Mental health and loneliness: the relationship across life stages
Published 12 June 2022
Executive summary
This report presents the findings from a qualitative study exploring the experiences of loneliness among those who had experienced a mental health condition. Previous research has shown there is a link between experiences of loneliness and poor mental health. The Department for Digital, Culture, Media and Sport (DCMS) commissioned this study to explore this issue across four key life stages as part of developing the evidence base for work on tackling loneliness.
The study aimed to explore:
- how those with diagnosed mental health problems experience loneliness
- the extent to which social stigma associated with mental health conditions plays a role in experience of loneliness
- how experiences of loneliness among those who have experienced mental health conditions vary by life stage.
The report draws on findings from:
- six interviews with professional expert stakeholders
- 37 in-depth interviews and 14 diaries from those experiencing loneliness who also had a history of mental ill-health
Participants were recruited from one of the following four life stages:
- young adulthood (18 – 30 years old)
- parents of young children (with children aged 5 or under)
- middle aged (40 – 60 years old)
- retired[footnote 1]
Across the sample there were a range of mental health conditions experienced including depression, anxiety, post-traumatic stress disorder, schizophrenia, bi-polar disorder and borderline personality disorder, among others.
The relationship between loneliness and mental health
Participants did not always describe themselves as feeling ‘lonely’. Instead they talked about feeling isolated, alone, or being a loner. Other ways in which participants talked about the lack of connection they felt in their lives was to describe not having anyone they could turn to for emotional support, or feeling like a burden on those they had existing connections with.
Across the sample there was a spectrum of experiences of loneliness. Those who were most lonely described feeling isolated, with no close friends or supportive others. Participants in this group tended to have depression and be in the middle-aged or retired life stages. At the other end of the spectrum, the least lonely people were those with a wider social network, including close connections who provided emotional support. Participants in this group tended to have experienced anxiety and depression and were found across all life stages. For this group, periods of loneliness correlated with poor mental health. In between these groups were people with a few close connections, and a small number of supportive others. However, these social connections were not always able to provide the level of support participants needed.
The relationship between loneliness and mental health was bidirectional and cyclical. Participants described the following ways in which mental health issues could lead to greater feelings of loneliness:
Mental health conditions reduced capacity for social interaction. Low mood could lead to social withdrawal or feeling disconnected from others. Mental health conditions could lead to people simply feeling too exhausted to engage with others. Public spaces for socialising could also feel overwhelming. Participants felt their mental health thwarted their capacity to be supportive to others.
Negative perceptions about themselves or others could lead to withdrawal. Mental health conditions were associated with feelings of low self-esteem and participants worried about the stigma they might experience if they revealed their mental health issues. Certain conditions could also lead to negative perceptions of social relationships, leading to brooding, anger or intolerance of others.
Not being able to share that they were struggling with others, and feeling the need to hide mental health symptoms for fear of being seen as a ‘downer’ could also lead to feelings of loneliness. Maintaining a pretence of being fine when around others was exhausting and unsustainable for participants, leading to them withdrawing from social contact instead.
On the other side, loneliness could also lead to a decline in mental health. This happened where participants had more time alone to ruminate on negative thoughts; where they lost confidence in their ability to socialise, leading to low self-esteem; and where not talking about their feelings led to them feeling even more overwhelmed. This deterioration in mental health could then precipitate further withdrawal and isolation.
Stigma associated with mental ill-health and loneliness clearly affected participants’ ability to be open about their feelings, leading them to also feel less connected to others. Participants experienced stigma associated with both mental ill-health and loneliness, with some elements of both overlapping. Although participants felt that mental ill-health is much more widely talked about than in the past, it was still largely felt to be misunderstood in society. The stigma associated with mental health conditions led to participants internalising negative views that they would be seen as ‘weak’, ‘unreliable’, ‘attention-seeking’, ‘a downer’ or ‘a burden’. On the other hand, the stigma linked to loneliness meant people avoided using the term, feeling that admitting they are lonely meant others would see them as ‘sad’, ‘needy’ or ‘desperate’. Reactions of dismissal or trivialisation when people admitted they were struggling left participants feeling judged or shameful, reinforcing stigma, and sometimes preventing them from seeking help.
Key events across life stages
There were a number of key events across the different life stages that were associated with periods of loneliness or a decline in mental health. Adverse events in childhood or adolescence such as experiences of abuse, neglect, losing a parent or having parents with mental health or substance abuse issues were linked by participants to effects on their mental health in later life. Stakeholders felt that these events could set up patterns of psychological difficulties in later life.
In early adulthood, leaving the family home and the transition to living independently was associated with a risk of loneliness or poor mental health. For participants whose mental health prevented them from working, not having a new social circle through the workplace could lead to feelings of loneliness.
For parents of young children, the increased stress associated with new caring responsibilities sometimes led to poor mental health or increased isolation. The weight of social expectations (for women that they should be able to manage, for men that they should take responsibility for their family) made it difficult to admit they were struggling and to ask for help.[footnote 2] This then fed into feelings of loneliness. Increased loneliness was felt by female participants who experienced fertility issues or pregnancy loss but who felt unable to share with others due to embarrassment.
For those in the middle-age and retirement life stages there were a number of overlaps in the types of experiences or events that led to loneliness. A decline in physical health was associated with increased feelings of loneliness and a deterioration in mental health. People experiencing chronic pain or mobility issues were sometimes no longer able to participate in social activities. For those in middle-age, managing difficult family situations could result in stress, anxiety and feeling overwhelmed. Examples included single parents of children with special educational needs or disabilities, or where fathers were estranged from children. For some single participants, difficulties finding and sustaining intimate relationships took on a greater significance later in life, with some saying they had lost hope of meeting a partner. Changes to work routines – whether redundancy, increased home working, or retirement - could also trigger feelings of loneliness where regular social contact with work colleagues was lost. Finally, experiences of bereavement became more frequent as people aged, and this triggered feelings of loneliness, particularly after the loss of a partner or close family member.
Recommendations for improving support
Participants had accessed a range of support for their mental health through formal health services. These services tended to concentrate on the treatment of mental health symptoms or conditions. There were few examples where services suggested specific support to tackle the loneliness that contributed to poor mental health, with mixed results in this respect. Instead, participants proactively sought out social support to tackle feelings of isolation themselves, through group activities or online interaction.
Participants made a number of recommendations about the way in which support could be improved. These were to:
- provide more local and tailored mental health support services in place of more generic online resources that participants found hard to navigate
- support group activities in communities around shared interests, including those tailored to personal characteristics e.g. faith, disability, gender, or sexual orientation
- provide mental health support that reduces feelings of loneliness and isolation organised around shared interests in activities (e.g. football, crafts, gardening), especially for people diagnosed with specific mental health conditions. These could be made available to people while on waiting lists for treatments
- establish community-based caseworkers who can help people navigate complex mental health services, signpost local support and group activities, and support participants’ families to understand mental health conditions, and how to respond to them.
These recommendations indicate that there could be an important role for the community and voluntary sector to play in supporting people experiencing loneliness and mental health issues. The wider findings of the study suggest that more initiatives to tackle loneliness could help to alleviate some mental health difficulties. These initiatives could be aimed at certain key moments in people’s lives (such as miscarriage, redundancy or retirement) which were associated with an increase in loneliness or deterioration in mental health, but were not associated with existing specialist support services.
Glossary
| ADHD | Attention deficit hyperactivity disorder |
|---|---|
| ASD | Autistic spectrum disorder |
| BAD | Bipolar affective disorder |
| BPD | Borderline personality disorder |
| CBT | Cognitive behavioural therapy |
| DCMS | Department for Digital, Culture, Media and Sport |
| GAD | Generalised anxiety disorder |
| Isolation | Social isolation describes an absence of social contact. This is an objective measure of the number of social contacts a person has |
| Loneliness | A subjective, unwelcome feeling of lack or loss of companionship |
| NatCen | National Centre for Social Research |
| OCD | Obsessive compulsive disorder |
| Participant (research participant) | A person who reported currently being lonely who took part in the research |
| PIP | Personal independence payments |
| PTSD | Post-traumatic stress disorder |
| Purposive sampling | Purposive sampling is an approach to selecting research participants based on characteristics that researchers expect to affect views or experiences on the topic of the study |
| Professional stakeholder | Professionals with expertise in loneliness or mental health who were interviewed as part of the study |
| SAD | Seasonal affective disorder |
1. Introduction
This report presents the findings of a qualitative study commissioned by the Department for Digital, Culture, Media and Sport (DCMS) that aims to understand the relationship between mental health and loneliness across four key life stages: early adulthood (18 – 30 years old); parents with young children (with children aged 5 or under); middle-age (40 – 60 years old) and retirement.[footnote 3] The study forms part of a developing evidence base which will feed into the government’s work on tackling loneliness. This research consisted of two phases: interviews with professional stakeholders who were experts in the field of mental health and/or loneliness, and interviews with people who had past experience of mental health conditions and were experiencing loneliness.
1.1 Background to the research
The issue of loneliness and the need for effective policies to tackle it have been increasingly recognised in recent years. Building on the Jo Cox Commission on Loneliness[pdf], in 2018 the government launched a strategy for tackling loneliness[pdf]. One of the aims of this strategy is to expand the evidence base on loneliness, making a compelling case for action, and ensuring everyone has the information they need to make informed decisions through challenging times. Loneliness is associated with negative physical health outcomes, including earlier deaths, an increased risk of dementia, Alzheimer’s, heart disease and stroke.[footnote 4] Loneliness is also known to have an association with mental health conditions. For example, people reporting loneliness are more at risk of becoming depressed, and depressed people are more at risk of becoming lonely.[footnote 5] The government now recognises loneliness as one of the country’s most pressing public health issues.[footnote 6]
In 2021 DCMS commissioned an evidence review to identify remaining gaps in the existing evidence base. One of the areas noted in the report was a lack of research on the link between mental health and loneliness, as well as gaps in relation to how the stigma associated with mental health affects loneliness. It also recommended that future research explore loneliness across the life course, as well as how experiences of loneliness among key population groups results in poorer mental health.
Although the evidence review has shown that there is an important link between the experience of loneliness and mental health conditions, the nature of the relationship between the two is less well understood, particularly among groups at greater risk of loneliness. The evidence review found a bidirectional link between depression and anxiety and loneliness, and that loneliness is a predictor of worse outcomes in those with depression.[footnote 7]
A 2022 qualitative study found that participants reported a close connection between feelings of loneliness and their mental health difficulties, with poor mental health leading to feeling lonely and loneliness leading to a decline in mental health. Notably, for some participants this was a one-way relationship whilst others found it to be cyclical. The paper emphasised that strategies to reduce loneliness are more likely to be successful if rooted in an understanding of what people with mental health problems mean when they say they are lonely, and how this relates to feelings of mental distress. For instance, they found loneliness was associated with not feeling connected, lacking choice over being alone, not feeling loved, or not feeling understood. They also observed the role that stigma associated with mental health played in not seeking help, and others not providing it.
Certain life stages have also been identified for their heightened risk of loneliness and mental health issues. Much attention has been paid to loneliness in later life[pdf], with older people found to be at greater risk of loneliness, in part due to a perception that it is a part of getting older and not something that can be changed. Adolescence and young adulthood has also been identified as a key life stage at which people may be more likely to experience loneliness. The 2020/2021 Community Life Survey found that 11% of young people report chronic loneliness, compared to 6% of the general population.[footnote 8] This issue has been exacerbated by the COVID-19 pandemic[pdf]. Research has also found that middle age is a time associated with poor mental health, as suicide and attempted suicide are particularly evident among men in the 45-64 age group.
This research thus sought to respond to the evidence gap around experiences of loneliness among groups of concern who had pre-existing mental health conditions. For this research, the groups of concern were young adults, parents with young children, middle-aged people, and retired people.
1.2 Research aims
The overarching aim of the research was to investigate the links between loneliness and mental health, with an interest in different life stages (young adult, parents of young children, middle age, retirement). With this in mind, the research questions we aimed to address were:
- How do those with diagnosed mental health problems experience loneliness?
- To what extent does the social stigma associated with mental health conditions play a role in the experience of loneliness among this group?
- How do experiences of loneliness among those who have experienced mental health conditions vary by life stage?
1.3 Methods
This research consisted of two phases: interviews with professional expert stakeholders and in- depth interviews and diaries with people who were experiencing loneliness and had pre-existing mental health conditions.
1.3.1 Professional stakeholder interviews
In the first stage of the research, six 45-minute interviews were carried out with professional stakeholders. These included experts from mental health charities; organisations that support people at key life stages; and those working specifically on loneliness, including academics. Insights gathered at this stage were used to inform the design of the next phase of research as well as providing expert insights reported throughout this report. Detailed notes from each interview were captured using NatCen’s Framework approach.[footnote 9]
1.3.2 In-depth interviews and diaries
In-depth interviews were conducted with participants who had current or past experience of mental health conditions and currently reported being lonely.[footnote 10] Participants were sampled based on their mental health condition (depression; anxiety; other mental health conditions) and their life stage (young adults; parents of young children; middle-aged; retired). For more details of the sample, methodological approach and ethical considerations, please see Appendix A.
The interviews were conducted over the phone or via video call (depending on participant preference) and were 90 minutes long to allow time to build trust with the participant and fully explore their experiences. 37 interviews were conducted in total. These were then transcribed and analysed using the Framework approach.
14 of the participants who were interviewed also agreed to complete an online diary before their interview. They completed five diary entries documenting their experiences with mental health and loneliness over the course of two weeks. The insights were then used in the interviews to facilitate the discussion and generate richer insights into the fluctuations of feelings from day-to-day. Diary entries proved a helpful way of surfacing more mundane, daily occurrences that could affect mood, stress and feelings of loneliness.
1.3.3 Defining loneliness
DCMS follow the Campaign to End Loneliness and the Jo Cox Commission in defining loneliness as “a subjective, unwelcome feeling of lack or loss of companionship. It happens when we have a mismatch between the quantity and quality of social relationships that we have, and those that we want”.[footnote 11] Loneliness is not the same as social isolation as you can feel lonely while surrounded by people. However, the two concepts are linked and can overlap.
In introducing the research and approaching the topic with participants, interviewers did not use the word ‘loneliness’ unless it was used by a participant first. This is because people have different understandings of loneliness and some people may be reluctant to use the word.[footnote 12] Instead, participants were asked about their feelings of connection to people in their social network. This allowed the discussion to be participant-led and to avoid any potential stigma attached to the concept of loneliness.
