Evidence summary of impacts to date of public health communications to minority ethnic groups and related challenges, 23 September 2020
Updated 13 May 2022
Evidence summary of impacts to date of public health communications to minority ethnic groups and related challenges
Key points
COVID-19 prevention and control measures require effective public health communication to inform and update members of the public of key mitigations to minimise transmission (high confidence).
Health messages should be tailored to reflect cultural drivers of behaviour that will increase knowledge using accessible language and including content that reflects the social norms and identity of the target community to increase engagement and awareness of the health risk (high confidence).
Tailored public health messages during the COVID-19 pandemic have increased reach and accessibility of health messages, increasing knowledge and awareness of symptoms, health risk and control measures, and message acceptance, motivation and intention to comply with guidelines. Optimising public health communications is achieved by community engagement, which is a key mechanism through which each of these positive impacts has been achieved (high confidence).
Negative impacts and challenges of tailored health messages include multiple guidelines causing confusion, stigmatisation and increased racialised explanations which could lead to lower health protective behaviour, and structural barriers which limit the impact of tailored health messages. Co-production of health messages, sharing positive stories and examples of good practice, and promoting collective aims (despite using different channels of communication) is required to minimise negative impacts (high confidence).
Executive summary
COVID-19 prevention and control measures require effective public health communication to inform and update members of the public of key mitigations to minimise transmission. Tailored health campaigns that include culturally appropriate content can lead to better health outcomes than non-tailored approaches for people in minority ethnic groups. [When should tailored health messaging be used, page 7.]
Positive impacts of tailored public health communications during the COVID-19 pandemic include increasing reach and accessibility of health messages which result in increased knowledge and awareness of symptoms, health risk and control measures, and increase acceptance, motivation and intention to comply with guidelines. Optimising public health communications is achieved by community engagement, which is a key mechanism through which each of these positive impacts has been achieved. [Synthesis of evidence, page 8.]
Culturally accessible channels of communication include digital and print media such as WhatsApp, voice notes, radio, television, and translated resources. These modes of delivery increase accessibility of health information and can increase reach of local specific guidance among minority ethnic communities. [Synthesis of evidence, page 9.]
Health messages shared via local trusted sources increases engagement with guidance, increases message persuasiveness and can minimise belief in conspiracy theories and myths which are barriers to complying with guidelines. [Synthesis of evidence, page 10.]
While there are several alternative ways to deliver health messages for minority ethnic communities, a mode of delivery that increases reach and acceptability for one community is not necessarily an effective approach for another community. Sub-groups within communities should also be considered as acceptance of public health messages can be affected by other factors such as gender, age, different denominations and socio-economic context. [Synthesis of evidence, page 10.]
Sustained community engagement is a key mechanism for identifying appropriate trusted sources and for understanding cultural drivers of behaviour to ensure that health messages promote information that is accessible and relevant. Co-production of health messages with community members can enhance social cohesion and increase trust which makes it more likely that people will adhere to government policies. [Synthesis of evidence, page 9.]
Negative impacts and challenges of tailored health messages include multiple guidelines causing confusion, stigmatisation and increased racialised explanations leading to lower protective health behaviour and structural barriers which limit the impact of tailored health messages. Clarity of trusted sources and clear explanations for changes and differences in guidelines are required using culturally appropriate language and acceptable channels of communication. [Negative impacts and challenges of tailored health messages, page 11.]
Targeting particular communities with tailored health communication may create inaccurate perceptions that a particular culture’s norms contribute to the health risk. This may also create a false sense of security in groups where people think they are at low risk, resulting in lower compliance with guidance as the risks are perceived as confined to particular groups. Public health messages should promote collective goals and use targeted messages as a mechanism to achieve the same wider collective aim (for example save the NHS, protect lives), promote awareness of symptoms and control measures, and so on. Even if the language differs from the national message or differs across groups, the content should promote the same collective aim. [Negative impacts and challenges of tailored health messages, page 12.]
There are differences in the experiences of people from specific minority ethnic groups, such as increased concerns about the impact of COVID-19 on personal finances or the extent to which information is viewed as clear or trusted which differs across minority ethnic groups. This highlights the importance of not treating minority ethnic groups as a single homogenous group and to understand how health information can more closely relate to specific concerns and contexts for different groups. [Negative impacts and challenges of tailored health messages, page 12.]
Culturally appropriate, tailored health messages achieve a number of positive impacts which includes reaching ‘hard to reach’ communities, as well as increasing understanding, knowledge, motivation and adherence to promoted behaviours. However, trust in leadership and ongoing community engagement is required to achieve this. [Negative impacts and challenges of tailored health messages, page 13.]
Variations in response to tailored campaigns highlight structural challenges that may limit the impact of a tailored communication strategy. Public health communications alone cannot fix structural factors related to ethnicity, like differences in economic status or population distribution. Maximising the impact of public health communication requires support from wider systems, structures and policies. Security of income and employment therefore needs to be addressed to maximise adherence with health messages as even if a culturally appropriate health message reaches the target community, impact will be limited if financial instability is experienced because of mitigations. [Negative impacts and challenges of tailored health messages, page 13.]
Recommendations
Community engagement and empowerment principles should be used to co-design health messages and identify appropriate message content, channels and sources for the target community.
Mechanisms for on-going engagement with minority ethnic communities, for example, via focus groups, online forums and rapid cycle groups, are required as engaging communities in all aspects of the decision-making process will increase community preparedness and satisfaction with communication.
