Evaluation of the Personal Support Package
Published 20 July 2021
Applies to England, Scotland and Wales
DWP research report no. 1000
A report of research carried out by NatCen on behalf of the Department for Work and Pensions.
Crown copyright 2021.
You may re-use this information (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit The National Archives or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email psi@nationalarchives.gov.uk.
If you would like to know more about DWP research, email socialresearch@dwp.gov.uk.
First published July 2021.
ISBN 978-1-78659-338-2
Views expressed in this report are not necessarily those of the Department for Work and Pensions or any other government department.
Executive summary
Introduction
The Personal Support Package (PSP) was introduced from April 2017 for new claimants in the Employment and Support Allowance (ESA) work-related activity group (WRAG) and their equivalents in the Universal Credit (UC) Limited Capability for Work (LCW). Eligibility was later widened to all ESA and UC Health Journey claimants. PSP is funded for 4 years.
The PSP offer consisted of tailored support from Jobcentre Plus (JCP) work coaches, plus a wide range of new initiatives as described in Annex A. This evaluation focussed on the implementation and delivery of the first 18 months of PSP as a whole, and the implementation and delivery of the Health and Work Conversation (HWC) as an initiative integral to the PSP. The evaluation consisted of a large-scale survey of 1,808 claimants who were eligible for PSP plus qualitative research with claimants and JCP staff in four case study areas that were delivering a PSP initiative, Journey to Employment (J2E) and two areas that were not delivering J2E. The HWC research consisted of a survey of 1,006 ESA and UC claimants who had experience of the HWC and was complemented by three qualitative case studies focussed on implementation and delivery of the HWC.
PSP key findings
Claimants health and readiness for work
The most commonly reported health condition among claimants in the PSP survey was a mental health condition (83% of respondents).
The majority of claimants (93%) reported having more than one health condition or disability.
Among claimants currently out of work 60% said they could work in the future if their health improved, 31% said their health ruled out work now and in the future and a small proportion (9%) could work now if the right join or support was available.
Support offered and taken up as part of PSP
Around two-thirds of claimants (65%) recalled being offered some form of general support, such as help with job search, condition management, money management or developing an action plan and 42% of all claimants took up at least one of the options offered.
14% of claimants recalled being offered one of the four external programmes highlighted in the PSP survey (namely the J2E, Work Choice, Work and Health Programme and, Specialist Employability Support), and 7% took up a place on one of these programmes. Claimants took up the support for a variety of reasons including for work-related reasons, to improve their health, to build confidence and not being sure if participation was voluntary.
Similarly, a range of reasons for not taking up support were reported, with the most common barriers being poor physical or mental health, a lack of confidence and the provision not being suitable for claimants’ needs for example, when mental health treatment was prioritised over PSP provision.
Experiences of and outcomes from PSP support
Three quarters (75%) of claimants in the PSP survey who said they received support from a work coach reported that they had found it helpful. The majority of claimants (59%) felt the support provided had been suitable to their needs.
Around two-fifths (42%) of claimants said that their confidence increased as a result of the support and advice they had received from their work coach.
46% of claimants said that the support and advice received had increased their motivation to find work.
Nearly half (44%) of respondents who had taken up support reported participating in work-related activities as a result of the support received, this included 13% who had found some form of work.
Key findings from the Health and Work Conversation (HWC)
The purpose of the HWC is to help individuals identify their health, personal and work goals, draw out their strengths, make realistic plans for the future and build their resilience and motivation. For ESA claimants, four techniques, ‘About me’, ‘My values’, ‘My 4 Steps’ and ‘Action Plans’ are used during a mandatory work focused interview prior to the Work Capability Assessment (WCA). For UC claimants on a health journey these can be used throughout the claimant journey, at work coach’s discretion.
Delivery of the HWC
The format and content of HWC training that staff reported receiving varied significantly in terms of duration and format. More experienced staff did not report gaining new skills but those who were less experienced reported developing in-depth interviewing skills on the training.
The majority of claimants in the HWC survey could recall experiences of one or more of the four HWC techniques, although a substantial minority (41%) did not recall experience of any techniques.
Overall, claimants were comfortable with the topics covered by the HWC, but they were less comfortable discussing their health than they were discussing their qualifications, work or money.
The qualitative research across both ESA and UC case study areas found that work coaches did not always use all four HWC techniques for a variety of reasons, including claimant’s health and time constraints.
Engagement with the HWC
For ESA claimants, the HWC was prior to the WCA which created a challenge for some ESA claimants, who were concerned that if they engaged in work-related discussions, this may prejudice the outcome of their WCA.
Claimants reported that location and surroundings could have a negative impact on engagement.
Both JCP staff and claimants perceived that the HWC and accompanying techniques were less effective for certain claimant groups, particularly those closest to and furthest from the labour market.
Where no HWC follow-up took place, almost half of all claimants felt it would have been useful.
Overall, claimants participating in the HWC survey felt comfortable with the HWC, with UC claimants highlighting that their on-going relationship with their work coach provided a strong framework for building relationships.
Acknowledgements
The authors would like to thank colleagues at the Department for Work and Pensions (DWP) who managed and supported this evaluation; Sophie Gerrard, Susanna Greenwood, Will McKinnon, Jo O’Shea, Sarah Kenny, Catherine Flynn and Janet Allaker.
We would also like to thank colleagues from Jobcentre Plus offices and external providers who gave up their time to participate in an interview. We are also grateful for ESA and UC claimants who took the time to participate in this research.
Finally, we would like to thank colleagues at the National Centre for Social Research, particularly to Ionela Bulceag, Sal Mohammed and Emma Sayers who provided support with the qualitative fieldwork.
The authors
This report was authored by researchers at the National Centre for Social Research:
Amelia Benson, Senior Researcher
Tim Buchanan, Research Director
Joe Crowley, Senior Researcher
Malen Davies, Research Director
Anna Marcinkiewicz, Senior Researcher
Katariina Rantanen, Researcher
Bethany Thompson, Research Assistant
Karen Windle, Director of the Health and Social Care team
Glossary of terms
Access to Work – a programme that helps disabled people start or stay in work. It provides practical and financial support to those who have a disability or a long term physical or mental health condition.
Access to Work Mental Health Support Service (AtW MHSS) – a programme that provided six-month support for claimants with a potential start date with an employer, but who were unsure of their ability to sustain employment without support.
Claimant - Throughout this report, the term ‘claimant’ is used to describe those benefit recipients who were eligible for support under the PSP.
Claimant Commitment – an agreement formed with Universal Credit claimants, comprising their job search or other requirements.
Community Partner (CP) – a specialist role employed by Jobcentre Plus for their expertise and local knowledge of disability issues. Worked with work coaches, local third sector organisations and employers to build relationships and strengthen their understanding of disabilities. The role ceased on 31st March 2019.
Disability Employment Adviser (DEA) – specialist Jobcentre Plus staff who provide support and advice to JCP work coaches and other staff to support their work with claimants who have a health condition or disability.
District Provision Tool – a locally updated intranet site for Jobcentre Plus staff, with information on local support and initiatives suitable for DWP claimants.
Employment and Support Allowance (ESA) – a type of unemployment benefit offering financial support to people who are not in work due to a health condition or disability.
Personal Support Package (PSP) – a suite of programmes and initiatives introduced in 2017 to support people who are not in work due to a health condition or disability move closer to employment.
Health and Work Conversation (HWC) – a mandatory work-focused interview for ESA claimants which is scheduled at the beginning of their claim and held prior to their Work Capability Assessment. For UC claimants, HWC techniques can be spread out across several appointments and work coaches can use their discretion to use the most appropriate elements.
Jobcentre Plus work coach – frontline DWP staff based in Job Centres who deliver personalised support and interventions across all benefits, coaching and supporting claimants into work by challenging, motivating, providing personalised advice and applying knowledge of local labour markets.
Journey to Employment (J2E) – Peer-led job clubs delivered by Disabled Peoples’ User Led Organisations / voluntary organisations.
Limited Capability for Work group (LCW) – claimants are placed in the LCW group after the WCA, when the claimant’s ability to work is reduced by their physical or mental health condition and it is not reasonable to require them to work.
Limited Capability for Work Related Activity (LCWRA) – claimants are placed in the LCWRA group after the WCA, when their ability to work is so limited by their physical or mental health condition that they are not required to work or to undertake any work-related activity.
Permitted Work – This is paid employment that ESA claimants can undertake if they work less than 16 hours per week and earn up to a maximum of £125.50 per week.
Provider – an organisation external to the Jobcentre Plus, providing a contracted employment support programme or service for claimants.
Single Point of Contact (SPOC) – a member of Jobcentre Plus staff selected to manage the relationship with providers of Personal Support Package initiatives and promote their provision within the Jobcentre Plus.
Small Employer Adviser (SEA) – a specialist that works with local small employers to identify opportunities for claimants with health conditions or disabilities and match people to jobs under the Small Employer Offer. The role ceased on 31st March 2019.
Small Employer Offer (SEO) – a PSP initiative where Small Employer Advisers work with local small employers to identify opportunities and match people to jobs.
Specialist Employability Support (SES) – a programme delivered by a range of provider organisations, to support people with a disability or health condition and complex support needs.
Support Group – people claiming ESA and UC are placed into different groups depending on the extent to which their illness or disability affects their ability to work. Those claiming ESA in the Support Group and those claiming UC in the Limited Capability for Work or Work-Related Activity group are considered to have such severe health conditions that there is no current prospect of them being able to undertake work or work-related activities.
Universal Credit (UC) – a DWP monthly benefit for those out of work or on a low income, replacing six previous benefits and tax credits including Jobseeker’s Allowance, Employment and Support Allowance, Income Support, Child Tax Credit, Working Tax Credit and Housing Benefit.
Universal Credit health journey – a group of people who have a health condition and/or disability which restricts their ability to work and claim Universal Credit. Claimants have either provided acceptable medical evidence prior to the Work Capability Assessment or been found to have Limited Capability to Work or Limited Capability for Work Related Activity after a Work Capability Assessment.
Work and Health Programme (WHP) – a programme mostly delivered by external providers, providing personal support to improve the claimant’s skills, manage their health condition and match claimants to jobs.
Work Capability Assessment (WCA) – an assessment that measures the extent to which illness or disability affects one’s ability to work, undergone by all ESA claimants and those UC claimants with a disability or health condition that prevents or limits their ability to find work.
Work Choice (WC) – a specialist disability employment programme delivered by a range of provider organisations, that offered work entry support and up to two years in-work support for people with disabilities. Referrals to Work Choice stopped in 2017.
Work Coach Team Leader – a member of Jobcentre Plus staff who manages and supports a team of work coaches.
Work-Related Activity Group (WRAG) – people claiming ESA are placed into two groups depending on the extent to which their illness or disability affects their ability to work. The work-related activity group are required to have regular interviews with an work coach and undertake work-related activities.
List of abbreviations
| Abbreviation | Explanation |
|---|---|
| CP | Community Partner |
| EA | Employer Adviser |
| DEA | Disability Employment Adviser |
| DWP | Department for Work and Pensions |
| ESA | Employment and Support Allowance |
| PSP | Personalised support package |
| HWC | Health and Work Conversation |
| J2E | Journey to Employment |
| JCP | Jobcentre Plus |
| JSA | Jobseeker’s Allowance |
| SEA | Small Employer Adviser |
| SEO | Small Employer Offer |
| SES | Specialist Employability Support |
| UC | Universal Credit |
| WC | Work Choice |
| WCA | Work Capability Assessment |
| WHP | Work and Health Programme |
| WRAG | Work-Related Activity Group |
Summary
Introduction
The Personal Support Package (PSP) was introduced from April 2017 for new claimants in the Employment and Support Allowance (ESA) Work Related Activity Group (WRAG) and their equivalents in the Universal Credit (UC) Limited Capability for Work Group (LCW). Eligibility was later widened to all ESA and UC Health journey claimants.
The PSP offers an enhanced menu of employment support options designed to be tailored to people’s individual needs and move ESA and Universal Credit (UC) claimants on a health journey closer to work. PSP is funded for four years from April 2017.
The PSP offer for year 1 (April 2017- March 2018) consisted of tailored support from JCP work coaches, plus a wide range of new and existing initiatives aimed at both work coaches and claimants (as described in Annex A). Some support was scheduled to run throughout the 4-year period, while other support was only planned to run between 12 to 18 months.
Evaluation approach
The Department for Work and Pensions (DWP) commissioned the National Centre for Social Research (NatCen) to evaluate the implementation and delivery of the first 18 months of PSP as a whole, and the implementation and delivery of the Health and Work Conversation (HWC) as an initiative integral to the PSP.
The evaluation of the PSP aimed to explore:
- Jobcentre Plus (JCP) staff views and experience of the implementation and delivery of the PSP
- eligible claimants’ reasons for taking up or not taking up support offered as part of the PSP
- claimants’ perceptions of the support offered by the PSP
- early outcomes of PSP support
The PSP research consisted of a survey with ESA and UC claimants who were eligible for the PSP (a total of 1,808 claimants participated), plus four qualitative case studies focused on the implementation and delivery of the Journey to Employment (J2E) programme, and an additional two case studies undertaken in areas which did not offer J2E. The latter focused on the implementation and delivery of all PSP strands.
The evaluation of the Health and Work Conversation aimed to explore:
- JCP staff and claimants’ experiences of the implementation and delivery of the HWC
- whether effective goals were set and followed up as part of the HWC
- any potential improvements to the HWC
The HWC research consisted of a survey of 1,006 ESA and UC claimants who had experience of the HWC and was complemented by three qualitative case studies with staff and claimants, focussed on implementation and delivery of the HWC.
PSP key findings
Claimants health, readiness for and attitudes towards work
The most commonly reported health condition among claimants in the PSP survey was a mental health condition (83%).
The majority of claimants (93%) reported having more than one health condition or disability.
Three-quarters of claimants (75%) reported that their health condition or disability caused them at least moderate problems when carrying out daily activities.
The majority of claimants in the PSP survey (93%) perceived their health as a barrier to returning to work.
Among claimants currently out of work 60% said they could work in the future if their health improved, 31% said their health ruled out work now and in the future and a small proportion (9%) could work now if the right job or support was available.
Staff awareness and understanding of the PSP
Staff awareness of the aims of the PSP and the initiatives under it was varied.
Some staff were able to identify all elements that constitute the PSP, but it was more common for staff to know of only some of the initiatives available to claimants and be unaware that existing provision had been altered or expanded to be incorporated into the PSP.
This may in part be a consequence of the staggered rollout of some elements of PSP and the fact that some elements were only available in selected districts.
Type of support offered to claimants as part of PSP
Staff referred and signposted claimants to four main types of provision: Pre-employment support / training; In-work support; Health and Disability- related services and other general provision.
Around two-thirds of claimants (65%) identified being offered some form of general support, such as activities that supported them with their job search, managing their health, making lifestyle changes, or developing an action plan.
14% recalled being offered one of the four external programmes highlighted in the PSP survey.
Decision-making and referrals to PSP and general provision
A range of factors influenced whether claimants were offered support, the most significant of which were severity of their health condition and proximity to the labour market.
Similarly, a range of factors influenced which provision work coaches referred claimants to. These included staff awareness of provision, promotion of provision by other staff, the work coach’s relationship with particular providers and feedback of provision from previous referrals.
Perceived likelihood of acceptance onto a programme and staff workload also played a part in determining referral pathways.
Support taken-up
Among all claimants responding to the PSP survey, 65% recalled being offered general support by their work coach, and 42% of all claimants reported taking up at least one of the support options offered.
This support included external provision, advice on managing their health condition or disability, money management, applying for jobs, making general lifestyle changes, accessing locally available support for their health condition, and developing an action plan.
In terms of the external PSP programmes highlighted in the survey, 7% of claimants said they took up at least one of these four initiatives (J2E, Work and Health Programme (WHP), Specialist Employability Support (SES) and Work Choice (WC)). Take-up was highest for J2E.
Reasons for taking up provision included wanting support with job applications, health-related issues, and confidence building.
From the qualitative analysis, there were three interrelated factors that influenced whether a claimant took up the offer of support: claimant motivation, the voluntary nature of participation and encouragement from work coaches and providers.
Barriers to taking-up support
A range of reasons for not taking up support were reported, the most common barriers being poor physical or mental health, and lack of confidence/anxiety. In the case studies it was also reported that support was not taken up because the provision was not suitable for claimants’ health needs, for example, when mental health treatment was prioritised over PSP provision.
For some claimants participating in the case studies, there was concern about the negative financial implications of moving into work. Negative perceptions of employment support also prevented participation.
Experiences of support
Experiences of support were largely positive. Three quarters (75%) of claimants in the PSP survey who said they received support from a work coach reported that they had found it helpful. The majority of claimants (59%) felt the support provided had been suitable to their needs.
Those who said that their health ruled out work now and in the future were more likely (60%) to report that support they received was not suited to their needs compared to those who could return to work straight away in the right job (45%).
The qualitative case studies found that views on the J2E programme among those who engaged in part or in all of the programme were particularly positive. On the whole, J2E participants found the peer support valuable, and both claimants and staff viewed J2E providers positively.
However, a peer support setting was not always appropriate for people with social anxiety.
Outcomes from PSP support
Around two-fifths (42%) of claimants who had accessed support said that their confidence increased as a result of the support and advice they had received from their work coach.
46% of claimants said that the support and advice received had increased their motivation to find work.
Qualitative interviews with claimants indicate that the drivers of improvement were increased confidence in managing their own health condition, improvements in self-esteem, and confidence in looking for work.
Nearly half (44%) of claimants who had taken up support reported participating in work-related activities as a result of the support received. This included volunteering or education and training.
Among those who took up support, 12% found some form of work. 8% had found permitted work, 3% had found part-time work, and 3% full-time work.
Those who reported no increase in confidence or motivation to find work as a result of advice and support from their work coach gave the following reasons for it: health barriers, the fact that their confidence/motivation did not depend on support from their work coach, and a lack of support from their work coach.