1.3.4 Limitations
The research adopted a purposive sampling approach in order to achieve range and diversity across the sample. The sampling approach included a focus on a number of primary criteria (mental health condition, gender, life stage) and also monitored secondary criteria (see Appendix A for full details). It was not possible within the sample to monitor and achieve diversity across all demographic criteria. As a result, the sample did not include any participants who identified as non-binary or trans. The research did not explicitly monitor sexual orientation or ethnicity, although this was reported by participants where relevant to the experiences under discussion. These limitations should be considered when reading the findings. Future research could explore in greater detail the specific experiences of loneliness and mental health among the LGBTQ+ community as well as among ethnic minority communities.
1.4 Report structure
The report is divided into the following sections.
- Chapter 2 describes the participants across the four key life stages including their experiences with mental health and how it affected their lives.
- Chapter 3 presents the main findings on how participants felt that loneliness and mental health interact.
- Chapter 4 presents findings related to how participants felt that the social stigma associated with mental health and loneliness impacts on their experiences of loneliness and affects their ability to get support.
- Chapter 5 explores how key life events affect experiences of loneliness and mental health across life stages.
- Chapter 6 explores the support and interventions participants accessed and provides recommendations on how these could be improved.
The report does not provide numerical findings, since qualitative research cannot support numerical analysis. This is because purposive sampling seeks to achieve range and diversity among research participants rather than to build a statistically representative sample. Instead the qualitative findings provide in-depth insights into the range of views and experiences of the participants in the study and verbatim quotes are used where relevant to illustrate these.
2. About the participants
This section provides a brief overview of the participants in the research. It starts by describing the mental health conditions experienced before exploring each of the four life stage groups in more detail (for more details on the sample please see Appendix A.
2.1 Mental health conditions
There were a range of mental health conditions represented across the sample. These included: depression, anxiety (taking different forms[footnote 13]), schizophrenia, borderline personality disorder (BPD), bi-polar disorder, post-traumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), seasonal affective disorder (SAD), and specific phobias. Participants reported both single and multiple conditions, and a number of more complex conditions (such as schizophrenia or borderline personality disorder) manifested through symptoms consistent with depression or anxiety. There was a range of experiences of diagnosis and treatment, from more formalised diagnosis with participants receiving talking therapies and/or medication, to self-diagnosis with no formal treatment in place. Experiences of mental health conditions tended to fluctuate with participants describing this as a ‘rollercoaster’. The sample included both those who reported currently experiencing a mental health condition as well as those who reported this as being in the past only.
Mental health conditions affected participants’ lives in a range of ways. Most obviously they manifested in symptoms affecting mood and emotions, including low mood, anger or irritability, crying, loss of joy, feelings of being overwhelmed or stressed, low self-esteem and negative self-talk. This could also lead to self-harm, suicidal thoughts or attempts. Experiences of hypervigilance, hallucinations, flashbacks, paranoia, mania, psychosis and dissociation were also reported, particularly among those with more complex or severe mental health conditions. Mental health conditions could also have physical effects, for example leading to chronic fatigue, insomnia, panic attacks or impact on diet. These symptoms could leave people unable to conduct daily activities such as being unable to work or study or unable to leave the house or travel. The severity of these impacts varied across the sample.
2.2 Life stage groups
Participants were from White British, White European, Black Caribbean, or South Asian backgrounds and fell into four life stage groups as set out in the sampling approach. This section provides a brief description of each of the four life stage groups.
2.2.1 Young adults
The young adult group included participants aged between 18 and 30. Participants were working or studying full- or part-time, or were not currently working or studying due to their mental health conditions. Participants also engaged with hobbies or other activities such as: going to the gym or playing football; online gaming; walking; taking care of pets; and playing musical instruments. This group tended to discuss greater use of online forms of socialising e.g. chatting online or making friends through gaming than other life stage groups. In terms of living arrangements, there were a range of situations, with people living alone, with a partner, with their parents, or in a shared house or student accommodation.
Among this group, mental health conditions were as varied as in the overall sample and included depression, anxiety, schizophrenia, BPD, PTSD, bipolar disorder. Participants also experienced some physical or neurological conditions such as migraines or ADHD.
2.2.2 Parents of young children
Participants in this group all had a child under the age of five in their household which was the defining criterion for this group. As a result, this included the greatest variety of ages from those in their twenties to those in their forties. Among this group, there were a range of different family situations, including: single parents living with their children; parents who were separated from their biological children and living with a partner and stepchildren; and those bringing up their children with their partners. Among this group, participants were either working full- or part-time, staying at home to take care of their family, or not currently working due to their mental health condition.
Once again there were a range of mental health conditions including depression, anxiety, PTSD with paranoia and specific phobias. Physical health conditions in this group included hypothyroidism, fibromyalgia and an arthritic condition.
2.2.3 Middle aged
This group of participants were aged between 40 and 60. Among this group there were a range of family situations including: single parents; those with partners and children; those with partners only; those who were single and did not have children. Relationships with children could also be complicated where children had disabilities, mental health issues or neurological conditions such as Autism Spectrum Disorder (ASD), or where participants were estranged from their children. Among this group, participants were working full- or part-time, or not working due to their physical health conditions. The latter group tended to be on disability benefits.
There were a range of mental health conditions experienced across this group including depression, anxiety, BPD and panic attacks. Participants in this group also experienced physical health conditions, some of which had started relatively recently and had a big impact on quality of life. These included colitis, neurological problems leading to chronic pain, past accidents at work, or illnesses/infections that had led to reduced mobility.
2.2.4 Retired
This group of participants included retired people of any age (all were over 50). Participants lived with long-term partners and/or grown up children or alone. Daily activities among this group included volunteering (for example in a local church or in an animal charity), caring for others, participating in arts and crafts activities (either alone or in a group), activities through the University of the Third Age and hobbies such as reading and walking.
Again, participants experienced a range of mental health conditions including depression, anxiety, SAD, and OCD. These had been experienced on and off over the course of people’s lives. Participants in this group were sometimes more reticent about talking about their mental health directly; instead using euphemisms such as being ‘low’ or being ‘blue’. Physical health conditions were common across this group and included: Chronic Obstructive Pulmonary Disorder (COPD), high blood pressure, type 2 diabetes, osteoarthritis and mobility issues, ulcerative colitis and heart disease.
3. Loneliness and mental health
This chapter presents the main findings on the relationship between loneliness and mental health. It begins by exploring how loneliness was experienced and described by participants. It then examines participant and stakeholder views on the relationship between mental health and loneliness, and the type and quality of social relationships that participants had. Finally, it looks at differences by demographic group in terms of how loneliness and mental health were perceived and experienced.
3.1 Experiences of loneliness
3.1.1 How loneliness was described
Participants across all groups and life stages were more likely to talk about not feeling close to and supported by others, rather than describing themselves as ‘lonely’. The words ‘lonely’, ‘isolated’ and ‘alone’ were more commonly used by participants in their written diary entries rather than during interviews. As noted in the introduction, interviewers only used the word lonely if participants themselves first used that word. Instead, participants were asked about their feelings of connection to people in their social network. When describing such connections, participants listed the people who they had contact with, the frequency of contact, and quality of the connection. As a result of this approach, it was not always possible within the study to differentiate between experiences of isolation and feelings of loneliness.
When describing a lack of connection to others, participants spoke of: not feeling close to or supported by family or friends; not having close friends or people they could talk to; not going to social events or enjoying mixing in groups of people; and spending a lot of time alone. Participants also described themselves as ‘a bit of a loner’ or ‘shy’, in some cases, despite having wide social networks such as a large extended family.
Loneliness, or a lack of connection to others, was generally described not as about the number of connections an individual had, but about the quality of connection. Participants spoke of feelings of distance, rejection or not being understood by those who they wanted and perhaps expected to feel closer to, such as close family members or a partner. A lack of connection with and emotional support from such individuals prompted feelings of loneliness.
I tried to see my great granddaughter who is 1 year old and my granddaughter always has an excuse to put me off (…) I love them both but find it difficult to have a closeness with them (…) My partner wasn’t in the best of moods and seemed rather distant. He apologised but I don’t feel very close to him at present (…) [I] feel a bit lonely.
– Female, retired, depression - diary entry
Conversely, a good connection with others was described not as having lots of social connections but as having someone who they could ‘talk to about anything’ or rely on when they needed emotional support.
3.1.2 How loneliness was experienced
There was a spectrum of experiences of loneliness, from those who were more isolated to those who were more socially connected. At one end of the spectrum were those with no social network, who felt that they had no friends at all, no social life, and no one they could depend on for support. Their social interaction was very limited, for example, only with colleagues at work, or an adult child who they did not see often. This group’s sense of loneliness was typically long-term, and something they had come to accept as their way of life. Depression was the most common mental health condition experienced by participants in this group, who also tended to be in the middle aged and retired life stages. As discussed further in section 3.2, depression and other mental health issues were explicitly linked by participants to long-term loneliness.
Further along the spectrum were those with a low level of social connection. They had a select few people who they trusted and could confide in, often a friend or partner. Their support network had some understanding of their mental health issues and how it affected them. This allowed the participant to feel connected to and supported by them. This group was likely to ‘often’ feel lonely, but also experienced moments of connection with and support from others which alleviated their loneliness to some extent. This group included participants across all life stages and with a range of mental health conditions.
At the other end of the spectrum were those who had wider social networks and were more socially active. Their social network could include friends, a partner or spouse, adult children, siblings and parents. This group was more likely to seek out social contact. This could include seeking support with their mental health issues, and involving themselves in social events. However, periods of loneliness experienced by this group correlated with periods of poorer mental health.
Sometimes I feel absolutely fine…you’ve got your family, you’ve got people you see on the beach…a WhatsApp group of old friends…but other times I feel quite isolated really.
– Male, retired, OCD and depression
Participants with anxiety and depression were more prominent in this group than participants with other mental health conditions, and it included people in all life stages.
Stakeholders suggested that experiences of loneliness varied by the type and severity of mental health conditions. Moreover, they suggested that someone with severe mental illness would be less likely to be able to transition out of loneliness than someone with a less severe mental health condition. Although this trend was not evident in our sample, the severity of participants’ mental health condition was defined subjectively by participants themselves, rather than based on clinical definitions that stakeholders would use.
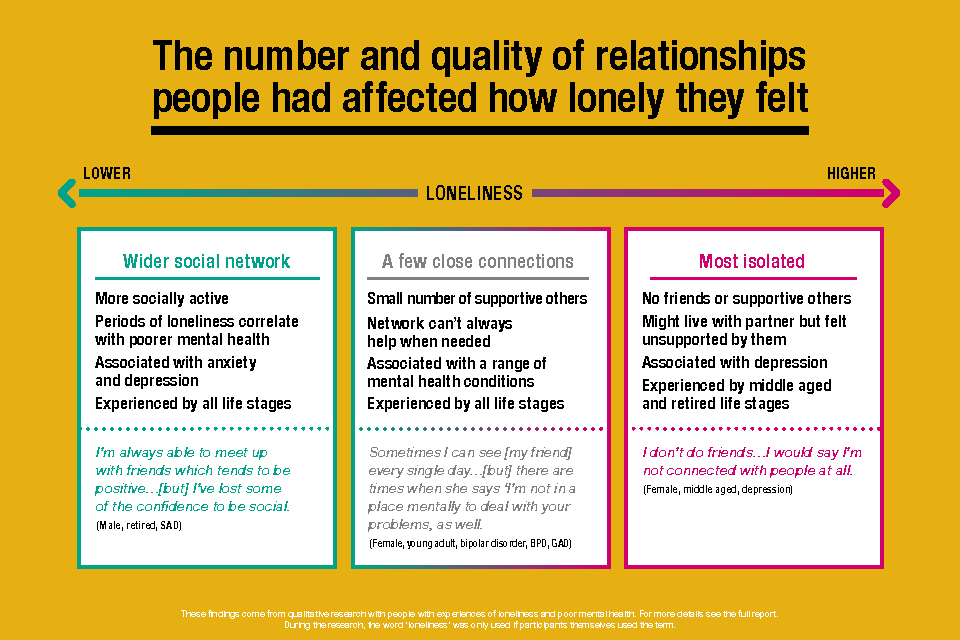
An image illustrating the spectrum of loneliness that participants in the research experienced, with the number of quality of relationships affecting how lonely people felt.
3.2 Views on the relationship between loneliness and mental health
There was a strongly-held view among participants and stakeholders that mental health issues and loneliness are closely intertwined. Although it was considered possible to feel loneliness without experiencing poor mental health, loneliness was considered to increase the risk of mental health issues and, conversely, mental health issues were considered to have a significant impact on feelings of social isolation and loneliness. Stakeholders were of the view that loneliness and depression or anxiety increase in tandem and that loneliness can be experienced as part of a mental health condition, with sufferers often unable to differentiate one from the other. Further, the relationship was perceived by both participants and stakeholders to be multidirectional; that is, poor mental health could lead to loneliness, and vice versa.
3.2.1 Views on how loneliness and mental health are linked
As discussed, the relationship between mental health and loneliness was considered to be bidirectional.
Mental health issues leading to loneliness
Participants and stakeholders identified various patterns of thought and physical symptoms of mental health issues that linked to loneliness. Some of these were related to the way in which participants considered themselves to be perceived negatively by others, such as:
- Low self-regard. Participants with mental health issues tended to have low self-regard and expected others to perceive them in the same negative light.[footnote 14] For example, they perceived their mental health issues to mean that they were a failure, weak, miserable, boring, or not fun to be around, so they opted to isolate themselves instead. One participant described in her diary how she was ‘dreading’ a weekend away with friends due to fears that others would perceive her negatively.
Not looking forward to packing for the weekend, to be honest I’m not looking forward to going at all. Everyone else (…) they’re going to think I’m boring (…) Absolutely dreading tomorrow.
– Female, middle aged, depression - diary entry
There were participants for whom the onset of their mental health issues had been sudden, and they felt that their personality had changed significantly at the same time. They grieved for the person that they used to be, who they felt was a more desirable person for others to spend time with. Participants who experienced paranoia also found that this aspect of their mental health acted as a barrier to social connection, because of their negative expectations and perceptions of how they were perceived by others.
- Fear of stigma leading to social withdrawal. The fear of being judged by people who do not understand their mental health condition acted as a barrier to participants talking to others about and asking for help with their mental health (discussed further in Chapter 4). Participants expected that others would not believe or understand how their mental health issues affected them, and so avoided social contact to protect themselves from critical judgement. Stakeholders echoed this view by describing people with mental health conditions who ‘get stuck not trusting anybody’.