Community engagement is required pre-, during and post-pandemics to maintain trust and mobilise quickly in the event of a pandemic to develop and share culturally relevant health messages. This incorporates the need to discern who target audiences trust versus who authorities might feel they currently do, or should, trust. The principles for co-production of guidance relating to the control of COVID-19 should be followed when engaging with communities to maximise effectiveness of this approach.
To minimise stigma and divisive racialised narratives, messages that recognise community efforts and successes should be promoted. Data should be collected and reported which highlights wider structural factors that increase risk for minority ethnic communities, including socioeconomic status data. The impact of chronic stress caused by racial discrimination and material deprivation that increases risk of poor health outcomes must also be acknowledged.
Structural barriers need to be identified and addressed to ensure health messages do not exacerbate or create health inequalities.
Research priorities
A mechanism for reporting and accessing evaluation data, such as a shared repository to review impact data of national and or local campaigns, is required to fully capture the impact of tailored health messaging campaigns. A number of international, national and local campaigns have tailored health messages for ethnic minority communities, but impact data is not reported or available to establish the mechanism of action and effectiveness of different components of tailored health messages. This will facilitate evidence-based, theoretically-informed and rapid development of tailored health messages.
A process to discuss and interpret impact data with the communities it has been gathered from is required to understand reasons for positive and negative impact. This will extend our understanding of impact data beyond patterns to understand the reasons why things have worked or not. Research is required to understand the impact of tailored health messaging or campaigns that include elements which are tailored, during the COVID-19 pandemic on a number of outcomes including mental health and behavioural outcomes.
Qualitative, ethnographic research and citizen science, as outlined in the SPI-B co-production paper, is required to understand within and between group differences to identify appropriate risk communications for different minority ethnic communities. In addition, evidence from a wide range of interventions for which some targeted messaging has been applied should be considered to identify themes in terms of effective communications. Drawing on themes from wider research can inform COVID-19 specific research more rapidly.
Quantitative, experimental research is required to understand the mechanisms underpinning the impact of tailored health messages and identify effective strategies to implement as part of targeted public health communication.
There is a distinction between inclusive population level messages that target diverse populations as part of mass media campaigns and more targeted tailored messaging for specific communities. The value of these approaches will vary depending on engagement variables such as trust, particularly if a source of distrust emanates from a point of ethnicity – feeling overly targeted for example. Research on the use of inclusive messaging in mass media is required to understand the impact of inclusive population level messaging.
Introduction
Health messages should take into account the role of culture to facilitate the development of messages using language, sources and content appropriate to diverse populations [footnote 1]. This report presents an evidence summary of the impact of tailored public health communication during pandemics and for infectious diseases more generally, but it is important to first clarify the social dimensions of ethnicity and terminology used to contextualise the report findings.
Social dimensions of ethnicity
Ethnicity is defined by social and cultural factors and includes varied ways in which people see themselves and others, including belief of common descent, cultural practices, religion, language and nationality. Individuals may define their ethnicity differently in different contexts. We note that there are very limited genetic differences corresponding to traditional ethnic categorisation [footnote 2] [footnote 3]. What constitutes different ethnic groups varies from country to country. Much quantitative UK research uses the ethnic categories developed for the census, which may not correspond to how people see themselves or others.
Terminology around ethnicity regularly shifts and is often seen to be problematic by those being described [footnote 2] [footnote 4]. BAME (Black, Asian and Minority Ethnic) is a UK term that has been used in prior COVID-19 work [footnote 5] and other health research, although it has been criticised due to the amalgamation of heterogeneous experiences and its emphasis on skin colour [footnote 6]. This report will adopt the term Minority Ethnic to refer to the groups, communities and individuals that encompass the ethnic categories developed for the UK census. As other organisations may use different terminology, where it is appropriate, such as when quoting from an external publication, this report may include terms other than Minority Ethnic on occasion.
Minority ethnic communities’ experiences in the UK during COVID-19
There is significant variation of experience, knowledge and behaviour both across different ethnic communities as well as within these groups.
Results from the CORSAIR study, which used the census categories reported as BAME, analysing national polling data collected on behalf of the Department of Health and Social Care (approximately 2000 people surveyed each week from January to August 2020; see [footnote 7] and detailed methods in [^8]), found BAME individuals show higher rates of worry about COVID-19 (Figure 1). The proportion of individuals correctly identifying the symptoms of COVID-19 is lower in BAME groups (Figure 2) [^8]. Qualitative research found that awareness of the NHS Test and Trace programme was lower in some minority ethnic groups with many participants having never heard of it, including community leaders. Similarly to the general population, while there was awareness of the need to isolate with symptoms, there was confusion over 7, 10 or 14 days and if you can or cannot leave the house. News reports that the virus disproportionately affected some minority ethnic groups raised scepticism due to some communities receiving contrasting messages at the beginning of the pandemic via social media and WhatsApp that reported lower risk for some groups [footnote 9].
Research findings on trust and perceived credibility of the government is mixed. Qualitative research conducted between May and September with minority ethnic groups during the pandemic found lower levels of trust in government across all ethnic groups interviewed, affecting the perceived rationale for certain measures and heightened concerns over privacy and ‘tracking’ data for the NHS Test and Trace app [footnote 9]. However, a cross-sectional study conducted in June to July found no differences in political trust by ethnicity [footnote 10]. Furthermore, the CORSAIR study found Mixed, Asian-British Asian and Arab-Other groups all score higher on perceived credibility of the government, a different but seemingly related concept to trust. Reasons for these different results are unclear, but may reflect differences in questions asked.