Key findings from the Health and Work Conversation (HWC)
The purpose of the HWC is to help individuals to identify their health, personal and work goals, draw out their strengths, make realistic plans for the future, and build their resilience and motivation.
Training staff to conduct the HWC
The format and content of HWC training that staff reported receiving varied significantly. The duration of the training ranged from one hour to two days, and it was delivered in a range of formats including face-to-face training, e-learning, and as part of the wider UC work coach training programme.
Staff who undertook the longer training reported HWC training gave them a good understanding of the purpose and structure of the HWC. Less experienced staff valued learning new skills and improving their in-depth interviewing skills.
Delivery of the HWC
The majority of claimants recalled discussing their health / ability to work with work coaches, even if they could not remember the four individual techniques used. Many claimants in the HWC survey could recall taking part in one or more of the four HWC techniques (“About Me”, “My Values”, “My 4 Steps”, “Action Plan”), although a substantial minority (41%) did not recall using any techniques.
Recall of individual components of the HWC varied by both claimant characteristics and by claimant journey.
Overall, claimants were comfortable with the topics covered by the HWC. However, it is important to note that, in general, they were less comfortable discussing their health than other topics. This may in part be a consequence of the use of open plan settings for the HWC[footnote 1].
The qualitative ESA and UC case studies found that work coaches did not always use all four HWC techniques.
Factors affecting engagement with the HWC
A range of operational constraints and personal characteristics affected engagement in the HWC.
For ESA claimants, the HWC was prior to the Work Capability Assessment (WCA). The timing created a challenge for ESA claimants, who were concerned that if they engaged in work-related discussions, this may prejudice the outcome of their WCA.
Claimants reported that location and surroundings had a negative impact on engagement, with open plan offices limiting the extent to which they could discuss personal or private issues.
Both JCP staff and claimants perceived that the HWC and accompanying techniques were less effective for certain claimant groups, particularly those closest to and furthest from the labour market.
Goal setting and follow-up
Around a third of claimants (30%) recalled agreeing actions or goals in their meetings with work coaches.
Claimants on ESA were most likely to set physical and mental health related goals, whilst those on UC were more likely to set work-related goals. This could be connected to the timing of the HWC, which can occur much later in UC.
Work coaches felt that the policy intention of claimants setting their own goals was essential to ensure ownership and follow through with the goals that were set.
Where no HWC follow-up took place, almost half of all claimants felt it would have been useful (48% of ESA claimants and 49% of UC).
Conclusions of PSP and HWC
PSP
Overall, the claimant perspective on support and advice received from their work coach was positive, with three quarters of claimants in the PSP survey finding the support provided either ‘very’ or ‘fairly’ helpful.
Reported outcomes were more mixed, with two fifths of claimants who took up support saying that the support and advice they had been offered by their work coach had increased their confidence and motivation to move closer to work. Similarly, direct work-related outcomes were mixed. Among those who took up some form of support, 44% said they engaged in work-related activity as a result of the support, such as volunteering, training, education or employment.
Running throughout both the quantitative and qualitative findings, there is a clear thread about the role played by type and severity of health condition or disability and the wider factors influencing distance from the labour market (such as age and education) in determining which claimants are likely to benefit most from support and advice offered by their work coach.
The findings indicate that tailoring and targeting of support is important to ensure claimants’ main barriers to work are addressed and the support meets their needs. Those with severe health conditions are likely to benefit from help targeted at supporting them to overcome their health and confidence related barriers, whereas those closer to the labour market benefit, with less severe conditions, will continue to benefit from work-focused support.
HWC
A significant minority of claimants did not recall taking part in any HWC techniques. While this will undoubtedly be driven by the challenge of recognising and recalling the specific initiatives in some instances, it is worth reflecting that the claimants least likely to recall the techniques were those who were furthest from the labour market. It is with these claimants that staff reported tailoring or choosing not to use HWC techniques. Building rapport and having adequate time and an appropriate setting to use HWC techniques were central to staff delivering the HWC as it was designed.
HWC techniques were felt to be less effective for those who were furthest from the labour market. It was also felt to be less useful for those closest to the labour market, with a job to return to. Similarly, it was felt to be less useful for older people close to retirement or those who had complex needs, such as drug and alcohol dependency.
However, overall, claimants in the HWC survey felt comfortable with the HWC, with UC claimants for example, highlighting that their on-going relationship with their work coach provided a strong framework for building relationships. Half of claimants in the HWC survey, who did not have a follow-up, would have liked one.
1. Introduction
1.1 Policy context
In 2017, the Government made a commitment to supporting one million disabled people into work over the next 10 years and working to ensure that everybody is given the opportunity to reach their potential. The 2017 Command Paper ‘Improving Lives: Work, Health and Disability’ outlined a range of actions to achieve this goal.
This included the introduction of an enhanced offer of employment support for Employment and Support Allowance (ESA) or Universal Credit (UC) claimants on a health journey, called the Personal Support Package (PSP). The PSP encompasses a range of employment support which can be tailored to people’s individual needs with the overall aim of moving people closer to the labour market or into work.
The Department for Work and Pensions (DWP) commissioned the National Centre for Social Research (NatCen) to evaluate the implementation and delivery of the PSP as a whole, and the implementation and delivery of the Health and Work Conversation (HWC), an initiative integral to PSP.
1.2 Aims of the evaluation
The overarching aims of the PSP evaluation were to explore:
- Jobcentre Plus (JCP) staff views and experiences of the implementation and delivery of the PSP
- PSP eligible claimants’ reasons for taking up/not taking up support
- perceptions of support among PSP eligible claimants who took it up
- early outcomes of PSP support
The overarching aims of the HWC evaluation were to explore:
- JCP staff and claimants’ experiences of the implementation and delivery of the HWC
- whether claimant goals were set and followed-up after the HWC
- any further improvements to the HWC needed
Alongside NatCen’s evaluation, DWP has commissioned independent evaluations of the Small Employer Offer (SEO) and the Work and Health Programme (WHP); both of which are elements of the PSP.
1.3 Overview of the Personal Support Package
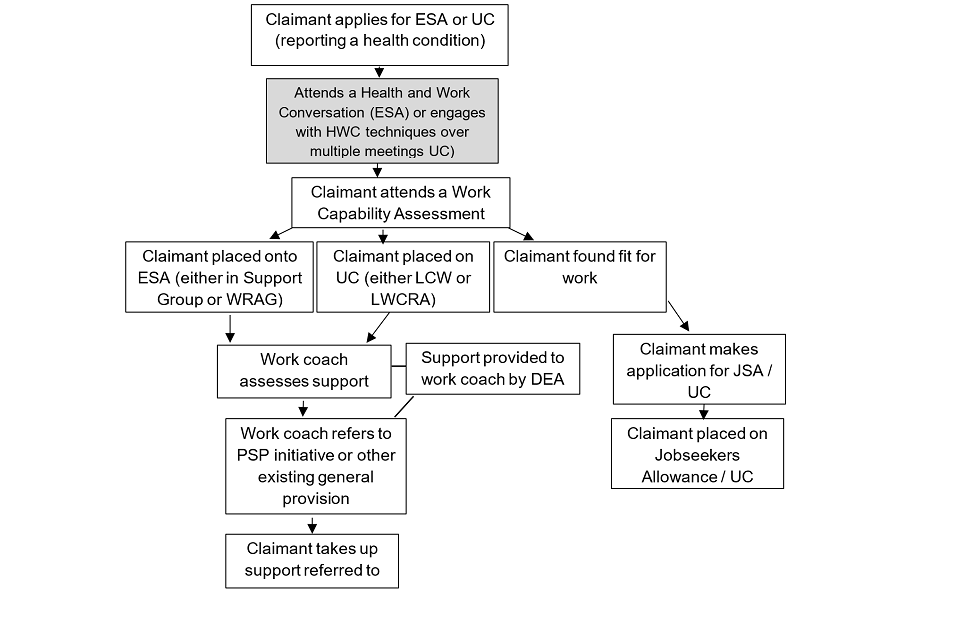
The PSP includes a range of measures and initiatives that aim to support ESA or UC claimants on a health journey. The individual components of PSP are outlined below, and the anticipated claimant journey is set out in Figure 1.1. The PSP package is scheduled to cover four years from April 2017. This research focuses on the package delivered within the first year to 18 months from April 2017 to November 2018.
1.3.1 PSP initiatives
During the first year of the PSP the package covered tailored support delivered by a JCP work coach plus a number of additional strands listed below.
New Initiatives
1. Small Employer Offer (SEO)
2. Journey to Employment (J2E)
3. Mental Health Training for work coaches
4. Community Partners - new JCP job roles
Extra places on existing provision
5. Work Choice
6. Work and Health Programme (WHP)
7. Specialist Employability Support (SES)
8. Access to Work Mental Health Support Service (MHSS)
Proofs of Concept (small scale tests in selected areas)
9. JCP led Personalised Support
10. Specialist Advice
11. Local Supported Employment
12. Young Persons Supported Work Experience
13. Work Related Activity Group (WRAG) intensive support
Other
14. Extra DEAs to support work coaches and other staff
15. Health and Work Conversation
Details of each initiative are provided in Annex A.
1.3.2 Health and Work Conversation (HWC)
The Health and Work Conversation (HWC) was launched in 2017 as part of the PSP. It is a mandatory work-focused interview for ESA claimants that is scheduled at the beginning of the claim and held prior to their Work Capability Assessment (WCA). For UC claimants, the HWC is not delivered in a single mandatory appointment, rather work coaches are encouraged to use elements of the HWC in their regular meetings with claimants on a health journey.
The purpose of the HWC is to help individuals to identify their health and work goals, draw out their strengths, make realistic plans and build resilience and motivation. The HWC comprises of 4 techniques:
- “About me”: A form that the claimant completes prior to or at the start of the HWC. It includes questions on claimant’s interests and skills, the effect of health on the claimant’s life, previous employment, and self-reported support needs
- “My Values”: An optional exercise used to encourage claimants to become more open to challenges
- “My 4 Steps”: A 4-step process where the claimant identifies a specific goal they would wish to achieve (for example, undertaking voluntary work), details any internal obstacles or barriers and sets out a plan to overcome those obstacles
- “Action Plan”: The purpose of the action plan is to support claimants to overcome external obstacles (for example, housing or debt issues). The outcomes of this exercise are measurable actions. For example, the claimant might find out more about a particular area online, or the work coach might refer the individual to further support across the DWP. For UC claimants, actions are recorded in the Claimant Commitment which can include both voluntary and agreed mandatory actions
Figure 1.1 Claimant journey
1.4 Methods
A mixed method approach was employed to evaluate both the PSP as a whole and the HWC in particular.
The quantitative strand of the research consisted of two large-scale national surveys of claimants, one focused on the PSP and one on the HWC.
The qualitative research applied a case study approach for both PSP and HWC. For the evaluation of the PSP, this involved in-depth interviews with JCP staff, ESA and UC claimants who had been offered and/or taken up one of the four PSP strands highlighted in the research (J2E, WHP, SES and WC), and externally contracted providers of employment support. The HWC case studies involved observations of HWCs, interviews with JCP staff, and ESA and UC claimants on a health journey who had experience of HWC techniques.
1.4.1 Quantitative methods
1.4.2 PSP survey
A quantitative telephone survey of 20 minutes was undertaken with ESA and UC claimants who were eligible for the PSP across England, Scotland and Wales. The survey took place between August and November 2018. In total, 1,808 individuals took part in the survey.
Sample and response rates
The sample issued for the PSP survey included 24,141 claimants. Of the initial sample 2,590 did not have valid phone numbers and were excluded from the final sample size used to calculate response rates. A further 738 were screened out because they reported that they had not attended the Job Centre. The sample issued for the PSP survey by DWP included 20,813 claimants and the survey achieved a response rate of 9%. An important requirement for this study was to ensure inclusion of those claimants who chose to access one of the four externally provided strands of PSP that were highlighted in the research (J2E, WHP, SES and WC) as well as those who did not take up any of these options.
Questionnaire
A total of eight cognitive interviews were carried out on a number of the survey questions prior to finalising the questionnaire. Cognitive interviews aim to investigate how people understand specific questions and how they recall information.
The full questionnaire and the cognitive interview report can be found in the technical report.
Weighting
Findings were weighted to the profile of all those eligible for PSP support at the start of the survey by gender, age group, region, and broad disability type (for example, mental health condition and physical health condition). Full details can be found in the technical report.
1.4.3 HWC survey
A quantitative telephone survey of 20 minutes was undertaken with ESA and UC claimants on a health journey who were eligible for HWC across England, Scotland and Wales. The survey took place between November and December 2018. In total, 1,006 individuals took part in the survey; 500 UC claimants on the health journey and 506 ESA claimants.
Sample and response rates
The sample issued for the HWC survey by DWP included 1,091 ESA and 4,663 UC claimants and achieved response rates of 46% and 11% respectively. DWP provided 2,228 ESA and 13,144 UC contacts. Two screener questions were introduced to ensure that claimants attended meetings at the Job Centre since the start of their ESA/UC claim and that they had a health condition; this screened out 137 ESA and 619 UC claimants. The difference in response rate may be explained by the different time points from which the samples were drawn. The ESA sample was drawn on a weekly basis between 22th October and 12th November 2018 to capture claimants who had undergone their HWC within the last four weeks. This ‘immediacy’ may have encouraged a greater response. In contrast, the UC sample was drawn at a single time point (22nd October 2018). This resulted in the inclusion of those UC claimants who had been claiming this benefit for a range of time periods, and who might not have had their HWC recently.
Weighting
Findings were weighted to the profile of all those eligible for HWC at the time of the survey, by age/sex and region. Full details can be found in the technical report.
Questionnaire
Pilot interviews were conducted with 30 claimants; 16 with UC claimants and 14 with ESA claimants. These telephone interviews took an average of 20 minutes. The pilot questionnaire included the following sections: participant demographic characteristics, experience of the HWC, setting goals, follow-up meetings, and perceived outcomes of the HWC. Following the pilot, a series of changes were made to the mainstage questionnaire. The final questionnaire can be found in the technical report.
1.4.4 Interpreting quantitative findings
The quantitative findings are based on frequencies and cross-tabulations of questions included in both surveys. This report explores how (and if) experiences and views of claimants differ by a range of socio-demographic factors including age, gender and education, as well as variables collected as part of both surveys on self-reported health status and attitudes towards work. All percentages cited in this report are based on the weighted data and are rounded to the nearest whole number. All differences described in the text (between different groups of people) are statistically significant at the 95% level or above. This means that we can be 95% sure that any difference we find in the survey data represents a difference in the total ESA /UC benefit population. Further details of significance testing and analysis are included in the technical report. All figures presented in the report include valid percentages excluding ‘don’t know’ responses.
Analysis on the impact of support covers all those who had received support from their work coach, as well as support from the four PSP strands highlighted in this research (J2E, WHP, SES and WC). The WHP, whilst part of the PSP, is a large-scale intervention that is subject to a separate evaluation.
1.4.5 Qualitative methodology
PSP case studies
Six case studies were conducted between May 2018 and September 2018. Four case studies focused on the implementation and delivery of the J2E initiative. The remaining two explored the wider implementation and delivery of the PSP in areas where J2E was not available. Case studies were selected to ensure the sample included JCP Districts in both rural and urban areas and there was a mix of areas where UC been rolled out for new claimants and places where this was yet to happen.
Within each case study, telephone and face-to-face group interviews were conducted with work coaches, Work Coach Team Leaders and Disability Employment Advisors (DEA). Telephone interviews were carried out with Community Partners, J2E providers and Small Employer Advisors (SEA), whilst telephone or face-to-face interviews were held with claimants who had either taken up a place on one of the four external PSP strands highlighted in the research or had been offered but declined this support. A total of 74 interviews were conducted.
HWC case studies
Three case studies were conducted between June and September 2018. Case studies were selected to ensure the sample included a mix of areas where UC been rolled out for new claimants and places where this was yet to happen. Additionally, a mix of rural and urban locations were included to take account of differences driven by local labour market conditions.
Each case study included one-day observation of HWC appointments, telephone interviews with work coaches, Work Coach Team Leaders and DEAs and a mix of telephone and face-to-face interviews with claimants who had some experience of the HWC techniques. In total 52 interviews were conducted.
1.4.6 Interpreting qualitative findings
The reporting of qualitative findings deliberately avoids using numerical language, as qualitative methods are designed to explore issues in depth rather than generate data which can be analysed numerically. The qualitative samples have been purposively selected to ensure the achieved sample has range and diversity. This approach to sampling is a hallmark of quality in qualitative research.
Verbatim quotes are used throughout the report to illuminate findings. Quotes from JCP staff and external providers are labelled to indicate job role, whether UC was live in the case study areas and whether J2E was available. Quotes from claimants are labelled to indicate the benefit type and whether J2E was available in the case study area.
1.5 Limitations
The following limitation should be considered when reading these evaluation findings; the PSP and HWC surveys and qualitative case studies relied upon claimants’ recall of their meetings with the work coach, support offered or taken-up. Recall of HWC techniques may have been difficult owing to claimants attending multiple appointments with their work coach, specifically in the UC context.
1.6 Report outline
This report presents the findings from the qualitative case studies (i.e. J2E, the wider PSP initiatives and the HWC) and quantitative claimant surveys (PSP and HWC).
Chapter Two draws on findings from the PSP survey of claimants and describes the claimants’ attitudes to and feelings about work.
Chapter Three uses data from the PSP case studies and claimant survey to explore the types of support claimants were offered.
Chapter Four draws on the same data and describes the types of support taken-up. This chapter also outlines the barriers and facilitators to take-up of support.
Chapter Five presents findings from the HWC case studies and claimant survey.
Chapter Six draws on all the data collected from across the case studies and both surveys identifying the perceived claimant outcomes.
Finally, Chapter Seven provides suggested improvements to the PSP and HWC.
2. PSP Claimant Survey – Impact of health on attitudes to work
This chapter describes claimants’ health alongside their attitudes towards paid work now and in the future, drawing out differences within the claimant group.
