DfT and FCDO: International importation, border and travel measures, 21 January 2021
Updated 13 May 2022
Executive summary
Countries can expect travellers infected with SARS-CoV-2 to arrive through air, land and sea borders. There is an increasing number of options available for consideration to prevent the importation of infection, given the emergence of a number of variations of concern. This paper considers the evidence behind different approaches, and highlights remaining unknowns and determinants of effectiveness.
Infected travellers have the potential to be detected at different points: through screening or testing before departure, through testing on arrival, testing during or after quarantine, or through becoming symptomatic at any point prior to travel up to the end of any period of quarantine.
Building upon the previous SAGE paper (S0943 3a at SAGE 71), that considered “Quarantine and testing strategies to prevent onwards infection from travellers returning to the UK”, this paper provides a summary of evidence related to the following questions.
-
How does the effectiveness of different measures (such as pre-departure testing, follow-up isolation, and so forth) vary by the effectiveness of each component of the intervention (for example, percentage of travellers who are tested (do not have exemptions, arrive through another source); sensitivity of test used; level of compliance with quarantine and isolation upon arrival, amongst other factors)? What is the combined (whole system) effect of a combination measures and how do they interact?
-
What does empirical evidence suggest about the effectiveness and sustainability of travel bans, as a means to reduce the risk of importation of cases?
Key assessments
1. The UK has a high level of international connectivity, driven by extensive international connections, a population with a high propensity to fly, the UK being a popular destination for business and tourism, as well as via its connectivity as a hub for international travellers connecting or transiting onward. This increases the likelihood that, at the time a new variant of concern is detected anywhere in the world, there will already be cases in the UK (weak evidence, moderate confidence). This risk will be higher when the variant occurs in countries with high volumes of direct international travel.
2. No single intervention, other than a complete, pre-emptive closure of borders, or the mandatory quarantine of all visitors upon arrival in designated facilities, irrespective of testing history, can fully prevent the importation of cases or new variants (moderate confidence, moderate evidence).
3. Evidence from the continued spread of the South African and UK variants suggests that reactive, geographically targeted travel bans cannot be relied upon to stop importation of new variants once identified, due to the time lag between the emergence and identification of variants of concern, and the potential for indirect travel via a third country (moderate confidence, moderate evidence). Travel bans will have the most impact if action is taken quickly, there are low volumes of direct or indirect travel, and if the variants have not already spread widely (weak evidence, moderate confidence).
- 4. Travel bans applied pre-emptively (for example, longer lasting or blanket travel bans, before specific issues of concern are identified) can have substantial social and economic implications for both the UK and other countries. These are appropriate in limited circumstances, 2 examples:
- a. when domestic incidence is very low but rates are growing (R greater than 1) and lockdown restrictions have been eased. This is because importations could increase prevalence towards the tipping point, after which the virus spread exponentially.
- b. There is a significant variant of concern, which could seriously undermine the effectiveness of existing control measures (Low-moderate confidence).
WHO analysis suggests that partial travel bans only have the potential to delay spread and peak by a few weeks or months. Extensive travel restrictions (over 90% of journeys stopped) would be required to meaningfully affect the magnitude of an epidemic [footnote 1].
5. The effectiveness of pre-departure screening, based upon symptoms, is dependent upon the extent to which symptomatic people seek to travel.
6. Estimates of the effectiveness of pre-departure testing, are dependent upon the extent to which symptomatic people seek to travel; how close testing is conducted, prior to travel, as well as the sensitivity of the test used. (weak evidence, moderate confidence). Irrespective of the test used, modelling from PHE and LSHTM suggests that pre-departure testing can make a limited contribution to reducing the proportion of people travelling whilst infectious. A residual proportion of infections would still arrive in the UK.
7. The timing and type of pre-departure test is an important consideration. Using the sensitivity estimates from the Liverpool Mass Testing, pre-departure LFD testing on the day of travel is estimated to detect an additional 11% (10%, 11%) of infectious travellers, if 70% of symptomatic individuals refrain from travelling (Quilty). The more that symptomatic individuals attempt to travel, the more effective this additional measure becomes. Effectiveness is highly dependent on timing, with the maximum benefit from performing the test as close as possible to the time of travel. Whether undertaken with a PCR or LFD class of device, this provides the most power to detect and deflect travel by an infectious person (PHE).
8. Test on arrival, with quarantine for those testing positive, could lower the volume of infectious travellers entering the UK. Effectiveness will be reliant on the sensitivity of the test used, adherence to isolation for those who test positive (weak evidence, moderate confidence). PCR testing on arrival could also give a potential opportunity to sequence positive tests from infectious arrivals on entry, with the findings being used to identify the importation of new, high-risk variants. Whilst this raises the theoretical potential for focussed interventions directed towards individuals with these variants, the practicalities associated with this may be significant.
9. Post-entry repeated testing which involves multiple tests on travellers on arrival into the UK, with no quarantine, is likely to be insufficiently sensitive to detect a significant proportion of infectious individuals (Moderate confidence). Daily testing scenarios, where travellers are released into the community upon arrival, and subsequently tested every day with lateral flow tests, will lead to a significant proportion of infected individuals not being detected. For example, LSHTM modelling suggests that, using 10 daily LFA tests, following syndromic screening and pre-flight LFA test, a quarter (26% (18%, 28%)) of infected individuals would not be detected.
10. Post-entry quarantine, with a required negative PCR test to exit quarantine, has the most substantial potential effect on reducing the risk of infected arrivals. (Moderate evidence, Low-moderate confidence). Effectiveness is dependent on the duration of quarantine period, usage of test during or at exit of quarantine, and adherence and behaviours (Moderate confidence). Most models suggest reduction of quarantine period from 14 to 10 days produces limited increase in incursion risk. (moderate confidence, moderate evidence) and a duration of at least 5 days or longer with PCR test on exit may be considerably effective (low-to-moderate confidence, moderate evidence).
11. The length of the infectious period has a significant impact on how many infected travellers can be detected at any moment in time. There is no scientific or medical agreement on the length of the infectious period, however there is general consensus it is equal to, or less than 5 (low-to-moderate confidence, moderate evidence). The effectiveness of isolation periods and exit tests will vary based upon the length of infectious periods. Longer infection periods present a higher risk of releasing still infectious passengers at the end of isolation and therefore longer isolation periods and exist tests are more effective, than if infectious periods are shorter. Note that infectious period is distinct from the commonly reported PCR detectability period.