In addition to variation in knowledge of symptoms, perceptions and control measures, there are differences in health outcomes from COVID-19 between ethnic groups which occur at multiple points from exposure to the virus, through infection to the development of severe disease [footnote 11]. Public health communication therefore needs to inform and update members of the public of key mitigations to minimise transmission (such as social distancing, hand washing, mask wearing) and raise awareness about symptoms and what to do if unwell (for example self-isolation, obtain a test).
When should tailored health messaging be used?
Low awareness and knowledge of symptoms and control measures indicate a health message may not have reached the intended audience. Where trust is low or mixed, a health message that reaches its intended audience may be rejected. Acceptance of public health messages can be affected by socio-cultural factors such as gender roles, generational differences, religious beliefs and language preferences [footnote 12]. Health messages that do not take into account these socio-cultural factors may not reach the intended audience and could widen existing ethnic inequalities in health [footnote 13]. Even if reached, they may not be engaged with due to lack of cultural relevance to the target community. Health messages should therefore be tailored to reflect cultural drivers of behaviour that will increase knowledge. Using accessible language and including content that reflects the social norms and is aligned with the identity of the target community, can increase motivation and engagement with control measures [footnote 14].
Guidelines on how to develop health messages for minority ethnic communities have been reported by SPI-B [footnote 14]. The current report will review the impact of tailored health messages on minority ethnic communities during pandemics or when managing infectious diseases. There is a difference between targeting messages for specific communities and ensuring that health messages for the general public are inclusive. Both are important for effective public health communication, but this report focuses on the former which has a stronger evidence base in the context of COVID-19. Impact is the “positive and negative, primary and secondary long-term effects produced by a development intervention, directly or indirectly, intended or unintended.” [footnote 15]. For the purpose of this report, impact is defined as change (positive or negative) to behaviour, determinants of behaviour and reach, (namely, did the health message reach the target community?) [footnote 16] and the intervention is the tailored health message. Data from a range of sources on tailored health messages has been synthesised to inform the evidence summary below. In addition to peer-reviewed journal articles, we include findings from 4 internal reports that include data from quantitative online river sampling with quotas and weights applied to ensure the results are broadly reflective of the local areas that were polled and qualitative research findings from interviews with 500 people [footnote 17] and 50, 66 and 5 focus groups and interviews [footnote 9] [footnote 18] [footnote 19].
Synthesis of evidence
Tailored health messages have improved public health communications during the COVID-19 pandemic by increasing reach and accessibility of health messages which result in increased knowledge and awareness of symptoms, health risk and control measures and can increase acceptance, motivation and intention to comply with guidelines. Optimising public health communications is achieved by community engagement, which is a key mechanism through which each of these positive impacts has been achieved.
Negative impacts and challenges of tailored health messages include multiple guidelines causing confusion, stigmatisation and increased racialised explanations which could lead to lower health protective behaviour, and structural barriers which limit the impact of tailored health messages.
Positive impact of tailored health messages
Community engagement is a key mechanism to optimise public health communications
Community engagement includes a range of approaches to involve local communities in initiatives to improve their health and wellbeing including conducting needs assessments, community development, planning, design, delivery and evaluation [footnote 20]. Community engagement is an important mechanism through which positive impact is achieved. It can facilitate understanding of the impact of race, ethnicity and culture on health-related decisions and can help determine which messages are most effective in communicating risk and risk reduction strategies during a pandemic [footnote 21].
Co-designing culturally relevant messages with communities results in increased engagement with health messages and awareness of the health risk by including culturally appropriate content and ensuring the mode of delivery is suitable for the needs of the target community [footnote 22]. Community participatory approaches to developing health messages by local communities, where they identify their own health problems and develop local stories, aligned with the health literacy of the target group, can increase knowledge of health risks. Empowering communities to address health risks in this way contributes to achieving sustained outcomes as this maximises exposure to the health risk message and promotes skills and knowledge relevant to the target community [footnote 23]. Co-production of health messages with community members can also enhance social cohesion and increase trust which makes it more likely that people will adhere to government policies [footnote 24].
On-going community partnerships, pre- and post-pandemic, are essential to provide a timely and effective response and increase trust and acceptance of health messages. Pre-existing community partnerships can facilitate rapid responses, enabling programme modifications which respond to immediate and critical needs of communities. During the COVID-19 pandemic, pre-existing partnerships were mobilised, and community health ambassadors provided insight into community needs. Building on the success of a pre-existing partnership with the community and having a history of practicing collective impact means partnerships can quickly understand the needs of the target community and implement resources required to mitigate the effects of COVID-19. For example, increasing resources (such as care kits in deprived areas) and developing multi-lingual communications on prevention methods [footnote 25] [footnote 26]. This highlights the importance of providing funding and resources to enable community partnerships and mutual aid groups to support communities.
Adapting channels of communication can increase reach and accessibility of health message and increase knowledge and understanding of health risk and mitigations
Tailored health messages that draw on culturally accessible modes of delivery are more likely to reach the intended community and increase health literacy by improving people’s access to health information and their capacity to use it effectively [footnote 27].
Culturally accessible channels of communication include use of digital media such as WhatsApp, voice notes, radio and storylines in popular cultural media, which have been positively received by some minority ethnic communities during the COVID-19 pandemic (see Table 1) [footnote 19]. This approach addresses health literacy barriers in communities where verbal communication is used instead of written communication. Leaflets and posters translated into different languages have also increased accessibility to local-specific COVID-19 guidance [footnote 17]. Digital and print media enables messages to be broadcast in native languages. During the COVID-19 pandemic, this has included signposting on local cultural media to national resources such as Doctors of the World who have translated national guidance [footnote 17]. These campaigns have increased reach of local-specific guidance among minority ethnic communities and demonstrated some success with changing behaviour with fewer people saying they were leaving their homes compared to England as a whole, increased awareness that face coverings on public transport are required and that people must self-isolate for 14 days if contacted by NHS Test and Trace [footnote 17]. Minority ethnic communities, however, were least likely to report that they had seen localised materials which highlights the importance of extending reach [footnote 17].
