HPR volume 19 issue 10: news (30 and 31 October 2025)
Updated 19 December 2025
Trends in diagnoses of scabies at sexual health services in England, 2014 to 2024
Scabies is a parasitic infection of the skin caused by the Sarcoptes scabiei mite, which buries into the skin and causes intense itching and rashes (1, 2). Transmission from person to person occurs through close physical contact including, but not exclusively, sexual contact.
Those who experience genital scabies may go to a sexual health service (SHS) for a sexual health check (3) and the descriptive analysis presented in this report uses data from GUMCAD, the national STI Surveillance system in England, to assess trends in scabies diagnoses at SHSs from 2014 to 2024. This report shows annual increases from 2021, markedly larger since 2023.
Diagnoses at SHSs can only provide a partial picture of the overall diagnoses across the country, but the SHS data could provide an indication of the wider trends in scabies diagnoses in England (2, 4).
Although there is limited data to quantify the overall scale of detections across all healthcare settings, indications of a wider rise have been seen within real-time syndromic surveillance, which can track scabies-like symptoms across some NHS health care services. This includes reporting from general practice surveillance, such as the Royal College of General Practitioners Research and Surveillance Centre, which has shown that scabies consultations have recently been higher than in previous years across all Regions of England (5).
The key findings of this report are as follows:
- there was a 44% increase in scabies diagnoses at sexual health services between 2023 and 2024 (4,872 in 2024, up from 3,393 in 2023), with diagnoses in 2024 exceeding those in 2019 (prior to the COVID-19 pandemic)
- increases were reported in all UKHSA public health regions between 2023 and 2024, with most 2024 diagnoses reported in London (34%)
- 41% of all SHS scabies diagnoses in 2024 were in people aged 20 to 24
A breakdown of cases by gender, age and region is provided below, as well as a proxy assessment of the prevalence of suspected persistent scabies in England based on SHS data.
Trends in scabies diagnoses
SHS data has shown the following annual trends:
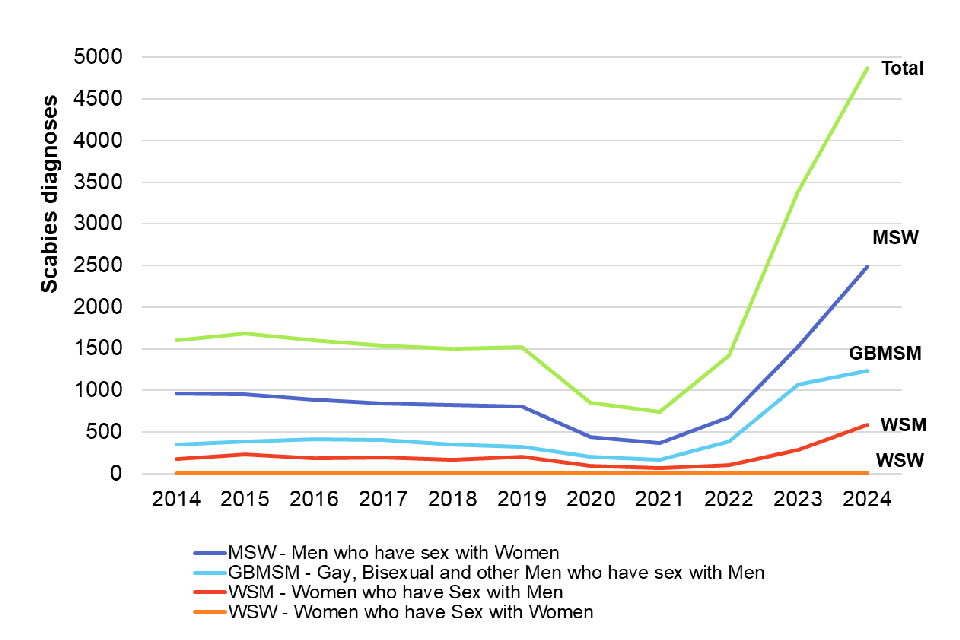
- from 2014 to 2019, the overall trend in scabies diagnoses was relatively stable, at around 1,500 diagnoses a year (figure 1)
- the number of scabies diagnoses decreased during the COVID-19 restriction period, reaching a low in 2021 (n=743)
- in 2022, diagnoses returned to 2019 (pre-COVID pandemic) levels; 1,421 compared to 1,516 in 2019
- however, 2023 saw a marked increase to 3,393 diagnoses, and in 2024 there was a further increase in diagnoses, reaching 4,872
Figure 1. Number of scabies diagnoses by gender and sexual orientation: England, 2014 to 2024
Diagnoses by gender identity and sexual orientation
In 2024, over three quarters of scabies diagnoses (81%, n=3962) were amongst men (figure 2). Heterosexual men had the highest number and proportion of scabies diagnoses accounting for half in 2024 (51%, n=2489). There was an increase of 962 diagnoses between 2023 and 2024 in this group.