Although this evaluation focuses on the take-up and outcomes achieved as a result of engagement with PSP initiatives, both the PSP and HWC surveys also explored claimants’ attitudes to health and work. This was important as attitudes to health and work for claimants with a health condition or disability are likely to have implications on the level of take-up of support offered, as well as the types of outcomes claimants might achieve.
2.1 Claimants’ health
All claimants who responded to the PSP survey had a health condition or disability and many had multiple complex health needs. The majority of claimants reported that their condition affected them in at least two ways (93%). Over eight out of ten (83%) of claimants reported that their condition or illness affected their mental health. The most commonly reported condition was mental health, reported by 83% of claimants (Figure 2.1).
Figure 2.1 Whether claimants’ condition or illness affects them in any of the following areas
| Condition or illness | Percentage (%) |
|---|---|
| Mental health | 83% |
| Learning or concentrating | 64% |
| Stamina, fatigue or breathing | 55% |
| Mobility | 56% |
| Memory | 53% |
| Dexterity | 42% |
| Social or behavioural | 40% |
| Vision | 22% |
| Hearing | 15% |
| Other | 7% |
Base: All respondents (1808). Note: PSP claimants could select more than one answer option at this question so the percentages in the figure do not total one hundred.
When claimants were asked to choose the main way in which their health condition affected them (for example, vision, memory, mental health), two main issues emerged. Mental health was the most commonly reported way in which participants’ health affected them, identified by 41% of people, followed by mobility related issues, reported by 18%. No other main health condition was selected by more than 4% of claimants. A further fifth (22%) of claimants responded to say that the different areas they were affected in were equally important and they could not choose between them.
There were differences by age, with younger people more likely to report mental health as their main health condition (48% of 16 to 24-year-olds compared with 28% of 55 to 78-year olds). In relation to mobility issues, 28% of 55 to 78-year-olds reported these as their main health condition compared with 11% of 16 to 24-year olds. To identify the severity of people’s health conditions, claimants were asked how much their health condition or disability limited their ability to carry out everyday activities. 15% said that they had no or slight problems carrying out everyday activities. Around a third (31%) described their problems carrying out everyday activities as moderate, with around a quarter (28%) identifying these as severe. 16% of claimants said they were unable to carry out their everyday activities (Figure 2.2).
Figure 2.2 How much health condition/disability limits everyday activities
| Level of problem | Percentage |
|---|---|
| No problems carrying out everyday activities | 5% |
| Slight problems | 10% |
| Moderate problems | 31% |
| Severe problems | 28% |
| Unable to carry out everyday activities | 16% |
| Differs too much to say | 10% |
Base: All respondents (1798)
2.2 Readiness to work
In the PSP survey 91% of claimants were not in paid employment. Of these, over half were out of work and had been claiming ESA or UC for more than two years. Those who were not in paid employment were asked what, in their view was, preventing them from finding work. Claimants were offered a number of barriers to choose from and the majority (93%) reported that their health condition or disability was a barrier to finding work. Although a fifth of claimants (21%) reported more than one barrier to finding work, health was the most commonly reported reason that was stopping claimants from working, followed by a lack of confidence in applying for jobs (8%).
Figure 2.3: Duration of current benefit claim
| Duration | Percentage |
|---|---|
| Less than 3 months | 3% |
| 3 months or more but less than 6 months | 3% |
| 6 months or more but less than a year | 11% |
| Between 1 and 2 years | 29% |
| More than 2 years | 53% |
Base: all those claiming benefits at the time of the survey (1645)
Among claimants in the PSP survey who were not in work, nearly a third (31%) reported that their health condition ruled out work now and in the future. A further 60% felt that work might be a possibility in the future if their health improved. 9% reported they could seek paid work now, if the right job and/or support was available (Figure 2.4).
Figure 2.4: Readiness to work
| Readiness to work | Percentage |
|---|---|
| Health rules out work now and in the future | 31% |
| Might be able to work in the future if health improves | 60% |
| Could work now if right job/support was available | 9% |
Base: All respondents currently not in work (1532)
Claimants in the PSP survey who were not in paid employment were also asked to what extent they would like to find paid employment in the future (either full or part-time). A majority of these claimants (64%) said they would like to work to a great or some extent. Under a fifth (19%) said that they would not like to work at all (Figure 2.5).
Figure 2.5 Extent to which claimants would like to work in the future
| Extent | Percentage |
|---|---|
| Not at all | 19% |
| A little | 17% |
| To some extent | 25% |
| To a great extent | 39% |
Base: All respondents currently not in work (1482)
When claimants in the PSP survey who were not currently in work were asked when they might be ready to undertake paid work, a third (33%) estimated that they may be ready within the next twelve months. A further third envisaged that they would be able to work in the more distant future (19% in between one to two years’ time and 22% in 2 years or more). A quarter (26%) felt they would never be able to work (Figure 2.6).
Figure 2.6 When in the future claimants will be able to undertake paid work
| When | Percentage |
|---|---|
| In the next year | 33% |
| In between 1 and 2 years | 19% |
| Later than 2 years | 22% |
| Never | 26% |
Base: All respondents currently not in work (1224)
2.3 Differences in attitudes to work
Attitudes to work amongst claimants in the PSP survey, who were not in paid employment at the time of the survey, differed by the severity of their health condition. Nearly half (47%) of those who were unable to carry out every day activities said they could not work (now or in the future) owing to their health status, compared with 13% of those who had no problems carrying out everyday activities. This measure of how severe people’s health condition is based on a survey question how much people’s health problems affect their ability to perform everyday activities. Answer options ranged from having no problems, to slight, moderate, or severe problems, to being unable to carry them out at all. Where severity of health condition is referred to elsewhere in the report, it is this question being to measure it.
Differences in attitudes to work were also observed in relation to the type of health condition reported by claimants in the survey. Those with mobility-related health conditions were more likely to say that this ruled out work now or in the future, compared with those living with mental health conditions (47% compared with 20%) (Figure 2.7).
Figure 2.7 Attitudes towards work, by main health condition
| Attitude | Mental health | Mobility |
|---|---|---|
| Health rules out work, now and in the future | 20% | 47% |
| Currently unable to work, might be able to in the future if health improves | 70% | 49% |
| Could work now if right job/support was available | 9% | 4% |
Base: All respondents currently not in work who reported mobility or mental health as their main health condition (mental health: 589; mobility: 294)
Claimants in the PSP survey attitudes to work also differed depending on their age, education, and length of benefit claim. Those groups more likely to identify that their health condition ruled out work as an option, now or in the future, included:
- those 55 and over: 47% of those aged 55 and over compared to 12% of 16-24-year olds
- those with no qualifications: 39% of those with no qualifications compared with 25% with A levels or above
- those claiming benefits for more than 2 years: 34% compared with 26% of those claiming for less than 6 months
2.4 Summary
The most commonly reported health condition or disability were mental health conditions, reported by 83% of claimants. The vast majority of claimants also had more than one health condition, with 93% of claimants reporting 2 or more.
Health was the main barrier identified as affecting claimants’ ability to enter into paid employment, reported by 93% of claimants, with the next most commonly reported barrier (a lack of confidence in applying for jobs), reported by only 8%.
The majority of claimants in the PSP survey (60%) reported that they might be able to work in the future if their health improved, with 9% saying they could work now if the right job/support was available.
Around a third of claimants (31%) reported that their health status ruled out work as an option now or in the future. This view was more prevalent among claimants whose health conditions limited their daily activities; those with mobility-related health conditions; in the older age groups (over 55); among those with no qualifications; and those who reported claiming benefits for more than 2 years.
3. Support offered under the Personal Support Package
This chapter explores staff awareness and understanding of the PSP and the processes for offering and referring ESA and UC claimants to support, including PSP initiatives. This chapter also covers staff views of factors that affected support offered to claimants.
3.1 Staff awareness and understanding of the PSP
3.1.1 Awareness of the PSP aims and initiatives
Awareness of the PSP aims differed among staff, with newer colleagues being less familiar with the PSP programme compared to more established colleagues.
Staff awareness of specific PSP initiatives also varied widely. There were examples of work coaches and Work Coach Team Leaders who were able to identify all initiatives offered as part of the PSP (Initiatives are described in further detail in Annex A). It was more common for staff to be able to identify only some of the initiatives within the PSP. For example, there were staff who did not realise that as part of the introduction of the PSP, extra spaces or support had been ring-fenced on the Work and Health Programme (WHP) or Access to Work for Mental Health Support Services. There was also limited knowledge that additional spaces had been funded on Work Choice (WC).
The range in levels of awareness is likely to be due to three factors. Firstly, some of the PSP strands were only available in selected areas and others were introduced via a staggered roll-out. Secondly, staff may have been aware of some strands under terms different to the descriptions used in the research interviews. Finally, workload pressures may have meant that staff had limited time to absorb all the PSP information circulated, for example, the fact that extra places on some existing programmes were now badged as part of the PSP offer.
Awareness of the increased numbers of Disability Employment Advisers (DEAs) and the introduction of Community Partners as part of the PSP similarly varied. Although the role of the DEA changed prior to the launch of the PSP, there were staff who had mistakenly associated the change in role focus (from a claimant-facing position to an advisory role working primarily with Jobcentre Plus staff) as part of the PSP, while others perceived the change to be related to the roll-out of UC. There were examples of staff initially lacking any awareness of the role of Community Partners, although this changed as Community Partners became more visible and integrated themselves into Jobcentre Plus (JCP). For other staff, although they were familiar with the Community Partners as individuals, there was limited understanding of how the role related to the PSP. In some circumstances (when PSP was first launched), Community Partners felt that there was a lack of clarity among all staff about their role and those of the DEA and Small Employer Adviser (SEA). This lack of clarity led Community Partners to feel cautious around interacting with the role of DEAs in supporting work coaches and the role of SEAs when contacting local employers.
There is a lot of overlap with what the small employer advisers do, what the Community Partners do, what the employer advisers do, what the DEA coaches do. I don’t think it was clearly thought through where the remits were and where the boundaries were, so there was a lot of dancing around each other because people were frightened of stepping on each other’s toes.
(Community Partner, ESA)
Over time, as staff across all grades in JCPs became more familiar with their role and the support they could provide. Community Partners reported that positive working relationships developed, and DEAs and/or work coaches began to approach them for advice and support about specific cases.
The PSP qualitative case studies indicated that PSP was introduced to staff in a variety of ways. There were a range of ways work coaches and DEAs had learned about the PSP, including through:
- attendance at launch/presentation given to staff by a team leader
- online via either e-learning, email or the DWP intranet
- one-to-one discussions with managers or other staff such as SEAs
- presentations about specific initiatives (rather than the PSP as a whole)
- team meetings
- workshops on delivering PSP
View on how PSP was introduced to staff were mixed. Some work coaches and DEAs reported being dissatisfied with the way PSP had been introduced. In some circumstances work coaches were dissatisfied because they perceived that their team leaders lacked knowledge of the PSP, which made it difficult to get a comprehensive overview. Other work coaches felt that the eligibility criteria had initially been unclear, making it challenging to identify who the PSP was targeting (although this was resolved once the eligibility criteria had been broadened to include any ESA claimant or UC claimant on a health journey). There were also mixed views on whether written information via email was a helpful way to introduce the PSP. In some circumstances, staff felt that there was too much information to absorb, while others reported that the information was too limited. Finally, work coaches and DEAs reported that there had been a time lag between launch and implementation, which made it more difficult to retain and use any information. This last finding may be in part a reflection of the staggered rollout of some of the PSP strands. There were a group of DEAs who were happy with the way PSP had been introduced. In particular, they found presentations from JCP staff and provider organisations, which provided details of the support on offer to claimants, a useful way of understanding different strands of the PSP.
3.2 Type of employment support offered
Evidence from the staff interviews suggest that claimants were referred or sign-posted to four main types of provision, these were:
- pre-employment support or training including PSP initiatives but also other specific provision such as nationally-recognised Security Industry Authority (SIA) and Construction Skills Certification Scheme (CSCS) training, and employability courses delivered by the National Careers Service. Claimants were also offered work experience through the JCP
- in-work support for those who had found and started work. Support was also offered through the Access to Work and Access to Work Mental Health programmes. However, there were few examples of this being offered
- health and disability-related services including NHS mental health services. For example, cognitive behavioural therapy (CBT) for customers with anxiety, depression or stress; Attention Deficit Hyperactivity Disorder and autism support; and drug- and alcohol-dependency recovery support
- other general provision focused on soft-skill development, including confidence building, basic IT skills, reading courses and local social groups
Staff became aware of provision via a variety of sources, including:
- knowledge from work coaches, DEAs and Community Partners
- District Provision Tool (DPT), a locally updated database of health and disability related support that all JCP staff can access
- internal documents using software such as OneNote that listed training and general provision
- providers’ visits to the JCPs to promote the support available.
3.3 Decision-making and selection of PSP strands and existing general support options
3.3.1 Roles and responsibilities of Jobcentre Plus staff
In all PSP case study areas, work coaches were the main decision-makers when considering which support to offer to claimants, in line with the policy design. Work coaches decided which support options were suitable for a claimant, discussed their ideas with the claimant, and managed the referral process where relevant. Several factors that influenced decision-making are discussed below in 3.3.2 and 3.3.3.
In exploring which support options are available and suitable for a claimant, work coaches were able to access advice and support from DEAs.
DEAs were also able to offer three-way conversations with the work coach and claimant. The extent to which DEAs were utilised by work coaches depended, in part, on the work coach’s experience. Long serving work coaches were more likely to report feeling confident that they could identify the right support for claimants without the need of DEA support.
Work coaches and DEAs across all case study areas reported that DEAs were not always available to offer support owing to their own high workloads.
Community Partners reported that initially they had been instructed to support work coaches by upskilling them to offer appropriate advice and support to claimants, rather than provide direct support to claimants. While this continued to be a key part of their role, in case study areas where J2E was not available, some Community Partners explained that over time they began to provide support to claimants via three-way appointments with the claimant and work coach.
What they [work coaches] find most valuable is these three-way interviews where I talk to a customer and actually share some of my own lived experience, that very special bit of my role which isn’t there for other civil servants. Claimants are responding to that and they’re working with work coaches in a way they hadn’t before, yes.
(Community Partner, UC)
Work coaches described using other sources of support to help decide which support options would be appropriate for a claimant. This included:
- less experienced work coaches accessing advice from those with more experience
- engaging in case-conferences[footnote 2] with other work coaches (and DEAs)
- speaking to providers directly about what the provision will involve
- referring to internal emails which promoted provision
3.3.2 Staff and provider factors affecting referrals to external provision
There were multiple factors that influenced which external provision work coaches referred claimants to. These were:
- staff awareness of provision
- work coach relationship with external provider
- feedback from previously referred claimants
- programme availability and the likelihood of acceptance
- staff workload
Staff awareness of provision
Staff reported that their awareness of the provision on offer was an important determinant of the referrals that were made.
The District Provision Tool was one information source used by work coaches in identifying available initiatives, although some staff had difficulties accessing this on-line tool due to a lack of training on how to do so. Other sources of information included the Disability Hub (an internal source of information), other on-line guidance and information from other JCP staff. Since some work coaches were not aware of all external provision some staff were more likely to use well-promoted initiatives. For example, WHP was highly visible within Jobcentre Plus as referral numbers were closely monitored. This visibility had a positive impact on work coach referrals.
For some provision, such as J2E, there was a designated lead role at the JCP known as the Single Point of Contact, who played an important part in increasing referrals by keeping the provision at the forefront of work coaches’ minds, even when providers were not present.
Relationships with providers
The relationship between individual providers and staff was an important factor in encouraging referrals. For example, J2E providers reported that they aimed to develop good relationships with staff by spending time at the Jobcentre Plus and getting to know work coaches on a one-to-one basis. Building rapport with staff helped them to explain the benefit of their projects. Providers across all programmes also attended events at JCPs to encourage referrals. For example, one work coach reported that biannual health fairs were established where existing providers of general support could meet staff and explain the aims of their provision.
Relationship-building was reported as particularly important when provision was based on cohort entry. For example, J2E providers reported that they worked particularly closely with the JCP staff when a new 12-week programme was due to start. This had a positive impact on referral numbers; providers and JCP staff reported that as relationships strengthened, referrals increased.
Towards the end - it was a … bit of a false start to us, but towards the end I think the working relationship with our community employment specialist (role within J2E) was really getting there and she was becoming part of the work coach team.
(Work Coach Team Leader, UC)
Feedback from previous referrals
Work coaches found it helpful to hear from the providers about the progress of the claimants that they had referred as this demonstrated the potential benefits of the provision. Similarly, claimants themselves gave feedback to work coaches during and after their participation. Positive feedback received from claimants encouraged future referrals. Similarly, claimants themselves gave feedback to work coaches during and after their participation. Positive feedback received from claimants encouraged future referrals to both existing general provision or PSP initiatives on offer, while negative outcomes or bad feedback discouraged referrals to both types of provision.
The provision you use is very much based upon … your experience, I suppose, of that provision. It’s really hard. You shouldn’t have it, but you do. You have your, I wouldn’t say favourites, but you know what I’m saying. You have those that you think have got more chance of success, I guess.
(Work Coach, ESA)
Ease of acceptance onto provision
A further factor that influenced the number of referrals to provision was the ease of acceptance onto the provision. Referrals to other specific provision such as programmes being run by a Further Education college, were viewed positively as work coaches reported hearing quickly whether the claimant they had referred had been accepted onto the provision. Work Coach Team Leaders and DEAs reported it was particularly difficult to promote referrals to PSP initiatives when work coaches had lots of information about other specific provision which they found simple to refer to in contrast to specific PSP initiatives such as the WHP. Some staff were reluctant to refer to PSP providers where acceptance was not guaranteed.
