Osteoarthritis of the knee in professional football players: position paper 44
Published 3 April 2020
Summary
This position paper updates an earlier review by the Council into Sporting Injuries published in 2005. That report concluded there was clear evidence that traumatic joint injury increased the later risk of osteoarthritis, and found the evidence for osteoarthritis of the hip or knee in footballers arising in the absence of identifiable accidental injury was weaker.
A comprehensive review of the recent published literature relating to osteoarthritis (OA) in footballers has been carried out by members with musculoskeletal expertise to understand whether, and to what extent, there is a risk of OA associated with playing professional football.
The Council did not find enough consistent evidence that the risk of knee OA is doubled amongst football players in the absence of a traumatic knee injury. The Council has therefore decided against recommending prescription for OA of the knee in footballers, but it remains open to the possibility of reviewing its position as the research evidence base continues to grow.
The Council does however encourage ex-professional footballers who had a documented knee injury during their playing career, and later developed osteoarthritis in that knee, to consider making a claim under the accident provision of IIDB.
This report contains technical terms, the meanings of which are explained in a concluding glossary.
Background
1. Osteoarthritis (OA) is a common and disabling condition which represents a substantial and growing health burden for individuals, healthcare services and wider society. With ageing populations and increasing obesity, the burden of the condition is increasing steadily [Hunter]. OA is a disease of the whole joint, involving structural changes to the articular cartilage, subchondral bone, ligaments, capsule, synovial membrane and peri-articular muscles [Hunter].
2. Clinically, the knee is the site most commonly affected by OA [Hunter]. In fact, it is estimated that knee OA accounts for 85% of the total burden of disability from OA worldwide [GBD]. It is estimated that 9% of European adult women have symptomatic OA knee, as compared with 3% of European adult men [Hunter].
3. Pain is the dominant symptom of knee OA but it can also cause swelling, stiffness, and restricted range of movement. It can be a significant cause of disability. Surgery is reserved for cases in which all appropriate, less invasive options have been tried for a reasonable period of time. Despite this, some 1.1 million partial or full knee joint replacement operations were performed in Britain in 2017-8 [NJR].
4. Genetic factors are thought to account for 40-80% of the variance in risk of OA. Well recognised non-occupational risk factors for osteoarthritis of the knee include female gender, advancing age, obesity, various inflammatory joint diseases, traumatic knee injury, previous meniscectomy and Heberden’s nodes [Cooper].
5. In addition, a growing body of research evidence indicates that OA is found more frequently in people whose occupations entail hard, repetitive, physically demanding use of the knee joints. Relevant observations include reports by Manninen (2002), Felson (1991), Sandmark (2000a, 2000b), Kivimaki (1992), Schouten (1992), Anderson (1998), Coggon (2000), Lau (2000), Dawson (2003), Vingard (1991, 1992), Cooper (1994), Seidler (2008) and Jensen (2000, 2005). Reviews of the evidence can be found in Palmer (2012) and in two earlier reports of the Council (Cm 7440, 2008; Cm 7964, 2010).
6. Knee OA is recognised as being eligible for benefit under the industrial Injuries Disablement Benefit (IIDB) Scheme as prescribed disease (PD) A14. However, prescription has proved possible so far only in two occupational circumstances:
1. work underground in a coal mine (for at least 10 years in aggregate in certain specified jobs and timeframes); and 2. work wholly or mainly fitting or laying carpets or floors (for at least 20 years in aggregate).
7. In 2005, the Council considered prescription of knee and hip OA amongst footballers in its Position Paper 15 – Sporting Injuries, which also considered the risk of dementia in boxers, footballers and jockeys (position paper 15, 2005). At the time, the Council found clear evidence that traumatic joint injury (e.g. fracture, ligamentous injury or torn cartilage) increased the later risk of osteoarthritis. However, where osteoarthritis of the hip or knee follows an identifiable accident, a claim for benefit can be made under the accident provisions of the Industrial Injuries Disablement Benefit scheme. The Council concluded that there was insufficient evidence that osteoarthritis of the hip or knee in footballers could arise in the absence of identifiable accidental injury and therefore, the Council could not recommend extending the terms of the prescription.
8. In 2018, the Council received a request from stakeholders such as the Professional Footballers Association (PFA) and Xpro to review the decision about prescription for knee OA amongst footballers in the light of new evidence published in the UK [Fernandes]. In response, the Council undertook an updated literature review and this report outlines its findings. The considerations and challenges behind prescription for PD A14 and the Council’s position on the scope for extending the prescription’s terms are also described.
Conditions of prescription
9. The Social Security Contributions and Benefits Act 1992 states that the Secretary of State may prescribe a disease where they are satisfied that the disease:
“a) ought to be treated, having regard to its causes and incidence and any other relevant considerations, as a risk of the occupation and not as a risk common to all persons; and
b) is such that, in the absence of special circumstances, the attribution of particular cases to the nature of employment can be established or presumed with reasonable certainty.”
In other words, a disease may only be prescribed if there is a recognised risk to workers in an occupation and the link between disease and occupation can be established or reasonably presumed in individual cases. This is the framework IIAC must observe when weighing the grounds for prescription.
10. For some diseases, attribution to occupation is relatively straightforward. If, for example, the disease rarely occurs outside work (e.g. mesothelioma) or has distinctive clinical features when caused by work (e.g. occupational asthma), then attribution to employment can be established or presumed with reasonable certainty in a given claim simply from the clinical picture and the occupational history.
However, for other diseases, including knee OA, there are no special features that allow individual claims to be attributed like this. Instead, attribution depends on evidence that the disease is more frequent in people with that type of work. The threshold normally applied by the Council, as explained in other reports, requires reasonably robust evidence that a given work exposure or activity more than doubles the risk of disease. Broadly speaking, this corresponds to the probability that an individual claimant’s disease is more likely than not to have arisen from their occupational exposure (i.e. it is attributable on the balance of probabilities).
Knee injury and risk of osteoarthritis
11/. The knee is a complex structure, combining two articulations with three bones (femur, patella and tibia) to produce six degrees of movement (Figure 1 and 2).