The number of scabies diagnoses in heterosexual women, while lower overall, doubled between 2023 and 2024 (from 288 to 589). Women who have sex with women (WSW) maintained the lowest diagnoses percentage, consistently, from 2023 at 0.3% of the annual total.
Diagnoses by age
The age profile of scabies diagnoses at sexual health services is relatively young, with a median age of 24 and a range of 15 to 87 years. Women diagnosed with scabies have a slightly lower median age (23) than men (24).
Those aged 20 to 24 years made up around 41% (n=1994) of SHS scabies diagnoses in 2024, and those aged 25 to 34 years made up 31% (n=1,495).
Figure 2. Number of scabies diagnoses by age: England, 2024

Diagnoses by UKHSA region (2024)
The UKHSA public health regions with the highest number of SHS scabies diagnoses in 2024 were London (n=1,670) and the South East of England (n=714) (figure3).
The largest regional percentage increase in SHS scabies diagnoses from 2023 to 2024 was in the North East of England – a 92% increase from 160 to 307 diagnoses. The North East, South East and East Midlands all saw large percentage increases in scabies diagnoses between 2023 and 2024 (92%,62% and 77% respectively).
Figure 3. Number of scabies diagnoses by UKHSA region: England, 2024

Persistent scabies infections
Given anecdotal reports from clinicians suspecting an increase in persistent scabies infections (an individual reattending a sexual health service with scabies symptoms after having been prescribed treatment), the total number of scabies diagnoses per person per year (not considered as part of the same episode) was calculated as a proxy for persistent infection to assess the contribution of these to the overall increase in diagnoses seen (6).
This showed that up to 2022, around 2 to 3% of the diagnoses per year were persistent infections. In 2023 this increased to 6%, followed by a further increase in 2024, where 9% (443 out of 4,872) of all scabies diagnoses were persistent infections (figure 4). Although this is an increase in the proportional contribution of persistent infections over time, it accounts for a relatively small proportion of the overall increase in diagnoses observed.
Regionally, London saw the greatest number of persistent infections (226 out of 443 cases; 51%) in 2024, with the second highest number seen in the South East (73 out of 443 cases; 16%).
Figure 4. Peristent scabies diagnoses at sexual health services as a percentage of total scabies diagnoses: England, 2014 to 2024

Public health actions to control scabies
UKHSA has issued guidelines for the management of scabies cases and outbreaks in communal and residential settings, while the British Association for Sexual Health and HIV has scabies management guidelines for sexual health services (2). UKHSA recommends diagnosis and treatment of suspected cases as soon as possible, as well as contact tracing for close contacts up to 8 weeks prior to diagnosis (5). If 2 or more epidemiologically linked cases occur within an 8 week period involving a closed setting (such as a care home, residential facility or prison), the local health protection team should be contacted for advice and support.
This report was prepared by Giulia Habib Meriggi, Stephanie Migchelsen, Alex Elliot, Hamish Mohammed and Katy Sinka on behalf of UKHSA’s Blood Safety, Hepatitis, Sexually Transmitted Infections (STIs) and HIV Division.
References
1. Rosumeck S, Nast A, and Dressler C (2018). ‘Ivermectin and permethrin for treating scabies’. Cochrane Database of Systematic Reviews
2. Morris G, and others (2025). ‘British Association for Sexual Health and HIV national guideline on the management of scabies in adults’. International Journal of STD & AIDS: volume 36, pages 516 to 532
3. UKHSA (2025). ‘Sexually transmitted infections and screening for chlamydia in England: 2024 report’
4. UKHSA (2025). ‘Guidelines for the management of scabies cases and outbreaks in communal residential settings’
5. RCGP (2025). ‘Research Surveillance Centre: public health data’
6. Broster B, Clarke A, Iwuji C. and Soni S (2024). ‘Scratching beneath the surface: an evaluation of the management of scabies 2017 to 2023’. International Journal of STD & AIDS: volume 35, pages 616 to 619
Joint NHSBT and UKHSA Epidemiology Unit annual report in summary
The latest annual report of the joint NHS Blood and Transplant (NHSBT) and UK Health Security Agency (UKHSA) Epidemiology Unit, ‘Epidemiology Unit: annual review’ has been published on the NHSBT website.