Other thought patterns were underpinned by concerns around negative consequences of revealing their true feelings to others, including:
- Not wanting to be a burden on others. Participants felt that if they told someone how they were feeling, that person would feel worried, sad, or stressed, and they did not want to make those they cared about feel that way. Additionally, there was a perception that other people did not want to know about their mental health issues, either because it upset them too much, they did not know how to help, or they just did not want to know. This prevented participants from making contact with others or telling them how they were really feeling. Furthermore, participants perceived others to have ‘more serious’ problems to deal with than their own mental health struggles. So instead of sharing, participants kept their difficulties to themselves, which enhanced their feelings of loneliness.
- Needing to mask true feelings. The sense of pressure to not talk about their struggles for fear of being a burden or being judged, could also make participants feel that if they did interact with others, they had to mask their true feelings and pretend to be ok. However, this pretence was exhausting and unsustainable, and led to participants opting out of social interaction.[footnote 15]
I’m conscious that I haven’t given my mum a ring this week and I feel guilty about this…I just haven’t been able to put on the usual act from my end- I’m ok act. (…) Trying to hide how miserable I’ve felt has been too hard.
– Female, middle aged, anxiety and depression - diary entry
Alternatively, if participants did interact with others while pretending to be ok, this compounded both mental health issues and feelings of loneliness as, not being their true selves, they could not feel genuinely connected to others.
Mental health issues could also limit individuals’ capacity for social interaction in the following ways:
- Mental health conditions limiting ability to support others. Participants felt that mental health thwarted their capacity to be a ‘good friend’. For example, not being able to predict when their mental health would vary meant that they sometimes had to cancel social arrangements at short notice. Participants felt this made them unreliable, which precipitated feelings of shame and guilt. This in turn worsened their mental health. Poor mental health could also make it difficult for people to be supportive of others, as their mental health struggles could be all-consuming. For example, those with anxiety explained that their thoughts and worries would take up all of their mental energy. Furthermore, physical symptoms of mental health issues, such as headaches, nausea and fatigue, could be distracting, so that they were unable to be fully present for another person. The overall effect was that people withdrew from social contact, thus increasing their sense of loneliness.
Today I was glad I was alone, I felt distant and conflicted… even when my girlfriend phoned me I wasn’t really there, I wasn’t listening. To be honest I wanted the phone call to end as soon as possible, it’s not that I don’t care what she had to say but I couldn’t even if I tried. I had no motivation or energy to do so.
–Male, parent of young child, depression - diary entry
- Feeling overwhelmed in spaces for socialising. Participants with BPD and schizophrenia described feeling ‘overwhelmed’ in crowds or busy public places. This meant they were unable to engage in social activities in public places such as meeting friends in a shopping centre. Feelings of being overwhelmed caused participants to ‘shut down’ so that they felt unable to interact with others.
Furthermore, mental health issues could inhibit an individual’s desire for social connection with others by giving them a distorted, overly negative view of other people:
- Mental health issues could induce negative perceptions of others. There were participants whose depression gave them a distorted view of others, so that they viewed others more negatively, or became less tolerant of or angry towards others when depressed. One participant with depression explained how he was unable to identify the influence of depression on his thoughts and feelings during a depressive episode. Instead, he would believe that his negative thoughts towards others were rational. This led him to shun contact with those who he felt negative towards, thus increasing his isolation.
The mind never accepts that it’s ill…it will put anything as a reason for you feeling bad in place of it. You are feeling that way because your family are not nice to you…you sort it out by cutting yourself off from what you imagine could be the problem…the person that you’ve been friends with all your life.
– Male, retired, depression and anxiety
There was a view among stakeholders, supported by findings from participants, that there were similarities in the way that people with loneliness and people with depression behaved, such as social withdrawal and brooding. Stakeholders explained that loneliness, like depression, affects how individuals feel about their social relationships. This means that they are more likely to think negatively about social interactions, take slights more seriously, or brood on things that have gone wrong during an interaction.[footnote 16]
One stakeholder illustrated how the way in which someone with a mental health condition perceives situations could prevent them from transitioning out of loneliness. They explained that, if an individual experienced an event that brought about loneliness, such as bereavement, moving to a new area, or retirement, there were two potential ways in which that person could respond. The more helpful response would be seeing the cause of feelings of loneliness as an external event and trusting that things would improve over time. A less helpful response would be seeing the experience as part of your identity, and therefore how your life would continue to be long-term, which would increase the likelihood of experiencing chronic loneliness. This idea, referred to as the locus of control, has been explored extensively in psychological academic literature in relation both to loneliness and mental health more generally.[footnote 17]
Loneliness leading to mental health issues
Conversely, participants had experiences of loneliness leading to poor mental health. Relationship breakdowns, poor physical health, lockdowns during the COVID-19 pandemic, and retirement, had brought about periods of loneliness which triggered mental health issues. For example, a young man who developed a disabling and painful physical condition in his early twenties was suddenly unable to go out to socialise with friends, who gradually stopped visiting. This period of sudden isolation triggered his first episode of depression. During such periods of isolation, participants described having ‘fallen out of practice’ in social skills and, consequently, had lost their social confidence.
Furthermore, participants described how negative emotions and thoughts became more intense as they endured prolonged periods of loneliness, which precipitated poor mental health.
[Isolation during the pandemic meant my feelings were] building up and got to the stage where you start dwelling on negative thinking…and it’s got to a stage where it’s exploding.
– Male, middle aged, anxiety and depression
Without the distraction of company, participants explained they were more likely to ruminate on their worries or think about traumatic events in their past, which worsened their mental health.
Not connecting with others…allows all sorts of imaginings and irrational thoughts…being really introspective, but at least if you’re mixing with people you’re not constantly thinking about your worries and ailments and your fears.
–Female, middle aged, depression
In addition to being a helpful distraction from distressing thoughts, socialising with others gave people a sense of purpose and motivation. In the absence of company, participants were more likely to feel despondent.
I am always able to meet up with friends which tends to be positive. It’s when I’m home alone where I note I lack drive (…) I find myself moping around, feeling tired and napping in the afternoon.
– Male, retired, SAD - diary entry
The link between loneliness and mental health was considered to be cyclical, and it was therefore difficult for participants to identify which factor they had experienced first. For example, mental health issues could make relationships more difficult to sustain, which prompted relationship breakdown, causing feelings of loneliness, which triggered a worsening of mental health, which led to further loss of social skills and capacity to interact with others.
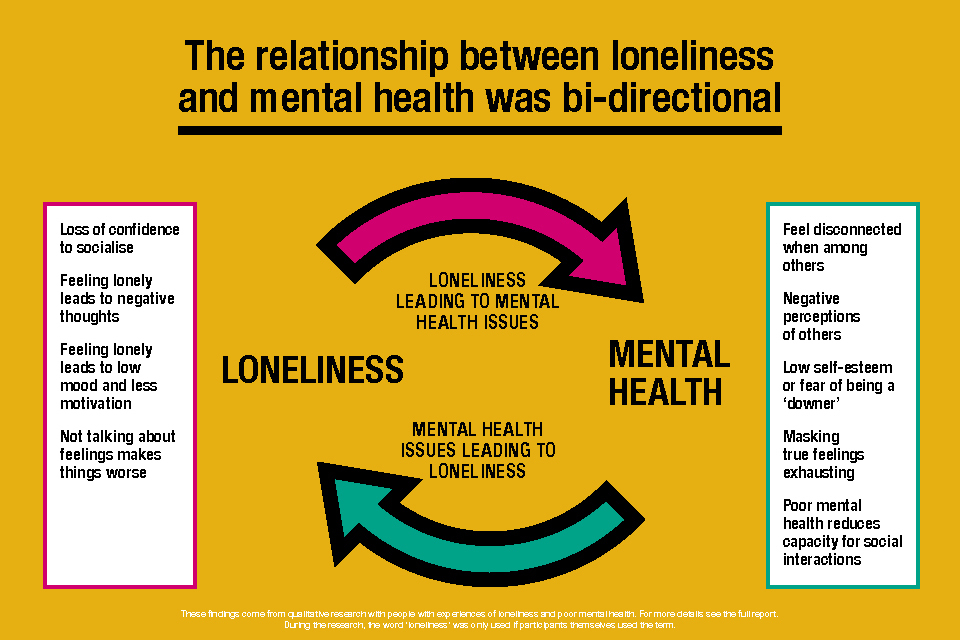
A visual showing that the relationship between loneliness and mental health was bi-directional, with loneliness leading to poor mental health and mental health issues leading to loneliness.
3.3 Type and quality of social relationships
It was emotional support rather than any other type of support that constituted a high-quality social relationship in the views of participants. The people who participants felt connected to were typically those who they felt understood, at least to some extent, their mental health issues. While participants did have others who provided them with practical support, such as help with childcare or accommodation, this did not make them feel ‘close’ or connected to that person unless they also provided emotional support.
As discussed earlier, there were three groups of participants on a spectrum of loneliness. Those who were most lonely (who tended to be in middle aged or retired life stages) described themselves as having no friends or people they could connect with.
I don’t do friends…I would say I’m not connected with people at all. It is because I don’t have the willpower to connect with people. I don’t trust people. The other issue is that I just don’t have time for other people
– Female, middle aged, depression
While participants in this group might have people they associated with, such as work colleagues, they did not have a close connection they could rely on for emotional support. There were participants in this group who felt close to an adult child, but these relationships were described as more supportive of the adult child than of the parent. That is, while the parent felt their child would talk to them about anything, they did not necessarily confide to the same extent, due to a reluctance to burden or worry them. This group included individuals who lived with a spouse or partner, but whose partner did not support them with their mental health. This furthered a sense of disconnection and isolation, as participants felt particularly alone when those who they were supposed to be closest to were unsupportive. This group lacked a connection with someone who they could confide in, who would show some understanding of their mental health, and provide emotional support.
The second group (which included participants across all life stages) had a small number of social connections who they felt close to. This could include a partner, a close friend and, among young adults more commonly, a sibling or a parent. Participants had made close friends in the workplace, online, or had close friends from childhood who they had known for many years. A sense that the other person knew and accepted their true selves, including their mental health issue, was a key constituent of a good quality relationship. This allowed participants to feel they could be ‘themselves’ when with that other person, confide in them, and not have to excuse or explain their behaviour. Talking to and spending time with these close others was a key protective factor for those with mental health issues. The social connection had a positive impact on their mental health, and talking to others about their mental health issues had, in some cases, encouraged participants to seek help from professionals.
However, support from such a small number of contacts had its limitations. Participants might not have contact with their trusted others often or at times when they really needed their support. Or, when they did have contact, they might not disclose the full extent of their mental health struggles for the reasons described in section 3.2.1, such as a fear of burdening them. Despite having close connections with others, their mental health issues could act as a barrier to reaching out to ask for support when they needed it.
The third group (which included participants across all life stages) had a wider social network which might include a partner, friends, colleagues, and family members. This group was more comfortable with group social situations and enjoyed social contact more unreservedly than the other two groups. However, during episodes of poor mental health (most commonly depression or anxiety), they lacked the quality of connection and support that they needed. For example, one participant experienced loneliness after her marriage broke down. Even though she described herself as ‘very, very social’, she felt isolated and alone with overwhelming responsibilities as a single parent.
As a single parent with teenage children with additional needs I worry about everything (…) It would be good if I had someone other than my oldest son to talk to about my worries. There’s no-one really.
–Female, middle aged, anxiety and depression – diary entry
A young adult in this group also described herself as a sociable person with a strong support network of family and friends, but experienced loneliness sometimes due to not having a partner.
Moreover, there were participants in this group who, despite having a wide range of social connections, found it difficult to trust people, so they struggled to make deeper connections with others. Instead, they had a number of more ‘surface level’ friendships, to whom they did not disclose the full extent of their mental health struggles.
Other factors that influenced participants’ social relationships included:
- An aversion to social interaction in groups and with strangers. It was common for participants in the more isolated groups (those with no or low-level social connection) to have an aversion to groups of people and social interaction with people they did not already know. Group situations could make participants feel stressed, anxious, threatened or overwhelmed, so there was a preference for social interaction on a one-to-one basis. Going on a group outing with people they did not already know was particularly daunting. One participant who had been offered a lift from a befriender to take them to a group event had not accepted the lift because she had never met the befriender before.
- A preference for online rather than face-to-face social interaction. There were participants who explained that they found it easier to interact with others online than face-to-face, particularly when experiencing periods of poor mental health. They felt that by not seeing the other person when talking online, they were less likely to be judged or critically appraised by the other person. In some instances, participants had formed close relationships with friends online over many years, and they considered the relationships to be of high quality.
- Friends had ‘fallen away’ with the onset of participants’ mental health condition. In some instances, this was interpreted by participants as their friends not being able to cope with their mental health issues, and the overall effect was increased isolation. Discord or relationship breakdown with family members was also a prominent feature of participants’ lives, with adult siblings or one parent who participants rarely, if ever, had contact with. It was also rare for older, retired participants to have sustained once-valued friendships from their youth. For example, retired army personnel spoke of having lost contact with close friends who they had been in the army with.
3.4 How experiences of loneliness varied across demographic groups
A number of demographic factors appeared to influence perceptions and experiences of loneliness and mental health, including ethnicity, sex, age, sexual orientation and physical ill health or disability. Some of this was linked to different experiences of stigma which is discussed further in Chapter 4.
3.4.1 Ethnicity, migration, culture and religion
Ethnicity was highlighted by both participants and stakeholders as a key factor influencing experiences of mental health and loneliness. Participants from ethnic minority groups highlighted their cultural backgrounds and upbringing, in which mental health issues were either not recognised, not spoken about, or minimised. Some saw this as wanting to play down traditional links, and shame, associated with the idea of ‘craziness’ or ‘madness’ in the family. Others, however, emphasised the struggle of first-generation migrants trying to make a new life for their family, to make friends and to fit in. One participant felt that in her South Asian community, women were expected to be fully competent in carrying out their responsibilities and were not allowed to say they were feeling unwell or were anything less than capable.
[In the Asian community] you cannot be mentally ill…There’s nothing called mentally ill
– Female, parent of young child, depression
In addition, participants from ethnic minority groups recalled experiences of racism, which had led to feelings of separation and isolation from others and low self-esteem. Echoing this, stakeholders noted that black men are disproportionately likely to be diagnosed with paranoid schizophrenia than white men, and considered there to be a link between experiences of racism and paranoia.