12. Combination of options. Modelling demonstrates a combination of specific policy options (Pre-departure testing, isolation and TTR), are effective at reducing the public health risk, although dependant on their specific details, even with relatively low public compliance.
-
All strategies are highly dependent on the rate of adherence to quarantine, self-isolation, and testing protocols. Analyses by SPI-B suggest that:
- i. Self-reported surveys of travellers suggest that the majority were compliant. Online polls suggest that many people would not comply with quarantine requirements. Social desirability bias means that reported intentions are likely to over-state levels of compliance.
- ii. Interventions that occur while the traveller is under direct observation of travel bodies have the highest likelihood of adherence. However, these control measures also incur significant time, costs, and effort which should be appropriately weighed against the added benefit of such a strategy.
- iii. Enforcing quarantine adherence (such as through the use of hotels or follow-up compliance adherence calls), is expected to reduce the number of infectious hours undetected travellers would be expected to be in the community by approximately 50%, compared to current at home isolation which is estimated to have approximately 67% compliance (ONS survey) (Moderate confidence, weak evidence). This study does not however provide insight into how individuals are breaking the rules and the inferred social risk associated with that.
- iv. Beyond this, there is an absence of evidence regarding the effectiveness of measures to enforce quarantine, other than the presumed high effectiveness of mandated methods. The relative balance between providing support for self-isolation and enforcement is also unknown.
- v. Any intervention imposed at the pre-departure stage is also subject to a wide variety of performance challenges, and there may be limited access for quality assurance and performance evaluation.
Next steps
a. Review or commission further research into the rate of public compliance. This should consider the levels of compliance with different policies and the form non-compliance
takes.
b. Review evidence and analysis on the tipping point, at which imported strains form a critical mass and reach exponential growth within the community. This needs to be considered at different levels of domestic restrictions.
c. Review evidence on the length of infectious period. PHE are conducting a review of current literature and will provide an update in February.
d. There is a clear need for global access to vaccines to facilitate a situation where travel restrictions and travel bans become the exception. Impacts of restrictions, isolation, testing and travel bans discussed in this paper provide an ongoing rationale for continuing UK international effort on global vaccine role out.
Full paper
1. Countries can expect travellers infected with SARS-CoV-2 to arrive through air, land and sea borders. Countries have therefore deployed a range of different approaches to minimise the risk of importing new infections into the community. This paper considers the science behind different approaches, including remaining unknowns.
2. Infected travellers may be detected at different points: before flying, testing on arrival, testing at the end of quarantine, daily testing at the end of quarantine, or through becoming symptomatic at any point prior to travel up to the end of any period of quarantine on arrival in UK.
- 3. This provides for a ‘menu’ of interventions that can be used alone or in combination to prevent infected travellers to the UK from seeding new chains of transmission. This list does not include interventions to mitigate risks to other travellers during travel such as environmental controls and public health and social measures at points of entry and on planes (such as minimising contacts, crowd control and physical distancing including through engineering modification, mask use, hand hygiene, ventilation, cleaning and disinfection, as well as other factors.):
- a. pre-departure syndromic screening
- b. pre-departure testing (0, 1, 2, or 3 days prior to departure)
- c. post-entry test-on-arrival without quarantine
- d. post-entry repeated testing with lateral flow tests without quarantine
- e. post-entry quarantine, with or without a negative test to exit quarantine
4. There is no ‘zero risk’ combination of approaches when considering the potential importation of cases in the context of international travel in the real world.
- 5. For strains already seeded domestically, the risk of infectious arrivals into the UK should be considered relative to domestic incidence. Restrictions on travel have a much higher relative impact in countries where the expected number of infectious arrivals exceeds domestic incidence.
- a. When the country of departure and the UK share similar levels of transmission, there is no substantial risk of adversely impacting domestic transmission (though this should take into account sub-national variations in both countries).
- b. When the country of departure is experiencing more intense transmission than the UK, the risk of potential impact on domestic transmission is higher.
- c. When the country of departure is experiencing less intense transmission than the UK, the risk of potential impact on domestic transmission is lower.
- d. Based on figures from December 2020, under no restrictions there would be an estimated 831 (412, 1618) infected entries per day compared to an estimated 58,623 (50755, 71800) new domestic infections per day (Quilty). Percentage reductions through the use of different interventions should be viewed in this context.
- 6. The emergence of new variants of concern has given rise to a rationale for attempting to reduce importation of even small numbers of infectious cases. This rationale will strengthen if new variants emerge capable of immune escape.
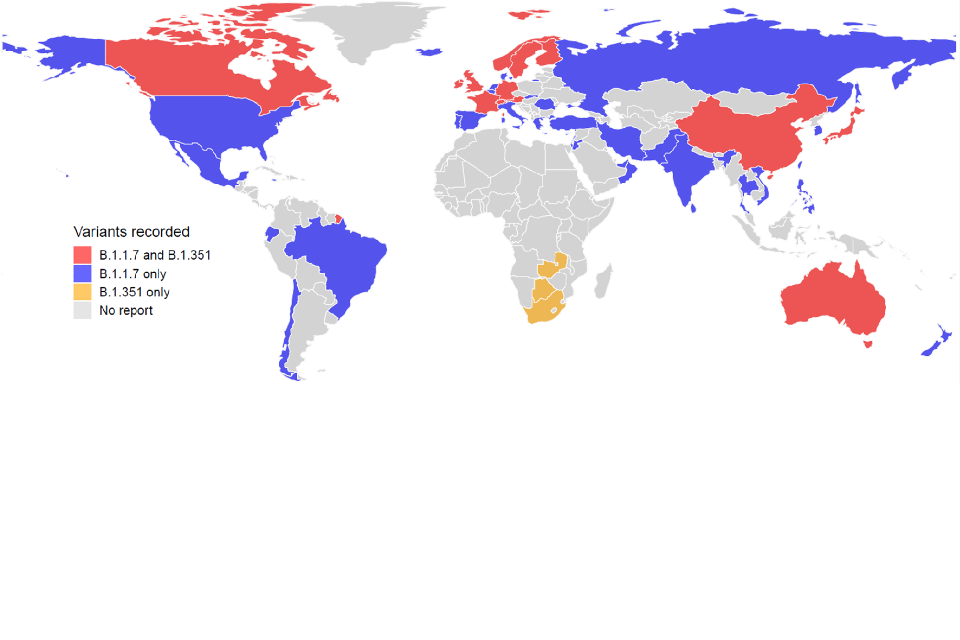
- a. Since the new variants of concern from lineage B.1.1.7 and B.1.351 were first detected by the UK and South Africa respectively, they have spread rapidly and have now been detected in a large number of countries. To date, the variant of concern from lineage P.1 has only been detected in Brazil and Japan (during airport screening of travellers from Brazil).