In addition to digital and print media, health messages conveyed via local, trusted sources is important as people are more likely to engage with guidance when the message comes from within their own community [footnote 28]. Community leaders, Mayors, local councillors, faith leaders and local community volunteers can increase reach making health messages more accessible. First-hand testimonies of local community members who have had COVID-19 can increase knowledge and understanding of the health risk and its severity [footnote 19]. In addition, GPs with their deep connections into communities, during the COVID-19 pandemic held online consultations from their local group practices with the neighbourhoods they worked in [footnote 19]. Delivering health messages via trusted sources can increase message persuasiveness [footnote 29] and minimise belief in conspiracy theories and myths which are barriers to complying with guidelines [footnote 18]. Local measures implemented in Liverpool following an increase in positive cases of COVID-19 demonstrates the impact of local teams that can take prompt action and make best use of local knowledge. Local teams including community leaders, faith leaders, council teams and volunteers visited homes and businesses to raise awareness and give advice which helped reduce the number of confirmed cases of COVID-19 from ‘amber’ down to ‘green’ [footnote 30]. This approach also highlights the impact of settings, namely different places and social contexts in which people engage in activities which relate to their health [footnote 31] such as workplaces that can be used to communicate tailored health messages particularly as key mitigations are required in this setting, such as, physical distancing.
Strategies that have been used in an international setting to communicate COVID-19 health messages include use of elders to communicate key messages such as advising tribal residents to stay at home, wash their hands, practice social distancing and wear masks [footnote 32]; and translated materials and Spanish-language community-facing webinars via Zoom which has improved knowledge of symptoms, mitigations and culturally relevant support including increased understanding of how to avoid spread of the virus and how and where to seek testing and healthcare support if symptomatic [footnote 26]. Wider literature indicates use of radio and videos are effective means of circumventing low health literacy and can increase awareness of health conditions and motivation to engage in protective health behaviours [footnote 33] [footnote 34]. Mobile phone messaging [footnote 35] [footnote 36] and apps can increase reach, particularly for potentially stigmatising conditions [footnote 37].
While there are several alternative ways to deliver health messages for minority ethnic communities, a mode of delivery that increases reach and acceptability for one community is not necessarily an effective approach for another community [footnote 21]. Different modes of delivery work for different groups based on cultural traditions and social context, for example written communication may not reach a community that draws on oral traditions such as story-telling to convey key health messages [footnote 38] and trusted sources should be tailored to different groups, for example the inclusion of female community leaders [footnote 19].
Tailored health messages increase acceptance, motivation and intention to comply with guidelines
Drawing on wider literature we can see the way information is presented can increase message acceptance, intentions and motivation to comply with guidelines. Health messages which include content that is matched to an individual’s culture can increase attitudes and intentions to perform health behaviours [footnote 39] [footnote 40]. For example, central to the identity of many collectivistic cultures, where the needs and goals of the group are prioritised before the needs and desires of an individual, health messages that draw on personal relations such as ‘I express my love for you by staying away from you’ to emphasise the importance of social distancing during COVID-19 [footnote 32] may increase motivation to comply with guidelines.
Tailored health messages can also modify beliefs and minimise fear and stigma of infectious diseases, which are barriers to protective health behaviours. Inaccurate causal explanations of infectious disease can be reduced, and intention to engage in protective behaviours can be achieved, by tailoring health messages using interactive 2-way communication and visual aids such as photographs [footnote 41]. Tailored strategies including community engagement, tailored educational materials, panel discussions and media interviews designed to minimise fear and stigma of SARS which resulted in increased understanding of SARS, strengthened community resiliency, mitigated fear, stigmatisation and discrimination, dispelled myths, and established community relationships and networks [footnote 42].
Beliefs, attitudes, intentions and motivation are important determinants of behaviour that can be modified with culturally appropriate health messages. Positive changes to these determinants of behaviour increases the likelihood that the target community will engage with recommended behaviours.
Negative impacts and challenges of tailored health messages
Multiple guidelines result in confusion and lack of clarity
During recent localised control measures, tailored health messages were used to inform local communities of restrictions which differed from national guidance. One UK study revealed some ethnic minority community members were confused due to mixed-messages and different national and local guidelines. Uncertainty of where to access relevant information, language barriers and low digital resources to access guidance exacerbated this [footnote 19]. Uncertainty during a pandemic can lead to mistrust in authorities and lower compliance [footnote 1]. In addition, government officials, police and community-facing key workers such as bus drivers were not role-modelling guidance, which resulted in some community members not complying with guidance [footnote 19]. Clarity of trusted sources and clear explanations for changes and differences in guidelines are required using culturally appropriate language and acceptable channels of communication in addition to government authorities role modelling the guidance to reinforce the localised health message [footnote 19].
Challenges for consistency in messaging can also relate to alignment of health messages with messaging in other countries as, for some members of minority ethnic communities that have family and friends abroad, messaging in countries outside the UK is part of the community view. Social, print and mass media from sources in other countries has been used to share information about outbreaks, usually hours ahead of information released locally, which can result in inconsistent information and coverage, creating fear and suspicion that the government is not telling the truth about the outbreak. This contributes to mixed messages and may create a lower perception of the health risk among those using evidence of low rates of infection in countries abroad to understand their risk [footnote 9] [footnote 42]. Ongoing community engagement with formal and informal community leaders is required to mitigate this risk and to ensure UK-based guidance is recognised as a primary and trusted source of information.
