Health matters: giving every child the best start in life
Published 12 May 2016
Summary
Public Health England (PHE) wants to increase the proportion of children ready to learn at 2 and ready for school at 5.
This resource for health professionals and local authorities is about investing in early years services from pregnancy to age 2.
Why the early years are so crucial
What happens in pregnancy and early childhood impacts on physical and emotional health all the way through to adulthood.
Supporting good maternal health is important for safe delivery and good birth weight to give babies the best start. The prevention of adverse health factors in pregnancy is vital. Premature and small babies are more likely to have poorer outcomes.
The earliest experiences, starting in the womb, shape a baby’s brain development.
During the first 2 years of life the brain displays a remarkable capacity to absorb information and adapt to its surroundings.
Positive early experience is therefore vital to ensure children are ready to learn, ready for school and have good life chances.
It is shaped by a number of factors such as:
- sensitive attuned parenting
- effects of socio-economic status
- the impact of high-quality early education and care
Parents have the biggest influence on their child’s early learning. For example, talking and reading to a baby can help stimulate language skills right from birth.
Language skills help children to develop a range of cognitive skills that are crucial for their development, including working memory and reading skills. This can help prepare children so that they are ready to learn at 2 and ready for school at 5.

Infographic showing how to give every child the best start in life.
Making the case for investing
Investing in early years services can improve babies’ and children’s health outcomes including:
- early cognitive and non-cognitive development
- social development
- children’s readiness for school
- later educational outcomes
This is a crucial time when parents have contact with health and early years services before, and after, the birth of their child and are especially receptive to offers of advice.
It is an opportunity to support all families to give children the foundations for good health and extra support when needed. Identification and early intervention can identify families at risk of problems escalating into neglect and abuse.
The All Party Parliamentary Group for Conception to Age Two says that tackling problems associated with early life should be no less a priority for politicians and health and social care professionals than national defence.
A failure to act early comes at great cost, not only to individuals but to society as a whole.

Infographic showing the financial benefits of investing in early years services.
Foundations for promoting child health
The Healthy Child Programme
The Healthy Child Programme is the heart of public health services for children and families. It brings together the evidence on delivering good health, wellbeing and resilience for every child.
It sets out the schedule for services covering care from 28 weeks of pregnancy through to age 5. This is delivered as a universal service with additional services for families needing extra support, whether short-term intervention or ongoing help for complex longer-term problems.
The programme comprises health promotion, child health surveillance and screening, providing a range of services to families. These include:
- screening
- immunisation during pregnancy and childhood immunisations
- health and development reviews
- advice and support to help children’s physical and emotional development
The programme can ensure families receive early help and support upstream before problems develop further and reduce demand on downstream, higher cost specialist services. This programme is led by health visitors in collaboration with other health professionals.
Universal health and development reviews are a key feature of the Healthy Child Programme and take place at:
- 28 weeks of pregnancy
- within 14 days of birth
- 6 to 8 weeks
- 9 to 12 months
- 2 to 2.5 years

Infographic showing the elements of the Health Child Programme from pregnancy to age 2.
Healthy Start
Healthy Start is a UK-wide government scheme to improve the health of low-income pregnant women and families on benefits and tax credits through provision of vouchers and vitamin tablets and drops.
Healthy Start provides a great opportunity for health professionals and others working with pregnant women and families to offer encouragement, information and advice on issues such as healthy eating, breastfeeding and vitamins.
Healthy Start vouchers can be used to help families on a low-income buy some basic foods such as milk and fresh or frozen fruit.
Fit for pregnancy: pre-conception
Good health before and during pregnancy is vital. Pre-conceptual care includes giving advice on:
- full immunisation status
- vitamin D and folic acid
- reducing alcohol consumption
- giving up smoking
- contraception, family spacing and sexual health
Women who are trying to conceive should be advised to take 400 micrograms of folic acid each day. This can help to help prevent birth defects known as neural tube defects, including spina bifida.