- b. Due to limited genomic sequencing capacity globally, these variants are likely circulating undetected in many more countries. This means that targeted travel measures that apply only to countries that have detected specific variants of concern (and their neighbours) are unlikely to be completely successful in stopping new introductions of these variants into the UK.
Figure 1: Reports of new SARS-CoV-2 variants, lineage B.1.1.7 and B.1.351 in different countries as of 14 January 2021 (does not show the variant from lineage P.1) (Lai).
7. By the time a case of a new variant is detected for the second time through sequencing approaches, there will already be a significant number of infections in the community. Not everyone infected with SARS-CoV-2 is tested, not all positive tests are sequenced, and delays occur at each stage.
a. Assuming a local R of 1.5 for the B.1.351 variant first detected in South Africa, the first imported infection was estimated to have occurred between 7.6 and 10 days before the second case was reported in the UK (which was before the variant was reported by South Africa). (Pearson)
b. At the time the second case of this variant was reported in the UK, there were already an estimated 78 (17, 230) people infected with this variant in the UK. (Pearson)
c. The UK has a high level of international connectivity. This makes it more likely that at the time a new variant of concern is detected anywhere in the world, there will already be cases in the UK. This risk of this will be higher for countries with high volumes of direct international travel.
d. Timely, high-volume testing and genomic sequencing are critical to detect cases and clusters of new variants. The UK has significantly increased both of these capabilities since the beginning of the pandemic. However, all interventions outlined are highly dependent on the capacity to deliver these basic functions to maximise effectiveness.
8. The length of the infectious period has a significant impact on how many infected travellers can be detected at any moment in time. There is no scientific or medical agreement on the length of the infectious period, however PHE currently use a mean duration of 0 to 5 days, whilst DfT use a mean of 2 to 5 days (low to moderate confidence, moderate evidence).
a. Longer infection periods present a higher risk of releasing still infectious passengers at the end of isolation periods. Therefore, longer isolation and exit tests are the most effective under this assumption.
b. The shorter infectious period (2 days), results in testing 48 hours prior to release having little additional benefit (approximately 1% to isolation without a test.
c. However, if the infectious period is longer (5 days), the additional benefit of testing 48 hours prior to release is significant.
i. Approximately 10% for the 10-day isolation (day 8 test).
ii. Approximately 20% for the 7-day isolation (day 5 test).
d. Increasing the isolation duration decreases the percentage of infected travellers that are undetected and released.
e. The relative effectiveness of different isolation periods also changes depending on the duration of the infectious period. DfT modelling, found 7-day isolation (day 5 test - TTR) was equally as effective as 10-day isolation, when using an infection period of 5 days. However, as the infection period is reduced, the 10-day isolation becomes relatively more effective.
f. PHE modelling, using an infection period of less than 2 days, found the 7-day isolation (day-5 test – TTR) results in an additional approximately 6%of infectious travellers being undetected and released, compared with 10-day isolation.
g. These ranges assume 99.7 to 100% sensitivity of a test and 100% compliance with isolation, switching these to ‘real world’ assumption will impact upon the results.
9. All strategies are highly dependent on the rate of adherence to quarantine, selfisolation, and testing protocols. Adherence is not binary, and different approaches to non-adherence will vary in terms of risk. For example, leaving quarantine to see friends and family indoors is a much higher risk than leaving quarantine to go for a walk outdoors alone. Additionally, even with quarantine there remains a residual risk of onward transmission associated with travel from their point of entry to their place of quarantine and also with the household members who may share the designated quarantine location. The attached paper by SPI-B considers drivers of adherence and how this may be improved. Relevant evidence includes:
a. A previous ONS international arrivals compliance survey indicated that 67% of arrivals were compliant with the previous 14-day (now 10-day) self-isolation policy, with 12% saying that they were not compliant and remaining proportion unsure or unlikely to be. [footnote 2]
b. An Ipsos Mori online poll found that only 55% would be ‘certain’ to comply with quarantine requirements. Estimated non-compliance ranges between 10% (stated would be unlikely to comply) and 36% (stated would be unlikely to comply, or only ‘likely’ to comply. [footnote 3] Social desirability bias means that respondents are likely to underreport behaviours that go against the rules or social norms and therefore these estimates of non-compliance could be underreported (and compliance estimates overstated).
c. Without enforcement, some objective measures of mobility showed small increases over time during lockdown in the UK and elsewhere, self-reports of staying at home decreased, and self-reports of complete compliance with government guidelines also decreased. Methods of enforcement include fines for violation – with and without electronic monitoring, denying entry to public spaces without electronically validated proof of being virus-free, and mandating self-isolation and quarantining in supervised facilities. The acceptability of these different methods varies across countries – with harsher measures more likely to be applied in authoritarian regimes, and harsher measures more acceptable as a condition upon entry or re-entry to a country than for those living in the country. There is an absence of evidence regarding the effectiveness of any of these methods of other than presumed high effectiveness of mandated methods described above. The relative balance between providing support for self-isolation and enforcement is also unknown [footnote 4].
d. Mandated interventions that occur while the traveller is under direct observation of travel bodies might be expected to have the highest adherence. However, these control measures also incur significant time, costs, and effort which should be appropriately weighed against the added benefit of such a strategy.
e. Hotel quarantine has been used by some countries; one well known example is New Zealand. Evaluation of these case studies is limited, and studies that do mention it have not isolated it from the range of other measures in place. We would expect that compliance levels when mandatory hotel quarantine is imposed would go up significantly, and likely deter travelling in the first place.
f. Evidence from the supported isolation procedures put in place for those returning from Wuhan suggests that compliance is likely to be increased by explaining the importance of isolating, ensuring those isolating have access to the supplies they need, and communicating throughout the isolation period. Increased support (practical, informational, emotional) for those isolating is likely to result in increased compliance. A small risk of onward transmission to the local community could exist via staff in those hotels, for example, but measures (such as PPE) could minimise these. There is low evidence in this area.
g. Any intervention imposed at the pre-departure stage is also subject to a wide variety of performance challenges and consistency, moreover there may be limited access for quality assurance and performance evaluation.