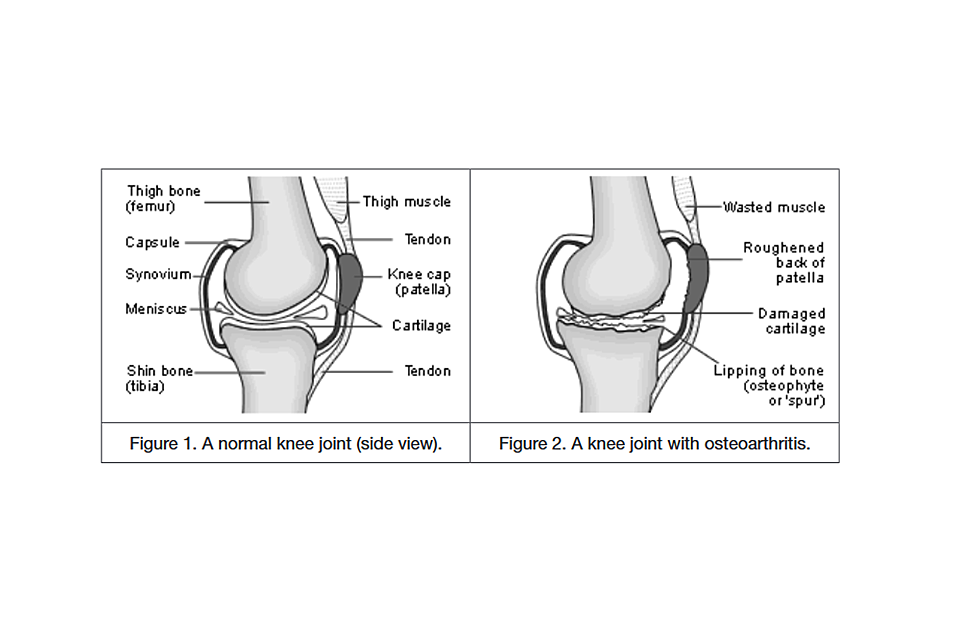
Fig 1. Image of a normal knee joint and fig 2. A knee joint with osteoarthritis
Its stability is derived from pairs of ligaments which are both inside the joint (anterior and posterior cruciate ligaments) and outside the joint (collateral ligaments). Two c-shaped pieces of cartilage (medial and lateral menisci) provide shock absorption within the joint. At one extreme, acute knee injury occurs after a significant level of external force (or trauma) is applied and the injury causes severe pain, rapid swelling and often is associated with a systemic reaction (hypotension, sweating and shock). However, at the other end of the scale, knee injuries can result in posttraumatic pathology that is not identifiable directly after the incident so that the patient or athlete may carry on as normal with/without symptoms. Research studies using MRI after mechanical insult show ill-defined subchondral bone signal changes, which are able to heal spontaneously, given the opportunity. However non-resolving, chronically symptomatic injuries can cause disuse leading to quadriceps atrophy and weakness with consequent increased vulnerability to future risk of injury [Salzmann].
12. In the general population, there is convincing evidence of the important relationship between acute knee injury and subsequent knee OA [Thelin, Lohmander]. The literature has grown since the 2005 Position paper 15 such that two meta-analyses have been published. A 2011 meta-analysis pooling data from 24 studies including 24,000 people reported that acute injury increases the risk of knee OA four-fold (OR 4.2, 95% CI 3.11-5.66) [Muthuri]. Subsequently, in 2015, Silverwood and colleagues reported that a previous knee injury increased the risk of knee OA 2.8-fold [Silverwood]. However, both sets of reviewers commented on the wide difference in the rates of knee OA found in the different studies, which they attributed to the range of different definitions of injury that had been applied by researchers.
13. Typically, during a football match, footballers will: run; jump; repetitively accelerate and decelerate; undertake cutting manoeuvres; tackle; dribble the ball; shoot and have duels with/without the ball, as well as periods of standing or walking about. The actual physical activity is dependent on several factors including: player position, score, team strategy, level of performance, leg dominance, type of competition, age and gender, fitness level, and motivation [Salzmann]. Knee injuries are recognised to be particularly common in football and similar contact sports because of the pace and competitiveness involved. Most (80%) of these injuries are trauma-related but the remainder are attributed to “overuse”. The injury rate is higher among younger, less-skillful footballers and injuries are different in female, as compared with male, footballers: women are twice as likely to sustain anterior cruciate ligament and meniscus injuries than men. In most cases, injury results from the player with the ball being attacked by at least one player from the opposing team, causing a contact injury (two-thirds of all injuries) [Salzmann].
14. In football (soccer), the incidence of football-related injuries has been estimated at > 2 injuries per player/year or between 10-42 injuries per 1000 playing hours in adult male players [Salzmann]. Aside from soccer, one study of former Australian Rules footballers reported that 62% of former footballers had ever sustained a knee injury as compared with 6% of controls [Deacon]. Comparing ligamentous and meniscal injuries amongst ex-footballers and controls, the rates were 11-fold increased. Similar data are available for players in the American National Football League but AFL and NFL are different contact sports which may have different injury profiles [Golightly].
15. Typically, severe football injuries include rupture of the anterior cruciate ligament, torn or displaced meniscus or cartilage damage. A more common injury is sprain or partial tear of the medial collateral ligament but these are mostly treated conservatively and do not appear to carry any long-term risk of consequences. Injuries to the cruciate ligaments and menisci in particular seem to cause greater risk of future knee OA, at least as compared with non-specific types of injuries. However, a large number of studies do not report on the site or severity of injuries, and injuries (both internal and external) are classified in a range of different ways (e.g. requiring hospital treatment vs. resulted in knee pain for > 24 hours vs. time lost from play/training resulting from injury).
16. Amongst soccer players, Drawer et al reported that 47% of footballers, mean age 47.6 years, had retired because of injury and that almost half of the injuries involved were of the knee [Drawer]. Kettunen evaluated former elite male athletes who had represented Finland and found that 41% of soccer players reported physician-diagnosed knee ligament injuries (as compared with 7% of runners and 11% of controls) and that 45% of soccer players reported meniscal injuries (as compared with 11% of controls) [Kettunen]. Moreover, 52% of former soccer players had undergone hospital treatment for their knee injury. Krajnc found that 29/40 former professional footballers, mean age 49.2 years, reported a knee injury sustained whilst playing which resulted in time off playing or training for days/weeks afterwards, and that 18/29 had undergone surgery at least once for those knee injuries [Krajnc]. They also reported a higher prevalence of injuries in the non-dominant, as compared with the dominant, knee (65% vs. 35%). Amongst former UK soccer players, currently aged on average 56.1 years, Turner reported that 43% of respondents (55% response rate) had been treated non-surgically for knee injuries during their playing career [Turner].
17. There is also direct evidence from studies amongst footballers that knee injuries are associated with an increased risk of OA. Following young female (mean age 31 years) footballers 12 years after an anterior cruciate ligament (ACL) rupture, Lohmander and colleagues found that 82% of these players had radiographic OA as compared with 37% of uninjured knees. Comparison of those who had, and had not, undergone surgical reconstruction showed no difference in the rates of radiographic OA [Lohmander]. Likewise, Neyret reviewed a cohort of soccer players who had undergone meniscectomy 20 years earlier. Comparing those with and without concomitant ACL rupture, they found that 24% had radiographic OA if they had meniscectomy but intact ACL yet radiographic OA was found in 77% of those with ruptured ACL as well as meniscectomy [Neyret]. Amongst 152 former elite female footballers, currently aged 33 years, 64.5% reported at least one knee injury, 1 in 3 of which injuries required surgery and there was a modest increased risk of “self-reported physician-diagnosed arthritis” associated with those injuries (OR 1.32, p<0.001). Von Porat and colleagues traced 205 male soccer players with ACL rupture sustained whilst playing the sport 14 years earlier (aged 30-56 years at time of study) [von Porat]. They found that 41% of injured knees showed evidence of radiographic OA and that the risk was not affected by whether or not reconstruction had been performed. Furthermore, most of the respondents indicated that they had significant knee-related pain and dysfunction from their injured knees, according to validated outcome measures (KOOS, SF-36, Lysholm knee score). Gouttebarge et al surveyed 964 current and 396 retired professional footballers and found that injured footballers (whether retired or not) were nearly twice as likely to report a physician diagnosis of OA as compared with those without injury [Gouttebarge]. The risks of physician-diagnosed OA were also somewhat higher amongst individuals who had undergone surgery for their injury, as compared to those who had not. The risks amongst current footballers were: history of injury, RR 1.74, 95% CI 1.5-2.01; history of surgery, RR 1.96, 95% CI 1.66-2.29 and amongst retired players: history of injury, RR 1.87, 95% CI 1.61-2.31; history of surgery, RR 1.72, 95% CI 1.50-1.95.