Stigmatisation and increased racialised explanations lead to lower protective health behaviour
Tailored health messages are more likely than non-tailored messages to promote behaviour change but there is a risk of stigmatising groups when tailoring or segmenting public health messages by race or ethnicity [footnote 43]. People who feel stigmatised during pandemic outbreaks may isolate themselves from social contact, making it difficult to engage with services or receive appropriate medical care [footnote 44], increasing their vulnerabilities including potential reluctance to get tested as part of the NHS Test and Trace programme [footnote 19].
Targeting particular communities with tailored health communication may create inaccurate perceptions that a particular culture’s norms contribute to the health risk. This may also create a false sense of security in groups where people think they are at low risk resulting in lower compliance with guidance as the risks are perceived as confined to particular groups [footnote 45]. Health messages that highlight ‘at risk’ groups may be counterproductive as these messages may erode collective identity and increase racialised explanations for poor health outcomes in surrounding areas and create a sense of racial inequality for the target community [footnote 19]. Community leaders have reported growing tension as communities felt that they were being blamed for the spread of COVID-19 [footnote 9]. Racialised explanations may also exist within minority groups with concerns that specific communities are being grouped with communities they do not identify with [footnote 46]. There are differences in the experiences of people from specific minority ethnic groups, such as increased concerns about the impact of COVID-19 on personal finances among the Black population compared to other minority groups, and differences in the extent to which information is viewed as clear or trusted which varies between minority ethnic groups. This highlights the importance of not treating ethnic minorities as a single homogenous group and to understand how health information can more closely relate to specific concerns and contexts for different minority groups [footnote 47], including the impact of age and gender. Public health messages should promote collective goals and use targeted messages as a mechanism to achieve the same wider collective aim (such as; save the NHS, protect lives), promote awareness of symptoms and control measures, and so on. Even if the language differs from the national message or differs across groups, the content should promote the same collective aim.
When documenting COVID-19 ethnic disparities, data should be contextualised with adequate analysis, such as inclusion of socioeconomic data, as disparity figures without explanatory context can perpetuate harmful myths and misunderstandings [footnote 48]. Minority ethnic groups are disproportionately likely to have low socioeconomic status and poorer health outcomes, and reporting data which reflects the connection between racial and ethnic disparities and economic inequality can mitigate narratives that frame COVID-19 as largely a problem of minorities [footnote 48].
Structural barriers limit impact of tailored health messaging
A number of factors influence the impact of tailored public health messages for minority ethnic communities including use of accessible language, acceptable and trusted sources, and inclusion of cultural identity to modify determinants of behaviour (such as knowledge, beliefs, attitudes, intentions) and behaviour (such as self-isolation). However, variations in response to tailored campaigns highlight structural challenges that may limit the impact of a tailored communication strategy. For example, the results of a tailored public health campaign in one area of the UK found, although key messages had reached the target community, those who had seen the message did not report any improvement in knowledge or behavioural change; they were not significantly more or less likely to identify symptoms of coronavirus, to stay at home more, or to keep their distance from others compared to residents in another part of the UK. Reasons for leaving the home during lockdown were to go to work due to being key workers or because their employer asked them to come in [footnote 17]. There is also evidence that individuals whose employment situation is precarious may be unwilling to engage with control measures that could leave them without income for 2 weeks. Security of income and employment therefore needs to be addressed to maximise adherence with health messages [footnote 45] as even if a culturally appropriate health message reaches the target community, impact will be limited if financial instability is experienced because of mitigations [footnote 9] [footnote 49]. This also highlights the importance of the role of employers and employer communications to promote control measures [footnote 17].
Low trust in government is a barrier which can limit the impact of tailored health messages. Those who feel the greatest uncertainty of the impact of COVID-19 – both individually and for their group - are likely to perceive a greater level of threat, the strength of which is dependent on their political trust [footnote 50]. Where trust in government is low, there is lower confidence in government testing programmes and increased concerns about privacy and security of the NHS app [footnote 9]. Communications that enhanced trust included receiving a letter from the Prime Minister, particularly for those who do not watch English television, with special requests to family and friends to translate the letter due to its perceived importance [footnote 9].
Maximising the impact of public health communication requires support from wider systems, structures and policies. For example, Australia has made a concerted effort to prevent COVID-19 outbreaks in its vulnerable indigenous populations and has succeeded in keeping infections at a very low level. Specific initiatives and guidelines aimed at mitigating the effects of COVID-19 on indigenous populations include community engagement, financial and practical support, proactive screening and educational resources on safety, hygiene practices and transmission reduction to assist with a community-driven response [^51]. The impact of this targeted approach was enhanced with a range of supportive mechanisms and policies and not only educational resources designed to improved knowledge and understanding.
Summary
Culturally appropriate, tailored health messages achieve a number of positive impacts which includes accessing ‘hard to reach’ communities, increasing behavioural determinants such as knowledge, intention and motivation and behaviour change, but trust in leadership and sustained community engagement is required to achieve this. Table 1 illustrates the impact and challenges specific to one UK based campaign during the COVID-19 pandemic. We are aware of several campaigns that have been tailored for minority ethnic groups during the COVID-19 pandemic, but impact data is not routinely collected or reported. To develop a rigorous evidence base for the effectiveness of tailored health communication, there is a need report impact data that captures the effectiveness and facilitates comparisons of different campaigns. Both quantitative and qualitative evaluation methods should be considered.
