?
Modelling of COVID-19 in university settings indicates that students are highly connected through their courses, which makes them susceptible to higher rates of transmission [footnote 1]. There is evidence to argue for a combination of measures to identify and contain infection, and to support students during outbreaks. Universal, asymptomatic testing of staff and students must be accompanied by other infection control measures as it cannot prevent or control outbreaks on its own. These studies consider the effectiveness of testing and other measures (such as contact tracing, mask wearing, ventilation, quarantine, moving large classes online, and so on) against the disruption caused by these measures. Similarly, an analysis of the effectiveness of the Taiwanese experience of keeping universities open suggests that a combination of strategies that include containment and mitigation are needed [footnote 2]. Results indicate that large scale randomised testing, contact tracing, and quarantine underpin successful strategies for containing campus outbreaks [footnote 3]. Many universities are already requiring students to engage with organisational tracing, quarantine, and isolation procedures as part of their social contract between the university and students.
Acceptability of testing in universities
Little is known about the feasibility and acceptability of universal, asymptomatic testing of staff and students in universities [footnote 3]. A two-week trial involving the offer of 4 COVID-19 PCR (polymerase chain reaction) swabs to staff and students (N=1053) based in the Norwich Research Park (the University of East Anglia and assorted business and research institutes) found that repeated self-testing for COVID-19 using PCR is feasible and acceptable to a university population [footnote 4]. They reported that 76% (798 of 1053 total) who registered provided at least one swab, and that 86%(687 of 798 total) of participants who received at least one result returned all 4 swabs (low dropout rate). A majority of participants (71%) agreed or strongly agreed that taking the swabs was easy to do. Feedback from 266 (59%) of respondents was generally positive including requests for continued testing, and 97% of participants reported that they would take up repeated testing if it was made available. Finally, an 11-item post-trial survey found high acceptability. Further research is needed to ascertain whether or not positive test results and resultant quarantine or isolation would impact the high levels of positive feedback and engagement with the process.
A note of caution is needed when interpreting these results. The generalisability of this work to a diverse Higher Education (HE) student population must be explored further [footnote 3]. The positive feedback from the post-trial survey was biased towards staff (81%), with only 16% of students engaging with this part of the study. Low rate of experimental uptake is a concern, with 19% of the eligible population enrolling, of which 24% dropped out without providing a sample. The researchers argue that the time of year (summer), pace of the study, and work from home guidance meant that many members of staff and students were not on campus. Additional work is needed to understand the costs, feasibility and acceptability of universal, asymptomatic testing of staff and students in universities. Existing research must be extended to broader, more diverse student and staff populations, and focus on student perceptions, experience, and responses.
Barriers to student engagement with university mass-testing programmes
Student intention to engage with university testing programmes appear high. Greater understanding of the enablers and barriers to engagement will inform more effective programmes. A December 2020 update of ONS data [footnote 5] exploring student intentions and views on COVID-19 testing found that:
- two-thirds of students have downloaded the NHS COVID-19 or Protect Scotland apps;
- between 85 and 89% reported that they would request a test if they developed COVID-19 symptoms. Between 82 and 86% said that they would stay at home
- 85% of students reported that they would be likely or extremely likely to share details of people they have been in contact with if contacted by the NHS test and trace service
- The most common reason for not getting a test was a belief that they only need to self-isolate, wanting the test to go to someone else who needed it more, or if their symptoms had only been mild or had improved
Low student response rates (2%) were a challenge for this wave of the ONS student insights survey [footnote 5]. This data is still useful as it demonstrates the variety of factors informing student unwillingness to request a test if they develop symptoms of COVID-19 (Annex A) [footnote 6]. The reasons provided echo previous SPI-B advice on ‘Increasing adherence to COVID-19 preventative behaviours among young people’ and the importance of symptom recognition in leading people to request a test [footnote 7] [footnote 8].
Specifically, barriers to student engagement with mass-testing programmes upon return to university may include [footnote 9]:
- uncertainty about whether to get tested;
- low perceived risk of coronavirus infection in self and contacts;
- concern about consequences of triggering self-isolation for self and others;
- concern about consequences of disclosing contacts; and
- practical and psychological barriers to self-isolation.
Enablers to student engagement with university mass-testing programmes
Universities can also provide unique opportunities to address common barriers to mass uptake. Their ability to do so will depend on the type of campus, courses, cohorts, embeddedness in local communities, relationships with on-and off-campus students, partnerships with external organisations (such as clinical placements), practical, and research capabilities.