There were participants who had immigrated to the UK as adults and had found it difficult to make social connections since arriving in this country. They had found the cultural and language barriers particularly difficult to overcome while also experiencing poor mental health. Similarly, stakeholders identified international students as a high-risk group for experiencing loneliness.
While not necessarily linked to ethnicity, religion could also play a role in delaying seeking spiritual or professional help, as participants saw their mental ill-health as a test from God that they needed to overcome themselves.
3.4.2 Sex
There were apparent differences by sex in how mental health and loneliness were experienced by participants. Male participants were more likely than female participants to think that society perceived mental health issues as a sign of ‘weakness’. This prevented them from disclosing their mental health struggles to other men, for fear they would be judged as less strong than men without mental health issues who were seemingly coping better than they were. Middle-aged and older men with a variety of mental health conditions were told to ‘man up’, and embarrassment about showing feelings to others, particularly to other men, set in from an early age. They were more likely to disclose and discuss their mental health issues with women rather than men. Two younger male participants had received help for emotional or psychological difficulties at school, but said they felt embarrassed to let their ‘mates’ know because of how they might view them. Some male participants said they would only talk about their feelings to a partner or dispassionate professional such as a GP or therapist.
Further, depression in male participants was more likely than depression in female participants to manifest as anger, irritation and intolerance towards others. The way in which expectations about being a ‘man’ affected the ability of men to express emotion, or to empathise with others experiencing psychological difficulties, also affected the women with whom they interacted. Female participants told us that their husbands or male relatives (e.g. father, husband) had been unsupportive, mocked them, or dismissed their feelings out of hand. In some cases, this had left female participants struggling with post-natal depression or suicidal thoughts by themselves.
Male participants were as likely as female participants to want a close emotional connection with others, someone who they could talk to and disclose their mental health struggles to and feel understood by. However, when describing their social connections, men were more likely to describe social activities they engaged with, such as going to the pub, cycling or playing golf with friends. In contrast, female participants were more likely to describe the relationship they had with close others, rather than describe activities that they did together.
Female participants were more likely than male participants to feel socially isolated and suffer poor mental health due to a lack of support with raising their children. However, male participants were more likely than female participants to have children from a past relationship who they no longer lived with. Not being able to spend enough time with their children was a key source of emotional pain for these fathers.
Missing my son has been the hardest experience of my life, I miss him every moment of every day. I have him every other weekend but it’s hard to connect with him, I don’t want to get used to him being there just for him to go again…it hurts so much to see him go. On Sundays before he goes home I almost completely shut down in preparation for him to not be there again.
– Male, parent of young child, depression and anxiety - diary entry
Other differences by sex included that there were female participants who had experienced violence from a male perpetrator who were now afraid of male strangers, particularly men showing aggression in public. This made them more reluctant to go out in public. This had been particularly acute for one participant who experienced what she referred to as a mental breakdown and was diagnosed with BPD after she experienced a sexual assault in her early twenties. After this point, she had not returned to work and her loneliness had increased.
3.4.3 Age
Younger participants said that they had parents, grandparents, or had encountered other older people who were less sympathetic in their views about mental and emotional struggles than they or their peers. These older people told participants who sought help from them to “get over it”, “go for a walk” or to find something to ‘distract’ them from their worries. Participants of all ages who encountered these views among older people tended to avoid further disclosure to them. Some older participants also appeared to have internalised the idea that they should get over their problems themselves. They tended to play down the symptoms of their mental health conditions as just ‘troubles’, ‘grumbles’, or unexplained feelings of anger, irritability or loss of joy.
3.4.4 Sexual orientation
Stakeholders reported that LGBTQ+ groups were more likely to experience loneliness as a result of social discrimination, whereby micro-aggressions would act as a reminder that they were not accepted in society. Echoing this view, a homosexual participant recalled a long history of poor mental health and loneliness due to experiencing discrimination for being ‘different’. He had struggled to come to terms with his sexual orientation during adolescence and had continued to struggle to find a partner since, which he felt was a key contributor to his loneliness. As the sample did not include participants from other LGBTQ+ groups, it was not possible to explore their specific experiences in this study.
3.4.5 Physical disability and ill-health
Mental ill-health was often associated with physical ill-health, especially where participants were in pain due to debilitating conditions (e.g. migraines, neurological conditions, ulcerative colitis) and/or had limited mobility. Difficulties arose where these problems were not treated together in a holistic way. Physical ill-health affected participants’ ability to engage in social activities organised around sports or socialising in public. This resulted in participants feeling more isolated. Disabled participants also said they felt that other people were shocked at their physical decline or weight change. They described feeling left at home by themselves, while partners, family or friends went out without them. However, they also felt guilty about asking partners or friends to change their plans to involve them. They felt that they could not share how the physical changes also affected their mental health leading to them feeling more lonely.
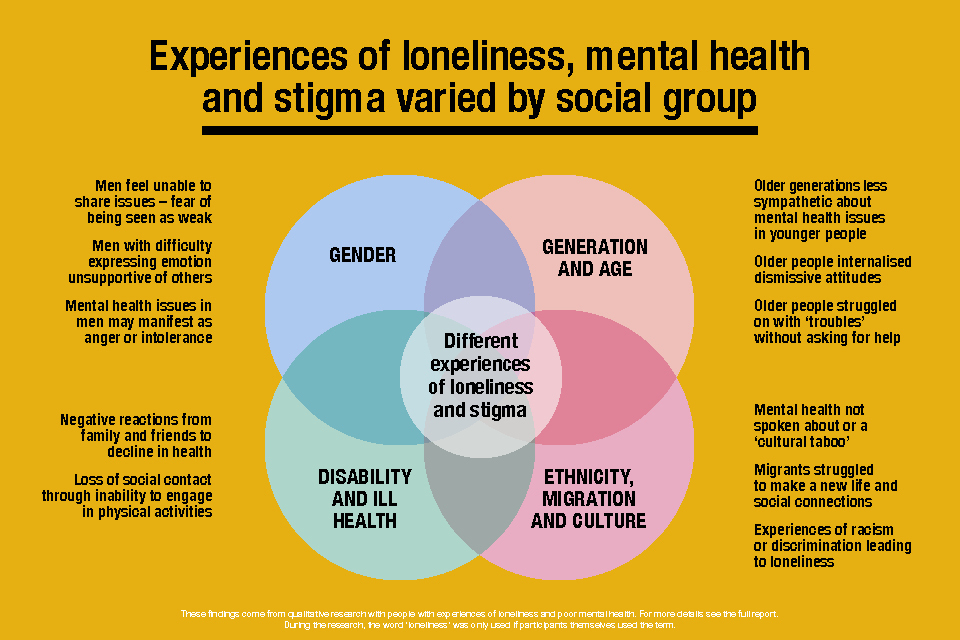
A diagram illustrating how experiences of loneliness, mental health and stigma varied by social group including based on gender; generation or age; disability or ill health; and ethnicity.
4. Stigma, mental health and loneliness
This chapter explores participants’ views on the stigma associated with mental ill-health and loneliness; how experiences of stigma produced or reinforced feelings of isolation and loneliness; and the effects this had on participants’ ability to seek help and support.
As highlighted in Chapter 3, mental health issues could lead to loneliness where people felt that they could not reveal their true feelings or struggles to others and so were unable to get emotional support from their social connections. Part of what prevented people being able to share their experiences was fear of the stigma associated with mental health conditions. This could relate to fear of the reactions that participants expected to receive from others or their own internalised stigma that their mental health issues were not worth sharing. This lack of feelings of closeness with those they expected or hoped to be understood by increased their feelings of loneliness.
Feelings of loneliness were also associated with stigma. This shared common features of shame, judgement and fear of negative consequences with the stigma associated with mental ill-health. The stigma attached to loneliness was often intertwined in participant accounts with the stigma associated with mental ill-health and was difficult to separate analytically.
4.1 Participants views on stigma
Participants identified stigma associated both with mental health conditions and symptoms, but also with loneliness. The form of expression this stigma took varied slightly between mental health and loneliness, although both were experienced in the common context of shame, embarrassment, and the fear of negative judgements by others.
4.1.1 The stigma associated with mental ill-health
Participants thought there was increased discussion of mental health in society, but that stigma associated with mental health conditions remained. Stigma associated with mental health was experienced as the dismissal of mental ill-health as ‘not real’, the trivialisation of the struggles people faced, and themisunderstanding of mental health conditions, their symptoms and effects.
Depression and anxiety were regarded as being more widely discussed in public than other conditions and this was believed to be because of the millions of people suffering from them. The COVID-19 pandemic, and the effects of lockdown restrictions, were considered to have put mental health and well-being, and the need for social connections, higher up the public policy agenda. However, participants felt that increased discussion of mental health did not automatically lead to greater understanding or acceptance of mental health conditions. Participants across all life stage groups thought that it is difficult for people who had not experienced mental ill-health to understand its debilitating or challenging effects, in part because the concept of illness was still framed in physical terms.
Participants identified different facets of the stigma associated with mental health conditions, all of which could lead in different ways to increased feelings of loneliness or people withdrawing from social contact.
- Weak or soft. As noted above, participants talked about how mental ill-health is viewed differently from physical ill-health. While there was acceptance that physical ill-health may affect one’s ability to do day-to-day activities, some participants said that others perceived mental ill-health as making them ‘weak’ or ‘inadequate’ overall, or that it made them unable to deal with everyday life at all. Participants across the different life stages regarded these views as being particularly present among older generations. Younger participants thought older people saw them as ‘soft’.
- Incapable or unreliable. Participants who were working said they felt that some employers viewed people experiencing mental ill-health as incapable or less reliable than other workers who did not experience poor mental health, sometimes based on personal experiences of these attitudes. Some participants said people had questioned whether they were making a real effort to do things or whether they were ‘just lazy’.
- Attention-seeking. Accusations of this kind were particularly levelled at participants who had told others that they had suicidal thoughts. They were told that, if they were ‘really’ suicidal, they would have just killed themselves. Where participants had attempted suicide, they were criticised for not having revealed how they were feeling sooner. This was sometimes despite their previous experiences of being told they were over-playing the problems they were facing.
- A burden or worry. This especially related to the worry of ‘being a burden’ to parents, children, or friends with whom the participant socialised or relied on otherwise for social connection. Participants with conditions ranging through anxiety, depression, BAD, PTSD, and psychosis, sometimes played down their illness, saying symptoms were a ‘blip’. They also withdrew from social contact so that people would not ‘fuss over’ them.
- A ‘downer’. Participants said that they thought other people did not want to be around them or spend time with them because they would be a ‘downer’. This word was especially linked to people with depression or other conditions with depressive elements, suggesting they lowered the mood of other people around them due to their own low mood. Some people with longer-term clinical depression would withdraw socially when they recognised symptoms coming on so as not to bring their family or friends down.
Today I feel down. I want to shut myself off from people. I can’t see the point in telling others how I’m feeling because it just brings them down with me.
– Female, retired, depression – diary entry
In another example, a participant described the way in which people ‘peeled away’ from him when he was depressed.
Although participants noted an increase in the discussion of mental health in wider society, some felt that the societal discussion was ill-informed. Participants pointed to the role of ‘influencers’ in promoting discussion about mental health, particularly, celebrities or sports people who are widely admired. They felt that some celebrities had jumped on the ‘bandwagon’ of mental ill-health, thereby diminishing the experiences of people who really suffered. In particular, some people had begun to mistake everyday changes in mood or anxieties as symptoms of mental health conditions. Participants emphasised the distinction between everyday anxiety or feeling a bit sad, and anxiety that prevents people being able to carry out everyday tasks, or depression that can lead to total isolation from others and suicide.
4.1.2 The stigma associated with loneliness
The stigma attached to loneliness was evident in the way that some participants wanted to avoid the term all together. Instead, they preferred to talk about feeling ‘isolated’ or ‘alone’, or not having the social or emotional connections as described in Chapter 3.
Admitting the need for social connection was considered intimate and potentially embarrassing to the person making the disclosure and to the person hearing it. There was a concern about appearing sad, needy or desperate. Participants who felt this way feared that, by revealing that they were lonely, friends, work colleagues, family or neighbours would see them as inadequate, socially or emotionally, and might avoid or reject them. A participant who had retired early expressed this through his disappointment that work colleagues who he thought of as friends did not keep in touch.
I lost contact with all these clients that I used to see on a regular basis, all the work people I used to see on a regular basis… You can’t be the sort of person that’s always going back into the office… You can’t do that sort of thing, so I guess I just thought better just to break away… not really have any contact.
– Male, retired, OCD
In another example, a retired female participant described feeling that it could be better to have a mental health condition than to be single or widowed in social situations, as you received less support for being alone. This was in part due to the fact that much socialising was done in couples, and so single people were less likely to be included.
Another notable theme across participants was that their mental health conditions made establishing and keeping relationships and friendships more difficult. Where anxiety prevented participants from socialising, or low self-esteem made them feel they were ‘not good enough’ to be around other people, the perception that other people viewed them as ‘sad’ or ‘needy’ was perpetuated.
A recurring theme was that participants often held back from saying how they really felt when others asked them for fear of embarrassing others and themselves. It was notable that some participants went further in describing the depths of their loneliness in their diary entries prior to being interviewed, than they did in their interviews. Discussion of feeling lonely was also often the part of the interview during which participants became most upset. Where participants were prepared to say they felt lonely, there was still a sense of embarrassment to saying it. It is likely that this impacted on participants’ ability to reflect on and explicitly talk about the stigma associated with loneliness. It is also notable that there is much less societal discussion about the stigma associated with loneliness.
4.2 Consequences of stigma
Stigma associated with mental health conditions manifested in other people’s reactions of dismissal and trivialisation to participants. This also applied to signs of mental ill-health arising from feelings of loneliness, or the consequences of mental ill-health that were made worse through depression, anxiety and tendency to isolate from others. The stigma associated with mental ill-health and loneliness could also be internalised as feelings of shame or embarrassment, making participants hesitant to ask for help and support.