Infographic showing ways of encouraging a healthy pregnancy.
Researchers believe that 1 in 6 (16.2%) pregnancies experienced in the UK are unplanned. Pregnancies in young, single women are most likely to be unplanned.
Recent experiences of smoking, having used drugs, and depression are more common amongst women reporting unplanned pregnancies. This highlights the need to help women and their partners to modify aspects of lifestyle that could harm their own health and wellbeing, and that of their child.
Teenage pregnancy
It is widely understood that teenage pregnancy and early motherhood are associated with:
- poor antenatal health
- lower birth weight
- higher infant mortality
Their health and that of their children is likely to be worse than average. Teenage mothers are less likely to finish their education, less likely to find a good job, and more likely to end up both as single parents and bringing up their children in poverty.
The number of teenage girls getting pregnant in England and Wales is continuing to fall. Latest statistics show that there were about 23 conceptions per 1,000 15 to 17 year old girls in 2014, compared to a high of 55 in 1971.
However, rates remain among the highest in Europe and variations continue between local areas, with reductions ranging from 30% to 70%.
Reducing the under 18 and under 16 conception rates is one of the key priorities of the Department of Health’s Framework for Sexual Health Improvement. This calls for local authorities to work with partners to use the evidence base and learning from successful areas to make further progress.
PHE has developed a range of resources to support teenage conception service improvement.
The Family Nurse Partnership provides targeted support for vulnerable young families and is an integral part of many local authorities’ early help offer.
Fit during pregnancy: staying healthy in pregnancy
A healthy woman is more likely to give birth to a healthy baby. Health professionals can support women, and their partners, to adopt positive health behaviours and reduce risk factors.
Nutrition and physical exercise
During pregnancy it is important to:
- eat a healthy diet and not to eat for 2
- take 10 micrograms of vitamin D each day throughout pregnancy and continue after the baby is born if the mother is breastfeeding
- continue to take folic acid up to week 12 of pregnancy
- advise on physical activity, signpost to trusted sources such as NHS Choices
Sexual health
Encouraging good sexual health during pregnancy is just as important, if not more so, than at any other time.
Some sexually transmitted infections (STIs) such as gonorrhoea can cause infertility. Others like HIV or syphilis can be passed to the baby in the womb or at birth.
All pregnant women are offered screening for Syphilis and HIV as part of routine antenatal care.
Vaccination
Pregnant women should be encouraged to have the seasonal flu vaccination which will protect both mother and baby.
Pregnant women are now offered a single dose of a pertussis containing vaccine (dTaP/IPV) between gestational weeks 16 and 32. This maximises the likelihood that the baby will be protected against whooping cough during the early weeks after birth until 8 weeks when the childhood immunisation schedule commences from birth.
Risk factors in pregnancy
There are a number of factors that can increase the risk of harm to the unborn baby and many of these are influenced by health inequalities.
Smoking during pregnancy
In England in 2014 to 2015, 11.4% of mothers were recorded as smokers at the time of delivery according to Health and Social Care Information Centre (HSCIC) data. This accounts for 70,880 out of 622,640 maternities.
There is wide regional variation in the number of women who smoke in pregnancy with mothers from areas of high deprivation more likely to smoke.
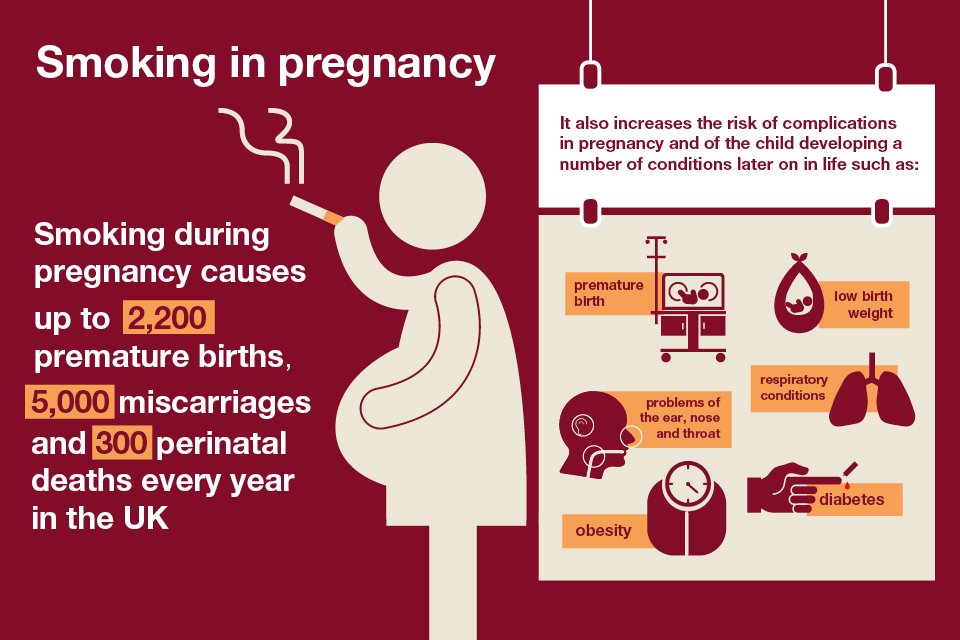
Infographic showing the risks of smoking in pregnancy.
Encouraging pregnant women to stop smoking during pregnancy may also help them stop smoking for good. This offers health benefits for the mother but also reduces exposure to secondhand smoke for the infant.
As the health gains are so large, even small successes with pregnant smokers, and their partners if they also smoke, are worth higher levels of investment.
Smokers should be informed that it is now illegal to smoke in a car, or other vehicle, with anyone under 18. This is designed to protect children and young people from the dangers of secondhand smoke.
National guidance from the National Institute for Health and Care Excellence (NICE) outlines interventions to support stopping smoking in pregnancy and after childbirth.
Use PHE’s early years profiles to see how your local area performs against 32 key indicators including, smoking status at time of delivery.
Drinking alcohol during pregnancy
Updated guidelines from The UK Chief Medical Officers now state that, for women who are pregnant or planning a pregnancy, the safest approach is not to drink alcohol at all, to keep risks to the baby to a minimum.
Drinking alcohol during pregnancy can increase the risk of miscarriage, low birth weight, as well as the risk of developing Foetal Alcohol Syndrome (FAS).
FAS is a serious condition, in which children have:
- learning and behavioural disorders
- restricted growth
- facial abnormalities
Social isolation and stress
Pregnancy can place a strain on relationships with:
- partners
- parents
- siblings
- friends
Supportive relationships during pregnancy are important for fostering good emotional wellbeing. They can reduce the risk of developing mental health issues during pregnancy, which can be an exciting but stressful time.
A number of studies suggest there can be an increased incidence of domestic abuse and violence during or shortly following pregnancy.
One in 4 women experience domestic violence over their lifetimes. Over a third of domestic violence starts or gets worse when a woman is pregnant.
Domestic violence and abuse can:
- make it harder for pregnant women to receive antenatal care
- impact on the development of the foetus and future development of the child
- increase the risk of premature birth
- increase the risk of low birth weight
NICE has produced guidance for health and social care commissioners, specialists in domestic violence and abuse staff and others who may bring them into contact with people who experience or perpetrate domestic violence and abuse.
Protecting health in infancy
Newborn Screening
The UK newborn screening programme aims to detect a number of rare but serious disorders present at birth and prevent serious consequences. Every newborn baby in England is offered screening.
The following 4 additional disorders have recently been added to the screening list:
- Homocystinuria (HCU)
- Maple Syrup Urine Disease (MSUD)
- Glutaric Aciduria type 1 (GA1)
- Isovaleric Aciduria (IVA)
Immunisation
After clean water, vaccination is the most effective public health intervention in the world for saving lives and promoting good health.
The UK has one of the best immunisation programmes in the world and recently added the meningitis B vaccine to the childhood immunisation schedule.
In the UK from September 2015, babies born on or after 1 July 2015 are being offered the meningococcal group B (MenB) vaccine as part of the routine immunisation schedule. Babies born on or after 1 May are being offered the vaccine as part of a one off catch-up campaign.