Access:
Where students are undertaking courses with clinical and professional preparation components (for example, medicine and nursing, but also education), testing arrangements and requirements will likely be informed by contracts with placement sites, such as NHS acute trusts. Adherence to these arrangements and requirements can be used as an additional tool to ensure uptake of testing.
Support:
HE institutions should put in place strategies to support students who are required to isolate to promote adherence to testing and isolation, including by providing dedicated accommodation where it is feasible to do so to minimise ongoing transmission in halls of residence or shared housing [footnote 10]. Rates of self-isolation following a positive test would likely be improved with the addition of different forms of support [footnote 7]. These include the following.
-
Financial support: Ensuring that those required to self-isolate would not experience financial hardship in doing so. Young people are more likely than adults to work in occupations with high numbers of social contacts, and with less recourse to sick pay, which may undermine their motivation to seek testing and ability to isolate in response to symptoms. Policy should be coordinated to ensure any offer to students does not cause inequalities by trumping the offer to other groups such as the self-employed and casual worker.
-
Tangible, non-financial support: Support for isolation does not always need to be financial. Avoiding catch-all funding can help universities avoid incentivising positive testing – namely, when the package for testing positive makes such an outcome appear desirable and therefore influences behaviour. Instead, consider the aims of the specific modes of support rather than catch-all funding. For example, facilitating social connections through access to data.
-
Proactive outreach is needed, to identify and resolve any practical needs that people have (such as access to food).
-
Information: Improved communication to the general public explaining how and when to self-isolate, and why it helps, would be useful, in addition to more detailed advice for those self-isolating (such as a help-line or SMS service). This information will also need to be adapted to specific target groups such as university staff and students. Diversity within the staff and student population must be considered when developing targeted communications.
-
Educational support: Accessible, high quality online education must be provided to students who are unable to attend in person. This will help offset the belief that face-to-face education is better, which can act as an incentive not to isolate.
-
Emotional support: For those who need it, access to social support or more formal clinical interventions delivered remotely if possible. Wellbeing in young people may impact their ability to adhere to interventions. Online, NHS and settings-based interventions to support young people’s mental health and wellbeing should be increased. [footnote 7] Most universities will have counselling services. These may require additional support to cope with increased demand.
Provision of a support package that encompasses these 6 components, should be rolled-out and evaluated as a matter of urgency in order to realise the considerable investment made in testing programmes, and the potential of testing and self-isolation to contribute to economic recovery and prevention of disease [footnote 11]. Although the focus of this paper is on student support, packages of support must also involve and support the workforces that support students such as lecturers, professional services, cleaners, security staff, and others.
Communication:
Guidance on how to behave is more likely to be adhered to if people understand the reasons they are asked to take certain actions, and if it is co-produced with a broadly representative group of the staff and students who will be affected by it [footnote 10].
-
‘Clear, consistent communications and an intuitive web application are needed for helping participants to understand the need for testing and the process of undertaking and returning the test’ [footnote 4]. All communications, whomever they target, should be appropriate and accessible for young people [footnote 7]. This should be supported by prompts (such as posters, signs) in relevant settings.
-
Following a positive test, information about the principles underlying self-isolation should help people understand why and how to adhere. Multiple studies in the current pandemic and in previous outbreaks have shown that low levels of knowledge, not believing the illness to pose a serious risk and not perceiving a benefit to self-isolation are associated with lower adherence. The importance of making information clear should not be underestimated. Targeted messages to those who are self-isolating may also be helpful [footnote 11].
-
The majority of students studying in person at HE institutions during the January 2021 restrictions are from clinical courses such as medicine, nursing and allied health professions. This poses a challenge in terms of additional pathways of exposure (see below) but it also poses an opportunity, as these students are being socialised into professional ‘helping’ careers. Targeted messaging to support adherence to protective behaviours, including testing, should draw on professional responsibilities and codes of practice to align these protective behaviours to aspirational professions and developing identities (for example ‘first do no harm’, GMC Good Medical Practice) [footnote 12].
-
Student intentions and efforts to follow COVID-19 related guidance must be recognised and reinforced. The evidence supports this though university students are often put in the frame for driving the infection.