Staff workload
Staff found the Specialist Employability Support (SES) referral process complex, in particular where the provider was based outside of the local area. In these circumstances staff had to spend long periods of time organising for a provider to visit the local JCP to meet the claimant. This was reported as time-consuming and difficult to do when staff had large caseloads. Some staff reported that the relative ease of referring to specific providers influenced which provision they offered to claimants.
The introduction of UC was also perceived by DEAs and Work Coach Team Leaders to make it difficult for work coaches to focus on referrals to external provision. During the UC training period, such activity was viewed as a competing priority, particularly when staff were out of the office for several weeks of training.
3.3.3 Staff views on claimant factors affecting referrals to external provision
JCP staff and providers identified several claimant-related factors that affected referrals to external provision initiatives.
Eligibility
As outlined in the introduction, when the PSP was launched, eligibility criteria for the initiatives was initially limited to ESA WRAG claimants (and UC equivalents) who had made an application for ESA or UC since April 2017. Work coaches found at the early stages of the PSP, the number of eligible claimants was very small.
At the time the [Personal Support Package] came about there was a huge backlog of work capability assessments … And that’s why we had so few people who had the right outcome decision for it.
(DEA, ESA)
Difficulty engaging claimants
JCP staff reported that it took time to build the necessary relationships with claimants that could facilitate the discussion of external provision. Staff reported particular challenges in building engagement for claimants for those that had previously been in the Support Group and had therefore not been required to attend regular appointments with their work coach.
Health condition
The severity of a claimant’s health condition was a factor in determining whether claimants were offered support as well as the type of support offered. Staff acknowledged that it would be inappropriate to ask claimants with more severe health conditions to attend certain types of provision. For example, one work coach stated:
I think [offering support] depends on the severity of their health as to what they can manage first and foremost … I would work out what they feel they can manage, it might be just interaction with me to start with to build their confidence because some find it so difficult just to get into the office, you know.
(Work Coach, ESA)
Some PSP strands were perceived as suiting claimants with particular health conditions. For example, some work coaches felt that the WHP was appropriate for claimants with mental health conditions as it provided the long-term support they were perceived as requiring. In contrast, one work coach reported that the J2E programme was not suitable for claimants who had social anxiety and/or depression as this was perceived to limit their ability to interact in a group setting (J2E is a peer support job club in a group setting).
Other claimant characteristics
Staff also reported that a range of other claimant characteristics influenced the choice of support options. For example, where claimants had drug or alcohol dependency, support to deal with this was prioritised over work-related support. Similarly, where claimants were perceived to have ‘chaotic lifestyles’, they were deemed as unsuitable for work-related support.
The duration of support was also reported as a consideration for some JCP staff. For example, the long-term support offered by WHP and SES might be seen as more appropriate for claimants with more significant barriers to work.
Proximity to the labour market and claimant motivation
Work coaches described some support options were targeted at different groups of claimants. For example, the WHP was identified as a better fit for people who would be ready for work within twelve months, while Work Choice was more appropriate for claimants who need longer term help. Work coaches also indicated that the motivation of claimants was important to consider. Willingness to move forward with their job search was identified as a factor in referrals made to the J2E programme.
3.3.4 Other factors affecting referrals
Location
Location of the provider or claimant was also felt to influence the take-up of local or PSP provision, as claimants preferred to attend provision closest to them:
[A factor that influences referrals] is the provision local. Like I say with [this] one it’s really close to the Jobcentre. Lots of people feel comfortable going there. They like the area … I hear that people feel quite comfortable that it’s going to be delivered locally and they understand exactly where they’re going.
(Work Coach, ESA)
3.4 Summary
There were varying levels of knowledge and awareness of the aims and initiatives of the PSP among JCP staff. There was broad awareness of individual initiatives and the provision available to claimants, with some staff aware of all PSP initiatives. However, others expressed limited awareness that the initiatives were part of the PSP or that existing support services had been altered or expanded as part of the PSP. A lack of uniformity in the way the PSP was introduced (in terms of staggered roll out and local differences in initiatives available) made it difficult for work coaches to understand the overarching offer available to claimants.
Work coaches were the main decision makers in suggesting which support options to offer claimants. DEAs assisted work coaches to do this through one-to-one support and/or three-way conversations between themselves, work coaches and claimants. In some circumstances, where Community Partners had specific specialist health knowledge, they also had three-way conversations with work coaches and claimants.
The qualitative case studies indicate that a range of factors influenced what provision was offered to PSP eligible claimants. These included: if staff were aware of the provision; the extent to which some provision had been promoted across JCP; staff relationships with providers; feedback and outcomes from prior referrals to provision the availability of spaces on the provision, and the likelihood of acceptance; and staff workload.
Staff also reported that claimant characteristics affected whether staff offered and/or referred claimants to local provision and PSP support. Perceived barriers (or enablers) included: eligibility of the claimant; type and extent of health condition; the location of provision; and the claimant’s proximity to the labour market.
4. Take-up of support
This chapter draws on the PSP claimant survey and PSP qualitative case studies. It discusses the support taken-up by claimants, including the factors that influenced take-up, experiences of support taken-up, any barriers encountered to participation, and reasons for dropping out of support.
4.1 Type of support taken-up
4.1.1 Support offered and taken-up
As discussed earlier in the report, PSP covers a wide range of both existing and new initiatives (including work coach support), which are focussed on helping claimants with health conditions and disabilities move closer to work. Consequently, the PSP survey explored claimants’ recall of all advice and support which they may have been offered by their work coach since the introduction of the PSP (April 2017).
Support offered
Claimants were asked about a list of possible support work coaches could offer them or refer on to, such as help applying for jobs or CV writing, but also more general support, including helping building confidence, advice on how to manage money, training to develop IT skills. The survey also asked specific questions about four externally delivered programmes within the PSP package, namely Journey to Employment (J2E), Work and Health Programme (WHP) and Specialist Employability Support (SES) and Work Choice (WC).
Overall, 65 % of claimants reported being offered one or more of the support options as summarised in Figure 4.1 below. The most commonly mentioned support option was developing an action plan (reported by 34 % of claimants).
Figure 4.1 Types of support offered by the work coach
| Type of support | Percentage |
|---|---|
| Developing an action plan | 34% |
| Info about local support | 29% |
| Training in how to look for work | 27% |
| Help to find voluntary work | 25% |
| Help with applying for jobs | 25% |
| Help building confidence | 23% |
| Help to find work experience | 21% |
| Group sessions with peers | 20% |
| Advice to manage health | 18% |
| Help with IT skills | 16% |
| Training on lifestyle changes | 15% |
| How to talk to employer about health | 13% |
| Advice on money management | 11% |
| Anything else | 2% |
Base: all respondents (1806).
Support taken-up
Out of all claimants in the PSP survey, 42% reported taking up at least one of the general support options offered by their work coach (for example, employment related support and/ or help to manage their health condition, confidence or finances). Figure 4.2 shows what type of support those claimants who recalled being offered support, then took up.
Figure 4.2 Proportion of claimants that took up support offered
| Type of support | Percentage |
|---|---|
| Advice on how to manage your health condition or disability (330) | 59% |
| Advice on money management (216) | 59% |
| Help with applying for jobs (496) | 58% |
| Training or advice on making general lifestyle changes (272) | 58% |
| Information about locally available support for your health condition (526) | 55% |
| Developing an action plan (654) | 52% |
| Help with building your confidence (442) | 52% |
| Help with IT skills (305) | 51% |
| Training in how to look for work (516) | 51% |
| Help to find voluntary work (487) | 47% |
| Advice on talking to your employer about your condition/adjustments (256) | 47% |
| Group sessions with peers (386) | 42% |
| Help to find work experience (396) | 40% |
| Anything else (89) | 62% |
Base: Number of claimants who recalled being offered each type of support (in brackets). The numbers do not sum up to 100% as respondents could select multiple options.
14% of all claimants were offered one or more of the four externally delivered programmes that were highlighted within the survey (J2E, WHP, SES and WC). The question was accompanied by a short description of the key elements of each of the programmes to help with claimants’ recall. 7% said they took up one of the four externally provided programmes. These programmes offer different types of support and are targeted at different sub-groups of claimants, so it was expected that the level of take-up of these options would vary. Table 4.1 below displays the percentage of claimants who recall being offered a place on an externally provided programme and had taken it up.
Table 4.1 Percentage of claimants that took up selected external provision highlighted in survey of those offered these programmes
| J2E | Work Choice | WHP | SES | Any of these programmes | |
|---|---|---|---|---|---|
| % of base who took up the support | 51% | 30% | 29% | 16% | 47% |
| Base: All respondents offered that programme | 196 | 109 | 104 | 66 | 257 |
Note: claimants could take up more than one programme.
4.2 Factors affecting take-up
4.2.1 Reasons for taking-up of any type of support
When asked about why they took up support, a quarter (25%) of claimants who responded to the survey (who took up some form of advice or support offered by their work coach) said they took up the support for work-related reasons. Support with health-related issues was the next most common reason claimants gave for taking up support (20%). These findings are presented in Figure 4.3.
Figure 4.3 Claimants’ reasons for taking up support
| Reason | Percentage |
|---|---|
| Work related | 25% |
| To improve health | 20% |
| Confidence building | 18% |
| Not sure if voluntary/concern about losing benefits | 13% |
| Social reasons | 9% |
| Work coach encouragement | 5% |
| Other | 10% |
Base: All respondents who took up some form of support (802)
Among claimants who took up some form of support or advice, people’s motivation for doing so differed by the severity and type of health condition. Those with less severe health conditions were more likely to take-up support for a work-related reason (56%), compared with those who were unable to carry out everyday activities (15%).
Claimants whose health mainly affected their mobility were more likely to report taking up support for work-related reasons, compared to those who reported mental health as their main condition (33% and 21% respectively). Claimants with a mental health condition were more likely to report that they took up support to help build their confidence (23%), compared to those with a physical health condition (6%).
Younger claimants (those aged between 16 and 24) were more likely to report the reason they took up support was to improve their health, compared to older claimants (55 and over) (29% and 14% respectively). This may be related to the type of health conditions claimants reported during the survey, younger claimants were more likely to report mental health related conditions as their main health condition, while older claimants were more likely to be affected in terms of mobility.
Over a fifth (22%) of claimants who believed their health condition ruled out work, now and in the future, reported taking up support or advice offered by their work coach through concern they might lose their benefit otherwise. In contrast, only 6% of claimants who reported that their health condition would not stop them from working straight away gave this response. Those with no qualifications were also more likely to give this as the reason they took up support, 19% of those with no qualifications reported this, compared with 11% of those with A levels of equivalents.
The PSP qualitative case studies found that there were three interrelating factors that influenced whether a claimant took-up the offer of a support option. These were:
- claimant motivation
- the voluntary nature of participation
- encouragement from work coaches and providers
Claimant motivation
The types of motivation that led to claimants taking up either PSP or other specific provision varied and depended on claimants’ perceived readiness to find work.
Claimants who perceived themselves to be close to the labour market and felt ready to return to work reported that they decided to participate in a support option to help them find work. Claimants who perceived themselves to be further away from work were motivated to participate in a PSP initiative or other specific provision to help them develop specific employability skills, such as in developing their CV. Others perceived that the value in such support was in the learning and application of a range of soft skills that could move them closer to the workplace, such as helping them become more active or supporting them in leaving the house.
Voluntary nature of participation
Whilst not a commonly reported response within the sample, there were claimants in the PSP qualitative case studies who identified that the voluntary nature of any PSP initiative was the primary reason for accepting a place. For example, in PSP case studies where J2E was available, claimants reported that they had taken up the programme as they felt no pressure on them to continue if they found it to be unhelpful.
It was something I wasn’t being forced into … I felt, you know, okay if I go there once, if I like it then I can continue to go back. If I don’t like it then I’m not … forced to go.
(ESA Claimant)
The voluntary nature of participation also alleviated anxiety related to trying new activities and meeting new people.
Other claimants believed that attendance at certain provision was mandatory but reported that they would have attended even had they perceived this as a voluntary initiative, as they felt it would be useful for them to attend. This suggests that although claimants may have been concerned about the risk of benefit sanctions[footnote 3], some were simply interested in taking up the offered support.
Encouragement from work coaches and providers
A group of claimants reported that it was the explanation of the PSP initiative by their work coach, that had persuaded them of the benefits and anticipated outcomes:
I decided to go because my work coach told me, they told me that it’s going to help me a lot with my CV, because the way my CV was wasn’t up to date. I needed to add stuff and then that this was kind of, it would be good for me.
(UC Claimant)
Work coach encouragement was not always welcomed by claimants. In some instances, claimants described feeling under pressure to attend the PSP initiative being offered. Examples of this included claimants who had attended J2E and said that the main reason they had joined the programme was to please their work coach. Those who attended for this reason appeared to have similar experiences to those who attended and believed it was voluntary, despite initial reservations about attending.
Interactions with the providers also influenced whether claimants took up support. For certain initiatives, including J2E, SES and WC, handover meetings took place within the JCP. Claimants reported that having these discussions alongside the provider gave them an opportunity to ask questions about the provision prior to attendance. This ensured concerns could be raised and mitigated, this being particularly beneficial for claimants who were anxious about attending provision.
In case study areas where J2E was available, J2E providers reported that they used these handover meetings to emphasise the distinction between their programme and support offered at Jobcentre Plus. They perceived such discussions as encouraging take-up, J2E often being seen as a ‘safe space’ outside the JCP. JCP staff reported that claimants who had attended handover meetings with J2E providers were more likely to attend the initiative, indicating the importance of these handover meetings in facilitating take-up.
It is having that good relationship more than anything else … that does it … about 50% of the people who … were booked in to see the [J2E provider] actually attended, at least once, anyway, the J2E Job Club.
(Small Employer Adviser)
4.2.2 Barriers to taking up support
Claimants who were offered advice and support from their work coach, but did not take anything up, were asked the reasons for this. The following section provides details on the main barriers to take-up reported by this group of claimants.
Health condition and lack of confidence
Of those claimants who were offered some form of support by their work coach and refused, almost two-thirds (62%), stated that this was because their health was not good enough. Almost four in ten (38%) identified that a lack of confidence or increased anxiety precluded attendance (Figure 4.4).
It would seem that this lack of confidence or increased anxiety is linked to perceived health status. Where claimants indicated no problems with everyday activities, a fifth (21%) reported that a lack of confidence and/or anxiety stopped them from taking-up support. In contrast, where claimants identified they were unable to carry out day-to-day activities, almost half (45%) reported lack of confidence/anxiety as a reason for not taking up support.
The qualitative interviews with JCP staff and external providers reported that mental health conditions were perceived as a key barrier to the take-up and continuation of a support option. Work coaches identified that claimants with mental health conditions were less likely to engage with provision on offer and were afraid of trying new forms of support, because they were unable to predict how support might impact their mental health condition.
Physical health conditions were also perceived as a barrier for some claimants, for example, those who had physical barriers to leaving the house.
Provision not appropriate to their needs
The PSP claimant survey found that a fifth (22%) of those who declined the offer of advice and support did so because the options on offer were not felt to be appropriate to their needs. This was reflected by the views of some claimants in the qualitative case studies. Examples of this included claimants feeling that employment-related support was unsuitable as it could not address their long-term health condition. Also, claimants prioritising drug and alcohol-dependency support or attending therapy or CBT, prior to accessing employment-related support.
Location and travel to PSP provision
While only 10% of claimants who did not take up support offered by a work coach cited transport issues as the reason for not taking up support, across all the PSP case study areas, location of provision and a lack of access to transport were reported by providers as one of the reasons why support had not been taken up. In PSP case studies where J2E was available, J2E providers in rural areas described a lack of public transport being a key barrier to attendance. J2E providers in both rural and urban areas also reported that claimants who had to travel long distances and suffered from anxiety found this difficult and exhausting, acting as a barrier to take-up.
Similarly, J2E providers reported that claimants were less likely to travel in the winter due to adverse weather and the shorter days, which had an impact on claimants’ mental health and their ability to travel in the dark.
Figure 4.4 Barriers reported by claimants to taking up general support
| Barrier | Percentage |
|---|---|
| Health wasn’t good enough | 62% |
| Lack of confidence/anxiety | 38% |
| Not appropriate to their needs | 22% |
| Worried couldn’t sustain commitment | 17% |
| Other | 12% |
| Transport issues | 10% |
| Too much time commitment/too intensive | 10% |
| Did not want to go to the jobcentre | 9% |
| Family or caring commitments | 8% |
| Inconvenient/other commitments at that time | 8% |
| Drug or alcohol problems | 8% |
Base: All respondents offered one of the general types of support who did not take-up any support (398)
Age
Views among JCP staff varied as to whether the age of a claimant influenced whether they would take up any PSP or existing general provision offered. One group of JCP staff felt that older claimants, who were further from the labour market, were less likely to take up support and were more likely to drop out of support. There was the perception amongst staff that older claimants were closer to retirement and did not see themselves as working in the future.
In contrast, other staff felt that older claimants were willing to access support and there were no demographic differences in take-up. JCP staff with this view, explained that younger claimants usually presented with mental health conditions and prioritised mental health-related support over employment-related support. These claimants did not feel ready to think about work while experiencing conditions such as anxiety or depression.
Concern about the financial implications of moving closer to employment
JCP staff also perceived that some claimants were afraid of taking up support as this would move them closer to the labour market, which they worried may have negative implications for the type of benefit they were entitled to claim. This was reported to be particularly relevant for claimants with anxiety or other mental health conditions:
People who have … mental health problems have that fear of breaking free from their safety net …. Even though the benefits system is trying harder to help people to be able to do things without losing everything at the same time … there’s still that big fear that it’s going to be down to them to do something and if they can’t, then … they might lose their home.
(Work Coach, ESA)
Negative perceptions of employment support
Work coaches described occasions where claimants had declined the offer of a support option on the basis that they had either had a negative experience of accessing employment support previously or, had accessed support and not achieved any positive outcome.
4.3 Experiences of support received
4.3.1 Positive experiences of support
Claimants who took up advice or support offered by their work coach were mostly positive about what they had received. Three quarters (75%) of those who participated in one of the four external programmes highlighted or accessed other advice and support from their work coach, reported that they had found it helpful, while 12% found it unhelpful. These findings are presented in Figure 4.5.