4.2.1 Stigma resulting in dismissal and trivialisation
Stigma linked to mental ill-health and symptoms was experienced through the way that participants felt that their feelings and struggles were dismissed or trivialised by others. Trivialisation of participants’ feelings and struggles was reported in the way that others dismissed their symptoms, condition or circumstances as:
- not having real effects on their lives
- being something they could control if they wanted to, and/or
- being just expressions of feelings or circumstances that everyone had to deal with
There were instances reported in which family members, friends, work colleagues, managers and employers had openly stated that they did “not believe in mental illness”. Alternatively, their experience of how badly others with mental health conditions or symptoms were treated, meant that participants felt they had to hide significant difficulties they were experiencing, or what they considered substantial parts of themselves.
Another guy I worked with very closely… had a complete nervous breakdown in the middle of the office. We never saw him again… Seeing how people deal with it, if you’re suffering it for yourself, the last thing you’re going to do is let any of them buggers know!
– Female, retired, depression and anxiety
Participants discussed only revealing how they were feeling for the first time when they were at their most desperate. But even in these instances, they received mixed, ill-informed or patronising responses. Common responses were: “everyone feels down or anxious sometimes”, or that they “just needed to get on with life like everyone else”.
As a result, participants could be left feeling frustrated that people were not trying to understand them, which made telling people in future even harder. A middle-aged participant working full-time, who had lived with depression since his teenage years likened trying to get people to understand how he was feeling to “screaming in a room full of people” where “everybody’s got ear defenders on”:
You want help so badly, but no one can hear the message that you’re trying to get across. (…) Then you find it so hard to do it the second time or the third time
– Male, middle aged, depression
Repeated experiences of dismissal, trivialisation and misunderstanding meant participants felt shamed or embarrassed about revealing their feelings leading to greater feelings of loneliness.
4.2.2 Internalisation of stigma
Echoing the discussion above, stakeholders also discussed the role of stigma in affecting peoples’ experiences of mental health and loneliness. This was particularly through the way that social stigma can be internalised psychologically. This could be through:
- shame or embarrassment
- the fear of rejection or negative consequences
- the burden or worry that revealing that they are struggling, or lonely, may bring to others
This internalisation was reflected in interviews where participants avoided talking about their feelings of loneliness. Among retired participants, internalised attitudes about mental health issues not being ‘real’ were also evident in euphemisms they used to describe and downplay how they were feeling. Even where participants knew they needed help, they would often not ask for it or take up offers of help. This was because they worried about rejection later, or that they would be a burden to others.
4.3 Effects of stigma on ability or willingness to seek help
Experiences of stigma or internalised stigma associated both with mental health and loneliness could impact participants’ ability or willingness to seek help or affect who they sought support from.
4.3.1 Delaying seeking help
The powerful effects of stigma, and its internalisation through shame, meant some people did not reach out to friends or family, or seek formal help at all, or delayed doing so until their condition or circumstances significantly worsened (e.g. leading to a serious mental breakdown or suicide attempt). The effect of stigma was particularly marked among some groups or circumstances. For example, middle-aged and retired men talked about “getting on with it” or struggling on with problems until they got worse. The shame or embarrassment of feeling lonely or isolated as a young mother, or a disabled person with mobility issues, also made it difficult to reach out for help.
Participants were put off seeking help where their initial, tentative requests were dismissed or trivialised, which meant they remained undiagnosed and/or struggling with feelings and symptoms they did not understand. This was particularly true for young adult participants, who did not understand what they were going through until a crisis brought them in touch with mental health services.
4.3.2 Selective disclosure and signposted support
Stigma related to mental health and loneliness also meant participants looked for help and support more cautiously. There were no examples of people who said they were open to everyone about their mental health or associated feelings of loneliness. Instead, the risk of experiencing stigma was minimised by careful selection of who participants told about the difficulties they were experiencing.
Who did people tell?
- Trusted and intimate contacts. The first group of people that participants told about their symptoms were those with whom they were most intimate or had established greatest feelings of trust, including partners, close family or close friends. Romantic partners were often the first or only person participants told. Mums or siblings were also particularly prominent in participants’ accounts as being supportive. However, the difficulties associated with mental ill-health could also mean that they did not want to worry their partners or parents, and that they therefore kept problems to themselves. Friends that they told tended to be people who they knew had also experienced mental health problems, thereby facilitating a more sympathetic response. Alternatively, they were friends that they gauged through conversations would not be judgemental about their condition. However, there were instances where family and friends that participants thought would be supportive came across as awkward when told about their condition. This in turn made them feel embarrassed or ashamed, sometimes leading to a reduction in social connection with them.
- Knowledgeable professionals governed by principles of confidentiality. The second group was professionals who participants expected would understand mental health conditions, or would treat their disclosure sensitively, confidentially and with respect. These professionals included GPs, community mental health nurses, accident and emergency staff, HR staff and line managers at work, and school staff where the participant was a parent. Positive experiences were when professionals exhibited discretion, demonstrated some knowledge of treatments or support, and made attempts to accommodate the difficulties participants were experiencing. The absence of stigma, and the feeling that a participant was listened to and taken seriously, could lead to people being more open about their condition or circumstances. However, positive experiences following disclosure to professionals were not universal and tended to relate to the diagnosis of anxiety and depression, rather than more complex conditions.
Who did they not tell?
The people participants were least likely to tell about their condition, or their feelings, was their wider circle of friends or acquaintances, some work colleagues, and neighbours. This was because they felt there was nothing to be gained from them knowing, or because they felt that the person in question did not know them well enough that their attitude towards them would not be affected by negative stereotypes of their condition or circumstances.
Work was an area where people struggled with who they should tell when they were experiencing difficulties. Poor responses to other employees who had mental breakdowns at work, or who had disclosed that they were struggling, prevented participants from opening up to other work colleagues. Although some younger participants had positive experiences of support at work, others described the way in which they had seen colleagues having rewarding or challenging work taken away from them or being manoeuvred out of the workplace entirely.
One other area where participants had very negative experiences of disclosing their mental health condition was related to seeking support for domestic abuse and sexual violence. Here participants said police and the criminal justice system had treated mental illness arising from abuse or violence as a reason to undermine their testimony, or to present them as an unreliable witness.
4.3.3 Seeking, but struggling, to find the right support
A third group of participants had sought help or support through partners, family or professionals, but struggled to name the problems they were feeling or to find the specific support they needed due to misunderstanding or dismissal of their situation. They tended to have partners or families who were dismissive of their feelings, trivialised their cries for help, and avoided discussing that they felt lonely or despairing. Where they had approached health professionals such as a GP, they felt channelled into the main options of treatment (medication or talking therapies), which they felt did not meet their needs.
They struggled with the fact that they did not always feel they had a mental health condition or did not want to be labelled in that way. Rather they had symptoms of mental ill-health that arose from their experiences of a lack of connection with others, or the absence of tailored help and support that met their needs. It was notable that these participants often had experiences that differed from a perceived norm, or that reflected being a minority group, or that related to a more unusual or complex mental health condition. For instance, women who were struggling with pregnancy or motherhood, felt that their needs were dismissed by a view that these experiences would be overwhelmingly positive. Participants from ethnic minority groups, who were LGBTQ+, or who had a physical disability, felt their struggles were often different to most people and misunderstood. People with less well-known mental health conditions (e.g. gaming addiction or specific phobias) also struggled to find the specific help and support they needed.
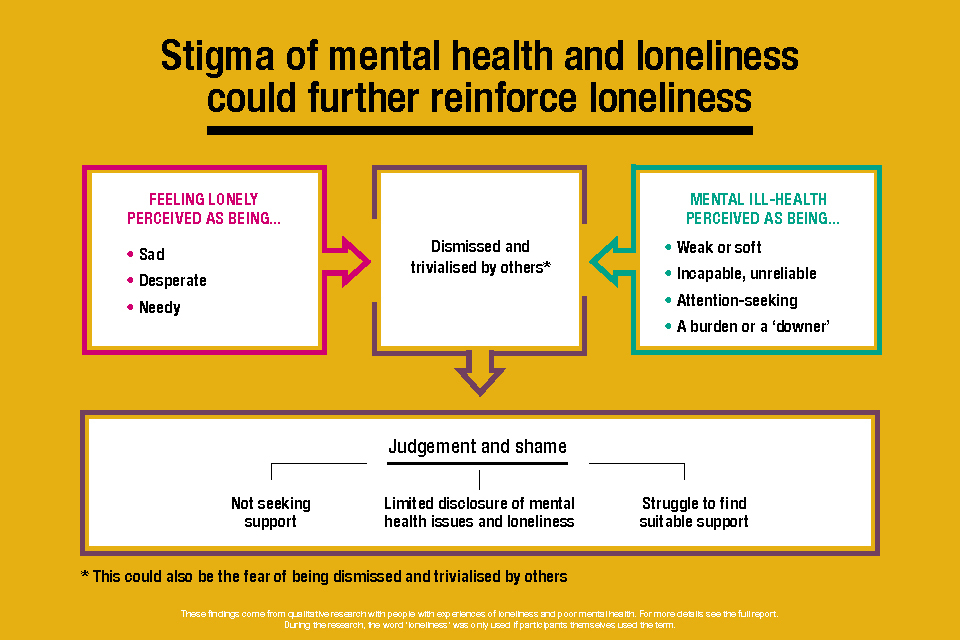
A visual showing how the stigma of mental health and loneliness could further reinforce loneliness as participants felt their feelings were dismissed or trivialised by others.
5. Experiences of loneliness across life stages
This chapter presents findings on how key life events, as well as social expectations associated with different stages of life, affect experiences of loneliness and mental health. Across the sample, participants identified key events that they associated with episodes of loneliness or poor mental health. Some of these were linked with life stages, while others could occur at any stage of life. Key events were associated with changes to circumstances or transitions that changed lifestyles. However, in addition to these, there were also social expectations that came with certain life stages which could compound these changes.
5.1 Key events across life stages
Events that are known to be associated with loneliness and isolation were identified by participants across the sample and could occur at different stages of life. These included:
- breakdown of romantic relationships, including being cheated on by a partner
- bereavement particularly related to the loss of close family members or partners
- experiences of domestic violence within relationships
Some events, such as a decline in physical health, could happen at any stage of life but were more associated with certain stages such as the middle aged and retired stages. Changes to physical health triggered changes to lifestyles and affected people’s ability to do social activities that they had previously enjoyed.
5.1.1 Adverse childhood experiences
Across the sample, participants identified incidents and experiences that had occurred in their childhood or adolescence as key events that had impacted their experiences of mental health and contributed to their feelings of isolation, echoing findings of previous research.[footnote 18] Participants with experience of these types of events directly traced the onset of their mental health issues or their experiences of loneliness to these points in childhood. Across the sample these experiences included:
- experience of physical or sexual abuse
- emotional or physical neglect
- having parents who had mental health or substance abuse issues
- losing a parent as a child or in adolescence, including through suicide
The impact of this trauma could manifest at different stages of people’s lives in different ways. It could lead to estrangement from family members in later life, particularly if certain family members recalled the experience in different ways or if there was blame or recriminations within families. For participants who had experienced abuse at the hands of a parent, the death of that parent at a later point could trigger complex emotional responses. These experiences could be very difficult to share with social connections leading to feelings of isolation.
I think I felt that I couldn’t reach out for help because of the subject matter of what was making me feel so awful and what had happened.
– Female, parent of young child, anxiety
Subsequent experiences of trauma, such as sexual assault, could re-activate the trauma associated with these childhood experiences and lead to a decline in mental health and increased isolation. Stakeholders noted that neglect or abuse in early life could lead to people adapting the way they think and behave. These adaptations could make it more difficult for individuals to navigate relationships and be open to receiving help and support from others in later life. They explained that adverse childhood experiences could have a significant impact on the development of social skills like trust and could lead to feelings of shame, which acted as barriers to forming healthy social connections.
5.1.2 Young adults
The young adult life stage was a period of gaining independence and establishing an adult identity. Stakeholders explained that at this stage, young adults are trying to work out who they are and what group they want to belong to. This can mean that greater importance is placed on social relationships and fitting in with or being socially accepted by others. At this stage of life, a number of key events were identified by participants as affecting mental health and/or experiences of loneliness.
- Leaving the family home and living independently, sometimes alone, for the first time. This involved moving to a new, unfamiliar environment. Young adults who moved away from the family home to start university recalled how the sudden, extensive freedom and lack of routine could destabilise their mental health. They also explained that, contrary to the image of university students as highly social, it was easy to go a whole day without seeing anyone else when at university, particularly when learning moved online during the COVID-19 pandemic. However, one participant had managed to transition out of loneliness when moving to a new area by proactively making social connections at work, in a local church community, and through a pre-existing social contact who lived in the area.
- Missing out on a social circle by not moving into employment. Some young adult participants had mental health conditions (such as schizophrenia or BPD) that were so severe that they were unable to work. They therefore lacked a social network of work colleagues. One young adult described how, once she finished her college course and did not move on to employment, it was more difficult to maintain friendships with her college friends because they no longer had shared experiences.
It got harder just to talk [with friends]… (…) When we were at college there was always something that we would all be doing, so it was something easy to talk about.
– Female, young adult, schizophrenia and psychosis
Some of the social expectations associated with this stage of life were the pressure to achieve, as well as the pressures associated with finding their identity. Young adult participants were likely to feel pressure to achieve, whether in further education or work. For example, one young woman felt pressured by her mother to go to university even though she did not want to go. After starting the course, her mental health worsened and ultimately, she withdrew, which prompted feelings of failure. Young adults who did start university courses also felt a sense of failure if they encountered difficulties and had to defer a year or withdraw from the course completely. These pressures could affect people’s sense of their own identity and self-worth, which could be compounded by other struggles, such as coming to terms with homosexuality, precipitating feelings of isolation and poor mental health.
Young adulthood was also a time when people received a formal diagnosis for their mental health condition. While this could come about as a result of seeking support, it was also associated with negative experiences of having to navigate the healthcare system, feeling labelled, and having to come to terms with what their diagnosis may mean for the future.
5.1.3 Parents of young children
Having children, and the period when children are very young and dependent on their parents, is associated with a higher risk of experiencing loneliness. Stakeholders noted that many of the challenges associated with parenting are not widely talked about and that this is an area of life in which there is a lot of judgement. Stakeholders commented that parenthood is a transition that involves many changes, most obviously the change to lifestyle from having a young dependent child but also changes to personal identity and the couple relationship. It could also trigger feelings about people’s own childhood and any trauma that was associated with it. Stakeholders noted that ambivalent feelings about becoming a parent could be associated with feelings of shame or lack of self-worth.