Since 1995, the joint NHSBT-UKHSA Epidemiology Unit has worked in collaboration with the UK and Republic of Ireland blood services, UK Health Security Agency, wider NHS, academia and other external partners to protect recipients from transfusion-transmitted infections and help ensure donors are respected at every stage of their journey.
This year’s review highlights how these partnerships helped deliver important epidemiological evidence to guide blood safety policy and respond to emerging threats throughout 2024.

Blood donor selection rules aim to allow as many donors as possible to give blood while maintaining the safety of the supply. In 2024, approximately 964,000 volunteer blood donors aged 17 and above gave a whole blood donation in the UK. Among almost 1.8 million blood and apheresis donations screened, there were 287 donors with a donation confirmed positive for markers of acute HBV (4), chronic HBV (59), occult HBV (6), HCV (21), HIV (10), HTLV (8) or syphilis (181) including 1 donor with occult HBV/syphilis and 1 donor with HIV/syphilis.
In 2024, 10 donors seroconverted within 12 months of a negative donation: 6 with HIV and 4 with acute HBV, an increase from 2023 (2 HIV and 3 acute HBV). In 2024, 8 out of 10 seroconverting donors were White, age range 31 to 53 years including 6 male donors, 4 reporting sex between men. Of the 6 donors who seroconverted for HIV, there were 3 men and 3 women. Two reported sex between men; 1 was ineligible, having not reported anal sex and both male and female partners in the last 3 months, the other was eligible, but their partner was using HIV prevention medication (PrEP). Four reported sex between men and women including 1 woman with very recently acquired HIV, identified by Nucleic Acid Testing (NAT) alone, who did not report information that may have made them ineligible. The small increase in HIV in repeat donors may reflect that ‘HIV testing in heterosexuals in the general population has not recovered after the COVID-19 pandemic’.
Of donors with markers of infection, 25% (73/287), including 20 repeat donors, were ineligible to donate due to: history of infection (60), sexual behaviour (4) or both (2), HIV prevention medication with (1) and without history of syphilis treatment (2), injecting non‑prescribed drugs (1) or a medical history (3) they should have reported before donating. This is an increase from 16% (32/206) in 2019, due to an increase in the number donating with treated syphilis. Research in collaboration with the University of Nottingham on the PROMPT (Prompts to Reduce Omissions in deferral or testing for Malaria, Past infection and Travel) study will help to understand what might help donors disclose information before donating.
The low number of HBV, HCV and HIV seroconverters detected in repeat donors (within 12 months of their previous donation) maintained the very low chance of non-detection on routine blood donation testing, known as the residual risk. In 2022 to 2024 the overall risk was estimated to be around 1 in 1 million donations screened; most risk from HBV. It is estimated that an early window period infection may allow approximately 2 HBV per year, 1 HIV every 6 years, and 1 HCV every 59 years, to be missed.
The introduction of hepatitis B core antibody (anti-HBc) screening in the UK led to the withdrawal of 1,875 donors in 2024 due to past exposure to hepatitis B, including 3 with occult, DNA-detected hepatitis B virus (HBV). While this has enhanced safety, it has disproportionately impacted Black and Asian heritage donors.
Additionally, there were 417 (1 in 4,284) donations confirmed positive for hepatitis E virus (HEV) and discarded. While this is a higher number than all other viruses detected, there are no specific donor selection rules to exclude those at risk for HEV as locally acquired cases in the UK are mainly foodborne. HEV positive donors can return to donate after recovery.
In 2024 across England, Scotland and Wales, 146,445 blood donors were invited by their blood service to take part in an anonymous online survey conducted by UKHSA in collaboration with the University of Nottingham. The survey was conducted as part of post-implementation monitoring of FAIR (For the Assessment of Individualised Risk) to assess the impact of the policy on donors and understand more about who is donating. A total of 23,861 donors (16.3%) participated in the survey, with representation from a diverse range of responders. The majority were repeat donors (90%), most identified as female (53%), and 95.5% identified as White heritage. Compared to the overall donor population, younger donors, first-time donors, males, and individuals from Black, Asian, or Mixed heritage were under-represented among responders. Donors not taking the survey may have different risk profiles and experiences to responders. Nonetheless, there was some participation from a range of diverse groups and most responders donated while eligible to the FAIR policy.