Figure 4.5 Experience of support among all claimants who took up some support
| Claimant experience | Percentage |
|---|---|
| Very helpful | 37% |
| Fairly helpful | 38% |
| Neither helpful nor unhelpful | 12% |
| Fairly unhelpful | 6% |
| Very unhelpful | 6% |
Base: All respondents who took up some form of support (843)
Over half (59%) of claimants who took up some form of support also said that the support received had been suitable to their situation and needs. Those identified as living with less severe health issues were more likely to feel that the support was suitable. Almost three-quarters (73%) of claimants who indicated they had no problems carrying out everyday activities, identified that the support was suited to their situation and needs. In contrast, just over half (51%) of those unable to carry out every day activities acknowledged this. Similarly, those who felt ready to return to work now were more likely to say support received suited their situation and needs (61%) compared with 48% of those who felt their health ruled out work, now and in the future. Findings from the PSP qualitative case studies mirrored these findings, with claimants who perceived themselves ready to work being the most positive about the support received.
Peer support
J2E participants who reported a positive experience of the programme attributed this to engaging with others with similar health conditions or disabilities, as well as those facing similar barriers to work. These claimants reported building friendships and support networks, where they shared practical advice and developed solidarity, helping each other to increase their self-confidence. The J2E programme lasted for 12 weeks and each cohort met once or twice a week during this time. Among claimants who enjoyed the peer support element, this weekly routine was central to their positive experience enabling them to complete something productive each week with a support network of peers. A further benefit cited by those claimants with positive experiences of J2E was the opportunity to hear about others’ experiences of managing health, general condition management and learning about working with their disability or illness.
Being in a group of people with the same problems as yourself and with lots of other problems was life-changing for me, to know that you are not a - you are not weird or a freak or that lots - if not - everybody suffers with different things some time in their lives.
(ESA Claimant)
Some claimants also described being inspired and encouraged by others through non-employment-based advice, such as tips for better physical health and sleeping.
However, the peer support format was not suitable for everyone. J2E providers reported that there were examples of claimants who were unable to engage in a group setting.
Claimants also reported that the group setting could provoke anxiety, whether for them individually or others in the group that they attended. Some claimants who observed that others found the peer support element difficult, reported this to be disruptive during the 12-week programme.
Supportive providers
Experiences with J2E facilitators were described positively. Claimants who participated in the PSP case studies felt that the J2E providers had lived experience of their health conditions or disabilities and viewed them as a source of support in both work-related and non-work-related issues. Relaxed and welcoming J2E facilitators also encouraged claimants to participate at their own pace.
There was no sort of right or wrong thing to do in the meetings or anything, it was exactly how you feel about it and it was up to you to whether you sort of joined in or not or whatever. You weren’t under any pressure to do anything or say anything.
(ESA Claimant)
Claimants undertaking other types of provision also reported that supportive staff were important. For example, a claimant on the WHP described their provider being friendly, understanding and non-judgemental, which encouraged them to see the provision in a positive light:
[She was a] lovely lady, and she talked me through and we made a CV together. Then she told me about whatever options that were available at that point, more of what they do, and yes, it was then that I started to smile inside and thinking well, hopefully this is going to end up somewhere.
(ESA Claimant)
Other positive aspects of support taken-up
Claimants who participated in the PSP case studies also regarded support to be high quality when:
- providers explained a disability to employers during the application process or prior to employment beginning, which reduced the burden on the claimants having to broach the topic with a prospective employer themselves
- providers offered job-brokering or matching or told claimants about jobs being available before they were advertised, giving claimants a longer lead-time to prepare their application
- support included one-to-one support with job search (this was reported in case study areas where J2E was not available); CV development; and support to develop employability skills such as job search/interview techniques
4.3.2 Negative experiences of support
J2E participants who were close to the labour market reported some frustrations with the provision. Claimants who were ready to find work found that working alongside those who were further from the workplace slowed the pace of activities. Discussions at J2E job clubs were not always tailored to individual needs. For example, discussions around health were not always relevant to those focusing on finding work. This led to some drop-outs, with some claimants finding alternative provision, such as training courses, which they felt would be more suitable to their needs.
In some of the case study areas, where J2E was not offered, claimants who had a negative experience of support explained this was because it had not been tailored to their needs.
4.3.3 Reasons for dropping out of support
Claimants and JCP staff who participated in the PSP case studies provided a range of reasons as to why claimants dropped out of a support option, including:
- untargeted support: there were a group of claimants who had either previous long work histories or perceived themselves to be immediately ready to move into work, who stopped attending support. This group perceived the support to be too basic or had been offered advice that they felt did not met their needs. For example, a participant with a long work history, but who had been out of work for a number of years, was hoping for support that could refresh his computer skills. In contrast, his advisor focused on how he should sell his previous work experience on his CV, which he felt was already one of his strengths
- accessibility of provision: there were some claimants who explained that they could not afford to travel the long distances required to attend the support they had been offered. While some claimants were aware that they could claim back expenses, they could not afford to pay the travel costs upfront
- deterioration of health condition: there were examples of claimants whose health condition had become worse since starting a support option. For example, a claimant with a mental health condition that had deteriorated during their participation in J2E explained that it had become too difficult for them to concentrate during the sessions
4.4 Summary
Among all claimants in the PSP survey, 65% recalled being offered general support options by their work coach for example, employment related support and/ or help to manage their health condition, confidence or finances and 42% reported taking up at least one of these. 7% of claimants said they took up one of the four externally provided programmes on PSP (J2E, WHP, SES and WC).
Of those who took up support almost a quarter (24%) did so for work related reasons, whilst 19% took up support to improve their health. Support was more likely to be taken up by those who felt their health was less of a barrier to returning to work and/ or reported higher levels of education.
The PSP qualitative case studies found that claimants closer to the labour market were motivated to take up support to help them find work, while those with more severe health issues, and further away from the labour market wanted to develop confidence, motivation or employability skills.
Nearly two thirds (62%) of claimants in the PSP survey who had been offered some form of support and refused it, had done so because their health was not good enough. Over a third (38%) of claimants said they had not taken up support offered because of a lack of confidence or anxiety. Health was also cited as a key barrier to taking up support in the PSP qualitative case studies.
Generally, claimants in the PSP survey reported positive experiences of the support taken up. The majority of those who took up support found it very or fairly helpful (75%) and suited to their situations and needs (59%). The PSP qualitative case studies found that most people who attended peer support provision J2E, found it beneficial to be in a group with others in similar situations. However, the case studies found that the group setting was not always suitable for all claimant groups. Those with social anxiety or who felt they were closer to work than their peers, struggled with the group setting. Where claimants in the qualitative sample had a negative experience of support taken up, the support had not been pitched at the right level and/or activities were not always perceived as relevant to all participants. Drop-out from provision occurred where those closer to work felt provision was pitched at too basic a level for them; where there were issues with the accessibility of provision or participants’ health had deteriorated.
5. The Health and Work Conversation
This chapter outlines the findings of the Health and Work Conversation (HWC) claimant survey, observations and qualitative interviews carried out with both claimants and JCP staff. It includes an overview of JCP staff views on the training received to deliver the HWC and describes how the HWC was delivered in both ESA and UC settings. Findings on the experiences of HWC are presented separately for ESA and UC claimants throughout this section due to the fact that delivery of the HWC is different for claimants receiving ESA and UC.
5.1 Staff perspective on HWC training
As part of the launch of HWC across JCP, staff were scheduled to receive one or two-days of face-to-face training focusing on how to deliver HWC. On-line training was also made available to complement the face-to-face sessions.
Format and content of training received
Staff interviewed reported a range of training formats and variation in the content of training. Staff in ESA case study areas reported receiving face-to-face HWC training that ranged in length from a one hour-long training session to a two-day training session. There were also some limited examples of work coaches receiving online training on the HWC, which supplemented the face-to-face training.
ESA work coaches who had received one or two-days’ training recalled that the training focused on explaining the aims of the HWC, as well as how to practically implement the techniques and use the HWC booklet. The HWC booklet provides work coaches with guidance on how to guide the conversation with claimants. A range of training methods were applied, such as role-play, to deliver the different techniques and small group work to explore different health conditions. Shorter training (one hour or half a day) focused on similar themes but did not include role-play.
In UC case study areas, staff who had been in their role a year or longer described receiving a one or two-day long face-to-face HWC training, which was similar in content to that received by ESA work coaches. Feedback from newer staff suggests a change in the delivery of HWC training over time. Work coaches who had been in the role for less than a year reported either receiving no HWC training, training via a three-hour e-learning module, or HWC training embedded in their general UC work coach training.
Views and outcomes of training
UC and ESA work coaches, Work Coach Team Leaders and DEAs who had undertaken one or two-day long HWC training or training through e-learning modules reported gaining a good understanding of the purpose and structure of the HWC. Those who received shorter training felt that they had not received enough information or guidance about the HWC. However, staff views on the extent to which training enabled them to develop new skills varied by experience. Those staff who had more experience in the role did not report gaining new skills from the training, highlighting that they felt that the solution-focused approaches introduced were already used by work coaches or, in the case of DEAs, had been taught in previous DEA training. According to staff, a solution-focused approach is one where time is spent not on the claimant’s challenges, but on solutions to overcome them. The claimant should come up with the solution themselves to increase their ownership over it. In the HWC context, staff referred to “My Values” and “My 4 Steps” as solution-focused techniques.
In contrast, ESA work coaches with less experience and who were new to the role reported that the training provided them with new skills, including in-depth interviewing skills, such as how to ask open questions. Among this group of work coaches, those who had experienced role-play found it helpful. There was, however, another group of work coaches who found role-play uncomfortable or ‘artificial’.
Where staff reported dissatisfaction with the training, this was due to the following factors:
- e-learning modules made available to UC staff were reported to thoroughly explain techniques, but did not provide opportunities to practice these through, for example, role-play
- the length of time between training and delivering the first HWC was too long; some ESA work coaches reported having forgotten the content of training
- training delivered by less experienced trainers was reported to lack structure and comprehensiveness
Staff suggested the following improvements to training:
- support to deal with a range of claimant needs: Less experienced staff would have appreciated training around a wider range of health conditions and different types of claimants, for example, claimants with mental health conditions, those with complex needs or those presenting as angry or upset at the JCP[footnote 4]
- opportunity to practice: Staff would have welcomed a longer period of the training dedicated to practicing the techniques and skills being taught. Work Coach Team Leaders suggested that work coaches may benefit from being observed to assess whether they were using techniques correctly
- reduced time between training and implementation: Staff wanted training to take place closer to the delivery dates of HWC. A time lag between training and delivery meant that recall of training was poor
- equal division of theory and practical training: Staff suggested splitting training over two days, with one day for theory and another day for practical implementation of the HWC
5.2 Structure and delivery of the HWC
For ESA claimants, HWC techniques (“About Me”, “My Values”, “My 4 Steps” and “Action Plans”) are used during a mandatory work focused interview prior to the WCA. This differs for UC claimants on a health journey, where HWC techniques can be used throughout the claimant journey, depending on the work coach’s assessment of claimant need.
5.2.1 Claimant recall of HWC techniques
The majority (59%) of ESA and UC claimants in the HWC survey recalled taking part at least one of the techniques. (Figure 5.1).
Figure 5.1 Claimants’ recall of taking part in HWC techniques
| Technique | UC | ESA |
|---|---|---|
| About me | 32% | 42% |
| My values | 14% | 22% |
| My 4 steps | 22% | 32% |
| Action plan | 39% | 30% |
| None | 41% | 41% |
Base: All respondents (ESA: 506; UC:500)
41% of ESA and UC claimants did not recall taking part in any of the techniques. This finding may, in part, be a result of the flexibility in which work coaches can use HWC techniques with UC claimants and that work coaches may exempt ESA claimants with severe health conditions. The HWC survey results show significant differences in recall by severity of health condition among ESA claimants. Almost half (48%) of ESA claimants who reported being unable to or having severe problems with carrying out everyday activities owing to their health condition, did not recall taking part in any techniques. Qualitative findings, outlined in Section 5.3, suggest that in line with DWP policy, work coaches chose not to use the techniques with some claimants with multiple or complex health conditions. Staff also noted that the open-plan office surroundings prevented claimants with particular health conditions from engaging with the HWC.
In contrast, among UC claimants on a health journey, recall of engaging in HWC techniques varied by type of health condition, feelings about work and age. Note that for UC claimants the HWC is not a single appointment, and individual techniques used across different meetings may be more difficult to recall.
Again, this may be a result of policy intent since the instructions for work coaches are to use the HWC as appropriate for UC claimants. Over half (54%) of HWC survey UC claimants, who perceived their mental and physical conditions as equally important, could not recall engaging in any techniques. Those with physical health conditions as their main health condition were more likely to be unable to recall any techniques (49%) compared to those with mental health conditions (36%).
UC claimants who perceived themselves to be far away from the labour market appeared less likely to have experienced the different techniques. Over half (55%) of UC claimants who reported that they could not see themselves working in the future did not recall engaging with any of the techniques, compared to 40% of those who felt that they could work in the future, and 35% of those who could work now[footnote 5]. UC claimants aged 35 and above were more likely to be unable to recall techniques than 16 to 34-year-old claimants (48% compared with 36% reported recalling ‘None’ of the techniques).
ESA claimants in the HWC survey were most likely to recall participating in ‘About Me’ (42%) compared with other techniques. For UC claimants on a health journey, just under a third (32%) recalled participating in the technique.
The “My Values” exercise was the technique the least recalled by claimants in the HWC survey (22% of ESA and 14% of UC claimants recalled undertaking the exercise). This is an unsurprising finding given that “My Values” was an optional exercise. Its purpose was to encourage less engaged claimants to become more open to challenges through thinking about their personal values, things that matter to them.
Recall of the “My 4 Steps” exercise was higher for ESA claimants participating in the HWC survey compared to UC claimants (32% and 22% respectively). However, in comparison to other techniques, recall of this technique was lower than others.
Over a third of UC claimants on a health journey (39%) and just under a third of ESA claimants (30%) recalled developing an “Action Plan” with their work coach.
5.2.2 Work coach views and use of techniques
As discussed above, the DWP policy is that HWC techniques are used flexibly to fit with personal circumstances. UC work coaches had been instructed to use elements of the HWC process when appropriate to claimant circumstances. ESA work coaches had been encouraged to use HWC for all ESA claimants unless the claimant’s personal circumstances warranted a waiver of the process.
The qualitative case studies in both areas where there were ESA and UC claimants found that work coaches did not always use all of the HWC techniques. The HWC case studies found that work coaches were using different techniques at different stages of the claimant journey, when they felt it appropriate. For example, a Work Coach Team Leader reported that where a claimant is noticeably very anxious at the initial appointment, work coaches would make the decision not to use the “About Me” form with them, as claimants can find it difficult to fill out forms and this could provoke higher levels of anxiety.
Work coaches had the option of spreading the HWC processes over more than one appointment for UC claimants. ESA work coaches reported that they did not always have enough time during a HWC appointment to introduce all four elements. This was either because claimants had complex health conditions or other circumstances which took time to discuss. ESA work coaches also felt one appointment did not afford them enough time to build a rapport with claimants, which they felt was needed in order to broach some of the HWC techniques (see Section 5.3 below on factors affecting engagement with HWC techniques).
A lack of time to introduce HWC techniques was also a factor influencing UC work coaches’ use of techniques. UC work coaches reported that introducing techniques required a longer meeting, which was difficult to organise when work coaches had limited availability. However, UC work coaches also reported that they had more time to build rapport through recurring meetings with the claimant and felt that this made it easier for them to introduce all four techniques over time.
Placement of the different techniques was, at times, challenging. For example, ESA work coaches reported that they did not always introduce all techniques during the HWC appointment as they perceived that not all techniques were appropriate for a particular claimant, at that stage of the claim (as described in section 5.2.3). ESA work coaches also reported departing from the HWC script outlined in the booklet where it was perceived to disrupt the flow of the conversation.
Those UC work coaches who reported not using any of the HWC techniques gave two reasons for this. Firstly, some work coaches did not feel capable of applying them because they had not yet undertaken training on the HWC. Secondly, there were some experienced work coaches not using the techniques at all, as they perceived them to be tools most useful for less experienced staff.
5.2.3 Staff feedback on the four elements of the HWC technique
The following sections describe the use of the four stages of the HWC process “About Me”, “My Values”, “My 4 Steps” and “Action Plans”.
Elements of the HWC: “About Me”
According to ESA and UC work coaches and team leaders, the “About Me” form provided a useful starting point and gave work coaches a comprehensive insight into a claimant’s life. As explained above, ESA work coaches were not always using all techniques during the HWC. Where ESA work coaches were not typically using the “About Me” form, this was in instances where claimants had a mental health condition or low self-esteem and found it difficult to approach a form, or independently identify positive aspects of their lives. Feedback on the usefulness of the “About Me” form also highlighted that conversations around what makes claimants proud could often feel stilted, as it is not something claimants are used to thinking about in their daily lives.
Elements of the HWC: “My Values”
“My Values” was the least popular technique among ESA work coaches, who found it difficult to explore personal topics with claimants during their first meeting. ESA work coaches described examples where the questions reminded claimants of how negatively their health conditions impacted their life, resulting in high levels of distress.
In contrast, UC work coaches, who had more time to build a rapport with the claimant over multiple meetings, had more positive views on “My Values”. They reported that it gave claimants the opportunity to lead the conversation and demonstrated to them that work coaches were delivering a personalised service. Elements of the HWC: “My 4 Steps Exercise”
According to ESA and UC staff, “My 4 Steps” works best when a rapport has been built, and when conversations around obstacles and goals can build on knowledge from “About Me” and “My Values”. Work coaches observed that the technique was least useful with claimants who had a physical health condition because they felt these claimants had less influence over their recovery.