For participants with young children, pre-existing mental health issues were often at the centre of accounts of loneliness, but key events and social pressures associated with this stage of life that exacerbated these feelings were identified. There were differences in the way these were experienced by male and female participants.
- Losing connection with a partner after the birth of a child. Participants, both male and female, described drifting apart from their partner when their children were young, leading to feelings of isolation. There were different reasons given for this: being busy with maintaining jobs while juggling caring responsibilities; as well as mothers being focused on the needs of the child. Where this had led to relationship breakdown, fathers described their distress in having less regular contact and connection with their children.
- Increase in stress due to caring responsibilities. Female participants described feeling a lack of support, with an expectation that they should be able to manage after the birth of children, even while undergoing physical recovery after traumatic births. The time needed for physical recovery could limit their ability to get out to socialise. This combined with other physical issues, such as a lack of sleep, contributed to an increase in stress and feeling isolated and could compound issues within a relationship. For fathers, this could manifest as feeling a greater sense of responsibility and the associated stress that came with this.
When my son was younger and I was working full time and at University, it was a time of great stress not only academically or due to work. But the expectations of being a good dad and a good husband. Things became very difficult, temper was shorter but a lot of that came from the lack of validation I received from my partner.
– Male, parent of young child, depression – diary entry
Participants also described having a lack of time to seek support when they were not coping well or when their mental health was suffering due to their caring responsibilities.
- Fertility issues and experiences of pregnancy loss. Female participants who had experienced issues getting pregnant or who had experienced pregnancy loss described this as a very isolating time. This was because they felt unable to share the experience with others due to feelings of shame. This experience made subsequent (successful) pregnancies an extremely anxious period.
- Experience of being pregnant or giving birth during the COVID-19 pandemic. Female participants who had been pregnant or given birth during the pandemic reported having less face-to-face contact from healthcare professionals and not having their partner with them throughout their ante-natal care. After the baby was born, participants had less support and social contact from friends and extended family who could not visit, and had not been able to attend usual new parent activities such as mother and baby groups.
- Losing social contact with work colleagues while on maternity leave. Female participants also talked about losing regular social contact with their colleagues while on maternity leave, particularly in cases where they had for one reason or another not gone back to the same job.
Having young children is a period in life often associated with various social expectations around parenthood – particularly with respect to mothers who were expected to be able to ‘cope’ with it. These could leave people feeling isolated and unable to reach out for support. In addition, participants described that some of their friends assumed they were busy and did not want to be bothered, once again leading to people feeling alone. Participants who had become parents in their late teens or early 20s were more likely to feel different to and therefore isolated from both other parents, the majority of whom were older, and their peers, who had a very different lifestyle with fewer responsibilities.
5.1.4 Middle-aged people
Middle age has been highlighted as a time of increased loneliness and is the life stage associated with higher rates of suicide, especially among men. Stakeholders observed that this stage is significant because it is when people expect to have a more secure, stable and established life. For those who were parents with older children, who were sometimes struggling with their own issues, or who had grown up and left home, this was a time when difficulties finding or sustaining intimate relationships took on a growing importance. This was also a time when hormonal changes and ageing began to take their toll. There were a number of key factors that affected people’s mental health and experiences of loneliness at this life stage.
- Managing difficult family situations. Single parents felt overwhelmed by looking after children, working and managing the household by themselves. Parents of children with disabilities or special educational needs felt unable to go out or have time for themselves. Struggling to get support for their child’s needs added even more to the sense of having too much to deal with and contributed to feeling isolated and alone. Fathers who were estranged or denied access to their children felt that this was a key factor in their mental health issues, sometimes expressing a sense of guilt or shame about not seeing them. Often these situations had arisen after difficult relationship breakdowns, including in some cases, domestic violence.
- Establishing and sustaining intimate relationships. Participants who were single described difficulties finding and sustaining intimate relationships, partly because potential partners found it difficult to respond to their mental health condition. Experience of having been cheated on in the past could lead to a lack of trust. More widely, some participants in middle age began to lose hope that they would find a partner, or decided it was not worth the effort. For single parents, and those worried about an ‘empty nest’ this raised issues of who they would have as social support as they aged. This was especially the case for participants who had made their children the focus of their lives.
- Decline in physical health. Participants who had experienced illness in middle age or had a physical health condition or a disability were left feeling low and isolated. These feelings were particularly strong when partners or their social circle were still active by comparison, or they had previously been very fit and active themselves.
It’s been hard for me on my mental health because I was such a fit and active woman before it [getting ill] happened, because I was very independent. I feel like my life stopped at 44 when I got ill.
– Female, middle-aged, depression
Difficulties dealing with pain, poor mobility, or lack of disabled access to the local area led to depression, and sometimes to suicidal thoughts. Partners or family and friends could struggle to deal with this or show a lack of understanding or empathy.
- Changes to work routine. Being made redundant in middle-age, or retiring due to ill-health, also meant participants lost social connections and their sense of a work identity. This left them struggling with feelings of isolation and lack of purpose. Working from home during the COVID-19 pandemic or social distancing within the workplace had left some feeling they lacked the social connections and interactions they valued from the work environment. For instance, one female participant suffering from depression said that when working from home she just went to bed at 4pm when she finished work. Another described missing having lunch or tea breaks with colleagues due to social distancing requirements. Not working or being unable to work due to mental health issues could lead to feelings of shame, leading to more isolation. One participant described telling a new friend that both she and her husband were working as she did not want to be judged. However, this led to worries about the lie being found out.
5.1.5 Retired people
Retirement and older age are known to be when people are at risk of loneliness. However, a number of the factors described by participants in this group overlapped with those in the middle-aged group. Stakeholders noted that ageing and physical decline can affect people at different ages, affecting a person’s ability to engage socially. Retirement itself is associated with losing social connection with colleagues as well as a work identity. In addition, the deaths of friends or partners can leave people with fewer social connections. Being on a limited income (such as a pension) could also affect people’s ability to engage socially.
Many of these factors were echoed by participants.
- Retiring and leaving the workplace led to participants losing social connections with work colleagues and feeling more isolated. This could lead to people having a lot of time to fill, getting bored or feeling low, and having time to ruminate on problems or troubles in their life. This was exacerbated when romantic partners were still working and participants felt at a loose end. One participant explained in his diary that the weekend was good as it meant more time with his wife (who was still working).
I spend lots of time alone by necessity, because there’s nobody else here. I don’t have a lot of friends at the moment, because a lot of them have left us or moved away…
– Male, retired, depression
Retirement could also trigger other changes, such as moving to live in different parts of the country – either for a more peaceful lifestyle or to be near family. However, these moves meant leaving existing social community networks. Retiring was also sometimes unexpected, where people had experienced a sudden change to their physical health and could no longer work.
- Decline in physical health could limit people’s mobility or leave them with less energy and therefore mean that they were unable to do as much socially as they previously had. This physical deterioration could lead to a decline in mental health with participants spending time thinking about the things they were no longer able to participate in, which in turn could lead to social withdrawal. Other physical conditions left people feeling anxious and worrying about their health (one participant who had a heart attack described waking up every day thinking this day could be her last). Similarly, people worried about how to manage symptoms and the availability of important facilities like public toilets when they were out. Poor physical health had also meant some participants had shielded during the COVID-19 pandemic, contributing further to the isolation experienced at that time.
- Bereavement. The loss of partners, family members or close friends was also associated with loneliness and periods of poor mental health, particularly at this stage of life. Whether unexpected or not, the loss of a partner could have a particularly detrimental effect leading to intense loneliness and poor mental health. Participants described operating on ‘automatic-pilot’ for a year or more. One female participant described eventually joining lots of social activities and groups in order to keep busy and tackle loneliness - a proactive strategy that tended to be more common among female participants than among males. As noted in section 4.2.3, participants in this life stage group tended to minimise their own mental health issues, in part attributing this to the attitudes they had grown up with where mental health issues were ‘swept under the carpet’.
5.2 Other factors across life stages
There could be daily variations in how lonely people felt, and diaries revealed a number of more transient or temporary factors that could affect loneliness or mental health. The importance of current events was highlighted. The fieldwork period corresponded with the onset of the war in Ukraine, with participants commenting on the worry it provoked:
I feel anxious and terrified about the threat of war.
– Female, middle-aged, depression and GAD – diary entry
Other factors were more personal, such as significant dates and anniversaries of bereavements or miscarriages. Daily worries such as having a blocked drain, changes to children’s routines or receiving notice of rising electricity bills could also affect people’s outlook on a daily basis. Beyond these more transient factors, three other key factors emerged from participants’ accounts as having significant impact on recent experiences of loneliness and mental health. These were related to neighbourhoods, financial resources and the COVID-19 pandemic. We discuss each factor in turn below.
5.2.1 Neighbours
Stakeholders reported that loneliness was more prevalent in urban than rural areas and in ex-industrial areas. They explained that those who feel safe and welcome in their local community are less likely to experience loneliness than those who perceive themselves to be at risk of crime and anti-social behaviour.
This was echoed by participants in interviews, with the neighbourhood and community that participants lived in an important element in how isolated they felt. Across all life stage groups, feelings of vulnerability and despair were evident among participants who said they lived in ‘not-so-great’ areas, with high levels of anti-social behaviour. This was especially the case when they were unable to afford to move to nicer or quieter areas. Participants described disputes with neighbours that led to them feeling uncomfortable spending time in their own garden for fear of encountering them, neighbours who made noise at all hours of the night affecting their sleep, and young people who threw stones at their homes. One female participant who had left an abusive partner had been unable to move away from the area and described avoiding certain parts of the neighbourhood for fear of seeing her ex or his family.
Participants who had moved more recently as part of their retirement to be closer to family, or in an area of more beauty, described not liking their areas. People cited a lack of transport options or amenities, or missing the previous community they had around them (a feeling exacerbated in cases where the move corresponded with the onset of the pandemic). Not being able to access services was particularly isolating for those who did not drive. Reductions in bus routes had left people feeling cut off.
[The cinema] is on a shopping estate by the motorway and there aren’t any buses that go there anymore. So, you can’t go to the cinema, you can’t go bowling. The largest supermarket is also on that estate that you can’t get to without a car. I don’t drive any more so that’s out.
– Female, retired, depression
5.2.2 Limited financial resources
Having limited financial resources, whether as a result of being on a small pension, on benefits, on a low income or with high debts led to people feeling unable to participate in activities and feeling isolated as a result. This was reiterated by professional stakeholders who reported that loneliness was more prevalent among groups with a lower socio-economic status. This affected participants across life stages. One female participant described being unable to take her children for activities in half term due to limited money. A retired participant described feeling less connected to her son as she was unable to afford the activities he and his family could, and another talked of feeling judged by others for receiving benefits. Limited financial resources also prevented people from seeking mental health support privately when waiting lists were too long on the NHS.
5.2.3 The effect of the pandemic
Unsurprisingly, the COVID-19 pandemic and associated social restrictions had a significant impact on experiences of loneliness and mental health across the sample. It was identified as a recent significant period of loneliness and poor mental health. Most obviously, the pandemic had disrupted people’s face-to-face social activities and led to a loss of contact with friends and family. Although social contact had usually been maintained for a while by phone, messaging or video calls, over time participants described the circle of contacts as waning. Feelings of isolation had been particularly acute for those who were shielding due to poor physical health. This sense of isolation was compounded by the feeling that support from medical services had been withdrawn, leaving some with both physical and mental health conditions feeling quite vulnerable. In addition, as noted above, the social distancing rules had precipitated a change to many people’s working practices, such as an increase in working from home, or restrictions on the ability to socialise in the workplace. University students whose lectures moved online described feeling particularly isolated during this period. The social restrictions had been particularly difficult for those with families overseas who had been unable to travel. One male participant explained that he had previously travelled several times a year to visit his overseas partner but this had ended with the pandemic and during this time his physical health had declined leaving him afraid that he would not be able to travel again. A mother to a young child described missing her father and sisters who lived overseas especially as they had not been able to meet her baby.
In spite of the challenges, participants felt they had become accustomed to the lack of socialising and felt anxious about the lifting of restrictions. Participants described an increase in anxiety, both from the risk of catching COVID-19 (particularly for those with physical health conditions or who were caring for elderly relatives), but also due to returning to socialising, demonstrating how isolation can lead to mental health issues. Participants described losing the ‘confidence’ to socialise. Being forced to stay at home had made some participants feel quite safe and secure, and returning to socialising required confronting anxieties.
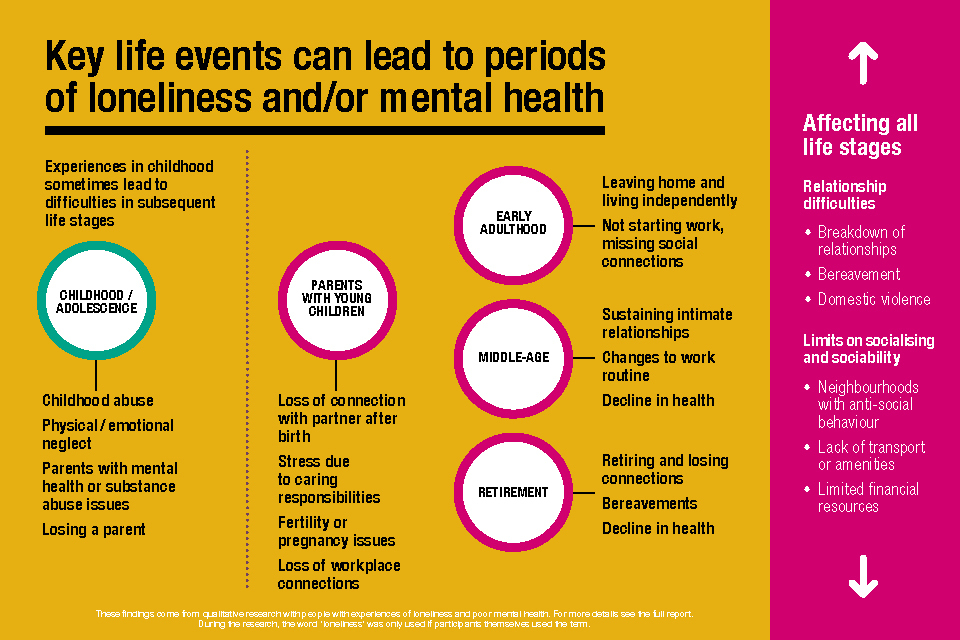
A visual outlining the key life events described in this chapter that can lead to periods of loneliness and/or poor mental.