10. A number of broad assumptions made across many or all available models. This is generally necessary given the existing state of knowledge, but modelled estimates need to be understood in this context and may therefore differ from real-world performance. These include:
a. Individuals are not infected during travel. Models using reported incidence to estimate the volume of potential imported infections only include those who have been infected before the point of travel. This underestimate both the number of possible imported infections and the subsequent timeline for infectiousness and detection.
b. A significant proportion of symptomatic individuals will not travel. Most models assumed between 70% to 100% of infected people already showing symptoms would either choose not to travel or be prevented from flying by pre-departure syndromic screening. SPI-B are looking at the question of what proportion of people are likely to try to travel despite knowing they are infected, but, particularly at the higher end of this range, this may be an overestimate. Accordingly, the true volume of imported infections under each intervention scenario is likely to be higher.
c. There are people who are infectious but not yet symptomatic and people who are infectious and asymptomatic who will travel. Some people who are infectious will travel that are not captured by some modelling and estimates.
d. Global parameters of distribution in SARS-CoV-2 infection are generalisable. Known heterogeneity in certain parameters will likely affect the modelled estimates of risk. For example, higher proportions of asymptomatic cases in countries from certain regions will decrease the overall effectiveness of many interventions.
11. This paper does not fully consider wider implementation issues relevant to each intervention. These include factors such as the availability of testing supplies; the operationalisation of COVID-safe environments for high-volume testing within airports in the UK and at points of departure; the ability to effectively enforce quarantine and or self-isolation of travellers, whether in homes or hotels and facilities; and the full range of legal, political, and practical considerations relating to travel bans.
Interventions
12. Pre-departure syndromic screening may detect a proportion of symptomatic individuals who have chosen to still travel to the airport. However, evidence remains limited on effective screening protocols that can be delivered in practice, and the sensitivity of these protocols in detecting cases.
a. WHO’s assessment is that the evidence supports visual screening for symptoms such as cough and difficulty breathing as an effective measure for COVID-19, but not exit or entry screening via temperature measurement. This is because people may not exhibit fever early in the course of the disease, or may reduce fever through the use of paracetamol and other anti-pyretic medications. However, visual screening for symptoms will also miss people travelling during the incubation period (between exposure and symptom onset), those who are only mildly symptomatic and not detectable through visual screening, or those who are genuinely asymptomatic.
b. There are likely to be behavioural impacts of implementing syndromic screening. These include positive impacts such as creating a deterrence for symptomatic individuals thinking about travelling, as well as negative impacts such as engendering a false sense of security in those who test negative – resulting in lower adherence to more effective public health measures following the test result. These questions are being considered by SPI-B in parallel.
13. Pre-departure testing can make a limited contribution to reducing the proportion of people travelling whilst infectious. However, the residual proportion of infections that would still arrive in the UK are so significant that it cannot remove the need for further measures.
a. Negative results from pre-departure testing cannot guarantee that travellers are free from infection at the time of travel since they may have been tested before they became infected or during the period when the viral load is not yet sufficient to be detectable, in addition to false negatives. New variants may also emerge that evade current commercially available PCR and LFD tests until these are re-tooled.
b. Effectiveness is highly dependent on timing, with the maximum benefit from performing the test as close as possible to the time of travel. Whether undertaken with a PCR or LFD class of device, this provides the most power to detect and deflect travel by an infectious person. (PHE)
i. The maximum fraction of people detectable if tested at time of travel is approximately 40% (if assuming a 7-day infection window) or 60% (if assuming 14- day infection window).
ii. The detectable fraction decreases by approximately 8 to 10% for every additional 24-hour period the test is done before departure.
iii. Using some estimates, the difference in sensitivity of PCR and LFDs are similar at 90% and 80% respectively and both have similar specificity, such that there may be no material difference in detection rates of infectious persons within 3-days of travel.
iv. Inevitably, the logistics of delivery of PCR versus an LFD is such that there is an increased time between test and travel for PCR compared to LFD. Many countries (including some UKOTs) lack the ability to do PCR outside of a clinical setting so there may be some logistical value in administering an LFD close to departure. To optimise the effects of pre-departure testing, an LFD closer to the time of travel may offer better rates of identification of infectious people than a PCR test taken 48 to 72-hours before departure.
To understand why having a test closer to departure is better than a more sensitive one further away the figures below show percentage of infected travellers detected by time and sensitivity of test. If we assume an 80% sensitive LFD at the airport at time of departure (represented by the black dashed line) we can see that the detectable fraction decreases the longer the test is taken ahead of the departure, approximately 8 to 10% for every 24-hour interval.
Figure 2: Percentage of infected travellers detected by time and sensitivity of ‘test’ (7 and 14 day infection window) (DfT analysis).