18. As reported in the 2005 Position paper, when OA ensues as a consequence of a specific injury in an employee whilst at work, they can apply for compensation under the IIDB scheme under its accident provision. Therefore, for the terms of the prescription PD A14 to be extended to footballers, there needs to be sufficient evidence that the risk of knee OA associated with disability is consistently elevated above the “doubling of risk” threshold.
Therefore, in the remainder of this report, we review the epidemiological evidence which considers the risk of OA knee associated with playing professional football in the absence of having sustained at least one acute traumatic event to the affected knee.
Case definition of knee osteoarthritis
19. For the Council to reach a decision about prescription, it considers evidence from epidemiological studies. Unfortunately, “knee osteoarthritis” has been defined in several different ways in the available epidemiological studies: through imaging (typically based on X-rays (radiographic) but sometimes based upon another imaging technique (MRI or ultrasound)); clinically (using symptoms and physical signs); self-reported “physician diagnosed” arthritis; awaiting or received knee arthroplasty because of knee arthritis. The use of different approaches to case definition hinders interpretation of the epidemiological literature as some criteria will be more sensitive (more cases but greater risk of false positives) and others will be more specific (less cases but greater risk of false negatives). Moreover, even within different types of methods, there has been some variation of which criteria need to be fulfilled to become a true case (e.g. the number and type of radiographic changes). The following sections describe this variation in more detail.
Radiographic (X-rays) knee OA
20. Traditionally, epidemiological studies of the prevalence of OA have used X-rays to determine the diagnosis and define a case. Using standardised protocols, participants undergo X-ray of the knee(s). The images are then interpreted according to pre-defined criteria which encompass assessment of some or all of the following “typical” changes seen in OA: joint space narrowing; osteophytes; subchondral sclerosis and/or bone cysts. A range of different systems have evolved by which to “grade” these findings, including: Kellgren & Lawrence [Kellgren]; Nottingham Line Drawing Atlas [Nagaosa]; Danielsson method [Danielsson] and Ahlback criteria [Ahlback], each of which has been used at least once in the soccer and OA literature. Unfortunately, these systems place emphasis on different radiographic features so that studies applying different methods can produce varying results. Moreover, some radiographic systems produce a “grade” of the severity of radiographic change. For example, the Kellgren and Lawrence system can be used to grade X-ray changes from I-IV (with IV representing higher numbers of structural changes). This leaves opportunity for grades of X-ray changes to be applied differently in defining a “case”. For example, some researchers in this literature have defined a case of knee OA as having Kellgren & Lawrence changes grade II and above [Arliani, Iosifidis, Kuijt, Lv], whilst others use grades III and IV only [Elleuch, Fernandes]. Obviously, different cut-offs will again yield different rates of prevalence and different estimates of the risk associated with the exposure.
21. In prescription PD A14, the Council required that the diagnosis, where possible, was substantiated with radiographic changes that were at least Kellgren & Lawrence grade III and IV but did not make mention of other systems of grading. Further complicating the issue, it has become clear more recently that X-rays taken from slightly different views can also yield different rates of prevalence in the same patients even when applying the same classification system [Bedson].
Knee osteoarthritis diagnosed on MRI scan or Ultrasound scan
22. As musculoskeletal science has developed, researchers have investigated OA using other imaging modalities, particularly MRI, to better understand the disease and circumvent the difficulties described above with X-ray changes. We found two epidemiological studies evaluating the risk of knee OA associated with football without including X-rays, one of which used MRI [Arliani] and the other of which used ultrasound [Paxinos], as their definition of cases (Table 1). Unfortunately, currently, there is no agreement on which structural changes seen in these imaging modalities correlate best with clinical knee OA and therefore, here again, any evidence about the risk associated with football is difficult to interpret.
Clinical knee osteoarthritis
23. It is important to note that X-ray changes only show moderate associations between the structural impacts and the presence of pain in affected individuals [Bedson]. For example, in the American National Health and Nutrition Examination Survey-I (NHANES-I) study, half of those with OA of the knee confirmed by radiograph did not experience pain [Anderson]. In their review, Bedson & Croft reported that the proportion of those with knee pain found to have radiographic osteoarthritis ranged from 15-76%, and in those with radiographic knee OA, the proportion with pain ranged from 15% - 81%. Similarly, there is recognised to be a relatively poor correlation between structural changes on X-rays and disability or impairment reported by the patient. Given that prescription for Industrial Injuries Disablement Benefit requires not only the presence of a disease, but also an assessment of disability, it is important to define the terms of any prescription so that only limited numbers of people who qualify for an award come forward for assessment.
24. Clinical OA (as distinct from radiographic OA) is a diagnosis made on the basis of symptoms (pain, brief morning stiffness, and functional limitations) and a brief physical examination looking for clinical signs of crepitus (grinding, creaking, cracking, grating, crunching sounds), restricted or painful movement, joint tenderness, or bony enlargement. Pereira and colleagues undertook a systematic review comparing prevalence rates derived from X-rays with those derived from clinical definitions and showed that, in the general population, rates of prevalence of radiographic OA are considerably higher than rates of symptomatic OA. [Pereira].
25. Criteria for clinical diagnosis have been established by authoritative bodies including e.g. the American College of Rheumatology [Altman] and the European League Against Rheumatism [Zhang], although these are not always applied in research studies, particularly not amongst occupational epidemiological studies. Evidence from epidemiological studies in which clinical knee OA is the outcome has the potential to be more useful in defining a prescription but, unfortunately, such studies are still relatively uncommon.
Self-reported “physician diagnosed” osteoarthritis
26. In some epidemiological studies, where clinical evaluation is impractical (usually in large-scale questionnaire surveys), participants are asked whether they have ever been diagnosed with arthritis (or osteoarthritis) by a physician. We found three studies of the risk of OA amongst footballers that applied this definition [Tveit, Fernandes, Kettunen]. Unfortunately, self-reported “physician diagnosed” arthritis has been described as a weak and unreliable outcome measure which cannot be validated in the majority of studies. This particularly applies in the situation where responder bias is a risk: in other words, people who perceive themselves to have the outcome of interest of the research (knee osteoarthritis) are more likely to take part. Such studies are also prone to recall bias, and it has been shown that the lay public confuse terms such as “osteoarthritis” and “osteoporosis”.
On waiting-list for or having received arthroplasty for knee osteoarthritis
27. Knee arthroplasty surgery has revolutionised the management of knee OA for people with severe pain and disability from OA. According to the National Joint Registry, 99% of knee arthroplasty surgery in 2017-18 was performed for knee OA [NJR]. Since some will be unfit for surgery and many will not need it, studies which define the risk of OA using arthroplasty as the outcome will under-estimate the total burden of symptomatic OA, and will include a small number of patients who did not have OA as the main indication. Such studies are however useful in assessing the likelihood of an increased risk of knee OA associated with an exposure (in this case, football). There are a growing number of football studies in which this definition has been applied [Fernandes, Sandmark, Tveit]. However, should any prescription be reliant upon arthroplasty, it is important to recall that, in >90% cases, total knee arthroplasty is highly successful, relieving the pain and disability of knee osteoarthritis so that, although prescription may be possible on the basis of this outcome, there is a risk of bringing forward for assessment a large number of people who will not have any related disability.