Table 1. Case study of the impact and challenges of tailored health messages for ethnic minority communities in the UK. [footnote 18] [footnote 19]
| Impact | Strategies to achieve impact | Challenges | Recommendations | |
|---|---|---|---|---|
| Message Delivery | Message reached the target community. | Use of social media: – Videos –Voice notes – Shared via WhatsApp Credible source: – Religious leaders – Mutual aid groups Language: – Linguistically appropriate. |
Language: – Additional alternative languages required. Format: – Videos in English with subtitles inaccessible to people who speak but cannot read other languages – Lack of internet to access guidance |
Use wider range of languages. Use visual aids, animations and verbal communication. Use local radio stations, papers and posters to cascade messages. |
| Message content | Increased motivation to comply with guidance. | Use of culturally tailored, clear messaging. First-hand testimonials from local community members who had contracted COVID-19. |
Understanding: – Different messages at national and local level – Divisive racialised narratives (religious, social, employment, language skills) |
Make messaging culturally-specific and personally relevant. Include positive messaging to celebrate success and counter blame narratives. |
| Message source | Increased willingness to listen to message. | Use of formal local sources trusted, including Mayor and Local Authorities. Consultation with religious and community leaders. Religious organisations disseminated clear message. |
Varying levels of trust in authorities (such as police) among different communities. Consultation with community and religious leaders not representative of all sub-groups within target community. |
Use trusted community leaders, local business and organisations (such as parent groups) to disseminate guidance. Include a wider range of sub-group representatives (such as female community leaders). |
Annex
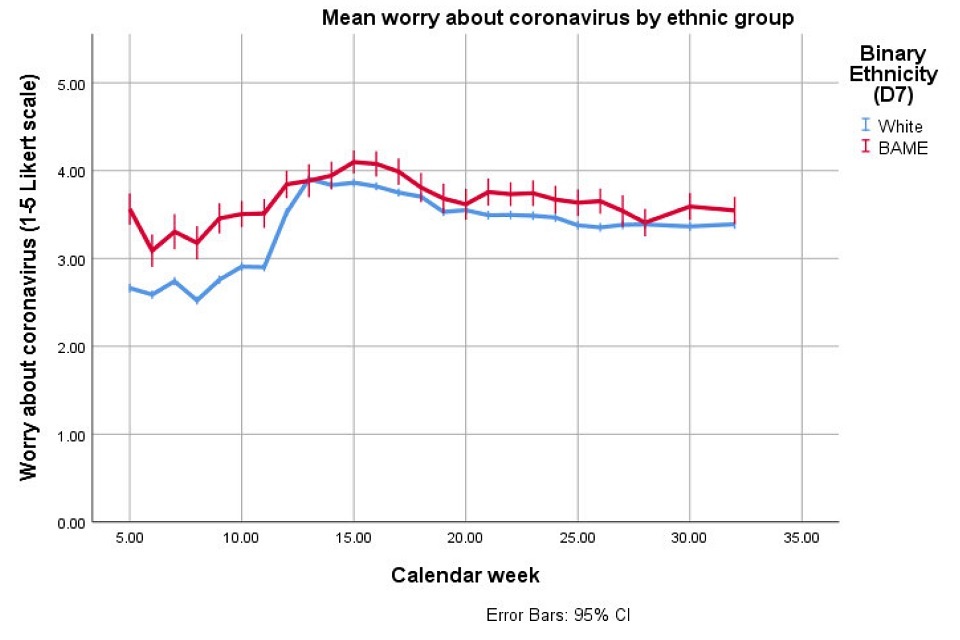
Line graph plotting COVID-19 worry (from 0 to 5 on the Likert scale) over time (calendar weeks 0 to 35). Two trendlines: blue and red lines respectively represent white and BAME ethnic groups. Data points have 95 per cent confidence interval error bars.
Figure 1: Mean worry about coronavirus by White versus BAME. (Note the White group includes groups identifying as Irish, Gypsy, Traveller or any other white background.)
Worry is scored from 1 = Not at all worried to 5 = Extremely worried. Performing a GEE, adjusting for week, we can model the effect in different ethnic groups. Taking White British as the baseline, those identifying as White Other scored statistically significantly lower, although the difference was small (-0.05, 95 per cent CI -0.10, -0.01). Those identifying as Arab Other showed no difference (0.17, 95 per cent CI -0.02, 0.35). Those identifying with the other census categories scored statistically significantly higher than White British or White Other: Black, Black British (0.09, 95 per cent CI 0.01, 0.17); Mixed (0.18, 95 per cent CI 0.11, 0.25); Asian, Asian British (0.31, 95 per cent CI 0.26, 0.36). Thus, those identifying as Asian, Asian British were also statistically significantly higher than those identifying as Black, British or Mixed.