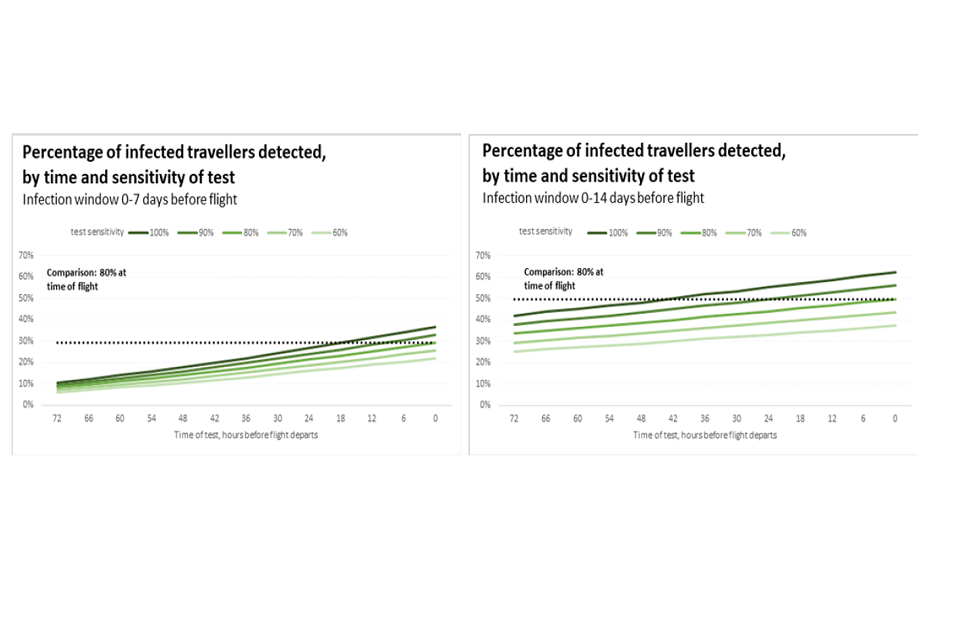
Two graphs: percentage of infected travellers detected (y-axis) against number of hours before flight departure the test was taken (x-axis). Left- and right-hand side graphs respectively show infection windows 0 to 7 and 0 to 14 days before flight.
c. However, effectiveness is also highly dependent on test sensitivity. Using the sensitivity estimates from the Liverpool Mass Testing, pre-departure LFD testing on the day of travel is estimated to detect an additional 11% (10%, 11% of infectious travellers beyond the proportion already captured by syndromic screening (Quilty) – similar to the 10% detected by PCR 3 days before departure (Gent). LFDs with higher sensitivity are available (with the WHO recommending minimum performance requirements of more than 80% sensitivity and more than 97% specificity), and these would therefore pick up a higher proportion of travellers [footnote 5].
d. The value of pre-departure testing is moderated by the effectiveness and or concurrent implementation of syndromic screening. In the absence of syndromic screening (or with lower screening effectiveness than the assumed model parameter of 70 to 100%), many individuals will likely instead be captured through pre-departure testing.
e. Even if more sensitive LFDs are used, test performance may be lower among travellers than the general population, since a significant proportion of symptomatic individuals and contacts should already have been prevented from travelling. Evaluations of LFD usage at points of entry are limited (WHO) [footnote 6].
f. On an absolute basis, pre-departure testing has little to no comparative advantage to post-flight quarantine of any duration (assuming full adherence) (Clifford). However, this neglects to account for potential behavioural effects including acting as a deterrent to symptomatic travellers who might otherwise choose to travel or providing a false confidence in negative results leading to a likely lower adherence to post-entry control measures.
g. Pre-departure testing may also reduce potential transmission between an infectious traveller and others in the process of travel. The impact of this on onward transmission is generally not modelled.
14. No single intervention, other than a complete, pre-emptive closure of borders, or the mandatory quarantine of all visitors upon arrival in designated facilities, irrespective of testing history, can fully prevent the importation of cases or new variants. Conversely, even if all other interventions are used in combination, some duration of quarantine is still likely to be necessary to minimise the number of imported cases.
15. Combined pre-departure syndromic screening and pre-departure testing may result in a total reduction of 44% (43%, 44% of infectious travellers prevented from arriving, though limited detail was provided for how this estimate for the 34% of this due to syndromic screening was reached (Quilty).
a. This assumes LFD sensitivity from the Liverpool Mass Testing study. Effectiveness is still dependent on previously outlined issues, and it is unclear whether the joint benefit of both interventions (including any behavioural effects) is justified by the additional financial costs of testing, personnel, and training.
16. Test-on-arrival without quarantine could lower the volume of infectious arrivals from entering the community. However, with limited evidence and impractical assumptions about adherence after testing, the true population-level benefit may be insufficient to justify the high-effort, potentially high-cost intervention.
a. When adherence to isolation (if test returns positive) is maximised, the effectiveness of test-on-arrival policies is driven by test sensitivity: with 100% adherence, use of an LFD reduces the proportion of travellers entering the community from 48% (36%, 56%) to 38% (28%, 43%) or 18% (14%, 26%) assuming Oxford and PHE results for test sensitivity; use of PCR reduces it to 10% (5%, 15%). (Quilty)
17. Post-entry repeated testing with LFDs and no quarantine is not likely to avert substantial transmission. Self-administered LFDs have not demonstrated real-world effectiveness at significantly reducing further infections at a population level.
a. Maximum stringency LFD testing strategies still allow a significant proportion of infectious travellers into the community. One modelled scenario using 10 daily LFDs including pre-departure syndromic screening and a pre-departure LFD still suggested 26% (18%, 28%) of infectious travellers are never detected and risk further transmission. (Quilty)
b. LFD usage is highly dependent on test sensitivity. Using the highest accepted sensitivity for the Innova LFD, the proportion of undetected travellers who arrive in the community reduces from 26% to 14% (10%, 20%) (Quilty).
c. These strategies also appear to produce more secondary infections than any other quarantine intervention, especially in the first few days. However, the effect of this approach is highly variable and is dependent on the effectiveness of contact tracing strategies.
18. Post-entry quarantine with a required negative PCR test to exit quarantine has the most substantial effect on reducing the risk of infectious arrivals of any other intervention considered in isolation. Compared to a 14-day quarantine period, a 7-day quarantine is likely to achieve comparably high levels of effectiveness in reducing the number of infections entering the community.
a. Several approaches to quarantine have been modelled. These include a simulated model evaluating the optimal timing and duration of self-quarantine and screening or testing strategies (Clifford), another assessing different types of post-exit testing (Quilty), and others looking at quarantine for various exposure situations including travel and contact tracing (Wells).