Results of epidemiological studies which have attempted to control for injury
28. As observed, there are a number of weaknesses within the epidemiological literature surrounding the risk of OA amongst soccer players, with case definition being a key issue. Table 1 summarises the available studies which have defined OA radiographically, after excluding or adjusting for injury. Evaluating these, the data appear to be conflicting. Some studies suggest an increased risk of radiographic OA associated with soccer whilst others find no effect (or even the opposite). Three studies [Roos, Kujala, Fernandes] reported a doubling of the risk of radiographic OA, although they all applied different radiographic criteria. Roos measured joint space narrowing only; Kujala applied the rather “sensitive” criteria of K&L II, III and IV but the best evidence comes from Fernandes et al which applied NLDA and K&L III and IV grading, showing a greater than doubled risk with both methods. In contrast, two studies found an elevated risk that was not doubled [Arliani, Elleuch] and four studies showed no significantly increased risk of radiographic OA in soccer players [Iosifidis, Lv, Paxinos, Thelin].
Table 1 Summary of Studies that excluded, or adjusted for, the risk of injury that reported OA on imaging
| Author | Comparators | Numbers | Injury | Radiographic criteria | Findings |
|---|---|---|---|---|---|
| Arliani 2014 | Former male professional footballers 30-55 years old | 27 cases /30 controls (non-sportsmen matched for age and previous injury) | “Matched for injury” but apparent imbalance of meniscectomy cases and ACL cases. 9/30 controls had surgery whilst 11/27 cases had surgery | X-rays scored by K&L (K&L II, III, IV) | Prevalence of OA on X-rays compared for dominant and non-dominant knees: Dominant knees: OA seen in 66.6% players and 46.7% controls (p=0.081) Non-dominant knees: OA seen in players 66.6% vs 43.3% controls (p=0.028) Most was “mild/moderate” OA |
| Arliani, 2006 | Former male professional footballers aged 30-55 years | 16 cases / 21 controls (matched for age) | Previous injury EXCLUDED | Knee MRI scans* | More changes of osteoarthritis in knee MRI scans of former players than controls |
| Elleuch, 2008 | Former top level soccer aged >45 years | 50 cases /50 controls | |||
| (groups matched for age, BMI, % of axis deviation knee) | Previous surgery and injury EXCLUDED | X-rays (K&L III and IV) | 40/50 footballers (80%) had radiographic knee OA as compared with 34/50 controls. Rates of radiographic knee OA (K&L III, IV) 57.5% vs 29.4% in controls (p=0.05) |
||
| Fernandes, 2018 | Male ex-professional footballers | 1207 cases (25% response) /4085 controls (24% response) AND 470 cases and 491 controls had X-rays | Previous “severe injury” 64.5% ex-footballers and 23.3% controls – adjusted for in Model 2 of paper | X-rays scored by NLDA method and K&L (III or IV) | NLDA: (adjusted for age, BMI) OR 2.21, (95% CI 1.92-2.54) K&L: (adjusted for age, BMI) OR 2.46, (95% CI 1.89-3.22) NLDA: (adjusted for age, BMI, injury) OR 1.91, (95% CI 1.65-2.22) K&L: (adjusted for age, BMI, injury) OR 2.10, (95% CI 1.58-2.80) |
| Iosifidis, 2013 | Former elite male athletes aged > 40 years | 121 soccer players out of 218 athletes, 181 controls | Excluded if had previous knee injury | X-rays (K&L II, III and IV) | Radiographic knee OA more common in former athletes than controls (35% vs. 21%, p=0.048) No difference in prevalence of radiographic OA amongst soccer players compared with other athletes. |
| Kujits, 1995 | Former runners, weight lifters, shooters and soccer players aged 45-88 years | 117 (31 soccer players) | Acute injury aged < 40 taken into analysis | X-rays scored by K&L (K&L II, III, IV) | Risk of radiographic knee OA after knee injury OR 4.73, 95% CI 1.32-17.0 Risk of radiographic knee OA related to soccer playing OR 5.21, 95% CI 1.14-23.8 |
| Lv 2017 | Professional footballers aged 45-70 years | 86/86 matched controls (age, weight, height, BMI) | Excluded if had previous knee injury | X-rays scored by K&L (K&L II, III, IV) | Radiographic knee OA rarer in former footballers (15.1% vs. 45.3%) (p<0.001) |
| Paxinos, 2017 | Veteran retired soccer players vs. veteran military personnel now aged 35-55 years | 100 soccer players /100 military | 32% of ex-soccer players had surgery to their knee and 17% of ex-military | Ultrasound knees* | 52% of ex-soccer players vs. 33% of ex-military had ultrasound evidence of OA changes (p=0.10) After excluding those with history of injury, 44.1% vs. 25.3% (p=0.10) |
| Roos, 1994 | Former male soccer players > 40 years | 215 non-elite and 71 elite players /572 age-matched controls | History of meniscectomy and ACL recorded | Where X-rays had been carried out as part of “routine” care, (24% of controls and 39% of players) they were reviewed for JSN by Ahlback criteria | 11% elite soccer players without history of meniscectomy or ACL had prevalent JSN as compared with 3% controls NB Could be bias/confounding by indication for X-rays |
| Thelin 2006 | Cases were diagnosed on X-ray with advanced OA or found to have had surgery for OA | 825 cases knee OA / 825 controls matched for age, sex, residential area | Injury adjusted for | Had arthroplasty or similar surgery for knee OA or advanced OA on X-rays | Risk of knee OA amongst cases (adjusted for smoking, BMI, family history, type of occupation) OR 1.52, 95% CI 1.04-2.02 After adjustment as above AND for injury, OR 0.94, 95% CI 0.61-1.44 |
29. Table 2 summarises the findings of the 10 studies which examined the risk of clinical OA, self-reported “physician diagnosed” OA, arthroplasty, or pain or dysfunction attributed to the knee, attempting to control for injury. Researchers assessed different outcomes using different tools, and here again, the results appear conflicting. One study reported rates of “clinical OA” but found no difference in the risk between cases as compared with controls [Iosifidis]. Three studies investigated the risk for self-reported “physician diagnosed” arthritis [Kettunen, Fernandes, Tveit]. Kettunen et al reported increased risks of “physician diagnosed” OA amongst team sport players, especially in younger participants, but could not find a doubling of risk after adjustment for age, BMI, or occupation (but not injury). Tveit et al showed that “soft tissue knee injuries” were common amongst former athletes and showed that “physician diagnosed” OA was more common in former athletes but only with an estimated 52% level of increased risk. After adjustment for age, BMI, occupation and soft tissue injuries, the risk of knee OA was 1.13, 95% CI 0.75-1.72.