Infographic showing the importance of childhood immunisation.
Access to immunisation services should be improved for those with:
- transport difficulties
- language or communication difficulties
- those with physical or learning disabilities
NICE makes a number of recommendations for improving access such as:
- providing longer appointment times
- walk-in vaccination clinics
- services offering extended hours
- mobile or outreach services
Supporting the transition to parenthood
Secure attachment
Sensitive attuned parenting is the foundation of attachment. If a parent or carer is responsive to a baby’s signals and ‘takes turns’ in communicating with them from birth onwards, babies develop a secure attachment to the carer.
A secure attachment ensures a child will feel secure and reassured their needs will be met. This promotes emotional self-regulation and resilience into adulthood.
Preventing and intervening early to address attachment issues will have an impact on ability to form trusting relationships, resilience and physical, mental and socioeconomic outcomes in later life.
Breastfeeding

Infographic encouraging the promotion of breastfeeding.
Creating the right environment to promote and support breastfeeding is crucial. UNICEF Baby Friendly Initiative provides a robust evidence based framework to develop a whole system approach.
PHE’s Start4Life campaign provides parents and parents-to-be with trusted NHS advice on pregnancy and early years. This includes advice on supporting breastfeeding that health professionals should signpost new mothers to.
Use PHE’s child health profiles to see local level data on breastfeeding initiation and rates at 6 to 8 weeks.
Maternal mental health
Mental health issues can impact on a mother’s ability to bond with her baby and be sensitive and attuned to the baby’s emotions and needs. This can affect the baby’s ability to develop a secure attachment.
Many women are, however, ‘falling through the cracks’ and not getting the help they need for mental health problems during and after pregnancy.
The Centre for Mental Health and the Royal College of GPs highlighted that the biggest barrier to providing better support to women experiencing poor mental health in the perinatal period is the low level of identification of need.
PHE has developed an interactive tool to help local commissioners and providers to plan their approach to perinatal and infant mental health in their area. The new needs assessment tool provides evidence-based information on risk factors affecting perinatal and infant health.