6. Support and interventions
This chapter presents the main findings on support accessed by participants for both mental health and loneliness and explores views on what made these effective. It further sets out participants’ recommendations for how support could be improved. Many of the interventions identified by participants that supported improvements in mental health also ultimately helped reduce loneliness as participants were either able to share their mental health issues or better manage them. Similarly, interventions to address loneliness would have a positive effect on mental health through improving overall wellbeing.
6.1 Support and interventions for mental health
Participants had accessed a range of support and interventions from mental health services. This included support through their GP and specific issue-based organisations, such as Drug and Alcohol Services, Veteran support, rape crisis centres and domestic violence support organisations.
The types of interventions that had been accessed included talking therapies, cognitive behavioural therapy (CBT), dialectical behaviour therapy[footnote 19], eye movement desensitisation and reprocessing (EMDR)[footnote 20], occupational therapy, life coaching, hypnotherapy, medication, graded exposure hierarchy therapy[footnote 21], psychotherapy and psychiatric support. The extent to which participants found each form of support effective varied greatly, with some having found the intervention beneficial, while others had not.
Talking Therapies
Various factors contributed to the extent to which participants regarded talking therapies (including CBT, counselling and group therapies) as effective as outlined below. Factors that made talking therapies effective:
- A positive rapport with the therapist. A non-judgmental approach and a longer time period (i.e. not only six weeks of therapy) facilitated this rapport.
- Being well-matched with the therapist. Some participants wanted a therapist who would just listen to them, while others needed to be asked direct questions and have a more solutions-orientated approach.
- Having an independent and dispassionate person to talk to who was not directly involved in their situation.
- Identifying triggers, learning coping strategies and or being helped to ‘see things differently’.
- Group therapy was felt to be effective when participants felt less alone in their struggles. Group discussion could also provide a sense of hopefulness for the future when other group members were doing well.
Factors that made talking therapies ineffective:
- The therapist was viewed as patronising, belittling or insufficiently skilled.
- The therapist or counsellor did not understand the participant, their condition or their situation.
- The therapist and participant had not been matched on characteristics such as age and gender. This tended to be important in specific circumstances, for example, where a female participant had previously experienced abuse from a male.
- The therapy did not address the underlying causes of their mental health condition. For example, where therapy was unable to successfully address the link between physical and mental health conditions.
- When other members dominated the conversation during group therapy sessions.
Medication
Medication was felt to have been effective for participants when it helped them get through a difficult period, reduced the symptoms of their mental health condition (such as experiences of low mood, anxiety and obsessive thought patterns) and helped balance their moods, enabling them to interact with others or carry out day-to-day activities. In contrast, medication had not proved effective for everyone or had sometimes required much trial and error to get right. Alongside this, participants chose not to seek medical intervention due to effects of feeling ‘nothing’ and like a ‘zombie’ or other negative side effects such as weight gain.
Informal support and self-management
Participants drew on informal forms of support and self-management techniques for their mental health. This included: speaking to friends and family; spending time in nature; exercising; practising meditation and mindfulness; breathing exercises; self-help books; mental health charity websites; and doing things they enjoyed, such as art and music. Participants also sought out others facing similar issues, whether online (YouTube and social media) or people they knew personally. Pets were further highlighted as important where they felt that their pets were ‘there for them’, ‘dependent’ on them and made them leave their house. In some cases, worrying what might happen to a pet had prevented suicide attempts.
6.1.1 Suggestions for improving mental health support
Participants identified a number of barriers to accessing effective mental health support through health services. These included: the perception that GPs do not have time and resources to provide support; poor monitoring of medication, exacerbated by the COVID-19 pandemic; and long waiting times for talking therapies and CBT, leading some to seek treatment privately. In addition, participants described difficulties finding the right treatment and support, which led to people being referred between services and a lack of continuity in care, and negative experiences when attempting to access support, either where staff were uninterested or unsympathetic or where they received no response from services. A range of gaps in mental health support provision were also identified.
- A lack of opportunities to speak to others with similar mental health experiences. Specifically mentioned was the ability to speak to those whose mental health had improved, and online anonymous forums dedicated to distinct experiences (such as emetophobia rather than phobias more generally);
- A lack of a central mental health service where effective communication between services takes place. The introduction of a caseworker who could help individuals navigate the complex support system and present them with all the different support options available was suggested;
- A general lack of mental health provision. As noted, long waiting times for NHS services put some people off seeking support through this route, instead seeking support privately (where they could afford to) or through charities. In some areas, a lack of services and charities was identified. Participants also commented that signposting often directed people to resources, like mental health charity websites, that were too general and did not actually provide practical support. A cycle of signposting was also described, where no practical support ended up being provided:
Signposting just leads to signposting at times and you just go from one signpost to another signpost to another signpost.
– Male, middle aged, depression, anxiety, OCD
6.2 Support and interventions for loneliness
Support around loneliness and connecting with others was not sought to the same extent that interventions for mental health were. Participants ranged from not having experienced any form of support to having participated in various activities which increased their social interactions. Interactions were both with new people and with their existing relationships. Both types of interactions led to reduced feelings of loneliness. Engagement in these activities was usually sought out by participants themselves. Generally, there were limited examples of participants having received formal support or signposting to initiatives tackling loneliness. Those who took part in activities to increase their social network tended to do so either through online methods or by joining in-person groups.
6.2.1 Online interactions
A range of online platforms were used by participants, particularly young adults and those with young families, to meet new people. For example, young adults described engaging with local Facebook groups which brought young people together for events. This, however, did not appear to be particularly effective, with participants only occasionally attending events, due to a lack of spare time and events taking place far away, meaning they had not developed any relationships. Participants with young children described engaging with social media groups and apps with the intention of meeting other parents. This appeared to be effective, with participants having developed lasting friendships.
6.2.2 Group activities
Participants discussed having joined various groups, clubs and activities (not specific to loneliness or mental health) which had enabled them to meet new people.[footnote 22] Although engaging with this form of indirect support was seen across young adults, middle aged and retired participants, it was predominantly accessed by those who were retired and those who had depression and anxiety. Examples of activities engaged in included: University of the Third Age; arts and crafts sessions; book clubs; church groups; Women’s Institute; sports groups; and volunteering. This was reflected by stakeholders, who discussed the role that volunteering could play in reducing loneliness.[footnote 23] This was echoed in our interviews, where volunteering was important in creating a sense of connectedness and belonging across the life stages. However, negative consequences on wellbeing were experienced when the participant was not needed for their voluntary work.
[when there is no volunteering work for me to do] my life just falls to pieces … because I’ve lost that structure, I’m not around people, I don’t feel as needed or wanted or as included…
– Female, young adult, depression, BAD
Engaging with these forms of activities were reported to have been particularly beneficial, and in some cases transformative, to participants’ lives. Attending group activities helped relieve feelings of loneliness by increasing social interactions and enabling participants to develop meaningful relationships with new people. As well as addressing feelings of loneliness, engaging in such activities was also felt to be beneficial for participants’ mental health. It provided them with structure and responsibility, and acted as a form of stress relief. This twofold outcome could explain why engagement in group activities was felt to be particularly effective.
Groups of any kind I think are great because even someone like me who classes himself as being largely a loner, I love that running group. It’s great. Just every week I run round with somebody different, have a chat while you’re going round
– Male, retired, depression
However, where hobbies were not typically carried out in a group, such as reading, baking and photography, participants felt they had limited ability to connect with others through their interests, stopping them from engaging in such support.
6.2.3 Support from existing relationships
Spending time with people they had existing relationships with was discussed by participants as a form of support they turned to when feeling lonely. It was highlighted that just being around loved ones, even without talking, often made participants feel less alone. This was particularly beneficial where similarities were shared, such as both having experience of the same mental health condition. Young adults, parents with young children and middle-aged participants tended to turn to this form of support, whereas those who were retired did not report doing so to the same extent. The companionship participants received from their pets further helped reduce feelings of loneliness.
6.2.4 Formal support
More formal forms of support which could help alleviate feelings of loneliness were experienced by participants, although examples of this were limited. These came in the form of university well-being groups, mental health day centres and a social prescriber. In most cases, however, they were deemed to be rather ineffective.
University well-being groups, where students meet and talk about their mental health and well-being, and mental health day centres provided participants with the opportunity to meet and socialise with others who had similar experiences. However, where the form of mental health intervention was not suited to the participant or where services closed, participants disengaged, therefore finding the support ineffective.
Although health services rarely signposted to initiatives tackling loneliness, there were examples where health professionals (such as counsellors) advised participants to join the group activities previously described. In one example, this was found to be extremely beneficial, resulting in a great improvement in wellbeing with the participant saying they wished their whole life had been like the last few years. The participant had also undergone a recent change in medication and counselling but attributed the significant improvements in their wellbeing mostly to the group activities.
In another example, access to a social prescriber (whose role was to refer the participant to a range of non-medical services and activities) was initially felt to be beneficial. This was because the participant became aware of a host of services aimed at increasing social connections that they had previously not heard of. However, after having contacted relevant services multiple times with no success, the participant eventually gave up. Although it was unclear in this case why the organisations had not responded, this highlights the need for services to have capacity to respond in order for social prescribing to be effective.
6.2.5 Barriers to accessing support for loneliness
Participants faced a range of barriers in accessing support that could help reduce feelings of loneliness, including health conditions, fear of judgement, time constraints and economic barriers.
- Health conditions. Physical and mental health conditions were one of the main barriers to accessing support for loneliness. For example, with regard to physical health conditions, migraines made socialising challenging, while conditions that limited mobility restricted the types of activities that participants could take part in. In terms of mental health, those with anxiety found group situations and meeting new people too challenging to engage with. Some participants found that moving to online platforms reduced this anxiety, whilst others found socialising online even more difficult. Participants further described not feeling comfortable going to places on their own, but whilst some were open to being accompanied to such activities, others would still find that too overwhelming.
When I was with the mental health group… both my doctors were very much trying to make me go to this group at the local leisure centre. It was people with similar experiences… and I chickened out every time because I was just too anxious
– Female, young adult, BPD and GAD
This highlights how simply providing the information may not be enough and that people with mental health conditions in particular may require further support to access these services.
- Fear of judgement. Concern over how others would perceive the participant when accessing these activities also acted as a barrier. In regard to support groups specifically targeted towards mental health, participants were uncomfortable that others in the group would know there was ‘something wrong with them’. They were also concerned about meeting someone they know personally, who would then perceive them as ‘crazy’. In relation to more general group activities (those not targeted towards mental health) there was apprehension in returning to sports clubs after the onset of physical health conditions, in fear that they would be mocked for not being as skilled as they had previously been.
- Time constraints. A further barrier was a lack of time to attend such activities. This was especially reported among young adults and parents with young children.
- Financial resources. Stakeholders discussed how people’s socio-economic status can act as a barrier in being able to take part in social activities. Although participants did not explicitly mention financial barriers, the affordability of group activities was raised (see section 6.3).
6.3 Recommendations for tackling loneliness
Stakeholders were asked about the interventions they believed to be effective in tackling loneliness among those with mental health conditions. Due to the link between mental health and loneliness, they argued that interventions for loneliness should be informed by psychology and that there is a strong case for targeting interventions at people with both mental health issues and loneliness. Psychological interventions, such as CBT, mindfulness and behavioural activation, were highlighted as having stronger evidence base to support them.[footnote 24] It was suggested that these may work best when they preceded or were combined with social interventions (such as group activities or befriending). However, it was noted that there were few examples of psychological interventions being used solely to address loneliness (i.e. not also for those with mental health issues) with social interventions more common. Stakeholders also highlighted the need for very careful design of interventions so that they avoided being stigmatising and suggested that tailored interventions at key life stages (e.g. retirement) could be effective.
Participants were also asked about what could have helped them in tackling their feelings of loneliness. Suggestions were provided on how to address loneliness, focusing around formal support and engagement in group activities.
6.3.1 Support for family or friends
Participants who did not have supportive friends or family suggested that more support could be provided to the people in their life. This provision could equip friends and family with the skills needed to support and communicate with the individual struggling with their mental health. It was thought that this could help reduce how alone people with a limited support network feel, and was particularly relevant for participants whose significant others were unsupportive or dismissive of their issues.
6.3.2 Group activities
There was a view that taking part in group activities was an effective way of tackling loneliness. This included groups targeted towards the general population as well as for those experiencing poor mental health or loneliness.
- General groups around shared interests. Participants who had not accessed group activities acknowledged that they may benefit from doing so. It was suggested that being able to bring a friend along and providing a mixture of online and in-person groups could help people engage with these activities. Participants identified gaps in existing support where there were no appropriate local groups, including those relating to their hobbies (such as baking and woodwork) or groups relating to their personal characteristics and experiences (such as a woman’s running group, a mothers’ group, ethnicity-specific groups, faith-specific groups and groups for active people with disabilities). Introducing these group activities in the local area was suggested. The importance of having group-specific social interventions was reflected by stakeholders, who discussed how social interventions tailored to men or women can be more effective.
- Mental health specific groups. Participants suggested that attending activity groups specifically for people experiencing mental health issues could be an effective way of connecting with other people and reducing loneliness. The importance of having groups with people with similar mental health conditions and life experiences was emphasised, as it enabled a sense of shared understanding, making members feel more comfortable attending and engaging with one another. This was reflected by stakeholders, who discussed that connecting to people with similar experiences enabled people to know that they were not alone in their struggle. However, as discussed in section 6.2.1, stigma and fear of judgement can act as a barrier in accessing mental health specific group support, meaning that they would not be appropriate for everyone.
Suggestions for the type and form of these groups included those based around sports or activities or online groups where people could meet others who live locally. Members could build online connections with one another and decide whether to meet in person on their own terms. This was believed to be a less intimidating way of meeting new people for those who felt anxious about doing so.
I would love there to be some kind of sport group that links with the mental-health-type thing. A group I could join where you go and have a kick around with these mates and you’re all just having fun, and then afterwards you go for a coffee, or you go to the pub or something. It’s just an informal setting, but they’re all people that have struggled with similar stuff, and you chat to each other a bit about how your week was.
– Male, young adult, anxiety
A further recommendation was to introduce these group activities to people while they are waiting for support from mental health services, although such activities would need to be affordable. Beyond these suggestions, the research identified key points in a person’s life where additional support could help those with mental health conditions feel less lonely. These included after key life events such as a miscarriage, redundancy, retirement or the onset of physical health conditions or disabilities. It was after these events that participants’ mental health deteriorated, sense of loneliness increased, and where gaps in support became evident. While other key life events were also identified, these were associated with some specialist support, such as grief counselling or domestic violence support services, although the effectiveness of such interventions varied.