Table 2 Summary of studies that excluded, or adjusted for, injuries and presented clinical OA, symptomatic OA or arthroplasty risk
| Author | Comparators | Numbers | Injury | Case definition (clinical, self-reported or arthroplasty) | DISABILITY: Pain, function, HRQoL | Findings |
|---|---|---|---|---|---|---|
| Arliani 2014 | Former male professional footballers 30-55 years old | 27 cases /30 controls (non-sportsmen matched for age and previous injury) | “Matched for injury” but apparent imbalance of meniscectomy cases and ACL cases. 9/30 controls had surgery whilst 11/27 cases had surgery | KOOS SF-36 Knee pain, VAS |
Former players had poorer scores on SF-36 (physical domain), p=0.005 On the KOOS, former players had more pain (p=0.005), more knee symptoms (p=0.002) and poorer knee-related quality of life (p=0.027) On the pain VAS, former players scored median 3 cm (IQR 2-5) whilst controls scored median 0 (p=0.001) |
|
| Arliani, 2006 | Former male professional footballers aged 30-55 years | 16 cases / 21 controls (matched for age) | Previous injury excluded | KOOS SF-36 Knee pain (VAS) |
Former players had poorer scores on SF-36 physical domain, (p=0.003) and vitality (p=0.04) On the KOOS, former players had more pain (p=0.035), more knee symptoms (p=0.006) and poorer knee-related quality of life (p=0.007) On the pain VAS, former players scored median 3.2 cm (IQR 1-5) whilst controls scored median 0 (p=0.005) |
|
| Elleuch, 2008 | Former top level soccer aged >45 years | 50 cases /50 controls | Previous surgery and injury excluded | Function (Lequesne score) Pain (VAS) | Only 6/40 footballers reported knee pain, mean score 25.4 mm (range 15-32mm). Knee pain was reported by 17 controls, mean score 39.2 mm (range 25-55 mm) (p=0.01) Only the same 6 footballers reported disability, mean Lequesne score 0.38 +/-1.27. Disability was seen in 23 controls, mean Lequesne score 1.71, +/- 3.2, (p=0.05) |
|
| Fernandes, 2018 | Male ex-professional footballers | 1207 cases (25% response) /4085 controls (24% response) AND 470 cases and 491 controls had X-rays | Previous “severe injury” 64.5% ex-footballers and 23.3% controls – adjusted for in Model 2 of paper | Total knee arthroplasty Self-reported “physician-diagnosed” knee OA |
Knee pain (VAS) | Ex-footballers were more likely to have had knee arthroplasty (11.1% vs 3.8%) (adj RR (age, BMI) 3.61, 95% CI 2.90-4.50) More ex-footballers reported “physician diagnosed” knee OA (28.3% vs 12.2%) (adj RR (age, BMI) 3.73, 95% CI 3.33-4.17) Ex-footballers were more likely to have current knee pain (adj RR (age, BMI) 1.91, 95% CI1.77-2.06) Ex-footballers were more likely to have had knee arthroplasty (adj RR (age, BMI, injury) 2.33, 95% CI 1.85-2.94) More ex-footballers reported “physician diagnosed” knee OA (adj RR (age, BMI, injury) 2.69, 95% CI 2.36-3.07) Ex-footballers were more likely to have current knee pain (adj RR (age, BMI, injury) 1.48, 95% CI 1.38-1.63) |
| Iosifidis, 2013 | Former elite male athletes aged > 40 years | 121 soccer players out of 218 athletes, 181 controls | Excluded if had previous knee injury | Clinical OA: Joint pain or disability in the past year plus one clinical sign of OA | Prevalence of clinical OA in former elite athletes (including soccer players) 15.6% vs 14.4% in controls (NSIG) No difference in prevalence of clinical OA for soccer players as compared with other athletes |
|
| Kettunen, 2001 | Former elite male athletes who represented Finland 1920-65 | 1321 cases /814 controls “healthy at aged 20 years” | Disability compared for those with/without history of knee injuries affecting ligaments or menisci | Self-reported “physician diagnosed” OA | Knee pain at least monthly past year Knee disability past year | Subjects with knee ligament or meniscal injuries reported more knee disability (29.5%, 95% CI 24.5% -34.6%) compared with those without (7.7%, 95% CI 6.0-9.6%) (p<0.001). Compared with control subjects, the age-adjusted risk for physician-diagnosed knee osteoarthritis before the age of 45 was significantly higher among team sport athletes (OR 2.92; 95% CI, 1.49-5.73; P=0.01) After adjustment for age, BMI and occupational load (but not injury), “team sports players” (including soccer, hockey and basketball players) have a higher risk of knee disability than controls (OR 1.76, 95% CI 1.03-3.02) |
| Lv 2017 | Professional footballers aged 45-70 years | 86/86 matched controls (age, weight, height, BMI) | Excluded if had previous knee injury | Hospital for Special Surgery Score (HSS) Iowa Knee Score (IKS) | Ex-footballers had better HSS scores than controls (93, 85-93 vs. 70, 50-77), p<0.001 Ex-footballers had better IKS scores than controls (87, 82-87 vs. 66, 47-73), p<0.001 |
|
| Paxinos, 2017 | Veteran retired soccer players vs. veteran military personnel now aged 35-55 years | 100 soccer players /100 military | 32% of ex-soccer players had surgery to their knee and 17% of ex-military | KOOS | No difference between groups for KOOS domains: symptoms; activities of daily living; sport; quality of life. Soccer players had less knee pain on KOOS than military controls (p=0.03) |
|
| Sandmark, 1999 | Cases who underwent total knee arthroplasty for tibio-femoral OA drawn from surgical register | 325/264 men and 300/284 women | Prior trauma or surgery were EXCLUDED as cases or controls | Tibio-femoral OA needing arthroplasty | Higher risk of being a male case if exposed to soccer (RR 2.0) (similar to results for cross-country skiing and ice hockey) but higher occupational physical exposures such as lifting also increased the risk. Some suggestion of exposure-response relationship and more marked impact on risk of surgery at younger ages (55-64 years) | |
| Tveit, 2012 | Former male elite athletes aged 50-93 years | 709 cases (74% response) / 1368 controls (64% response) | Recalled “soft tissue knee injuries” | Self-reported knee arthroplasty | Self-reported “physician diagnosed” OA | Soft tissue knee injury was reported in 245 (36.1%) former athletes and 332 (25.2%) controls (P<0.001) Self-reported “physician diagnosed” knee OA was reported by 129 (19.4%) former athletes and 163 (13.0%) controls (p<0.001) (52% higher risk on soccer players) Self-reported knee arthroplasty was reported by 24 (3.6%) former athletes and 30 (2.4%) controls (p=0.12 NSIG) After adjustment for age, BMI, occupational load and soft tissue injuries, no elevated risk found for knee OA (OR 1.13, 95% CI 0.75-1.72) or knee arthroplasty (OR 1.21, 95% CI 0.38-3.84). |
30. Three studies reported that soccer players are no worse off (or even in some cases better off) than controls for current knee pain/function [Elleuch, Lv, Paxinos]. In contrast, Kettunen found higher disability scores reported by former athletes as compared with controls, but these rates were less than doubled (OR 1.76, 95% CI 1.03-3.02). However, three others used similar measures and found that ex-soccer players had significantly worse pain/function than controls [Arliani, Fernandes]. Fernandes and colleagues reported that the risk of knee pain was 1.91-fold increased (after adjusting for age and BMI) but there may be bias in pain reporting as the footballers also reported higher levels of “bodily pain” than the controls. This study also had a poor response rate, increasing the risk of responder bias. Where arthroplasty was the outcome, two studies suggested an increased risk amongst ex-players [Fernandes, Sandmark] and both suggested that this risk was more than doubled. However, after adjustment for age, BMI, occupational load and soft tissue knee injuries, Tveit found no significantly increased risk of this outcome associated with former athletes (OR 1.21, 95% CI 0.38-3.84).
