Diabetic eye screening HEA example
Updated 24 September 2020
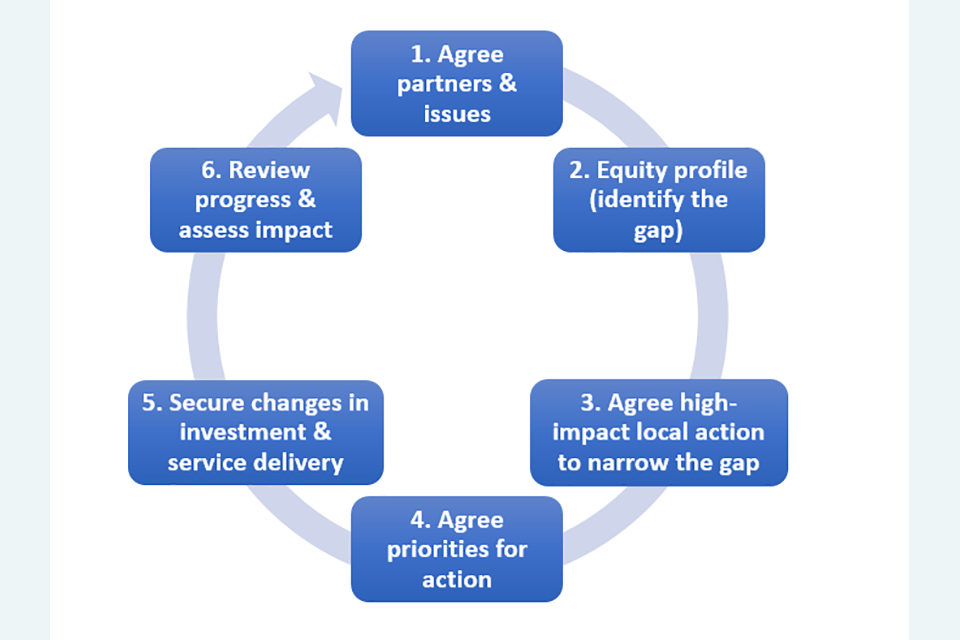
Figure 1: the Health Equity Audit cycle (Health Development Agency, 2005)
Figure 1 above shows the Health Equity Audit cycle, consisting of 6 stages:
- Agree partners and issues.
- Equity profile (identify the gap).
- Agree high-impact local action to narrow the gap.
- Agree priorities for action.
- Secure change in investment and service delivery.
- Review progress and assess impact.
The following illustrative example from a diabetic eye screening health equity audit (HEA) has been divided into the 6 stages of the HEA cycle.
Links have also been provided to the HEA guide for screening providers and commissioners to illustrate sections of relevance.
1. Agree on partners and issues
The aim was to identify inequities relating to the invitation, uptake, attendance at screenings and onward referral by the South East London Diabetic Eye Screening Service.
It looked at individuals aged 12 years and older, registered with GPs covered by the 6 South East London clinical commissioning groups (CCGs) over a 12-month period.
Individuals were deemed eligible for screening if they were recorded on their GP database as having diabetes mellitus.
Excluded individuals were those who had been excluded from screenings or those who had diabetes mellitus but were not registered with a GP.
Scope: acknowledge and accept limitations rather than delay the HEA. This includes the inability to identify the unregistered population with diabetes mellitus, or those with diabetes mellitus but not coded or undiagnosed.
Preparing: consider target population, inclusion and exclusion criteria, geographical catchment and aims of the screening programme.
2. Equity profile
This audit looked at whether age, sex, ethnicity, deprivation, mental health status, ambulatory status, diabetes type, need for an interpreter, use of text messaging, CCG, registered GP and provider of screening resulted in inequity.
Quantitative analysis and qualitative analysis was carried out with stakeholders including a commissioner, GP with a special interest in diabetes mellitus, programme manager and service user.
There was significant variation in uptake by the GP practice, CCG and screening location and significant inequity in screening attendance associated with deprivation.
There were high levels of missing data for mental health and ambulatory status.
Health inequalities across the screening pathway:
- Cohort identification (via GP systems).
- Provision of information about screening measured by need for an interpreter.
- Access to services measured by ambulatory status.
- Outcomes, which in this audit meant a referral to ophthalmology.
Data and evidence: sources of data.
3. Agree on high-impact local action to narrow the gap
The HEA contributed to existing valuable workstreams that aimed to reduce inequities in uptake and provision.
High and low-performing GP practices were paired to improve performance.
Screening capacity issues relating to lower screening invitations were addressed.
Communication with CCGs with low uptake was improved.
Data and evidence: use local intelligence including qualitative data to address any identified inequities.
4. Agree on priorities for action
A rapid review of published literature aimed to identify evidence-based interventions that may reduce inequalities in screening.
Data and evidence: rapid reviews of what has worked to address inequalities identified.
5. Secure changes in investment and service delivery
Develop protocols for data extraction and quantitative analyses so that future HEAs can be conducted more quickly.
Determine if more systematic ways of routinely collecting data related to mental health, ambulatory status and interpreter needs can be developed.
Implementation, evaluation and feedback: in this audit, designing IT systems to routinely collect data that would be useful to identify and address inequalities.
6. Review progress and assess the impact
Annual review of recommendations was agreed.
Recommendations included in service improvement plan which is reviewed at quarterly programme boards.