Infographic showing signs and extent of postnatal depression.
NICE has produced guidance on postnatal depression which can help health professionals recognise the signs of mental health problems and to select the appropriate treatment.
The first 2 years in life

Infographic showing important elements to encourage a healthy start in life.
Nutrition and physical activity
It is important to introduce a healthy diet and encourage physical activity from a young age to help reduce the risks of childhood obesity and tooth decay. Government advice is to breastfeed exclusively for 6 months and to start introducing solids from 6 months onwards.
Oral health
Improving oral health is a priority for PHE and will be covered in detail in a future edition of Health matters.
Safety
Ensuring that babies and toddlers stay safe in and around the home will help to reduce the number of unintentional injuries.
PHE’s guidance on reducing unintentional injuries in and around the home among children under 5 sets out 3 action areas for local authorities and their partners that will reduce the numbers of children injured and killed.
Ready to learn
All disadvantaged 2 year olds are entitled to 15 hours early years provision. Research shows high quality early education can reduce inequalities in educational outcomes for children living in disadvantage.

Infographic showing important milestones for children at age 2.
A review of the child’s development at 2 to 2.5 years
The 2 to 2.5 year review is offered to all families. It is led by a health visitor and can take place at the home, local clinic or children’s centre.
The universal 2 year review provides an opportunity to discuss and promote a child’s health and development and to identify children who are not developing as expected and who may require additional support.
The review is an opportunity to:
- assess the health and development of the child within the context of his or her environment of home and family circumstances
- ensure that families are linked in with the right services and support
- identify and address issues the parent or carer may have regarding the child’s health
As part of the review, health visitors will work with parents to complete an Ages and Stages Questionnaire (ASQ) about their child’s development. Where a child already attends an early years setting, the 2 year health review should form part of a holistic integrated review which includes the progress check undertaken at age 2 by early years providers. The integrated review may be done jointly or through systematic sharing of information and should be undertaken in partnership with parents.
We all have a role to play
The Chief Medical Officer has stated:
We need everyone in the public services to think family and children and young people at every interaction.
Health and wellbeing boards
The health and wellbeing board (HWB) is the main partnership board with responsibility for integration for all age groups including early years. The HWB is statutory and has senior membership with responsibility for identifying local needs and producing the Joint Strategic Needs Assessment (JSNA) from which a health and wellbeing strategy is developed.
Health and wellbeing boards are uniquely positioned to take a holistic view of the needs of children and to build settings and services around them to ensure that they are able to reach their potential. They have a key role to play in ensuring effective leadership and making the case for investing in early years services.
This includes:
- ensuring children have access to the health services they need
- adequate safe housing
- benefits and employment support for parents
- parks and leisure facilities
- access to children’s centres and early years settings
Commissioners
Clinical commissioning groups (CCGs) are responsible for commissioning midwifery services and local authorities for commissioning a wide range of children’s services including children’s centres, early intervention services and social care.
Joint commissioning of early years services can support integrated delivery through identifying and commissioning against agreed shared priorities and outcomes.
The 6 early years high impact areas, developed to support the transition of 0 to 5 commissioning to local authorities, can help inform decisions around the commissioning of the health visiting service and integrated children’s early years services.
Healthcare Practitioners
All health care professionals have a role to play in supporting the health of families. All Our Health is a call to action to healthcare practitioners to increase their contribution to prevention and health protection and promoting wellbeing and resilience.
Many healthcare practitioners have specific roles in supporting good health and development and encouraging the best start in life.
Midwives
Midwives are able to use every contact with women to make assessments and discuss:
- mental health
- smoking
- healthy nutrition
- drinking alcohol
- exercise
- supportive relationships
- future contraception use
Health visitors
Health visitors are pivotal to delivering early years services and work closely with early years staff. The 6 high impact areas highlight where health visitors can have the most impact on children’s health and wellbeing.
Health visitors provide expert information and support to families, developing relationships that enable difficulties to be identified early and help to be offered when needed.
The contact made with parents during the early weeks can inform the level and type of support needed. This includes supporting early parenting such as:
- feeding
- sleeping
- starting nursery
- identification of risk and additional needs
This is set out in the Health Visitor 4 5 6 model and 0 to 19 model service specification.
GPs and practice nurses
Children have frequent contact with general practice and GPs and practice nurses are ideally placed to have conversations with pregnant women and parents of small children about a range of health issues including vaccination. Primary care can signpost or refer families to a range of services including:
- community paediatrics and secondary care
- child, adolescent and adult mental health services
- smoking cessation services
- weight management
- Troubled Families teams
- drug and alcohol misuse services
Pharmacists
Community pharmacies are well placed to advise and signpost families on topics such as:
- managing minor illnesses and minor accidents
- Healthy Start vitamins
- contraception and sexual health
- smoking cessation
- weight management