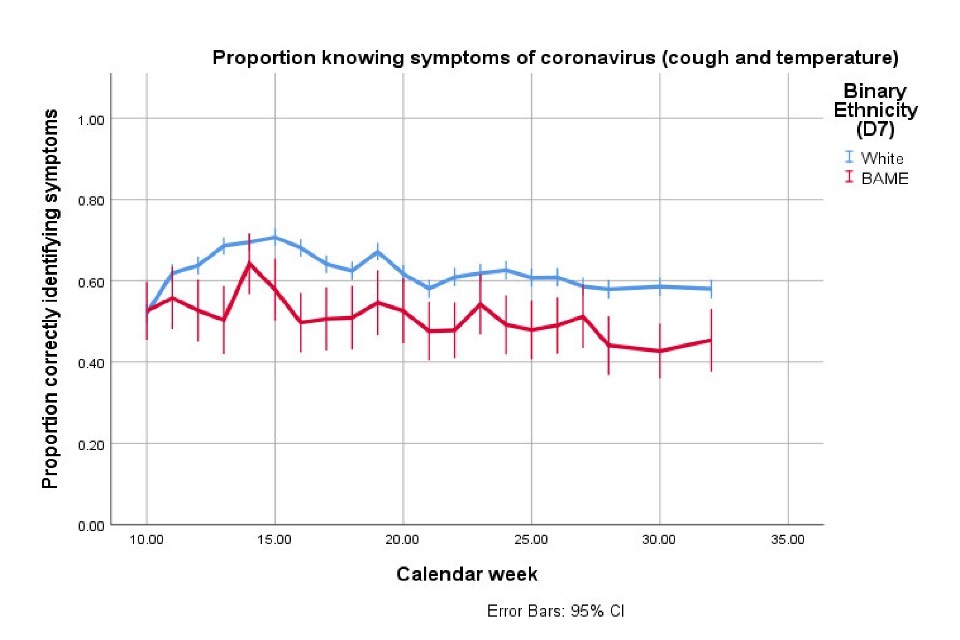
Line graph plotting proportion of white and BAME ethnic groups (respectively blue and red trendlines) correctly identifying COVID-19 symptoms (cough and temperature) from calendar week 0 to 35. Data points have 95 per cent confidence interval error bars.
Figure 2: Proportion correctly identifying symptoms of COVID-19 by White versus BAME. (Note the White group includes groups identifying as Irish, Gypsy, Traveller or any other white background.) Performing a GEE, adjusting for week, we can model the binary outcome of correctly identifying symptoms or not. Taking White British as the baseline, all other groups show lower correct symptom identification, although the result is not statistically different for the small Arab, Other group: Black, Black British (odds ratio = 0.55, 95 per cent CI 0.47, 0.64); Mixed (OR = 0.55, 95 per cent CI 0.48, 0.63); White Other (OR = 0.59, 95 per cent CI 0.54, 0.64); Asian, Asian British (OR = 0.65, 95 per cent CI 0.58, 0.72); Arab, Other (OR = 0.70, 95 per cent CI 0.48, 1.02).
References
-
World Health Organization. Communicating risk in public health emergencies: a WHO guideline for emergency risk communication (ERC) policy and practice. World Health Organization; 2017. ↩ ↩2
-
Agyemang C, Bhopal R, Bruijnzeels M. Negro, Black, Black African, African Caribbean, African American or what? Labelling African origin populations in the health arena in the 21st century. Journal of Epidemiology and Community Health. 1 December 2005;59(12):1014-8. ↩ ↩2
-
Chowkwanyun M, Reed Jr AL. Racial health disparities and Covid-19—caution and context. New England Journal of Medicine. 6 May 2020. ↩
-
Aspinall PJ. Collective terminology to describe the minority ethnic population: the persistence of confusion and ambiguity in usage. Sociology. November 2002;36(4):803-16. ↩
-
Public Health England (2020), “Beyond the data: Understanding the impact of COVID-19 on BAME groups”. ↩
-
BBC News. Should BAME be ditched as a term for black, Asian and minority ethnic people?, 17 May 2018. ↩
-
Potts HWW, Smith LE, Fear NT, Michie S, Amlȏt R, Rubin GJ. Ethnicity, COVID-19-related behaviours, attitudes and outcomes. Report to DHSC, 4 June 2020. ↩
-
National Resilience Hub – Public Qualitative BAME Research Findings (June to September 2020). ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8
-
Abrams D, Lalot F, Broadwood J, Davis-Hayon K (2020). Social Cohesion in the time of Covid-19: Headline Evidence on Integration Area Local Authorities and BAME relative to others. University of Kent report. ↩
-
SAGE Ethnicity Sub-group paper (2020) ‘Drivers of the higher COVID-19 incidence, morbidity and mortality among ethnic minority groups’. ↩
-
Vaughan E, Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. American journal of public health. October 2009;99(S2):S324-32. ↩
-
White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations.Social inequality and public health.22 April 2009;65:82. ↩
-
SPI-B, 2020. Public Health Messaging for Communities from Different Cultural Backgrounds. ↩ ↩2
-
Organisation for Economic Co-operation and Development – Development Assistance Committee. ↩
-
Linnan L, Steckler A. Process evaluation for public health interventions and research. ↩
-
National Resilience Hub – Local Lockdowns Quantitative Research (Leicester Lockdown and Blackburn with Darwen, July 2020). ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7
-
Holt J. Holt M. Findings from the Leicester City COVID-19 community engagement focus groups. 2020. ↩ ↩2 ↩3
-
Simpson, N. Bear, L. (2020). Leicester Local Lockdown: Preliminary Interview Findings. ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9 ↩10 ↩11
-
National Institute for Health and Care Excellence. Community engagement: Improving health and wellbeing and reducing health inequalities. 2016. ↩
-
Nsiah-Kumi PA. Communicating effectively with vulnerable populations during water contamination events. Journal of water and health. March 2008;6(S1):63-75. ↩ ↩2
-
Tyus NC, Freeman RJ, Gibbons MC. Development of a replicable process for translating science into practical health education messages. Journal of the National Medical Association. September 2006;98(9):1505. ↩
-
Nguyen HV, Le GM, Nguyen SM, Tran MN, Ha NM. The effect of participatory community communication on HIV preventive behaviors among ethnic minority youth in central Vietnam. BMC Public Health. 1 December 2012;12(1):170. ↩
-
SPI-B (2020) Principles for co-production of guidance relating to the control of COVID-19. ↩
-
Michener L, Aguilar-Gaxiola S, Alberti PM, Castaneda MJ, Castrucci BC, Harrison LM, et al. Engaging With Communities — Lessons (Re)Learned From COVID-19. Prev Chronic Dis 2020;17:200250. DOI: https:// doi.org/10.5888/pcd1.200250. ↩