Co-design:
High levels of engagement also require bridging cultural and language barriers to achieve engagement across diverse communities. The key principles for achieving this include co-design with representatives of target communities of interventions and messages, and promotion of testing and isolating in terms of an ethic of care for others rooted in collective identities and norms [footnote 13].
High levels of engagement in health-related interventions are built on trust, shared goals, and perceived fairness. Trust in those running services may be particularly important for engagement in government test and trace systems, with perceived credibility of government associated with likelihood of self-isolating [footnote 13]. Data suggest that young people may have strong motivation to adhere, but this is undermined by lack of trust in government and lack of clear information [footnote 7].
Additional Considerations for Testing and Student Behaviour:
A variety of university testing programmes and approaches are posted online [footnote 14] [footnote 15] [footnote 16]. However, there is a dearth of easily accessed data on what is currently happening in universities. This need for data extends beyond testing to include the other combinations of protective actions universities are taking (for example, ventilation, one-way systems, face masks, as well as other actions). Quantitative and qualitative work are needed urgently to identify the most common approaches to and requirements for testing and other interventions in universities. If institutions are not implementing specific interventions, it would be useful to understand why.
Universities may wish to consider creating a social norm around testing for staff and students where it becomes socially unacceptable not to adhere to testing programmes. There is a risk that students will believe that their initial test upon return applies throughout their term. The need for regular testing must be communicated clearly. While the Norwich COVID-19 testing initiative pilot suggests that students may be open to repeated testing if offered, assumptions about the acceptability of a mandatory approach must be tested. It is worth discussing whether access to university spaces will be made conditional on students having recent negative results and what will happen to existing students who decline testing. It may be possible to prioritise students who need to travel to university in local testing centres prior to their departure.
Further consideration must be given to the ways in which a record of testing can (or should) be linked to student ID’s and access. Again, the Norwich COVID-19 testing initiative included useful suggestions about data and reporting of test results to students [footnote 4].
Finally, the diversity of student populations must be recognised alongside the varied impacts of a positive test result. Some students will be unable to isolate due to caring responsibilities, others due to their household conditions, others due to their financial situation, amongst other reasons. Support packages must be flexible enough to support those most in need to enable them to engage with the requirements of the testing system.
2. Impact on the wider community
In September, there was an increase in the rate of transmission across regions at the same time as students were returning. Is there any evidence of a connection between the two?
Links between university students and the wider community are diverse. It is important to gain a better understanding of these links and interactions as, ‘reduction of infectious disease transmission in this demographic will reduce overall community transmission, lower demands on health services and reduce risk of harm to clinically vulnerable individuals while allowing vital education activity to continue’ [footnote 17]. Some of the links between universities and wider communities will be determined by the type of university (whether rural, urban (suburbs), urban (city centre), science parks), campus designs (self-contained, or spread-out across multiple campuses), university programmes of study (such as health, management, security, geography, physical sciences and STEM, SHAPE, and more), the number of students and staff who live on campus or in the community, the number of students and staff who commute, and the number of students who take on campus-based or local employment.
Consider clinical placements which may carry a particular risk to wider communities and to students of localised outbreak arising from non-adherence, where the transmission pathway is clinical contacts in students undertaking clinical courses. This is poorly characterised. Additionally, there is no strong evidence that those in HE demographics in general play a smaller role in transmission than adults in the general population (medium confidence). Evidence suggests there are a higher proportion of asymptomatic cases among younger age groups, meaning that cases and outbreaks are likely to be harder to detect among student populations [footnote 10].
DfE reported that 62% of students in the HE sector surveyed by NUS had a job alongside their study in the latest academic year (7,239 HE responses, weighted to HE student population) [footnote 18]. 24% of HE students surveyed were in part time employment, 13% had zero hours contracts, and 12% were in full time employment [footnote 19]. This is only part of the picture, however, with HESA reporting great variation in the number of staff and students commuting to English HEIs by region. These figures increase to over 50% in Greater London.