Evidence from Systematic Reviews
31. Four relevant systematic reviews have been identified [Kuijt, Spahn, Tran, Driban]. Driban et al reviewed the evidence for an increased risk of OA amongst former male elite or professional athletes. They were able to include 17 papers, 6 of which involved soccer players. The authors concluded that the ways in which papers “controlled” for injury were markedly heterogeneous with no consistency of what was defined as injury (acute, severe, leading to hospital treatment, needing surgery, leading to time out of training etc.). Despite this, they reported a high rate of radiographic knee OA among soccer players (elite 7.6%, non-elite 2.3% with a crude OR of 3.47 as compared with non-soccer players). They also commented that uninjured non-elite soccer players had a higher prevalence of knee OA than non-soccer players (OR 3.75, 95% CI 1.46-9.64). They reflected however that these risk assessments were likely to be confounded with lack of control for level of play and injury.
32. Tran and colleagues undertook a systematic review and meta-analysis of the risk of OA in sports, comparing elite and non-elite sportspeople [Tran]. They reported that the evidence was very low quality and that there was evidence of publication bias. They reflected on the diversity of methods of diagnosis of OA (radiographic, clinical etc.) and that 1:4 studies failed to explain fully their method of diagnosis of OA. However, they concluded that there was very low-quality evidence to suggest that soccer, especially elite soccer, “may increase the risk of OA”.
33. Kuijt focused on studies of former elite soccer players only and could only include 4 papers, two reporting on radiographic OA and two reporting on clinical OA [Kuijt]. They concluded that two “high quality” studies estimated an increased risk of radiographic OA 60-80% and two “moderate quality” studies found an increased risk of self-reported “physician-diagnosed” OA 40-46%.
34. Spahn et al (only published in German) undertook a systematic review and meta-analysis of the risk of knee OA in soccer players. They only included papers which attempted to control for the effect of knee injuries and identified 6 such papers. They concluded that, after adjustment for the effect of injuries, the risk of knee OA was not established (OR 1.3, 95% CI 1.0-1.7) and that there was currently insufficient evidence that OA knee was an “occupational disease”.
Assessment of Bias and Confounding
35. The literature on this topic is very heterogeneous. Knee OA is recognised to be associated generally with key risk factors (age, gender, BMI) which were, for the most part, controlled for, or adjusted for, by the authors. Occupational factors, including kneeling and squatting, are also recognised risk factors and more modern studies have made some adjustment for these before reporting their estimates of risk associated with football. This is particularly important as many ex-professional footballers either remain in the sport (coaching, training) or move to other non-sedentary manual occupations.
36. The more recently published papers have attempted, to a greater or lesser extent, to consider the effect of previous knee injuries in their analyses. As discussed in the systematic review by Lohkamp and colleagues however, the field is currently hampered by a lack of agreement as to how to define injuries [Lohkamp]. For the most part, injuries resulting in surgery or recognised internal derangement (ligamentous or meniscal) are being better recorded and controlled for but undoubtedly, during a career of 10-15 years of playing >200 hours of competitive matches, footballers will have many “knocks” to their knees and there are currently very limited ways of exploring the effect of repeated cumulative mild trauma.
37. Furthermore, there are likely to be other factors which are currently unknown but could also be significant confounders. For example, the Council found only one paper which discussed the use of knee injections amongst footballers in their sample [Arliaini]. The paper reported that 44% of 27 footballers had received knee joint injections, a mean of 5 times each. In practice, most knee injections would involve a combination of corticosteroid mixed with local anaesthetic. Animal studies have suggested the potential for high and frequent doses of intra-articular slightly soluble corticosteroids to produce alterations in ligament strength and function, reducing the maximum failure load [Noyes] and hypothetically, at least, this may mean that some treatments if used more frequently in footballers, may be at least partly explain the variation.
Conclusions
38. Overall, there have been more, better quality, studies published since the Council last reviewed this topic. In particular, more investigators have sought to understand whether and to what extent there is a risk of OA associated with playing professional football that is separate from the risk associated with traumatic injury. The Council have reviewed these studies in considerable detail. However, this research is being hampered by the lack of consensus methods to describe injury characteristics and the fact that many studies rely on recall of past injuries. Studies of ‘radiographic’ OA produce significantly higher risk estimates of the risk of OA but this is of limited relevance to the Council. The data for self-reported “physician diagnosed” OA are inconsistent and are open to misclassification. Two from three studies suggested a doubling of the risk of knee arthroplasty but the third found no risk associated. There is inconsistency around pain and function attributable to the knees later in life. The one recent high-quality UK study [Fernandes] contributes importantly to this literature but itself suffered from only 25% questionnaire response amongst former footballers and even lower rates of participation in X-ray examination, which makes it difficult to exclude a response bias whereby those with knee problems were more likely to participate.
Recommendations
39. Taken together therefore, the Council does not find enough consistent evidence that the risk of knee OA is doubled amongst football players in the absence of a traumatic knee injury. As a result, the Council is currently therefore unable to recommend prescription for former professional football players without evidence of traumatic knee injury. The Council does however encourage ex-professional footballers who had a documented knee injury during their playing career, and later developed osteoarthritis in that knee, to consider making a claim under the accident provision of IIDB. The Council has been assured that there is no restriction in the time frame over which such a claim can be made in relation to the current disability and the past injury.
40. Moreover, the Council remains committed periodically to updating its appraisal of the evidence-base on work and knee OA. It would be pleased at any time to receive new evidence, both on risks of the disease by occupational title and on representative information on exposures to knee-straining activity by occupational title in Britain. Both types of evidence may in future serve to strengthen the arguments for extending the terms of PD A14.
Prevention
41. Although many risk factors for osteoarthritis have been identified, it is not currently possible to prevent osteoarthritis altogether. However, professional footballers may be able to reduce their particular risk of developing osteoarthritis of the knee. Since the development of knee osteoarthritis in footballers is linked to knee injury, it is possible that reducing the risk of injury may also reduce the likelihood of developing knee osteoarthritis. FIFA has developed a training programme (FIFA 11+), which has been shown to reduce the risk of lower limb injuries. Therefore, if managers and trainers implement the FIFA 11+ programme, it has the potential to help reduce the number of football players developing knee osteoarthritis.
References
Ahlbäck S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Stockholm 1968; (suppl 277):7-72.
Altman RD, Block DA, Brandt KD, Cooke DV, Greenwald RA, Hochberg MC, Howell DS, Ike RW, Kaplan D, Koopman W, et al. Osteoarthritis: definitions and criteria. Ann Rheum Dis. 1990;49:201.
Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national health and nutrition examination survey (Hanes I). Evidence for an association with over- weight, race, and physical demands of work. Am J Epidemiol 1998;128:179-89.
Arliani GG, Astur DC, Yamada RK, Yamada AF, Miyashita GK, Mandelbaum B, Cohen M. Early osteoarthritis and reduced quality of life after retirement in former professional soccer players. Clinics (Sao Paulo). 2014;69:589-94.