Elements of the HWC “Action Plans”
The purpose of the “Action Plans” is primarily to support the claimant to overcome external obstacles, such as housing or debt issues. However, the Action Plan can also cover goals set within the My 4 Steps exercise. ESA and UC work coaches reported that this exercise worked best when it was claimant-led. However, ESA staff reported that the lack of mandatory follow-up on actions meant that it was difficult to engage ESA claimants in goal-setting for the Action Plan element.
UC work coaches and team leaders reported that the Action Plan could be used as a basis for actions specified in the Claimant Commitment.
5.2.4 Topics discussed
The HWC survey asked ESA and UC claimants on a health journey what topics they had discussed during their meeting(s) with the work coach. As Figure 5.2 shows, the most commonly selected topics were health (UC 82%, ESA 93%) and ability to work/feelings about work (UC 75%, ESA 82%). These findings are in line with DWP policy intent which provides the option of claimants discussing work and non-work related goals during the HWC discussions. This suggests that although 41% of claimants did not recall participating in specific HWC techniques, the majority had discussed their health and how it impacted on their ability to work.
Figure 5.2 Topics discussed during meetings with the work coach
| Topics | UC | ESA |
|---|---|---|
| Other commitments | 30% | 24% |
| Financial issues | 40% | 25% |
| Voluntary work | 43% | 35% |
| Personal interests | 44% | 47% |
| Details of their benefits claim | 47% | 39% |
| Training courses | 48% | 33% |
| Qualifications and work experience | 69% | 57% |
| Ability to work/feeling about work | 75% | 82% |
| Health | 82% | 93% |
Base: All respondents who attended a meeting at the Jobcentre Plus (UC: 500; ESA: 506)
As Figure 5.3 shows the majority of both ESA and UC claimants on a health journey who discussed these topics with their work coach reported feeling comfortable talking about all topics that are usually discussed during a HWC.
Figure 5.3 Proportion of claimants who felt comfortable discussing topics
| Topic | UC | ESA |
|---|---|---|
| Qualifications | 80% | 84% |
| Work | 66% | 68% |
| Money | 63% | 71% |
| Health | 58% | 65% |
Base: All respondents who discussed these specific topics with their work coach (Qualifications: 635; Work: 793; Money: 325; Health: 883)
The topic that claimants in the HWC survey were least comfortable talking about with their work coach was their health. ESA and UC claimants on a health journey who felt their health condition ruled out work now and in the future were less likely to feel comfortable discussing their health than claimants of the HWC survey who felt able to work now or in the future.
5.3 Factors affecting engagement in the HWC
Findings from the HWC case studies suggest that there were a set of operational factors and personal claimant characteristics that influenced engagement with the HWC.
5.3.1 Operational factors
Timing of the HWC
For ESA claimants, the HWC appointment is designed to take place before the WCA. However, ESA work coaches explained that claimants often used the HWC appointment as an opportunity to ask the work coach for advice on how to approach their WCA, moving the focus away from the HWC.
It’s very difficult for them to think about other things, really think about getting into work or getting ready for work or overcoming their [barriers] because their goal at that point is to get through the [work capability assessment].
(Work Coach, ESA)
ESA work coaches and claimants also reported that without the outcome of a claimant’s WCA confirmed, claimants felt they had to prove to the work coach that they were unfit for work. Work coaches described that this led to claimants using a large proportion of the meeting explaining their health condition and how it limited their ability to work. This decreased the time the work coach had to introduce and engage claimants in HWC techniques.
I just felt a bit like I was having to prove that I was unfit for work […] if you go for the medical first then … you’ve got them agreeing with you straightaway, you haven’t got to prove that you’re unfit for work, yes, the proof is there, it’s on paper.
(ESA Claimant)
Similarly, in UC case study areas, a focus on urgent matters such as housing, prevented the use of HWC exercises during the first meeting.
Until we’ve got their claims up and their housing side sorted, they’re going to be focusing on that. There’s no point in me talking about, ‘So what’s your long-term goals’? … all they’re worried about is I want the housing to be sorted now’.
(Work Coach Team Leader, UC)
Location and surroundings
The HWC qualitative case studies found that the location and surroundings of the HWC were perceived to affect engagement. Claimants in the HWC qualitative sample reported that their HWC had been carried out in an open-plan office. Claimants with health conditions like asthma or anxiety described that being in a busy room triggered or exacerbated their health conditions, distracting them from the conversation with the work coach. There were also claimants who reported feeling uncomfortable discussing personal or private issues in a space where they could be overheard by other people.
Work coaches have the option of booking a private room for appointments in locations where rooms are available. Work coaches reported two kinds of approaches to offering a private room. One approach was to always ask the claimant during a phone call prior to the appointment whether they need a private room, whilst the second was to only book a private room for ESA claimants if they were otherwise unable to attend the HWC. It was, however, sometimes difficult to predict how a claimant would react to using the open plan area.
5.3.2 Personal characteristics
It was perceived by staff and claimants that the HWC and accompanying techniques were less effective for certain claimant groups.
Length of time out of work
The HWC techniques can be used to explore goals related to work and non-work areas of life. ESA and UC work coaches reported that it was difficult to discuss work related goals with claimants who had been out of work for a long period. Some UC claimants with a long period of unemployment reported finding it difficult to engage with the HWC discussions about work related goals, since they had previously accessed employment support but not succeeded in finding work. This sub-group of claimants perceived the JCP was unable to help them and therefore disengaged during encounters with the work coach.
Claimants with short-term conditions and a job to which to return
Both ESA work coaches and claimants considered the use of HWC techniques to be unsuitable for those who had short-term physical health conditions and jobs to which they could return to. This group of claimants did not have relevant obstacles to overcome and had often already put steps in place to return to work. In these cases, the work coach has the option of wavering the HWC approach.
Mental health conditions
According to ESA and UC work coaches, the open-plan JCP environment exacerbated the symptoms of claimants with agoraphobia, anxiety or depression, which made it challenging to engage them in the techniques. ESA and UC staff also reported that claimants with anxiety and depression found it hard to complete the “About Me” form as they could not think positively and identify those areas they were good at or proud of. Some of the main external obstacles identified by claimants with a mental health condition were those they had little influence over (such as being on a long waiting list for therapy), making the formation of an “Action Plan” around external obstacles challenging.
Age
ESA and UC work coaches reported that it was difficult to motivate claimants close to retirement age to consider training in a new field of work. It was also felt that for some older claimants, a combination of lower education levels and reduced physical capability limited the pool of employment opportunities available to them. Similarly, claimants near retirement age also perceived that employers would not consider hiring someone of their age with a health condition. Note that while the finding implies that these claimants perceived the HWC to focus on finding work, the HWC and the goals formulated do not have to relate to finding work or accessing training.
Multiple and complex needs and substance misusers
ESA and UC work coaches reported that using the HWC techniques with claimants with complex or multiple needs was not always appropriate or feasible. Discussing multiple needs could take time, and work coaches found it difficult to get claimants to focus on addressing just one of their needs. Claimants with substance misuse issues also found exercises difficult to focus on and complete, especially when they were using replacement medication such as methadone. In line with the policy guidance in these instances, work coaches used their discretion and decided not to use any of the HWC techniques.
5.4 Action planning, goal-setting and follow-up
5.4.1 Action-planning and goal-setting
It is expected that actions and/or goals are set at two points of the HWC. In “My 4 Steps”, the claimant identifies a specific goal that will overcome an internal obstacle which is within their control. The goal should be an action (for example, phoning a friend if they feel anxious or worried about leaving the house). The “Action Plans” can cover goals discussed in “My 4 Steps” but can also cover other actions to overcome external obstacles, such as housing or debt issues. For example, an action could be that the claimant finds out more about the issue that they have identified, or that the claimant is referred by the work coach to DWP provision related to the issue.
The HWC survey and qualitative case studies explored the process and perceptions of goal and action plan setting, rather than identifying whether these goals could be linked to specific HWC techniques. While the qualitative interviews focused on goals set during the HWC or follow-up meetings, the survey asked about actions or goals set during any meeting with the work coach. Actions for UC claimants on a health journey are recorded on their Claimant Commitment rather than an Action Plan.
Around a third of claimants in the HWC survey (39% of UC claimants) and (30% of ESA claimants) recalled agreeing actions or goals in their meetings with work coaches. Claimants who set actions or goals were asked what kinds of actions or goals these were (claimants could choose several categories). Figure 5.4 shows the spread of answers among claimants in the HWC survey who reported developing any actions or goals. ESA claimants were most likely to set physical and mental health related actions or goals, followed by those associated with making small every day changes. In contrast, UC claimants were most likely to set actions or goals related to finding work, voluntary work or training. These differences could be related to the timing of the ESA and UC qualitative interviews, in that UC claimants were interviewed later in their claim.
Figure 5.4 Types of actions or goals agreed
| Action/goal | UC | ESA |
|---|---|---|
| How to find/get work | 72% | 51% |
| Training and voluntary work | 61% | 53% |
| Mental health | 57% | 66% |
| Small every day changes | 53% | 61% |
| Physical health | 47% | 66% |
| Childcare, housing or debt | 39% | 29% |
Base: All respondents who discussed an Action Plan (ESA: 146; UC: 188)
Work coaches reported that it was essential claimants set their own actions and/or goals, perceiving that claimants would find it easier to achieve these if they had played a role in setting them. Work coaches felt that their role was to ensure that actions and/or goals were realistic and achievable, and to help claimants identify solutions to any barriers identified in achieving those actions or goals set. The HWC survey found that the majority of ESA (73%) and UC claimants (78%) had developed their actions or goals together with their work coach.
A majority of claimants who participated in the HWC survey and set actions or goals, felt that they were achievable (85% of ESA claimants and 81% of UC claimants). A similar majority of claimants felt that their actions or goals were clear.
Figure 5.5 shows that whilst two-thirds of the interviewed ESA claimants (68%) perceived the actions or goals agreed with work coaches as voluntary, over a quarter (27%) perceived them to be compulsory. In comparison, 43% of UC claimants felt that the actions or goals were voluntary and 46% believed them to be compulsory.
These findings are likely to be linked to two factors. Firstly, actions or goals agreed prior to a WCA are voluntary for ESA claimants and both voluntary and mandatory actions can be set for UC claimants. Post-WCA actions or goals can be made mandatory for those claimants in the Limited Capability for Work group. Secondly, work coaches have discretion in terms of when to apply mandatory requirements.
The qualitative interviews with claimants mirrored these findings, with claimants unable to distinguish between the compulsory actions or goals agreed as part of their Claimant Commitment, and any voluntary actions or goals set with their work coach during other meetings.
Figure 5.5 Perception of actions or goals as voluntary or compulsory
| Perception | UC | ESA |
|---|---|---|
| Voluntary | 43% | 68% |
| Compulsory | 46% | 27% |
| Don’t know | 11% | 5% |
Base: All respondents who set goals (ESA: 135; UC: 176)
Reasons for not setting goals
Findings from the HWC qualitative case studies suggested that actions or goals were not set with ESA claimants when:
- they were recovering from a short-term health condition and had a job to return to
- they had already begun pursuing work related goals
- they found it challenging to consider and set achievable goals when they were waiting to be assessed by their GP to find out more about their health condition
- their health condition was degenerative, or their mental health condition was so severe that it did not seem appropriate to set goals
The HWC survey also found that UC claimants on a health journey with severe problems carrying out everyday activities were less likely to set goals (31%) than those with no or slight problems carrying out everyday activities (45%). There was a similar pattern among ESA claimants, where 25% of those with severe problems or unable to carry out everyday activities set goals, compared with 45% of those with no or slight problems carrying out everyday activities.
5.4.2 Follow-up
ESA work coaches are encouraged to arrange a voluntary follow-up conversation with ESA claimants to discuss progress with their actions or goals. UC work coaches have regular meetings with UC claimants on a health journey where follow-ups could be discussed.
The HWC survey asked those who had agreed actions or goals with their work coach whether they had received any further contact with the JCP about the actions or goals they had set. Half of UC claimants (51%) recalled having follow-up contact with the JCP about their actions or goals. In contrast, one-fifth (21%) of ESA claimants reported having follow-up contact. In interpreting the results, the timing of the survey must be borne in mind. While the UC claimant sample consisted of claimants at different stages of their claim, the ESA claimant sample only contained claimants up to a few months into their claim.
Work coaches in case study areas where UC was not yet live, explained that follow-up appointments with ESA claimants were optional for work coaches to arrange and were often not prioritised owing to time constraints or a focus on other claimant groups. Work coaches also reported that where they did arrange follow-up appointments, this was as a consequence of claimants fully engaging in the HWC and techniques used or where they had set up an action plan jointly with the claimant.
The HWC survey also asked those claimants who did not receive follow-up, whether they would find it useful to have follow-up meetings to discuss their actions or goals. Approximately half of both ESA and UC claimants (48% of ESA claimants and 49% of UC claimants) who did not receive a follow-up, said they would have found one useful. Claimants in the HWC survey were asked what topics they would like to discuss further with their work coach. Ability to work and feelings about work were the most commonly chosen topic for future discussion by both ESA claimants (73%) and UC claimants (65%). Support to manage health and other details of the claimant’s benefit claim were also selected as desired topics for further discussion by more than 60% of ESA and UC claimants.
5.5 Summary
Staff views on the training received varied and was influenced by the format of training they attended. Those who had undertaken one or two-day long HWC training or training through e-learning modules reported gaining a good understanding of the purpose and structure of the HWC. Whilst those who received shorter training felt that they had not received enough information or guidance about the HWC.
Staff views on the extent to which training enabled them to develop new skills varied by experience. More experienced staff did not report gaining new skills from the training, whereas work coaches with less experience and who were new to the role reported that the training provided them with new skills, including in-depth interviewing skills, such as how to ask open questions.
Claimants and staff were asked for feedback on the use of the four HWC techniques. While a minority of claimants in the HWC survey recalled taking part in all the individual techniques, the majority did recall discussing their health and ability to work/ feelings about work. This suggests these topics were being addressed during meetings even if claimants were not aware a specific technique was being used.
In line with the policy intent, work coaches’ use of the HWC techniques varied. UC work coaches were using a wider range of techniques over the course of several meetings compared to ESA work coaches, who sometimes found it difficult to introduce all four techniques during one appointment. A range of operational constraints and the personal characteristics of the claimants affected engagement in the HWC, including the timing of the HWC (prior to the WCA) and the location (open-plan office) which could be challenging, particularly for claimants with mental health conditions.
Around a third of claimants reported agreeing actions or goals in meetings with their work coach. Among claimants in the HWC survey who set goals or actions, the majority felt that these were clear and achievable.
The HWC survey and qualitative case studies found that follow-up appointments after a HWC were uncommon for ESA claimants, because they were not mandatory and therefore not prioritised due to work coach time constraints. It is noted that ESA claimants were interviewed for this research in the early months of their claim, so any follow-up appointments that occurred after this point would not have been picked up by the research. UC claimants, who were interviewed at a later point in their claim, were more likely to have had a follow-up conversation on their actions or goals, as the HWC techniques are introduced over a number of meetings. Almost half of both ESA and UC claimants in the survey who had not received a follow-up conversation, thought a follow-up appointment would have been useful. Claimants would have liked to spend time during follow-up appointments primarily discussing their feelings about work and ability to work.
6. Reported outcomes from support
This chapter draws on data from both the PSP and HWC claimant surveys and qualitative case studies with JCP staff, providers and claimants. It focuses on the reported outcomes following participation in the HWC and PSP initiatives. All outcomes reported in this chapter must be read with caution. Due to there being no counterfactual, it is not possible to determine whether reported outcomes are a direct result of PSP support.
6.1 Reported outcomes of support received
The claimant outcomes described below are those reported by claimants in the PSP survey, as a result of any support received between April 2017 and the time of the interview.
6.1.1 Confidence and motivation
The PSP claimant survey found that around two fifths (42%) of those who took up support felt that the support and advice they had been offered by the work coach had increased their confidence. A slightly higher proportion (46%) reported that it had increased their motivation to find work. These findings are presented in Figure 6.1.
Figure 6.1 Extent to which confidence and motivation have increased or decreased as a result of the support offered by the work coach
| Extent | Confidence | Motivation |
|---|---|---|
| Increased | 42% | 46% |
| Not changed | 46% | 42% |
| Decreased | 12% | 12% |
Base: All respondents who took up support and answered (confidence: 838; motivation: 825)
Some claimant groups were more likely to say their confidence and motivation to move closer to work had increased. This included those closer to work: 53% of those who said that they could work straight away reported increased confidence, compared with only 26% of those who felt unable to work now and in the future, and 40% of those who might be able to work in the future. A similar trend is seen with motivation to move closer to work in the future, with 71% of those who felt able to work straight away seeing an increase in motivation as a result of support, compared to 46% for those who think they will be able to work in the future and 18% for those unable to do so at all.
Figure 6.2 Proportion of people whose confidence increased as a result of support they received, by their feelings about work
| Feelings about work | Percentage |
|---|---|
| Health rules out work, now and in the future | 26% |
| Might be able to work in the future if health improves | 40% |
| Could work straight away | 53% |
Base: All respondents who took up support, split by feelings about work (the base for each group is shown in brackets): Health rules out work now and in the future (156), Might be able to work in the future if health improves (451), Could work straight away (98).
The age of the claimant results in differential findings around confidence and motivation. Younger people were more likely to report that their confidence and motivation to move closer to work increased as a result of the support they were offered. Half (50%) of those aged 16-24 reported their confidence increased, compared to 40% of those aged 55 and over. Similarly, 62% of those aged 16-24 reported their motivation to move closer to work increased, compared to less than a third (32%) of those aged 55 and over.
There were also differences found by education level. Those with higher qualifications were more likely to report an increase in confidence and motivation to move closer to work because of engaging in support. Two-fifths (43%) of those with A levels or above reported an increase in confidence compared with 38% of those with no qualifications. Similarly, 52% of claimants with A levels or above saw increased motivation to move closer to work compared to 39% of claimants with no qualifications.