-
Calo WA, Murray A, Francis E, Bermudez M, Kraschnewski J. Peer Reviewed: Reaching the Hispanic Community About COVID-19 Through Existing Chronic Disease Prevention Programs. Preventing Chronic Disease. 2020;17. ↩ ↩2
-
World Health Organization. Health promotion glossary. World Health Organization; 1998. ↩
-
Gray L, MacDonald C, Mackie B, Paton D, Johnston D, Baker MG. Community responses to communication campaigns for influenza A (H1N1): a focus group study. BMC Public Health. December 2012;12(1):1-2. ↩
-
Kreuter MW, McClure SM. The role of culture in health communication. Annu. Rev. Public Health.21 April 2004;25:439-55. ↩
-
Liverpool Express. Leaders thank community for Princes Park Covid-19 success. 2020. ↩
-
World Health Organization. Healthy settings. ↩
-
Chen CM. Public health messages about COVID-19 prevention in multilingual Taiwan. Multilingua. 25 September 2020;39(5):597-606. ↩ ↩2
-
Odedina F, Oluwayemisi AO, Pressey S, Gaddy S, Egensteiner E, Ojewale EO, Moline OM, Martin CM. Development and assessment of an evidence-based prostate cancer intervention programme for black men: the WORD on prostate cancer video. ecancermedicalscience. 2014;8. ↩
-
Hall IJ, Johnson-Turbes CA, Williams KN. The Potential of Black Radio to Disseminate Health Messages and Reduce Disparities Posted on 15 June 2010. ↩
-
Jabour SM, Page A, Hall SF, Rodriguez L, Shields WC, Alvanzo AA. Information and communication technologies interest, access, and use: cross-sectional survey of a community sample of urban, predominantly black women. Journal of medical Internet research. 2018;20(8):e248. ↩
-
McBride B, O’Neil JD, Hue TT, Eni R, Nguyen CV, Nguyen LT. Improving health equity for ethnic minority women in Thai Nguyen, Vietnam: qualitative results from an mHealth intervention targeting maternal and infant health service access. Journal of Public Health. 1 December 2018;40(suppl_2):ii32-41. ↩
-
Fields EL, Long A, Dangerfield DT, Morgan A, Uzzi M, Arrington-Sanders R, Jennings JM. There’s an app for that: Using geosocial networking apps to access young Black gay, bisexual, and other MSM at risk for HIV. American Journal of Health Promotion. January 2020;34(1):42-51. ↩
-
Huff RM, Kline MV, Peterson DV, editors. Health promotion in multicultural populations: A handbook for practitioners and students. SAGE publications; 2 January 2014. ↩
-
Uskul AK, Sherman DK, Fitzgibbon J. The cultural congruency effect: Culture, regulatory focus, and the effectiveness of gain-vs. loss-framed health messages. Journal of Experimental Social Psychology. 1 May 2009;45(3):535 to 41. ↩
-
Uskul AK, Oyserman D. When message-frame fits salient cultural-frame, messages feel more persuasive. Psychology and Health. 1 March 2010;25(3):321-37. ↩
-
Parveen S, Islam MS, Begum M, Alam MU, Sazzad HM, Sultana R, Rahman M, Gurley ES, Hossain MJ, Luby SP. It’s not only what you say, it’s also how you say it: communicating nipah virus prevention messages during an outbreak in Bangladesh. BMC Public Health. December 2016;16(1):1-1. ↩
-
Person B, Sy F, Holton K, Govert B, Liang A. Fear and stigma: the epidemic within the SARS outbreak. Emerging infectious diseases. February 2004;10(2):358. ↩ ↩2
-
Fields EL, Long A, Dangerfield DT, Morgan A, Uzzi M, Arrington-Sanders R, Jennings JM. There’s an app for that: Using geosocial networking apps to access young Black gay, bisexual, and other MSM at risk for HIV. American Journal of Health Promotion. January 2020;34(1):42-51. ↩
-
McCauley M, Minsky S, Viswanath K. The H1N1 pandemic: media frames, stigmatization and coping. BMC Public Health. 1 December 2013;13(1):1116. ↩
-
What factors make a community more vulnerable to COVID-19 ? A summary of a British Academy workshop. 2020. ↩ ↩2
-
Kandula NR, Khurana NR, Makoul G, Glass S, Baker DW. A community and culture-centered approach to developing effective cardiovascular health messages. Journal of general internal medicine. 1 October 2012;27(10):1308-16. ↩
-
Wellcome Monitor. Anxiety, Confusion and Distrust How BAME people in Britain have had a worse experience of the COVID-19 pandemic. 2020. ↩
-
Chowkwanyun M, Reed Jr AL. Racial health disparities and Covid-19—caution and context. New England Journal of Medicine. 6 May 2020. ↩ ↩2
-
SPI-B Consensus on the impact of financial and other targeted support on rates of self-isolation or quarantine (2020). ↩
-
Lalot F, Abrams D, Travaglino GA. A version amplification in the emerging COVID-19 pandemic: The impact of political trust and subjective uncertainty on perceived threat. Journal of Community and Applied Social Psychology. 2020. ↩