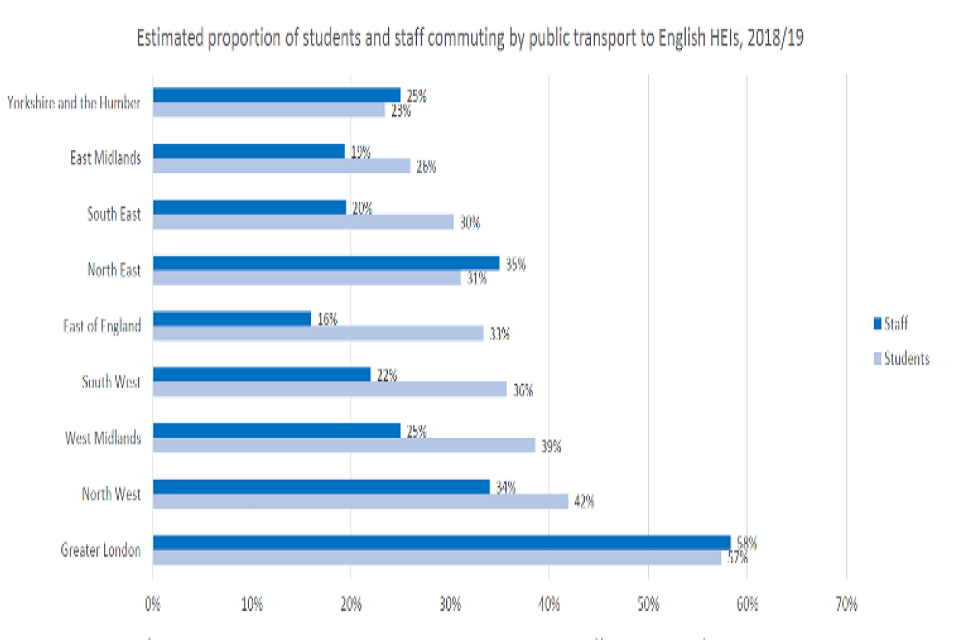
Source: HESA 2018 to 2019 Estates data for English Higher Education Institutes. Based on complete data for 84 providers for staff. Averages were calculated internally. Public transport includes bus and train.
While we are more reliant on modellers to illustrate the impact of on and off-campus employment, accommodation, socialising, and commuting on infection rate, the behavioural and social sciences can bring fresh insights into the understanding of the dynamics connecting universities to communities. For example, around 25% of the student population stay in the family home during their university degrees. Their ‘commuter student’ status can intersect with other disadvantages such as lower Socio-economic Status, BAME backgrounds, mature students, and students who are the first generation in their families to enter higher education [footnote 20]. Commuter students also tend to have poorer outcomes compared to students who relocate to a university to study, report lower rates of belonging, engage in lower rates of continuation, and receive lower degree classifications [footnote 20]. Specific communications on managing infection risk should include commuter students and students with part time jobs or caring responsibilities [footnote 10].
In terms of longer-term impacts, the closure of universities during COVID-19 has the potential to amplify the importance of the contributions these institutions make to society. Specifically, unless mitigations are put in place, university suspension and disruption interrupts the supply chain of newly trained graduates into key worker professions including health (nursing, medicine), social care, science, engineering, teaching, and more. ‘Suspending university education would increase existing shortages of essential degree-qualified workers across multiple sectors’ [footnote 17].
In spite of these potential long-term impacts, the relationship between universities and transmission suggests that, when sequencing the lifting of restrictions, university returns could feasibly be one of the last restrictions to be removed; student returns are likely to make a big difference to transmission and, relative to other restrictions, non-returns are likely to create fewer harms if alternative modes of education, training and accreditation are found.
3. Risk to students and those of their age group
What transmission behaviours have been observed for young people in this age group who are students in higher education, compared to those who are not and have stayed in the wider community? Is there any evidence to suggest that students are less at risk when in a university setting?
Universities expose young people to very large numbers of social contacts. Young people are more likely to live in all-adult, crowded, multi-occupancy housing often with poor ventilation which may further contribute to rapid transmission [footnote 7]. Therefore, accommodation and social interactions are likely to be a high-risk environment for transmission to occur [footnote 22]. Recent ONS Universities Surveillance work investigated the risk of infection to students in different settings [footnote 20]. Bringing together information gathered at a number of English universities, they found:
- the risk of transmission to be greater in residential settings such as halls and student houses
- minimal evidence of the virus being spread in face-to-face teaching settings such as classrooms and lecture theatres
- the largest outbreaks occurred in halls of residences
However, students living in halls were over-represented in the testing data, so the higher rates found in halls may be influenced by students living in halls being more likely to present for testing than those in private accommodation. Where possible, strategies to mitigate transmission risk include segmentation of students to co-locate courses or year groups, and good communication on behaviour and hygiene in household and social environments [footnote 10].