In the qualitative case studies, claimants who had participated in J2E reported that their confidence increased in three different ways: confidence in managing their own health condition, improvements in self-esteem, and confidence in looking for work, through for example, improved knowledge of how to approach interviews.
In case study areas that were not covered by J2E, both claimants who participated in externally provided PSP provision and JCP staff, felt that claimants’ increase in confidence and motivation to move closer to work had been directly influenced by the frequent face-to-face appointments with PSP providers. Attending regular appointments gave claimants a purpose to leave the house and a routine similar to that they might have in employment. Claimants perceived that the structure and accountability associated with attending regular appointments with a JCP work coach or external provider was the first step in preparing for the workplace and made the prospect of employment feel less overwhelming.
An improvement in job search skills was also reported to increase confidence and motivation to move closer to work. Claimants who accessed regular one-to-one support with work search, support with CV development and support to develop basic computer skills, reported feeling confident to begin to look for work online and apply for jobs.
6.1.2 Developing employment skills
Claimants in the PSP survey who had received support and advice were asked if that had helped them develop skills relevant to work or to their job search. Around two-fifths (42%) agreed that it had (Figure 6.3).
Figure 6.3 Support received helped develop skills relevant to work or job search skills
| Opinion | Percentage |
|---|---|
| Agree | 42% |
| Neither agree nor disagree | 29% |
| Disagree | 29% |
Base: All respondents who took up support and answered (820)
There were some key differences between demographic groups. For example, those with less severe health conditions were more likely to report they had developed their employability skills (67%) through the support and advice received compared with those with severe health conditions (44%). Claimants with no educational qualifications were also more likely to report an increase in their employability skills (53%) compared to those with A levels or above (39%).
6.1.3 Work-related outcomes
Fewer than half (44%) of claimants in the PSP survey, who had taken-up a support option, reported then going on to participate in work-related activities, such as volunteering, training or education, employment or a work trial or work experience. As shown in Figure 6.4 the most common type of work-related activity was volunteering (26%). Of the 12% in work, 8% had found permitted work, 3% had found part-time work and 3% had found full-time work.
Figure 6.4 Work-related activities engaged in as a result of support taken up
| Work-related activity | Percentage |
|---|---|
| Volunteering | 26% |
| Training or education | 15% |
| Full-time, part-time or permitted work | 12% |
| Work trial/work experience | 5% |
Base: All respondents who took up support and answered (846). Note: This was a multicode question, so respondents could select more than one response.
Those with more severe health conditions were less likely to have taken up volunteering or work than claimants with less severe conditions. This group includes those who said they were unable to or had severe problems with everyday activities due to their health. The group described as having less severe conditions includes those who said they had slight problems or no difficulties with their everyday activities. Among those with less severe conditions a third (33%) did some volunteering, compared with one in five (21%) of those with more severe health conditions. 16% of those whose health affected them less severely reported working in either full-time, part-time or permitted work, compared to 7% of those with more serious conditions.
There were also differences by education. Those with A levels or above were more likely to take up work-related activities (54%) compared to those with no qualifications (33%). Specifically, they were more likely to take up education and training (21% compared to 6% among those with no qualifications) and some form of work (either full time, part time or permitted) (18% compared with 6%).
Both the qualitative and quantitative data suggests that claimants perceived that the support received influenced their ability to find work. In case study areas without J2E, one person in the sample had moved into work. The claimant attributed their success in finding work to the support received from an externally provided PSP provision. During their first meeting with the PSP provider, the claimant noticed jobs being advertised on a job board and mentioned this to their support worker. The support worker then phoned one of the employers on the job board and explained the claimant’s situation and health condition. The claimant met with the employer, who then employed them.
In addition to employment, volunteering and training outcomes, the PSP survey found that 44% of claimants who had taken up support felt that the support received gave them a better idea of what kind of jobs they would like to do or would be good at. These findings are presented in Figure 6.5.
Figure 6.5 Whether the support provided a better idea of what kind of jobs claimants would be good at/would want to do
| Opinion | Percentage |
|---|---|
| Agree | 44% |
| Neither agree nor disagree | 28% |
| Disagree | 28% |
Base: All respondents who took up support and answered (822)
Those with less severe health conditions were more likely to agree that the support provided gave them a better idea of the types of jobs they would be good at or want to do (78% compared to 36% of those with severe health conditions). There were also differences by education level, and a greater proportion of claimants with no qualifications (51%) agreed with this statement compared to those with A levels or above (36%).
Perceptions also varied by attitude towards work. Among those who felt their health condition or disability ruled work out now or in the future, only 29% agreed that they had a better idea of what jobs they would want to do as a result of support, compared with 63% of those who felt able to work straight away.
6.1.4 Barriers to achieving outcomes from support received
Among claimants in the PSP qualitative case studies who reported that they achieved no outcomes from the support in which they had engaged or received, three reasons were given to explain this lack of impact. Firstly, claimants perceived the work or volunteering opportunities they were referred to by providers to be too demanding for them to be able to manage alongside their health condition. Secondly, other claimants felt that the support was not pitched at the right level. This group perceived that they would benefit from a more thorough assessment of their support needs by the work coach, which would help the work coach to direct them to more suitable support.
Thirdly, among claimants who reported no increase in confidence or motivation to move closer to work, there was a view that the J2E course or other support accessed was too short to have a lasting effect on confidence or motivation to move closer to work.
Some JCP staff also perceived that employers’ negative attitudes were a key challenge that all external providers needed to overcome in order to support claimants into work. This was perceived to be particularly important for successfully supporting those with a mental health condition into work.
Some JCP staff felt that any external provider, whether that is a PSP or other external provider, could only support claimants to improve their own capabilities, and a large part of moving people forward is the claimant’s own motivation to move closer to work.
The PSP claimant survey explored the self-reported barriers to increases in confidence or motivation to move closer to work. Figure 6.6 presents the breakdown of reasons given by the group of claimants who felt that their confidence or motivation to move closer to work had not changed or decreased as a result of the support received.
Figure 6.6 Reasons support decreased or did not change confidence and motivation to move closer to work
| Reason | Confidence | Motivation |
|---|---|---|
| Health has deteriorated | 42% | 52% |
| Confidence/motivation not dependent on the support received | 34% | 25% |
| Lack of support from work coach | 15% | 10% |
Base: All respondents whose confidence (485) or motivation (434) decreased or did not change. Note: This is a multi-code question so responses do not add up to 100
As demonstrated in Figure 6.6, the most likely reason for no increase in confidence and motivation to move closer to work, was a deterioration in health.
6.2 Exploring the outcomes of HWC
As outlined in Chapter Five, the HWC allows work coaches to engage with claimants to help them to identify personal goals, draw out their strengths, make realistic plans and build resilience and motivation. This section explores outcomes of the HWC and draws on findings from the HWC survey of ESA and UC claimants and the qualitative case studies with ESA claimants who had experience of the HWC techniques.
Measuring the perceived impact of the HWC is challenging because it is difficult for claimants to isolate the impact of the HWC from general work coach support. This is because the HWC process may be covered alongside a discussion of other topics within a work coach appointment and the different elements of the HWC may be spread across a number of appointments. As result it was not feasible for the HWC survey to ask claimants about the specific impact of the HWC techniques. As a proxy measure, the HWC survey asked about the impact of the work coach appointments in general. We can speculate that some of this impact may have been a result of the HWC approach, but this cannot be verified. However, the qualitative data presented here is directly linked to the HWC because the in-depth conservations used in the qualitative interviews helped claimants pinpoint the specific impact of the HWC approach.
Increase in confidence and motivation
The HWC survey collected claimants’ views on whether their confidence or motivation to start preparing for work changed because of meetings with their work coach. Due to the differences in how HWC is delivered in ESA and UC, ESA claimants were asked about changes to their confidence and motivation to start preparing for work, as a result of a single appointment they attended early in the claim. In comparison UC claimants were asked about meetings with the work coach more generally.
The majority of ESA and UC claimants in the HWC survey, who attended meetings with their work coach, reported no change in their confidence or motivation to start preparing for work, as a result of single or multiple meetings with their work coach (Figure 6.7 and 6.8). Note that while the objective of the HWC was to build claimants’ confidence and motivation more generally, the survey questions on motivation asked specifically about motivation to start preparing for work. Where claimants did report an increase in confidence or motivation to start preparing for work, the proportion of UC claimants who said this was greater than ESA claimants. The difference seen here may be explained by the fact that UC claimants were surveyed later in their claim, so they will have attended more work coach appointments than the ESA claimants.
Figure 6.7 Whether confidence has increased or decreased as a result of meetings with the work coach
| Outcome | UC | ESA |
|---|---|---|
| Increased | 27% | 18% |
| No change | 56% | 69% |
| Decreased | 17% | 14% |
Base: All respondents who attended meetings with a work coach UC (487) ESA (496)
Figure 6.8 Whether motivation to start preparing for work has increased or decreased as a result of meetings with the work coach
| Outcome | UC | ESA |
|---|---|---|
| Increased | 29% | 20% |
| No change | 53% | 63% |
| Decreased | 13% | 11% |
| Not applicable | 5% | 6% |
Base: All respondents who attended meetings with a work coach UC (483) ESA (496)
The HWC case studies found examples of ESA and UC claimants who felt that their confidence and motivation to prepare for work increased as a result of discussing actions with their work coach or pursuing the actions that were set. For example, a UC claimant who had been out of work for two years felt that they had lost confidence in their abilities during unemployment. Their work coach encouraged them to apply for a particular job and assured them that they would be good at it, which helped them regain some confidence.
In another example, an ESA claimant who had been out of work for many years, caring for a relative, felt that they were not good at anything or qualified for any job. The work coach changed their outlook by pointing out that the care work they had done at home resembled work in the care sector. Another ESA claimant realised that they might be able to work again in spite of their health condition, when the work coach suggested a range of varied employment options, different from their previous jobs.
Referrals to support
The HWC survey also asked whether ESA and UC claimants had been told about or referred to other support, such as support to find a job, support with their health, debt, housing and childcare, as a result of meetings with the work coach. 38% of UC claimants who had attended meetings with their work coach reported being told about or referred to support. 28% of ESA claimants reported being told about or referred to other support during their HWC or follow-up.
6.2.1 Improved perceptions of the Jobcentre Plus
The qualitative case studies with ESA claimants suggest that the HWC helped to reduce worries and concerns that claimants would be expected to look for work immediately. This was the case in spite of a letter and a pre-call that ESA claimants received prior to the meeting. There were examples where the letter had contributed to claimants’ worry, due to its authoritative tone and reference to ‘work’. In addition, it enabled the claimant to feel that they were ‘working alongside’ the work coach, in partnership, rather than taking part in a formal interview. Claimants also reported that there had been an increase in transparency and understanding of their benefit claim. ESA claimants who had gone in feeling nervous or concerned came out feeling positive about their interaction with a work coach and attributed this to the ability of the work coach to put them at ease. In addition, the work coach spent time explaining that they would not be expected to look for work immediately.
Any concerns that I did have, when I actually sat down for the interview, were quickly dispelled. He handled the interview very well and put me at ease and didn’t put any pressure on me at all that I was having to start to look for work there and then.
(ESA Claimant)
The qualitative case studies indicate that ESA and UC claimant views on their work coach were almost exclusively positive, and work coaches were described as friendly, encouraging and compassionate.
6.2.2 Barriers to all types of outcomes
ESA and UC claimants in the HWC qualitative case studies who reported that they felt the HWC had resulted in a limited impact on their life, either:
- had a job to go back to after recovery from physical injury
- were not offered the courses they would have wanted by their work coach, who instead suggested they wait for the outcome of their WCA before being placed on their desired course
- perceived that the HWC did not present them with new options of support owing to their prior negative experience of a range of different initiatives
- perceived themselves too ill to consider work-related activities
These perceived barriers to outcomes reflect the perceived barriers to engagement with the HWC techniques outlined in Chapter Five.
ESA and UC claimants described further elements likely to limit effective outcomes, including the point at which the HWC takes place in a claimant’s benefit application journey available time allocated to the HWC. For ESA claimants, the lack of a private room was particularly challenging, reporting that they felt uncomfortable discussing personal topics in the open-plan office, or that the open-plan setting triggered physical or mental health symptoms. This is likely to have caused barriers to engagement and an inability to focus on the techniques being used by work coaches. There were also examples where UC claimants felt that their appointments were not long enough to have conversations about their health or job prospects, again, limiting any achieved outcomes.
6.3 Summary
In the PSP claimant survey, two fifths (42%) of claimants who accessed support through their work coach reported improvements to their confidence and 4% reported improvements to their motivation to move closer to work. Younger claimants (aged 16-24 years) were more likely to report improvements to their confidence and motivation than older claimants (aged 55 and over).
Of those claimants who took up support, 44% then went on to participate in work-related activities such as volunteering, education and training and work. Staff and claimants in the case studies identified a range of barriers to achieving outcomes, such as challenges managing work or voluntary activities alongside their health condition.
In the HWC claimant survey, the majority of claimants reported no change in their confidence or motivation to begin preparing for work, and only around a third of claimants recalled being referred to support following meetings with their work coach. Claimants in the case studies did, however, almost exclusively report positively about their experiences working with a work coach, who they described as friendly, encouraging and compassionate and noted having less anxiety around being made to immediately find paid employment, after they have had a HWC.
A possible explanation for this difference found (i.e. positive changes in confidence and motivation to move closer to work for claimants in the PSP survey when compared with claimants in the HWC survey) is that the PSP claimants are likely to have had multiple meetings with their work coach at the time of the survey interviews (they could have begun seeing their work coach since April 2017 and the survey was completed in September 2018). In comparison, claimants in the HWC survey were responding to the question having attended a limited number of meetings. ESA claimants were likely to have attended only a single meeting with their work coach at the time of the survey; and UC claimants were likely to have had around two meetings at the time of the survey.
7. JCP staff and claimants’ suggested improvements
This chapter describes JCP staff and claimants’ suggested improvements to the PSP and the HWC that emerged from the qualitative data.
7.1 Reflections on the PSP
Claimants and JCP staff who participated in the PSP case studies were asked how the PSP and the support on offer could be improved.
Increased tailoring of provision
Among claimants in the PSP case studies, who perceived themselves to be close to the labour market, there was a suggestion that the support offered was not tailored to their needs. An example of this is claimants being offered CV development support when they already had a recent CV available for job applications.
Changes to support formats
A group of J2E claimants recommended more one-to-one support, perhaps in combination with group support, as one-to-one support can provide hands-on help with job search. There were also claimants, who identified that one-to-one support was preferable to group support for people suffering from panic attacks or anxiety.
Some J2E participants who felt ready to look for work and who had accessed group support reported that being in a group with claimants who were further away from the labour market lowered their confidence. These claimants suggested that grouping cohorts by proximity to labour market might allow groups to be more or less work focused, depending on need.
The suggested improvements to PSP from JCP staff centred upon raising the profile of PSP initiatives or, improving the working relationships among JCP staff:
Improved publicity of the PSP
JCP staff suggested that greater promotion and marketing of positive claimant experiences and outcomes should be shared among work coaches. Work coaches reported that claimants might feel more encouraged to take up the offer of support if they were able to see how it had made a tangible difference to others.
Staff also suggested that improved publicity targeted at work coaches around the PSP claimant provision would improve staff awareness of the initiatives. To this end, staff called for more extensive promotion of provision using the District Provision Tool.
Improved presence of providers in Jobcentre Plus
Work coaches felt that having providers present in the JCP might increase awareness of initiatives available. Work coaches across all types of case study areas also felt that it would facilitate appropriate, timely and person-centred handover to the provider. This had proved to be a key facilitator in areas where take-up of J2E provision had been high.
Improved communication among JCP staff
DEAs also suggested that there could be better communication and collaboration with Community Partners. DEAs perceived that Community Partners were not always visible in all Jobcentre Plus offices, making it difficult for work coaches and DEAs to build relationships with them. According to DEAs, work coaches would have benefited from Community Partners spending time with them to help understand the referral processes and eligibility criteria of specific programmes to which the Community Partners have links.
Further training on the wide range of health conditions or disabilities with which claimants present
Views were mixed as to whether this was necessary. Community Partners and Work Coach Team Leaders in the PSP case studies felt that work coaches had been upskilled to support claimants with a range of different needs. Work coaches themselves reported that they would welcome further training and advice that touched on supporting claimants with different health conditions or disabilities.
7.2 Reflections on the Health and Work Conversation
ESA work coaches highlighted that the HWC is more suitable for some groups than others. As a response, they suggested a process of ‘screening out’ claimants who do not benefit from a HWC, such as those with substance misuse problems, those with severe illness or disability, or those with a job to return to. Work coaches had the option to ‘screen out’ claimants who they felt the support was not suitable for, including those with severe health conditions. The following suggested improvements to the HWC were given by staff:
Timing of the HWC
A group of ESA and UC staff felt that the use of the HWC techniques was best placed after the WCA. Having it prior to the WCA meant that claimants were focusing on demonstrating the extent of their health condition or the practicalities of their benefit claim, making it difficult for work coaches to make realistic plans and help build resilience and motivation to prepare for work. In contrast, as the first point of face-to-face contact with JCP, the HWC was reported by some claimants to allay worries related to having to immediately look for work.
Earlier introduction of the “About Me” technique
Staff felt that claimants could benefit from being sent the “About Me” form prior to their appointment, to have more time to consider their responses. It was also suggested that those who had complex needs or learning difficulties would benefit from a longer meeting with their work coach, to support them in completing the form.
Increase the length of appointment and introduce mandatory follow-ups
ESA staff reported that the HWC was not long enough to build rapport with claimants and introduce each technique. Staff reported that claimants would benefit from a longer meeting and mandatory follow-up meetings with the same work coach. This would enable staff to build-up rapport over time and introduce techniques when the claimants perceived they were ready. There was a view that the longer HWC meeting should take place after the WCA, so that those in the support group could have a different conversation to those in the Work Related Activity Group.