It appears that informal support provided through the voluntary and community sector could have a role to play in filling these gaps. For example, groups for those who have experienced pregnancy loss or experienced life-changing declines in physical health could help people feel less alone in their experience and provide a sense of support that people may not receive elsewhere. This would work particularly well if delivered by the voluntary and community sector as such initiatives could be very targeted to specific needs and provide an informal form of support not available through formal health services. Similarly, pre-retirement initiatives organised by workplaces and local social groups for retirees could support the transition out of the workforce and alleviate loneliness. However, barriers relating to the availability of information about such groups, the feelings of stigma associated with accessing them, and the support that those with certain mental health conditions might need to access them would all need to be addressed in order for them to be successful.
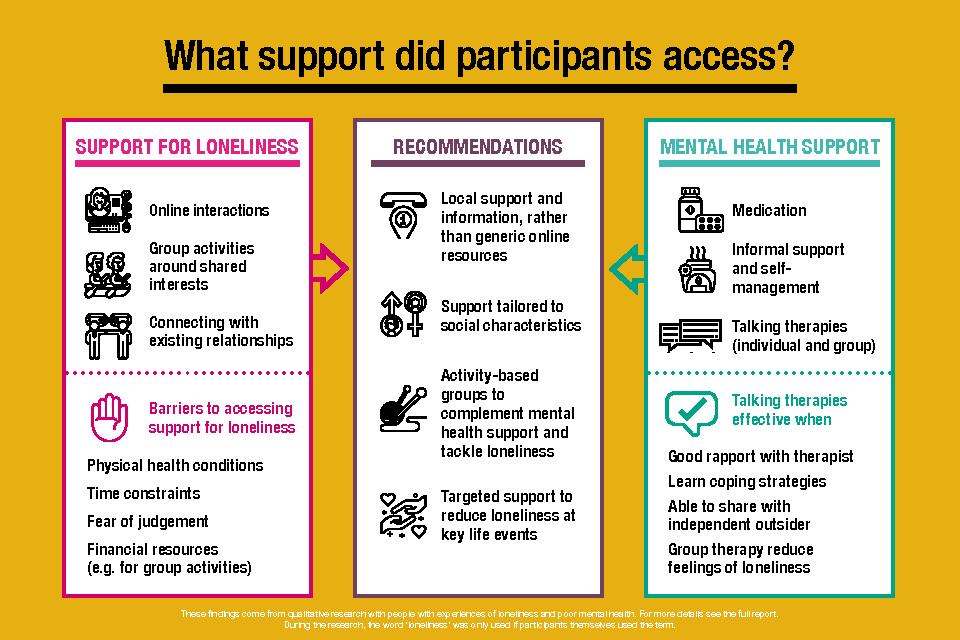
A visual outlining the different types of support participants in the research study accessed for both their mental health and their feelings of loneliness.
7. Acknowledgements
The authors would like to thank colleagues at the Department for Digital, Culture, Media & Sport, particularly Adam Jenson, Jasmin Keeble and Daisy Sherratt who provided valuable input and support throughout the project. We would also like to thank Professor Manuela Barreto of the University of Exeter for providing her expertise throughout the project. Finally, we are very grateful to all of the people who gave up their time to participate in this research and share their experiences and views with us.
8 References
Barreto, M., Victor, C., Hammond, C., Eccles, A., Richins, M. T., Qualter, P. (2021). Loneliness around the world: Age, gender, and cultural differences in loneliness. Personality and Individual Differences, 169
Cacioppo, J.T., Hughes, M.E., Waite, L.J., Hawkley, L.C., and Thisted, R. (2006). Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140–151.
Lim, M. H., Rodebaugh, T. L., Zyphur, M. J., & Gleeson, J. F. M. (2016). Loneliness over time: The crucial role of social anxiety. Journal of Abnormal Psychology, 125 (5), 620–630.
Matthews, T., Caspi, A., Danese, A., Fisher, H.L., Moffitt, T. E., & Arseneault, L. (2020). A longitudinal twin study of victimization and loneliness from childhood to young adulthood. Development and Psychopathology, 1-11, doi:10.1017/S0954579420001005
Newheiser, A.-K., & Barreto, M. (2014). Hidden costs of hiding stigma: Ironic interpersonal consequences of concealing a stigmatized identity in social interactions. Journal of Experimental Social Psychology, 52, 58–70. https://doi.org/10.1016/j.jesp.2014.01.002
Nowland, R., Talbot, R., & Qualter, P. (2018). Influence of loneliness and rejection sensitivity on threat sensitivity in romantic relationships in young and middle-aged adults. Personality and Individual Differences, 131, https://doi.org/10.1016/j.paid.2018.04.047.
Ritchie, J et al. (2014) Qualitative Research in Practice; London: Sage.
Wang, J., Mann, F., Lloyd-Evans, B. et al. (2018) Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry 18, 156.
Ye, Y. and Lin, L. (2015). Examining Relations between Locus of Control, Loneliness, Subjective Well-Being, and Preference for Online Social Interaction. Psychological Reports, Vol 116, Issue 1. https://doi.org/10.2466/07.09.PR0.116k14w3
Young Minds (2020). Coronavirus: Impact on young people with mental health needs[pdf]
Appendix A: Methodology
Given the exploratory and sensitive nature of the research aims, the study used a qualitative approach. This included:
- six scoping interviews with professional expert stakeholders
- 37 in-depth interviews with people experiencing mental ill-health and loneliness; including
- 14 of the 37 in-depth interviewees who also completed five online diary entries over the course of two weeks prior to the interview
Ethics
Ethical approval was sought via NatCen’s ethics committee, which complies with UK Research and Innovation, Government Social Research and Social Research Association guidelines and standards. Particular attention was paid to:
- Informed consent to take part. Professional stakeholders and research participants were made aware of the nature of the study and the type of topics to be covered before being asked to agree to take part. At all stages it was stressed in writing and verbally that participation was voluntary. For the main fieldwork, a staged approach to consent was used. Firstly, information about the study was sent to prospective participants by email, asking them to opt in. If they opted in, they were then contacted by NatCen’s Telephone Recruitment Unit (TRU) or our trusted recruitment agency. Participants were screened to ensure they met criteria for inclusion and felt well enough to take part. Consent to take part was audio recorded following reiteration of key information about the study prior to the start of the interview. Participants who had completed diaries were asked following the interview if they were happy for the entries to be quoted in the report.
- Sensitive handling of the topics, including avoiding stress or harm to participants. The nature of the topic meant that there was a risk to participants by having to discuss upsetting experiences or circumstances. The study was conducted by experienced researchers who met prior to the start of the fieldwork to discuss potentially upsetting parts of the interview and how these should be handled. Researchers were led by participants in terms of the language used to describe ‘loneliness’ or ‘mental health’. Participants were told they did not have to talk about topics they did not want to, could take a break, or reconvene the interview at another time. They were also told they could have someone with them during the interview to support them if they wanted (although no one took up this offer). All participants were sent a leaflet after the interview listing helplines and organisations they could contact if the interview had raised difficult issues for them.
- Disclosure. Participants were advised that the researcher may have to disclose information from the interview to someone else if we believed they or someone else close to them was at risk of harm in line with NatCen’s Disclosure policy. In the event, no issues arose that required researchers to take this path.
- Avoiding stress or harm to researchers. All researchers were told to check in with a senior researcher following their interviews, to debrief. Issues or difficulties arising from the interviews, or integration of diary information into the interviews, were discussed at weekly project team meetings.
- Ensuring inclusivity of participation. In addition to purposive sampling, every effort was made to ensure that participants could take part in ways most suitable and convenient for them. They were given the opportunity to take part by phone or video interview using MS Teams. Interviews took place during daytime and evenings. An incentive was offered for the interview as a thank you and a recognition of the participant’s time. An additional incentive was offered for online diary entries, recognising the additional work involved. Participants who were part of the ‘young family’ group struggled completing five diary entries, and so were given the option of completing fewer entries for a reduced incentive.
Recruitment
Professional stakeholders
A long-list of possible expert stakeholders or organisations were identified by DCMS who provided contact details and followed up by NatCen researchers. These included experts from mental health charities; organisations that support people at key life stages; and those working specifically on loneliness, including academics.
Fieldwork with participants experiencing loneliness
Research participants were recruited in two ways:
- via NatCen Panel – analysis of recent waves of NatCen Panel participants who had consented to recontact for further research showed approximately 125 people reported experience of mental health conditions and loneliness in recent waves. These participants were emailed and invited to opt into the research. They were contacted and screened by NatCen TRU (as outlined above). These participants were invited to take part in an interview only, or an interview and diary entries.
- via trusted recruitment agency – Propeller Field contacted people on their database with information about the research, inviting them to respond if they were interested and fit the selection criteria. Propeller screened the participants in the same way as the TRU. These participants were invited to take part in interviews only.
Sampling
As is the quality standard in qualitative research, the aim was not to be statistically representative of the wider population, but to sample the range and diversity of experiences and circumstances relevant to research aims within the target population. Participants were only included in the study if they currently reported being lonely (sometimes or often, measured on the direct and indirect scale). In addition to this, participants were selected based on the following primary sampling criteria:
- mental health condition (principally, depression, anxiety and/ or other)
- key life stages identified in prior research linked with loneliness (young adults, parents of young children, middle age, retired)
- gender
Secondary selection criteria which we also monitored, involved: age, whether mental health issues arose now or in the past, subjective assessment of severity of their mental health condition, employment status, and whether they were currently in a long-term relationship.
Achieved sample
The achieved sample against primary section criteria for interviews and diary elements are shown in table A.1 below.
| Criteria | Diary | Total interviews | |
|---|---|---|---|
| Mental health condition | Depression | 13 | 29 |
| Anxiety | 13 | 30 | |
| Other | 7 | 13 | |
| Life stage | Young adults | 3 | 10 |
| Parents of young children | 1 | 8 | |
| Middle-aged | 7 | 9 | |
| Retired | 3 | 10 | |
| Gender | Man | 10 | 19 |
| Woman | 4 | 18 | |
| Total | 14 | 37 |
Fieldwork
Interviews were conducted for professional stakeholders in January 2022, and for the main stage fieldwork between February and March 2022.They were carried out by telephone or video call using topic guides agreed with DCMS, and with advisory academic input. Findings from the professional stakeholders’ interviews were also used to shape the form and topics for main stage data collection. Interviews with stakeholders lasted up to 45 minutes. Interviews with research participants lasted between 60 and 90 minutes and were scheduled in advance. This allowed time to build trust and rapport with the participant and fully explore their experiences. 37 main stage interviews were conducted in total.
Diaries: in addition to the interviews, 14 participants also completed an online diary over a two-week period prior to their interview. Participants were provided with a personal web link to their diary and guidance suggesting they concentrated on how they were feeling on certain days, what influenced those feelings, or a reflection of how they were felt after one or two weeks. Entries were limited to approximately 700 words each. The entries were used during the interviews to stimulate discussion, and to explore how they related to participants’ broader experiences of mental health or feelings of connection to others. The entries helped to surface issues they were not so easily raised through the interviews alone.
Analysis
Interviews were transcribed verbatim and charted using NatCen’s Framework approach for qualitative data analysis (Ritchie et al, 2014) in NVivo. The Framework approach uses a ‘matrix’ to conduct case-and-theme-based analysis by identifying key topics emerging from the data and summarising data from each participant under each topic. This generates rich insights by systematically and comprehensively mapping the data. The facility in NVivo which allows summarised data to be linked to relevant points in individual transcripts also allows further analysis required.
-
Retired participants ranged in ages but were all over 50. While some participants had retired earlier than 65 on a voluntary basis, others had retired on health grounds and were sometimes receiving disability benefits. ↩
-
Our sample of young parents only included individuals in heterosexual relationships or single parents so this may not reflect the experience of other types of relationships. ↩
-
Within the sample, retired participants ranged from people in their 50s to 70 and over. While some participants had retired earlier than 65 on a voluntary basis, others had retired on health grounds and were sometimes receiving disability benefits. ↩
-
A connected society A strategy for tackling loneliness[pdf] ↩
-
Ibid. ↩
-
Ibid. ↩
-
Cacioppo et al., (2006); Lim et al., (2016) and Wang et al. (2018) as found in the Tackling Loneliness Evidence Review. ↩
-
DCMS 2021. Wellbeing and Loneliness - Community Life Survey 2020/21 ↩
-
NatCen’s Framework approach for qualitative data analysis The Framework approach uses a ‘matrix’ to conduct case-and-theme-based analysis by identifying key topics emerging from the data and summarising data from each participant under each topic. See Ritchie et al, (2014). ↩
-
The sample included those who reported being lonely ‘sometimes’ as well as ‘often’. This was assessed using Measuring loneliness: guidance for use of the national indicators on surveys, the ONS standardised indirect and direct measures of loneliness ↩
-
Tackling Loneliness Strategy. ↩
-
As a result of these differences in understanding the ONS recommends using both direct and indirect measures when asking about loneliness. ↩
-
Anxiety can take different forms and be associated with other conditions such as phobias, OCD, or PTSD. Some commonly diagnosed anxiety disorders include: Generalised Anxiety Disorder and social anxiety disorder ↩
-
This has also been associated with feelings of loneliness, see Campaign to End Loneliness (2020). ↩
-
As also found in Newheiser, A.-K., & Barreto, M. (2014). ↩
-
This has been found in other studies for example, Nowland et al. (2018). ↩
-
The literature distinguishes between those with an internal locus of control versus an external one where people think events in their lives are beyond their influence. For an example of how this has been applied see Ye and Lin (2015). ↩
-
See for example, Matthews et al (2020). ↩
-
Dialectical behaviour therapy is a talking therapy based on CBT which is specifically adapted for people who feel emotions very intensely ↩
-
EMDR is a form of talking therapy that helps the brain reprocess memories of a traumatic event so the negative images, emotions and physical feelings they cause have less impact. ↩
-
Graded exposure hierarchy therapy can be a self directed or led therapy through which phobias are addressed by staged and supported exposure to the issue of concern. ↩
-
As also found by Birken et al (2022). ↩
-
The Co-Op Foundation (2016). Trapped in a bubble: An investigation into triggers for loneliness in the UK ↩
-
Although it was noted that this may be to do with these interventions having undergone more evaluation. ↩