Student behaviours and risk mitigations
In many respects, student behaviour may be less risky than that of other adults. ONS data found that students reported that they were more likely not to have left their residence in the past 7 days prior to being surveyed (between 2 and 3 in 10) than the general public (less than one in 10). These ONS surveys also shown students reporting high levels of adherence to social distancing (2 meters), hand washing, and a decrease in inviting others over [footnote 5].
Greater recognition of high-risk activities and the associated evidence-based mitigations can facilitate the re-opening of universities when levels of infection decrease. Behaviours identified through a Hazard Analysis of Critical Control Points (HACCP) framework assessed the risks associated with university student activity and identified key critical control points for on and off-campus university student’s activities, lifestyle and interaction patterns [footnote 17]. This approach identifies behaviours that are likely to present direct and indirect risks for the transmission of SARS-CoV-2. Critical Control Points (CCPs) are points at which pathogen transmission can be prevented or eliminated. Table 1 provides a summary of high-risk CCPs. Each point provides an opportunity to identify and adopt measures to reduce transmission risks for students who are currently on campus, and students who will return when the infection rates decrease. Evidence-based recommendations accompany each CCP in the original document.
Table 1: A summary of the high-risk activities identified through a Hazard Analysis of Critical Control Point (HACCP) Assessment. [footnote 17]
- Preventing arrival of virus into the student household
- Shared car or minibus journey (including shared transport to placements, sporting events, field courses, social events, and so forth)
- Returning to university household after time (overnight) away
- Interaction with people beyond university household (this includes the students having different placement groups to their household members)
- Sharing of personal items
- Indoor queuing or crowding
- Sharing of study facilities
- Outdoor queueing
- Sharing of prayer facilities
- Sharing of changing facilities
- Sharing training or practice facilities
- Singing or cheering
- Participation in conferences, meetings, and so forth
- Sharing accommodation on field courses
- Examining patients (High to low, depending on use of PPE)
- Remaining in one room whilst on placement
- Moving around within buildings
- Sessions in teaching rooms
- Working in a group
- Seating in teaching rooms
- Undertaking physical exams such as OSCEs, consultation skills or physical manipulation
- Provision of ad hoc in-person support (such as advisors, last minute support)
Student mental health
Disruption and closure of universities during COVID-19 carry mental and physical health costs for university students. While individuals under 25 years of age are least in danger from the virus, they stand to disproportionately shoulder the most significant long-term burden as a result of the efforts to control the virus. ‘These dis-benefits and disadvantages include reduced education, reduced employment opportunities, living longer with degraded quality public services that in turn includes education that is likely to be highly resource-restricted in the near future’ [footnote 23] [footnote 17].
Young people’s (16- to 24-year-olds) mental health was disproportionately affected during the last stay at home order. University College London found that loneliness during early lockdown was common for 18- to 24-year-olds in the UK at an age when social contact counts tend to peak rather than contract [footnote 24] [footnote 25]. Full-time home-study increased loneliness and was often beset by practical problems; young adults are often living in rented accommodation without adequate space and quiet to study effectively [footnote 24] and where high-quality internet access and access to a PC or laptop cannot be assured [footnote 26] [footnote 27].
There is evidence of physical and mental health impacts from missing or limited access to education and from the reduced social interaction and support that can arise from remote learning. Although direct evidence in HE is more limited than in schools, survey evidence related to COVID-19 indicates disruption to research and learning, lower wellbeing and increased mental distress [footnote 5]. Further restrictions and short-term actions such as isolation in response to test and trace may have additional impacts on wellbeing.
Data may be limited, but COVID-19 specific-impacts can be observed. The Covid Student Insights Survey reported the following statistics as part of the November and December waves of results [footnote 28] [footnote 5].
- More than half (57%) of respondents reported a worsening in their mental health and well-being between the beginning of the autumn term (September 2020) and the November survey.
- Changes to the student experience because of COVID-19 resulted in 29% of students reporting being dissatisfied or very dissatisfied with their academic experience, and over half (53%) of students reported being dissatisfied or very dissatisfied with their social experience in the autumn term.
- The main reasons for dissatisfaction with their academic experience related to limited opportunities for social or recreational activity (86%), limited opportunities to meet other students (84%) and limited access to sports and fitness facilities (52%).