Arliani GG, Astur DC, Yamada RK, Yamada AF, da Rocha Corrêa Fernandes A, Ejnisman B, de Castro Pochini A, Cohen M. Professional football can be considered a healthy sport? Knee Surg Sports Traumatol Arthrosc. 2016;24:3907-3911
Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord 2008; 9: 116.
Coggon D, Croft P, Kellingray S et al. Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum 2000;43:1443-9.
Cooper C, McAlindon T, Coggon D et al. Occupational activity and osteoarthritis of the knee. Ann Rheum Dis 1994;53:90-3.
Danielsson L, Hernborg J. Clinical and roentgenologic study of knee joints with osteophytes. Clin Orthop Relat Res. 1970;69:302-12.
Dawson J, Juszczak E, Thorogood M et al. An investigation of risk factors for symptomatic osteoarthritis of the knee in women using a life course approach. J Epidemiol Community Health 2003;57:823-30.
Deacon A, Bennell K, Kiss ZS, Crossley K, Brukner P. Osteoarthritis of the knee in retired, elite Australian Rules footballers. MJA 1997;166:187-90.
Department for Work and Pensions. Sporting injuries. Position paper 15, London, The Stationery office, 2005
Department for Work and Pensions. Osteoarthritis of the Knee in Carpet Fitters and Carpet and Floor Layers. Cm 7964, London, The Stationery Office, 2010.
Department for Work and Pensions. Osteoarthritis of the Knee in Coal Miners. Cm 7440, London, The Stationery Office, 2008.
Drawer S, Fuller CW. Evaluating the level of injury in English professional football using a risk based assessment process. Br J Sports Med. 2002;36:446-51.
Driban JB, Hootman JM, Sitler MR, Harris KP, Cattano NM. Is Participation in Certain Sports Associated With Knee Osteoarthritis? A Systematic Review. J Athl Train. 2017;52:497-506.
Elleuch MH, Guermazi M, Mezghanni M, Ghroubi S, Fki H, Mefteh S, Baklouti S, Sellami S. Knee osteoarthritis in 50 former top-level soccer players: a comparative study. Ann Readapt Med Phys. 2008;51:174-8.
Felson DT, Hannan MT, Nalmark A et al. Occupational physical demands, knee bending, and knee osteoarthritis: results from the Framingham study. J Rheumatol 1991;18:1587-92.
Fernandes GS, Parekh SM, Moses J, Fuller C, Scammell B, Batt ME, Zhang W, Doherty M. Prevalence of knee pain, radiographic osteoarthritis and arthroplasty in retired professional footballers compared with men in the general population: a cross-sectional study. Br J Sports Med. 2018;52:678-683.
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1545–602
Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired national football league players. J Phys Activity & health 2009;6:638-43.
Gouttebarge V, Aoki H, Kerkhoffs GMMJ. Knee osteoarthritis in professional football is related to severe knee injury and knee surgery. Inj Epidemiol. 2018;5:26.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet 2019; 393:1745-59.
Iosifidis MI, Tsarouhas A, Fylaktou A. Lower limb clinical and radiographic osteoarthritis in former elite male athletes. Knee Surg Sports Traumatol Arthrosc. 2015;23:2528-35
Jensen LK, Mikkelsen S, Loft IP et al. Radiographic knee osteoarthritis in floorlayers and carpenters. Scand J Work Environ Health 2000;26:257-62.
Jensen KJL. Knee-straining work activities, self-reported knee disorders and radiographically determined knee osteoarthritis. Scand J Work Environ Health 2005;31:68-74.
Kellgren J, Lawrence J. Radiologic assessment of osteoarthritis. Annals of the Rheumatic Diseases 1957;16:494-501
Kettunen JA, Kujala UM, Kaprio J, Koskenvuo M, Sarna S. Lower-limb function among former elite male athletes. Am J Sports Med. 2001;29:2-8
Kuijt MT, Inklaar H, Gouttebarge V, Frings-Dresen MH. Knee and ankle osteoarthritis in former elite soccer players: a systematic review of the recent literature. J Sci Med Sport. 2012;15:480-7
Kivimaki J, Riihimaki H, Hanninen K. Knee disorders in carpet and floor layers and painters. Scand J Work Environ Health 1992;18:310-6.
Krajnc Z, Vogrin M, Recnik G, Crnjac A, Drobnic M, Antolic V. Increased risk of knee injuries and osteoarthritis in the non-dominant leg of former professional football players.Wien Klin Wochenschr. 2010 May;122 Suppl 2:40-3.
Kujala UM, Kettunen J, Paananen H, Aalto T, Battié MC, Impivaara O, Videman T, Sarna S. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arthritis Rheum. 1995;38:539-46
Lau EC, Cooper C, Lam D et al. Factors associated with osteoarthritis of the hip and knee in Hong Kong Chinese: obesity, joint injury, and occupational activities. Am J Epidemiol 2000;152:855-62.
Lohkamp M, Kromer TO, Schmitt H. Osteoarthritis and joint replacements of the lower limb and spine in ex-professional soccer players: A systematic review. Scand J Med Sci Sports. 2017;27:1038-1049
Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequences of anterio cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35:1756-69.
Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145-52.
Lv H, Chen W, Yuwen P, Yang N, Yan X, Zhang Y. Multivariate analysis of factors related to radiographic knee osteoarthritis based on the comparison between football players and matched nonsportsmen. Int Orthop. 2018;42:519-527
Manninen P, Heliovaara M, Riihimaki H et al. Physical workload and the risk of severe knee osteoarthritis. Scand J Work Environ Health 2002;28:25-32.
Muthuri SG, McWilliams DF, Doherty M, Zhang W. History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthritis Cartilage 2011;19: 1286-93.
Nagaosa Y, Mateus M, Hassan B, Lanyon P, Doherty M. Development of a logically devised line drawing atlas for grading of knee osteoarthritis. Ann Rheum Dis. 2000; 59:587-95
See National Joint Registry 15th Annual Report 2018 (accessed Aug 2019)
Neyret P1, Donell ST, DeJour D, DeJour H. Partial meniscectomy and anterior cruciate ligament rupture in soccer players. A study with a minimum 20-year followup. Am J Sports Med. 1993;21:455-60.
Noyes FR, Grood ES, Nussbaum NS, Cooper SM. Effect of intra-articular corticosteroids on ligament properties: a biomechanical and histological study in rhesus knees. Clin Orthop Relat Res. 1977;(123):197-209.
Palmer KT. Occupational activities and osteoarthritis of the knee. British Medical Bulletin 2012;102:147-70.
Paxinos O, Karavasili A, Delimpasis G, Stathi A. Prevalence of Knee Osteoarthritis in 100 Athletically Active Veteran Soccer Players Compared with a Matched Group of 100 Military Personnel. Am J Sports Med. 2016;44:1447-54.
Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage 2011; 19: 1270–85.
Roos H, Lindberg H, Gärdsell P, Lohmander LS, Wingstrand H. The prevalence of gonarthrosis and its relation to meniscectomy in former soccer players. Am J Sports Med. 1994;22:219-22
Salzmann GM, Preiss S, Zenobi-Wong M, Harder LP, Maier D, Dvorak J. Osteoarthritis in football: with a special focus on knee joint degeneration. Cartilage 2017;8:167-72.