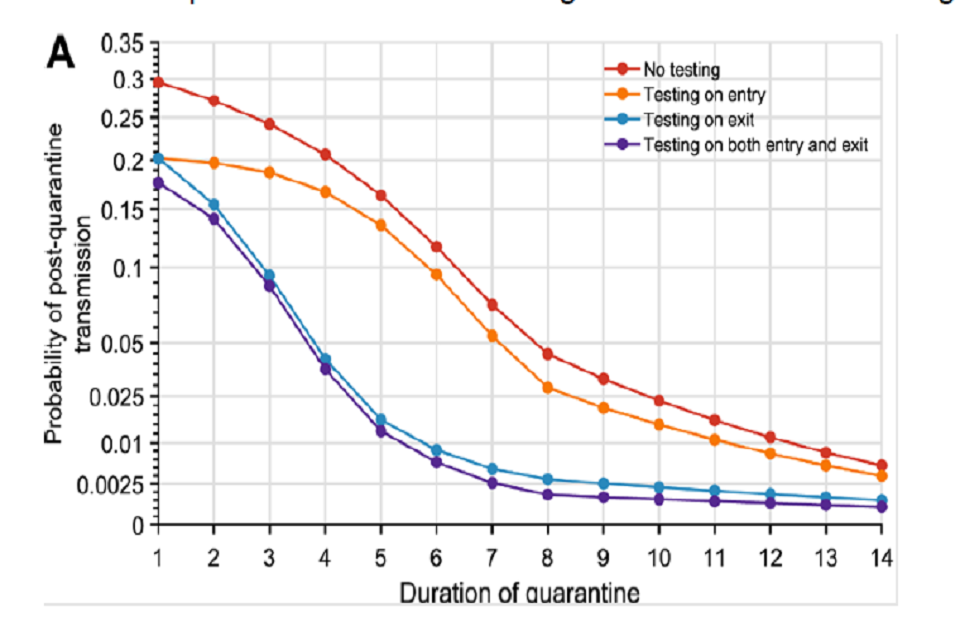
Graph showing probability of post-quarantine transmission (y-axis) against quarantine duration (x-axis). Four trendlines are seen: red for no testing; orange for testing on entry; blue for testing on exit; purple for testing on both entry and exit
Figure 5: Probability of post-quarantine transmission, by duration of quarantine and testing strategy (Wells).
b. Most models suggest the maximum 14-day quarantine period may be reduced, and a duration of at least 5 days or longer with PCR test on exit may be considerably effective. While the full duration is almost completely effective at reducing the number of infections entering the community (more than 99%) (Clifford, Quilty), one model suggests a 7-day and 5-day quarantine (8 and 6 days with test) would have an approximately 95% and 89% reduction, respectively (Clifford). A second model shows that 10 days without a PCR test could be as effective as the 14-day period (Quilty), while a third showed that a 7-day quarantine with test could result in a less than 1% chance of post-quarantine transmission.
c. The effectiveness of different approaches depends on the usage and timing of tests during quarantine. All analyses agreed that testing on exit was the best strategy, while models that evaluated the usage of a second test concluded that the addition of another test either on entry or at different points during quarantine have limited benefit beyond a slight reduction at the longest quarantine durations (Wells, Clifford).
d. Quarantine strategies are also ultimately driven by the proportion of asymptomatic infections. (Clifford) As duration of quarantine increases, those who become symptomatic develop symptoms in quarantine instead of the community, and those released from quarantine are more likely to no longer be infectious. One model evaluated a range of asymptomatic population proportions, finding that even isolating 100% of symptomatic individuals immediately upon onset of symptoms would still be insufficient to lower Rt less than 1 in an epidemic with a basic infectivity profile (Wells).
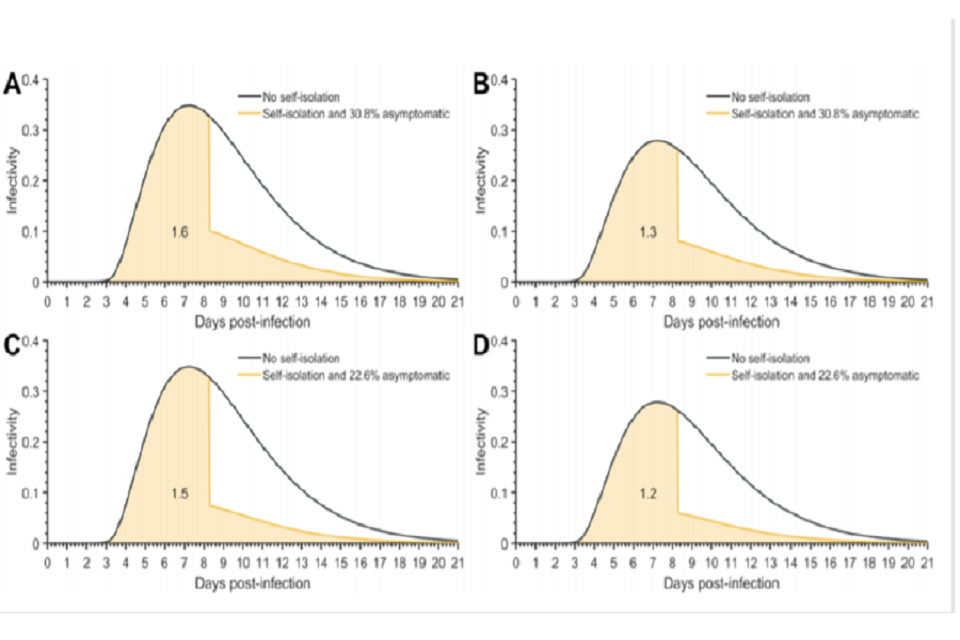
Four infectivity curves plotted against days post-infection. Clockwise from top left: 1.6 written under curve A; 1.3 B; 1.5 C; and 1.2 for D. Black lines represent no self-isolation. Peach lines show self-isolation with varying asymptomatic percentages.