- Students are significantly more anxious than the general population of Great Britain, with mean scores of 5.3 compared with 4.2 respectively, (where 0 is ‘not anxious at all’ and 10 is ‘completely anxious’).
- Students responding to the SCIS reported lower levels of life satisfaction, life worthwhile and happiness, and higher levels of anxiety, compared with the general population through the OPN.
- In contrast, half of students reported that they were satisfied, or very satisfied with their academic experience; this was slightly higher for first-year undergraduate students (55%) compared with other undergraduate students (44%).
Figure 2 demonstrates that, over recent years, personal well-being measures of undergraduate students have declined for students and are lower than the general population aged 20 to 24 years.
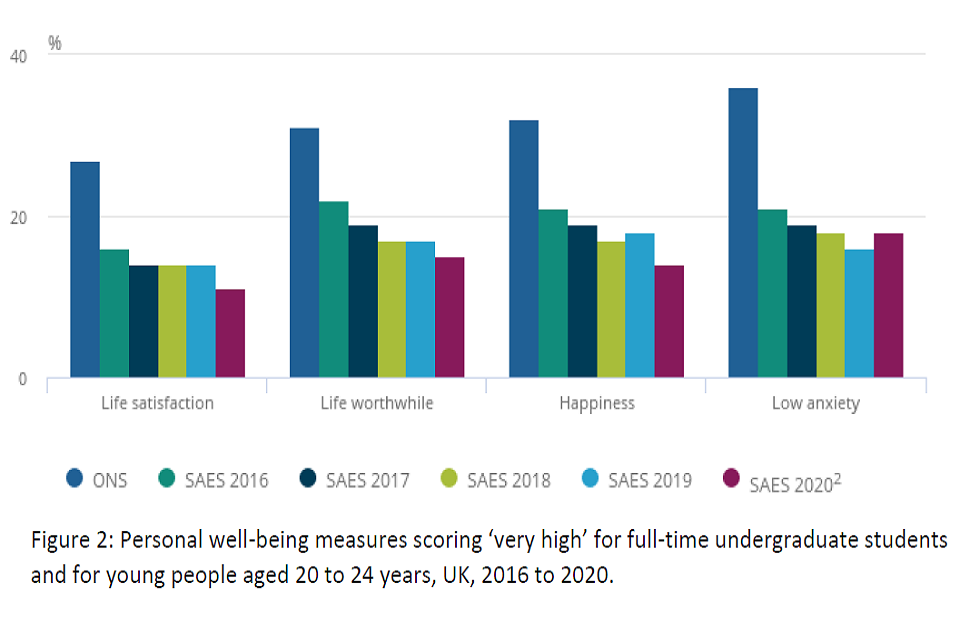
Figure 2: Personal well-being measures scoring ‘very high’ for full-time undergraduate students and for young people aged 20 to 24 years, UK, 2016 to 2020.
Additional Considerations for Student Mental Health:
- The mental health impacts of COVID-19 on university students is evident. University counselling and support services struggled to meet rising demand prior to COVID-19. Universities will need to support in addressing the impacts of COVID-19 on the mental health and well-being of their student population. Consideration of extending this support beyond graduation is needed.
- The evidence-base surrounding the impact of COVID-19 on HE student mental health, well-being, and course satisfaction is growing. Additional information is needed in the areas of educational impacts (such as lost learning) and the longer-term impacts of disrupted education on graduate study and employment.
- Evidence of the COVID-19 related health, mental health, well-being, and job satisfaction impacts on university staff must be explored. Staff play a fundamental role in supporting students, delivering education, maintaining safe environments, and mitigating the impacts of COVID-19 on the student population.