TTI and lookback investigations support the UK blood services in monitoring blood safety and haemovigilance by identifying donors and recipients potentially at risk. All suspected transfusion-transmitted infections (TTIs) investigated by the UK blood services are reported to the NHSBT and UKHSA Epidemiology Unit for monitoring and have formed part of the Serious Hazards of Transfusion (SHOT) haemovigilance scheme since 1996. In 2024, there were no confirmed bacterial TTI among 118 investigations of suspected transmission; the last confirmed bacterial TTI was identified in 2015. In addition, in 2024, there were no confirmed viral TTI among 18 investigations of suspected transmission and lookback investigations in England in 2024 did not identify any transfusion transmissions. Hospital engagement and collaboration are key to ensure those affected are promptly identified, tested and referred for appropriate care. For more information see Annual reports on the Serious Hazards of Transfusion (SHOT).
Bacterial screening of platelets confirms very low rates of bacterial contamination in platelets, and clinically significant bacteria identified in England continue to remain at low levels. Screening of platelets cannot guarantee the absence of contamination, but transfusion transmission of bacterial infection is extremely rare.
The UK’s HTLV National Register is a collaboration between UKHSA, NHSBT and Imperial College Healthcare NHS Trust that assesses disease progression in a non-endemic population to guide public health policy. By 2024, 306 participants were recruited by blood services and HTLV specialist clinics, including 132 donors. Of the 283 participants who had markers of HTLV, 76% were female and 41% were of Black Caribbean ethnicity. Health and wellbeing questionnaires are completed at recruitment and every 2 to 3 years. Among 248 participants symptom-free at registration, over 1,839 person-years of follow-up revealed a low incidence of severe disease (1%).
Collaborative CJD surveillance between the National CJD Research and Surveillance Unit and the UK blood services since 1997 linked information to identify transfusion-transmission of variant CJD to 4 recipients before leucodepletion began in 1999. The Transfusion Microbiology Epidemiology Review (TMER) surveillance was a collaborative project which ceased in 2025. CJD surveillance activity up to 2024 identified 89 recipients of sporadic CJD donors with no evidence of sporadic CJD transfusion transmission to date, despite continuing searches in 2024.
A decrease in the number of deceased organ donors was seen in 2024, following some recovery to pre-pandemic levels between 2020 and 2023.Consented donors undergo mandatory testing for markers of infection, and some donors will also undergo discretionary testing depending on their exposure to risk criteria, including travel history. Reactive results are not confirmed. Screening identified 2 HBV, 25 HCV, 1 HEV, 54 HHV-8, 1 HTLV, and 10 syphilis reactive markers of infection in donors where organs were utilised for transplantation. Markers of infection are not necessarily barriers for transplantation.
NHSBT uses similar protocols for tissue and cord blood donors as for blood donors, but with individual NAT testing and phased FAIR policy implementation. Living surgical bone donors donate femoral heads, when undergoing elective primary hip replacement and generally have only one opportunity to give. In 2024 there were 767 donors. One was positive for HBV and 1 for HCV, with an overall rate of 261 per 100,000 donors, neither had evidence of recent infection. Cord blood collection targets ethnically diverse populations around London. In 2024 there were 135 cord blood donors, 1 was positive for HTLV, and 2 of 52 tested for positive for malaria antibodies. Deceased tissue donors give bone, skin, heart valves, corneas and tendons. In 2024, there were 2,684 donors. 15 were positive for markers of infection. These included 7 OBI, 3 HCV, 1 HCV/HBV co-infection, 1 HEV and 3 syphilis, approximating to an overall rate of 559 per 100,000.
The unit also undertakes horizon scanning to enable risk assessment of potential emerging infection threats that may impact the safety or sufficiency of the blood supply that relies on close links with public health and One Health surveillance. In 2024, 952 entries in the Emerging Infection Report were reviewed with spread of arboviruses, mpox and avian influenza accounting for a significant proportion of activity. In 2024 the Unit escalated items for immediate attention including: West Nile Virus in Spain prior to the May-November transmission season; locally acquired dengue in areas not covered by the GDRI (France, Italy, Spain, Iran, United Arab Emirates and USA); and the Marburg virus disease outbreak in Rwanda.
More information about the NHSBT/UKHSA Epidemiology Unit can be found at Epidemiology – Hospitals and Science – NHSBT.
Infection reports in this issue
Group A streptococcal infections: report on seasonal activity in England, 2025 to 2026
Vaccine coverage reports
RSV vaccine coverage report in older adults for catch-up cohorts in England: September 2025