Figure 6: Infectivity curve at days post-infection, by proportion of asymptomatic infection (Wells).
e. The impact of quarantine should be considered in context of local incidence. As with most models in this area, the relative risk of onwards infection or number of imported infections demands translation to absolute risk and a comparative interpretation to the domestic situation.
f. To supplement quarantine strategies, PCR testing on arrival with quarantine could give the potential opportunity to sequence all positive tests from infectious arrivals on entry to identify new high-risk variants. A subsequent risk-stratified strategy with increased intensity of interventions on new high-risk variants may prevent further entry the community, though this brings significant operational challenges (and would require a significant proportion of sequencing capacity to be focussed on travellers).
g. Overall effectiveness also depends on adherence and the quarantine approach used. Ideally quarantine should be in a location which removes the risk of within-household transmission, such as in a dedicated hotel. It will be important to explore the evidence, and apply measures that can be taken to maximise effectiveness and adherence to quarantine, and reduce risks of onward transmission. SPI-B are looking into the specific question of drivers of adherence, how these can be enhanced through interventions, and the maximum level of adherence we can expect in real-world settings after deploying these interventions.
Travel bans
19. Travel bans are not the most effective tools to reduce the infection rates in all circumstances. They are likely to be more effective if domestic rates are near a tipping point on exponential virus growth and infection rates domestically are already very low. Travel bans are likely to be less effective (but not ineffective) where tight domestic restrictions are in place (such as lockdowns) which minimises local domestic onward transmission and or an effective international arrival isolation, quarantine or testing regime (with high compliance) is in place.
a. Travel bans can be effective in delaying the spread of SARS-CoV (McLeod et al, Russel et al) [footnote 7] [footnote 8].
b. The closure of borders can only positively affect the epidemic trajectory if combined with a 50% or higher reduction of transmission within the community or where epidemics are close to tipping points for exponential growth (Chinazzi, et al).
c. The risk of international policy is relative to domestic incidence, with countries with low domestic incidence but high travel volume requiring more stringent measures to reduce relative risk. [footnote 9]
d. When travel bans targeted at specific countries are put in place, there is also a risk that travellers cross borders and travel to the UK via a third country, which is difficult to track. Therefore, such a policy does not eliminate the importation risk-specific risks are country and connectivity dependant.
e. Travel bans imposed by another country (for example, outbound, in absence of an inbound travel ban) will also reduce inbound travel and therefore risk of importation.
20. Travel bans applied in isolation cannot stop the importation of new variants. Whilst they do offer potential to delay the spread, the time lag associated with the identification of a new strain (sequencing, genomic surveillance, and so forth) and then policy implementation has been found to allow variant to be exported from the country of origin.
a. International examples show new strains have spread before being identified.
b. LSHTM suggest there are many more of the new SA variant infections in the UK than have been reported. They estimate “there were 78 (95% CI: 17 to 230) infections with the SA 501Y.V2 in the UK at the point the second case tested positive on 12 December”.
c. A new strain that originated in Manaus, Brazil was initially picked up in Japan, following the exportation of cases to Japan (Faria). The higher diversity and the earlier sampling dates of P.1. in Manaus corroborates the travel info of recently detected cases in Japan, suggesting the direction of travel was Manaus to Japan [ref].
d. If there is an effective policy regime including testing and or quarantine or isolation for travellers in place with high adherence, or if strict domestic lockdown measures are in place, then the risk of infection spreading is reduced, as noted in other studies. If this is not the case, then the time lag issue may be a more significant issue.
e. Identifying, tracking and reacting requires high levels sequencing and testing capability and capacity, rapid exchange of information and high levels of coordination between countries, particularly those with high levels of connectivity. There is an important opportunity for coordinated and supporting international action and standard practices to deal with this exchange and minimise future risks and minimise cost associated with pre-emptive travel bans.
21. We do not know what the impact of travel bans is on the ‘critical mass’ of traveller importations. We didn’t find any evidence to indicate if travel bans could reduce the risk of the critical mass of importation being reached.
a. WHO found partial travel bans to only have potential to delay the spread and peak by a few weeks or months, but they found no evidence it could be contained within a defined geographical area. It would take extensive travel restrictions (over 90%) to meaningfully effect the magnitude of the epidemic.
22. Travel bans have social, economic and political implications. They could in some circumstance be high-cost policy to keep in place in the absence of a well-known or credible risk. The potentially large negative impacts of imposing a ban means there needs to be high confidence in the effectiveness of such a tool if used in isolation.
Further questions and considerations
22. Further modelling and investigation to understand the magnitude and difference of whether current or other test and isolation regimes offer enough protection against new variants of SARS-CoV-2 over and above a pre-emptive, ongoing travel ban (such as being imposed before a risk has been identified)?
23. Further evidence of adherence and compliance rates is crucial to the effectiveness of testing, quarantine, and isolation regimes. What enforcement and measures are most effective? What international traveller non-adherence behaviours represent the largest risk? How can adherence to quarantine be maximised, including behavioural interventions, and use of non-household locations?
24. Trip length is likely to impact on testing effectiveness, particularly PDT. Further modelling should be undertaken to understand the impact of trip length on effectiveness of testing and isolation or quarantine regimes?
25. Further evidence and surveillance needed to understand the size of indirect or third country importation risk (following a direct travel ban) as well as the importation risk following a travel ban.
26. What is the evidence associated with current available tests ability to detect new variants? How easily can new variants be detected and distinguished from other variants via the current (or alternative) testing regime?
27. Could better surveillance, scientific developments or medical interventions speed up the process of identification of a new variant, so that we can more effectively target a travel ban?
Annex 1: Travel ban case studies
1. New Zealand
a. New Zealand implemented a national lockdown in early 2020, this led to the successful elimination of community transmission there. This eventually eliminated SARs-CoV-2 from New Zealand for approximately 120 days, after which is was reintroduced following importations from international travellers [footnote 11]. Travellers were initially allowed to self-quarantine, however after incidences of improper isolation, compulsory lockdown at airport hotels was introduced.
b. Geoghegan, J L, et al (2020) finds the introduction of a New Zealand lockdown in March 2020 resulted in fewer than 20% of introductions into New Zealand leading to more than one additional case [footnote 10].
c. In mid-January, New Zealand had an approximately 0.002% test prevalence and had recorded 1,872 total cases.