Bibliography
-
K. A. Weeden and B. Cornwell, ‘The small world network of college classes: Implications for epidemic spread on a University Campus,’ ‘Sociological Science’, vol. 7, no. 9, p. 222–241, 2020. ↩
-
M. M. D. Shao-Yi Cheng, ‘How to Safely Reopen Colleges and Universities During COVID-19: Experiences From Taiwan,’ ‘Annals of Internal Medicine’, vol. 173, no. 8, 2020. ↩
-
J. R. P. Philip T Gressman, ‘Simulating COVID-19 in a university environment,’ ‘Math BioSci’, vol. 328, 2020. ↩ ↩2 ↩3
-
T. Berger-Gillam, J. Cole, K. Gharbi and . al, ‘Norwich COVID-19 testing initiative pilot: evaluating the feasibility of asymptomatic testing on a university campus,’ ‘Journal of Public Health’, no. https://doi.org/10.1093/pubmed/fdaa194, 2020. ↩ ↩2 ↩3
-
ONS, ‘Coronavirus and the impact on students in higher education in England: September to December 2020,’ 2020. ↩ ↩2 ↩3 ↩4 ↩5
-
ONS, ‘Student Covid Insights Survey (Pilot), 20 November to 25 November’. ↩
-
SPI-B, ‘Increasing adherence to COVID-19 preventative behaviours among young people,’ 2020. ↩ ↩2 ↩3 ↩4 ↩5 ↩6
-
SPI-B, ‘How important is symptom recognition in leading people to seek a test for COVID-19?,’ 2020. ↩
-
SPI-B, ‘Key behavioural issues relevant to test, trace, track and isolate,’ 2020. ↩
-
SAGE, ‘Priniciples for Managing SARS-Cov-2 Transmission Associated with Higher Education,’ 2020. ↩ ↩2 ↩3 ↩4 ↩5
-
SPI-B, ‘The impact of financial and other targeted support on rates of self-isolation or quarantine,’ 2020. ↩ ↩2
-
H. Rashid, J. K. Yin, K. Ward, C. King, H. Seale and R. Booy, ‘Assessing Interventions To Improve Influenza Vaccine Uptake Among Health Care Workers,’ ‘Health Affairs’, vol. 35, no. 2, 2016. ↩
-
SAGE Multidisciplinary Task and Finish Group on Mass Testing, ‘Behavioural Considerations,’ 2020. ↩ ↩2
-
E. Mahase, ‘Covid-19: Universities roll out pooled testing of students in bid to keep campuses open,’ ‘BMJ’, vol. 370, 2020. ↩
-
King’s College London, ‘Lateral Flow antigen testing for coronavirus (COVID-19),’ [Online]. [Accessed January 2021]. ↩
-
University of Bristol, ‘Mass testing for COVID-19,’ [Online]. [Accessed January 2021]. ↩
-
K. L. Edmunds, L. Bowater, J. Brainard, J.-C. d. Coriolis, I. Lake, R. R. Malik, L. Newark, N. Ward, K. Yeoman and P. R. Hunter, ‘The COVID University Challenge: a Hazard Analysis of Critical Control Points Assessment of the Return of Students to Higher Education Establishments,’ https://doi.org/10.1101/2020.12.11.20247676, 2020. ↩ ↩2 ↩3 ↩4 ↩5
-
NUS, ‘COVID-19 and Students Survey Report,’ 2020. ↩
-
DfE, ‘Additional information on Higher Education Settings in England: Note to SAGE to support COVID19 modelling,’ 2020. ↩
-
L. Thomas, ‘Commuter Students during and after Covid-19,’ June 2020. [Online]. ↩ ↩2 ↩3
-
ONS, ‘How has coronavirus (COVID-19) spread among students in England?’, 2020 ↩
-
C. S. Maher, T. Hoang and A. Hindery, ‘Fiscal Responses to COVID‐19: Evidence from Local Governments and Nonprofits,’ ‘Public Administration Review’, vol. 80, no. 4, 2020. ↩
-
C. Leavey, A. Eastaugh and M. Kane, ‘Building the case to protect young people’s future health,’ ‘The Health Foundation’, 30 August 2020. ↩ ↩2
-
J. Mossong, N. Hens, M. Jit, P. Beutels, K. Auranen, R. Mikolajczyk, M. Massari, S. Salmaso, G. S. Tomba, J. Wallinga, J. Heijne, M. Sadkowska-Todys, M. Rosinska and J. Edmunds, ‘Social Contacts and Mixing Patterns Relevant to the Spread of Infectious Diseases,’ ‘PLOS Medicine’, March 2008. ↩
-
B. Auxier, M. Anderson, A. Perrin and E. Turner, ‘Parenting Children in the Age of Screens,’ ‘Pew Research Center’, 2020. ↩
-
J. Wakefield, ‘Coronavirus: Coping with lockdown on poor broadband, BBC News,’ 02 May 2020. [Online]. ↩
-
ONS, ‘Coronavirus and higher education students: England, 20 November to 25 November 2020,’ 2020. ↩