Location of the HWC
As outlined above, there were examples of claimants who found it difficult to engage in their HWC in an open plan office. UC and ESA work coaches identified that there should be some flexibility around the location of the HWC. A phone-call or a private room[footnote 6] should be offered in some circumstances, i.e. when the claimant is unable to travel to the JCP or they find the open plan office exacerbates their health condition or disability.
8. Conclusions
This chapter summarises the main findings from each strand of the evaluation.
8.1 Personal Support Package
8.1.1 Information, training and roll out for PSP
Established staff were more likely to be aware of the aims of the PSP, but awareness of the PSP initiatives varied widely across both new and established staff members. Early confusion about eligibility, and the gap between receiving information and training and PSP inception were both seen by JCP staff as contributing to this mixed picture. The nature of the PSP as a menu of options, whilst optimising the potential to tailor support and interventions to claimants, might introduce additional challenges in disseminating information and training staff. Focusing on ensuring that all staff understand the PSP goals and the initiative ‘menu’ is an important first step towards securing impact for the programme.
8.1.2 Claimant experience of support
PSP covers a wide range of both existing and new initiatives including work coach support. The PSP survey explored claimants’ recall of all advice and support which they may have been offered by their work coach since the introduction of the PSP (April 2017), plus specific questions about four selected elements of PSP (Journey to Employment (J2E), Work and Health Programme (WHP), Specialist Employability Support (SES) and Work Choice (WC)).
65% of claimants in the PSP survey recalled being offered some form of support to move closer to the labour market and into work as part of their interaction with JCP; and 14% recalled being offered a place on one of the four selected PSP strands highlighted in the survey (J2E, WHP, SES and WC).
Overall, claimants in the PSP survey were positive about the advice and support they had received from their work coach. Three quarters of claimants in the PSP survey who took up some form of support (this includes general provision as well as PSP initiatives), found the support either ‘very’ or ‘fairly’ helpful. This high level of satisfaction in the support and advice received indicates that the menu of support (including support from work coaches, existing provision and new PSP initiatives) offered as part of the PSP has the potential to be a good platform for providing support to this claimant group. The support offered was perceived as helpful by a majority of claimants (75%) in the PSP survey.
8.1.3 Targeting and tailoring support
Running throughout both the quantitative claimant surveys and the qualitative case study findings, there is a clear thread about the role played by type and severity of health condition or disability, and wider factors influencing distance from the labour market (such as age and education) in determining which claimants are likely to benefit most from support and advice offered by their work coach.
Poor health or disability and lack of confidence were the two main reasons claimants stated as their rationale for not taking up any support. These barriers were most prevalent among those with severe health conditions or disabilities. This suggests that to move this group of claimants closer to work, the support may need to be tailored to first addressing these barriers. The findings also suggest that this group may need support to be longer-term. Programmes such as the WHP, were perceived as beneficial for this claimant group due to the length of support it offers.
The findings similarly indicate that tailoring of support must consider the type of health condition claimants present with. Mental health conditions, specifically anxiety or depression, differentiates what claimants need. Peer support appears to be less successful for those with social anxiety. One-to-one support may be more beneficial for this claimant group at the beginning of their journey back to work, with peer support considered later.
Tailoring of support is also important for those who feel close to moving into work. For those claimants that are closer to the labour market, supportive providers offering bespoke support, such as job-brokering or peer support, are perceived by claimants to be the most helpful. However, it is important to make sure that if approaches like peer support are used, then groups could be segmented to ensure that people with similar needs are in each group.
8.1.4 Outcomes
Perceived outcomes from engaging in support were mixed, with under half of claimants in the PSP survey reporting that participation in support had increased their confidence, or motivation to move closer to work. For those who did engage in support but reported no change in their confidence or motivation to move closer to work, the main reason for this reported was a deterioration in their health.
Similarly, work-related outcomes as a result of engaging in support were mixed, with 44% of claimants in the PSP survey reporting to be in some work-related activity, such as volunteering, training or education or employment as a result of the support they received. These findings must be read with caution as there was no counterfactual in the evaluation, so we do not know what the outcomes for these claimants might have been if they had not engaged in the PSP.
8.2 The Health and Work Conversation
8.2.1 Staff training in HWC techniques
Feedback on the training provided to support the HWC was positive overall, but there is evidence that the training was not as effectively targeted as it might have been. For more experienced staff, the shorter training sessions were seen as more appropriate given the potential to build on existing skills and experience. While for less experienced staff, longer training courses with the opportunity to practice techniques would have been appreciated. It is also clear that for some staff the time lag between training and the delivery of the HWC was too long to optimise the value of the learning.
8.2.2 Recall and use of HWC techniques
A significant minority of claimants (41%) did not recall taking part in any of the HWC techniques. While this will undoubtedly be driven by the challenge of recognising and recalling the specific initiatives in some instances, it is worth reflecting that the claimants least likely to recall the techniques were those who were furthest from the labour market, and it is with these claimants that staff reported tailoring or choosing not to use HWC techniques, in line with DWP policy. It is also clear that building rapport and having adequate time and an appropriate setting to use the HWC techniques were central to staff delivering the HWC as it was designed.
Further challenges to the structure and process of the HWC were highlighted. For some ESA claimants, the placement of the HWC prior to the WCA was perceived as particularly problematic because of the limited number of on-going appointments within which rapport could be built. For UC claimants, there was also confusion between the voluntary HWC actions and goals and the mandatory claimant commitment actions and goals.
8.2.3 Outcomes from the HWC
The qualitative HWC case studies also highlighted that the HWC worked less well for particular claimant groups. HWC techniques were felt to be less useful in supporting those who were furthest from the labour market. It was also felt that the use of HWC techniques was not suitable for those closest to the labour market, with a job to return to. Similarly, it was perceived as less useful for older people close to retirement or, those who had complex needs, such as drug and alcohol dependency.
Overall claimants in the HWC survey felt comfortable with the HWC, with UC claimants highlighting that their on-going relationship with their work coach provided a strong framework for building relationships. That almost half of claimants who had not had a follow-up after their HWC wanted one, suggests that this element of the HWC is viewed as a useful form of support.
Annex A: List of PSP initiatives
The Personal Support Package (PSP) is a suite of programmes and initiatives introduced in 2017 to support people who are not in work due to a health condition or disability move closer to employment. These included:
A. New Initiatives
Small Employer Offer (SEO)
Small Employer Advisers worked with local small employers to identify opportunities and match people to jobs. The SEO provided an opportunity for Jobcentre Plus to actively engage with small local employers, establish relationships and raise awareness of the support that is available to them if they were to consider employing a person with a health condition or disability.
Journey to Employment (J2E)
Disabled Peoples’ User Led Organisations and local Voluntary Sector Organisations delivered personalised peer support job clubs to disabled people and people with long term health conditions. The job clubs were overseen by a Community Employment Specialist who has a lived experience of disability or an in-depth knowledge of the issues these claimants face in finding and staying in employment.
Mental Health Training for work coaches
Increasingly high volumes of claimants flowing into either the ESA Work Related Activity Group or Universal Credit Limited Capability for Work groups have mental health conditions and it is important to ensure work coaches are confident and capable to support this group. Work coaches were provided with additional Mental Health Training to enable them to better support claimants with mental health conditions.
Community Partner (CP)
A specialist role employed by Jobcentre Plus for their expertise and local knowledge of disability issues. They worked with work coaches, local third sector organisations and employers to build relationships and strengthen their understanding of the needs of disabled people and those with health conditions to ensure tailored claimant support. The role ceased on 31st March 2019.
B. Extra places on existing provision
Work Choice
A specialist disability employment programme delivered by a range of provider organisations, that offered work entry support and up to two years in-work support for people with disabilities. Referrals to Work Choice ceased in 2017 but some claimants had already been offered places on the programme as part of PSP
Work and Health Programme (WHP)
A programme mostly delivered by external providers, providing personal support to improve the claimant’s skills, manage their health condition and match claimants to jobs. Launched in 2017, the programme complements the Jobcentre Plus work coach delivery model to employment support, providing enhanced specialist support for those who need it particularly those claimants who volunteer and are prepared and motivated for the intensive support the new programme offers.
Specialist Employability Support (SES)
A programme delivered by a range of provider organisations, to support people with a disability or health condition and complex support needs. Additional places on the Specialist Employability Support programme were provided as part of the PSP.
Access to Work Mental Health Support Service (MHSS)
Provided increased funding for this programme which offers support for those with mental ill health moving into work or needing help to retain their current employment.
C. Proofs of Concept (small scale tests in selected areas)
Jobcentre Plus led Specialist Employability Support
Testing an in-house Jobcentre Plus led alternative to Specialist Employability Support (SES) model of provider-led support.
Specialist Advice
Testing the use of voluntary specialist advice from Health Care Professionals. Advice is offered via a three-way conversation between the specialist, work coach and claimant covering general health management and appropriate work related activities to transition an individual towards work.
Local Supported Employment
Working with local authorities to deliver locally supported employment on an outcome payment basis focussing on those with learning difficulties, autism or severe mental health conditions who are known to local authority adult social care.
Young Persons Supported Work Experience
A programme aimed at young people with long term conditions who are further away from the labour market and have little or no work experience to enable them to gain valuable supported workplace experience, help them get the most from the opportunity and support their future job search.
D. Other
Health and Work Conversation (HWC)
A mandatory work-focused interview for ESA claimants which is scheduled at the beginning of their claim and held prior to their Work Capability Assessment. For UC claimants, HWC techniques can be spread out across several appointments and work coaches can use their discretion to use the most appropriate elements.
Extra DEAs to support work coaches and other staff.
Annex B: HWC survey: Impact of health on attitudes to work
Table 1: Main area health condition/disability affected Universal Credit claimants
| Health condition | Percentage |
|---|---|
| Mobility, Dexterity or Stamina | 31 |
| Mental health, memory, social or learning | 44 |
| Other | 12 |
| Areas affected are equally important | 13 |
Base: All UC respondents
Weighted base: 483
Unweighted base: 483
Table 2: Main area health condition/disability affected ESA claimants
| Health condition | Percentage |
|---|---|
| Mobility, Dexterity or Stamina | 34 |
| Mental health, memory, social or learning | 41 |
| Other | 9 |
| Areas affected are equally important | 15 |
Base: All ESA respondents
Weighted base: 496
Unweighted base: 497
Table 3: Number of barriers UC claimants reported to returning to work
| Number | Percentage |
|---|---|
| None | 1 |
| One barrier | 46 |
| More than one | 53 |
Base: All UC respondents out of work
Weighted base: 341
Unweighted base: 351
Table 4: Number of barriers ESA claimants reported to returning to work
| Number | Percentage |
|---|---|
| None | * |
| One barrier | 51 |
| More than one | 49 |
Base: All ESA respondents out of work
Weighted base: 434
Unweighted base: 434
Where values rounded to zero these are represented by an ‘*’.
Table 5: Whether UC claimants affected by more than one health condition
| Number | Percentage |
|---|---|
| None | 3 |
| One barrier | 21 |
| More than one | 76 |
Base: All UC respondents
Weighted base: 499
Unweighted base: 499
Table 6: Whether ESA claimants affected by more than one health condition
| Number | Percentage |
|---|---|
| None | 1 |
| One barrier | 12 |
| More than one | 86 |
Base: All ESA respondents
Weighted base: 506
Unweighted base: 506
Table 7: Barriers to finding work reported by Universal Credit claimants
| Barrier | Percentage |
|---|---|
| Physical health condition/disability | 60 |
| Mental health condition/disability | 47 |
| Family caring commitments | 15 |
| Lack jobs suitable for someone with their health condition | 11 |
| Lack of skills/experience | 8 |
| Lack of confidence applying for jobs | 8 |
| Lack of vacancies/competition | 7 |
| Public transport not suitable due to health condition | 6 |
| Lack of jobs for people with caring commitments | 5 |
| Time/cost of travelling to interviews/workplace | 4 |
| Not knowing how to find suitable jobs | 3 |
| Criminal record | 3 |
| Available jobs won’t pay enough to live on | 2 |
| Housing problems | 2 |
| Age barriers | 2 |
| Drug or alcohol problems | 2 |
| Not interested in working | 1 |
| An immediate crisis | * |
| Other | 9 |
| None of the suggested barriers | 1 |
Base: All UC claimants not in work
Weighted base: 342
Unweighted base: 352
Note: respondents could select more than one answer when responding to this question.
Where values rounded to zero these are represented by an ‘*’.
Table 8: Barriers to finding work reported by Employment and Support Allowance claimants
| Barrier | Percentage |
|---|---|
| Physical health condition/disability | 65 |
| Mental health condition/disability | 56 |
| Lack jobs suitable for someone with their health condition | 9 |
| Lack of confidence applying for jobs | 8 |
| Public transport not suitable due to health condition | 6 |
| Lack of skills/experience | 6 |
| Family caring commitments | 6 |
| Lack of vacancies/competition | 4 |
| Lack of jobs for people with caring commitments | 3 |
| Not knowing how to find suitable jobs | 3 |
| Drug or alcohol problems | 2 |
| Time/cost of travelling to interviews/workplace | 2 |
| Housing problems | 2 |
| Available jobs won’t pay enough to live on | 2 |
| Criminal record | 2 |
| An immediate crisis | 1 |
| Age barriers | 1 |
| Not interested in working | * |
| Other | 7 |
| None of the suggested barriers | * |
Base: All ESA claimants not in work
Weighted base: 434
Unweighted base: 434
Note: respondents could select more than one answer when responding to this question.
Where values rounded to zero these are represented by an ‘*’.
Table 9: How health conditions/illnesses affected UC claimants
| Health condition | Percentage |
|---|---|
| Mental health | 65 |
| Stamina or breathing or tiredness | 54 |
| Learning or understanding | 46 |
| Mobility | 45 |
| Memory | 37 |
| Dexterity | 23 |
| Socially or behaviourally | 21 |
| Hearing | 14 |
| Vision | 13 |
| Other | 13 |
| None of these | 3 |
Base: All UC respondents
Weighted base: 500
Unweighted base: 500
Note: respondents could select more than one answer when responding to this question.
Table 10: How health conditions/illnesses affected ESA claimants
| Health Condition | Percentage |
|---|---|
| Mental health | 66 |
| Stamina or breathing or tiredness | 66 |
| Mobility | 57 |
| Learning or understanding | 53 |
| Memory | 46 |
| Dexterity | 28 |
| Socially or behaviourally | 20 |
| Vision | 15 |
| Hearing | 11 |
| Other | 15 |
| None of these | 1 |
Base: All ESA respondents
Weighted base: 506
Unweighted base: 506
Note: respondents could select more than one answer when responding to this question.
Table 11: How much health condition/disability limits everyday activities among UC claimants
| Level of problems | Percentage |
|---|---|
| No problems carrying out everyday activities | 14 |
| Slight problems | 18 |
| Moderate problems | 30 |
| Severe problems | 21 |
| Unable to carry out everyday activities | 8 |
| Differs too much to say | 8 |
Base: All UC claimants
Weighted base: 498
Unweighted base: 496
Table 12: How much health condition/disability limits everyday activities among ESA claimants
| Level of problems | Percentage |
|---|---|
| No problems carrying out everyday activities | 7 |
| Slight problems | 15 |
| Moderate problems | 33 |
| Severe problems | 28 |
| Unable to carry out everyday activities | 12 |
| Differs too much to say | 5 |
Base: All ESA claimants
Weighted base: 503
Unweighted base: 503
Table 13: Extent to which UC claimants would like to work in the future
| Extent | Percentage |
|---|---|
| Not at all | 9 |
| A little | 12 |
| To some extent | 21 |
| To a great extent | 58 |
Base: All UC claimants not currently working
Weighted base: 326
Unweighted base: 334
Table 14: Extent to which ESA claimants would like to work in the future
| Extent | Percentage |
|---|---|
| Not at all | 8 |
| A little | 13 |
| To some extent | 16 |
| To a great extent | 63 |
Base: All ESA claimants not currently working
Weighted base: 406
Unweighted base: 407
Table 15: When UC claimants think they will return to work
| Timeframe | Percentage |
|---|---|
| Within the next six months | 37 |
| Within the next year | 18 |
| Within the next two years | 14 |
| Later than two years | 10 |
| Never | 21 |
Base: All UC claimants not currently working
Weighted base: 266
Unweighted base: 270
Table 16: When ESA claimants think they will return to work
| Timeframe | Percentage |
|---|---|
| Within the next six months | 36 |
| Within the next year | 27 |
| Within the next two years | 14 |
| Later than two years | 9 |
| Never | 14 |
Base: All ESA claimants not currently working
Weighted base: 306
Unweighted base: 307
Table 17: Feelings about paid work among UC claimants
| Feeling | Percentage |
|---|---|
| My health condition/disability rules out work as an option now and in the future | 23 |
| I am currently unable to work, but might be able to in the future if my health condition/disability improves | 48 |
| I could return to work now if that right job was available or if I had the right support | 28 |
Base: All UC claimants not currently working
Weighted base: 334
Unweighted base: 346
Table 18: Feelings about paid work among ESA claimants
| Feeling | Percentage |
|---|---|
| My health condition/disability rules out work as an option now and in the future | 17 |
| I am currently unable to work, but might be able to in the future if my health condition/disability improves | 72 |
| I could return to work now if that right job was available or if I had the right support | 11 |
Base: All ESA claimants not currently working
Weighted base: 426
Unweighted base: 426
-
The HWC can be conducted in a private room upon request, if a room is available. ↩
-
Case-conferences are meetings held within the JCP where work coaches are invited to discuss complex customer cases and needs with colleagues in similar positions. ↩
-
A benefit sanction is a temporary stop or reduction of a claimants benefit for a period of time if they do not meet conditions that are attached to their benefit claim. ↩
-
Note that this was not the objective of the HWC training provided to Jobcentre Plus staff. ↩
-
These differences are marginally significant. ↩
-
The HWC can be conducted in a private room, if a room is available. For UC claimants, a phone call can also be offered, if requested. ↩