Sandmark H, Vingård E. Sports and risk for severe osteoarthrosis of the knee. Scand J Med Sci Sports. 1999;9:279-84
Sandmark H. Musculoskeletal dysfunction in physical education teachers. Occup Environ Med 2000;57:673-7.
Sandmark H, Hogstedt C, Vingard E. Primary osteoarthrosis of the knee in men and women as a result of lifelong physical load from work. Scand J Work Environ Health 2000;26:20-5.
Schouten JSAG, van den Ouweland FA, Valkenburg HA. A 12 year follow up study in the general population of prognostic factors of cartilage loss in osteoarthritis of the knee. Ann Rheum Dis 1992;51:932-7.
Seidler A, Bolm-Audorff U, Abolmaali N et al., and the Knee Osteoarthritis Study Group. The role of cumulative physical work load in symptomatic knee osteoarthritis – a case-control study in Germany. J Occup Med Toxicol 2008;3:14.
Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage 2015; 23: 507–15.
Spahn G, Grosser V, Schiltenwolf M, Schröter F, Grifka J. Football as risk factor for a non-injury-related knee osteoarthritis - results from a systematic review and metaanalysis.[Article in German] Sportverletz Sportschaden. 2015;29:27-39.
Thelin N, Homberg S, Thelin A. Knee injuries account for the sports-related increased risk of knee osteoarthritis. Scand J Med Sci Sports 2006; 16:329-33.
Tran G, Smith TO, Grice A, Kingsbury SR, McCrory P, Conaghan PG. Does sports participation (including level of performance and previous injury) increase risk of osteoarthritis? A systematic review and meta-analysis. Br J Sports Med. 2016;50:1459-1466
Turner AP, Barlow JH, Heathcote-Elliott C. Long term health impact of playing professional football in the United Kingdom.Br J Sports Med. 2000 Oct;34(5):332-6. Tveit M, Rosengren BE, Nilsson JÅ, Karlsson MK. Former male elite athletes have a higher prevalence of osteoarthritis and arthroplasty in the hip and knee than expected. Am J Sports Med. 2012;40:527-33.
Vingard E, Alfredsson L, Fellenius E et al. Disability pensions due to musculoskeletal disorders among men in heavy occupations. Scand J Soc Med 1992;20:31-6.
Vingard E, Alfredsson L, Goldie I et al. Occupation and osteoarthrosis of the hip and knee: a register-based cohort study. Int J Epidemiol 1991;20:1025-31.
Von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269-73.
Zhang W, Doherty M. EULAR recommendations for knee and hip osteoarthritis: a critique of the methodology. Br J Sports Med. 2006;40:664-9.
Glossary
Types of study
Case control study: A study which compares people who have a given disease (cases) with people who do not (non-cases, also called controls) in terms of exposure to one or more risk factors of interest. Have cases been exposed more than non-cases? The outcome is expressed as an Odds Ratio, a form of Relative Risk.
Cohort study: A study which follows those with an exposure of interest (usually over a period of years), and compares their incidence of disease or mortality with a second group, who are unexposed or exposed at a lower level. Is the incidence rate higher in the exposed/more exposed workers than the unexposed/less exposed group? Sometimes the cohort is followed forwards in time (‘prospective’ cohort study), but sometimes the experience of the cohort is reconstructed from historic records (‘retrospective’ or ‘historic’ cohort study). The ratio of risk in the exposed relative to the unexposed can be expressed in various ways, such as a Relative Risk, or Standardised Mortality Ratio.
Cross-sectional study: A study which classified people at a point in time as having a given disease (or characteristic) or not (controls), and then compares them in terms of exposure to one or more risk factors of interest. Is disease more frequent in those with exposure than in those without? The outcome can be expressed as an Odds Ratio, Prevalence Ratio or Relative Risk.
Measures of association
Statistical significance and P values: Statistical significance refers to the probability that a result as large as that observed, or more extreme still, could have arisen simply by chance. The smaller the probability, the less likely it is that the findings arise by chance and the more likely they are to be ‘true’. A ‘statistically significant’ result is one for which the chance alone probability is suitably small, as judged by reference to a pre-defined cut-point. (Conventionally, this is often less than 5% (P<0.05)).
Relative Risk (RR): A measure of the strength of association between exposure and disease. RR is the ratio of the risk of disease in one group to that in another. Often the first group is exposed and the second unexposed or less exposed. A value greater than 1.0 indicates a positive association between exposure and disease. (This may be causal, or have other explanations, such as bias, chance or confounding.)
Odds Ratio (OR): A measure of the strength of association between exposure and disease. It is the odds of exposure in those with disease relative to the odds of exposure in those without disease, expressed as a ratio. For rare exposures, odds and risks are numerically very similar, so the OR can be thought of as a Relative Risk. A value greater than 1.0 indicates a positive association between exposure and disease. (This may be causal, or have other explanations, such as bias, chance or confounding.)
Other epidemiological terms
Confidence Interval (CI): The Relative Risk reported in a study is only an estimate of the true value in the underlying population; a different sample may give a somewhat different estimate. The CI defines a plausible range in which the true population value lies, given the extent of statistical uncertainty in the data. The commonly chosen 95%CIs give a range in which there is a 95% chance that the true value will be found (in the absence of bias and confounding). Small studies generate much uncertainty and a wide range, whereas very large studies provide a narrower band of compatible values.
Confounding: Arises when the association between exposure and disease is explained in whole or part by a third factor (confounder), itself a cause of the disease, that occurs to a different extent in the groups being compared.
For example, smoking is a cause of lung cancer and tends to be more common in blue-collar jobs. An apparent association between work in the job and lung cancer could arise because of differences in smoking habit, rather than a noxious work agent.
Studies often try to mitigate the effects of (‘control for’) confounding in various ways such as: restriction (e.g. only studying smokers); matching (analyzing groups with similar smoking habits); stratification (considering the findings separately for smokers and non-smokers); and mathematical modelling (statistical adjustment). March 2020
Industrial Injuries Advisory Council
Dr L Rushton, OBE, BA, MSc, PhD, CStat, Hon FFOM (Chair)
Professor R Agius, MD, DM, FRCP, FRCPE, FFOM
Professor K Burton, OBE PhD Hon FFOM
Professor J Cherrie, CFFOH
Mr K Corkan, BA
Ms L Francois, MA, LLM
Dr M Henderson, MSc, PhD, MRCP, MRCPsych, HonFFOM
Dr J Hoyle, MD, FRCP, MRCPE
Dr S Khan, BMedSci, FFOM, FRCGP, FRCP, DM
Dr I Lawson, MB, BS, FFOM, FRCP
Ms K Mitchell, LLB
Professor N Pearce, BSc, DipSci, DipORS, PhD, DSc
Mr D Russell, BSc (Hons), MSc, CMIOSH
Mr D Shears, BA(Hons)
Dr C Stenton, BSc, MB, BAO, FRCP, FFOM, FFOM.RCPI
Professor K Walker-Bone, BM, FRCP, PhD, Hon FFOM
Dr A White, BSc (Hons), PhD, CMIOSH, AIEMA
Former Council Members
Dr V Gallo, MD LSHTM-MSc PhD
Mr H Robertson
HSE Observer
L Darnton
IIAC Secretariat
Secretary Mr S Whitney
Scientific Advisor Mr I Chetland
Administrative Secretary Ms C Hegarty