2. South Africa
a. In late 2020, genomic sequencing identified a new variant of SARS-CoV-2 (501Y.V2) in South Africa. By the time this variant had been identified and a UK travel ban imposed on South Africa and all southern African nations, confirmed cases had already reached the UK.
b. This suggests that genomic sequencing cannot be relied upon to trigger timely international travel bans. This is especially true when South Africa where routinely conducting genomic sequencing – the delay in detection would be much longer in other countries without these capabilities.
c. Modelled estimates of this variant by LSHTM [footnote 11] finds the new South Africa variant to be ‘roughly 50% (95% CI: 26 to 79%) more transmissible, under the assumption there is complete cross protection from previous infection with the wild type’.
d. PHE’s current predicted test predicted prevalence in South Africa is 82.4%.
3. Manaus, Brazil
a. A new strain that originated in Manaus was initially picked up in Japan, following the exportation of cases to Japan. The higher diversity and the earlier sampling dates of P.1. in Manaus corroborates the travel info of recently detected cases in Japan, suggesting the direction of travel was Manaus to Japan [footnote 12].
b. This raises concerns about the ability for short term-travel bans to effectively contain new variants, given exportation of the new strain is likely given the time lag associated with identifying and applying a travel ban.
4. Australia
a. In 1918, Australia implemented a maritime quarantine to control against the spread of influenza, which has spread rapidly across other South Pacific Islands. The arrival of influenza was delayed reaching Australia; 3 months later than it reached New Zealand, which had not implemented the same restrictions [footnote 13].
b. The first SARs-CoV case identified in Australia was in January 2020. In March, various measures were introduced to control the outbreak, including lockdowns, the closure of international borders, social distancing and quarantine hotels for returning citizens. These measures have resulted in one of the lowest prevalence rate per million worldwide.
c. In mid-January, Australia had a 0.001% test prevalence rate and recorded 28,658
total cases.
Annex 2: Full list of Department for Transport potential policy measures
Proposed measures and sub measures
1. Stay off, remove from travel corridor list.
2. Increased surveillance.
2a. Increase surveillance in post.
2b. Genome testing all positive cases.
3. Reduce risk – improve hygiene, minimise exposure.
3a. Improved cleaning and social distancing standards, and or separation of crew and pax (for example, crew with full PPE).
3b. More stringent travel advice on outbound (FCDO); could include the risk to passengers in that HMG may not repatriate British nationals if borders are closed.
3c. Wider campaign of information, for example through freight operators.
4. Enhanced quarantine.
4a. Enhanced enforcement for those travelling from affected areas.
4b. Retrospective self-isolation, those who have travelled from the region or country previously voluntary or mandatory self-isolation.
4b. Require all household members to self-isolate.
4c. Remove red+ countries from test and release.
5. Compulsory testing at those returning from high-risk areas
5a. Testing before return departure. Not allowed on flight, ferry, or international train without negative result.
5b. Testing at port of arrival.
5c. Those testing positive will need to stay in reception centres.
5d. Quarantine all passengers in reception centres until day X and X negative tests.
Bibliography
Anon., 2021. Global Report: Lineage B.1.1.7 [online]. cov-lineages.org.
Chan, Daniel.Z.L. (2020). The impact of a national COVID-19 lockdown on acute coronary syndrome hospitalisations in New Zealand (ANZACS-QI 55). The Lancet Regional Health - Western Pacific, [online] 5, p.100056.
Chinazzi, M., Davis, J. T., Ajelli, M., Gioannini, C., Litvinova, M., Merler, S., Piontti, A. P. y, Mu, K., Rossi, L., Sun, K., Viboud, C., Xiong, X., Yu, H., Halloran, M. E., Longini, I. M., and Vespignani, A., 2020. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak [online]. ScienceMag.
Clifford S, Quilty BJ, Russell TW, Liu Y, Chan YWD, Pearon CAB, Eggo RM, Endo A, Flasche S, Edmunds WJ. Strategies to reduce the risk of SARS-CoV-2 re-introduction from international travellers. [online] medRxiv.
Cov-lineages.org. (n.d.). global report. [online]
Du Plessis, L. and COVID-19 Genomics UK Consortium, n.d. Establishment and lineage dynamics of the SARS-CoV-2 epidemic in the UK. ScienceMag.org [online].
Faria, N. R., 2021. Genomic characterisation of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings [online]. Virological.org.
Geoghegan, J. L., Ren, X., Storey, M., Hadfield, J., Jelley, L., Jefferies, S., Sherwood, J., Paine, S., Huang, S., Douglas, J., Mendes, F. K., Sporle, A., Baker, M. G., Murdoch, D. R., French, N., Simpson, C. R., Welch, D., Drummond, A. J., Holmes, E. C., Duchene, S., and Ligt, J. de, 2020. [Genomic epidemiology reveals transmission patterns and dynamics of SARS-CoV-2 in Aotearoa New Zealand] (https://www.medrxiv.org/content/10.1101/2020.08.05.20168930v3) medRxiv. [online].
Hien, T.T., Boni, M.F., Bryant, J.E., Ngan, T.T., Wolbers, M., Nguyen, T.D., Truong, N.T., Dung, N.T., Ha, D.Q., Hien, V.M., Thanh, T.T., Nhu, L.N.T., Uyen, L.T.T., Nhien, P.T., Chinh, N.T., Chau, N.V.V., Farrar, J. and van Doorn, H.R. (2010). Early Pandemic Influenza (2009 H1N1) in Ho Chi Minh City, Vietnam: A Clinical Virological and Epidemiological Analysis. PLoS Medicine, 7(5), p.e1000277.
Ipsos Mori, 2020. Public Perception of Self-Isolation Rules [online]. Ipsos MORI.
Mateus, A. L. P., Otete, H. E., Beck, C. R., Dolan, G. P., and Nguyen-Van-Tam, J. S., 2014. Effectiveness of travel restrictions in the rapid containment of human influenza: a systematic Review [online]. World Health Organization. Available from:
McLeod, M.A., Baker, M., Wilson, N., Kelly, H., Kiedrzynski, T. and Kool, J.L. (2008). Protective Effect of Maritime Quarantine in South Pacific Jurisdictions, 1918-19 Influenza Pandemic.
Emerging Infectious Diseases, [online] 14(3), pp.468–470.
Office for National Statistics, n.d. Non- Exempt International Arrivals Self-Isolation Behavioural Survey.
Oxera and Edge Health, Nov 2020, Modelling effectiveness of airport testing regimes, Prepared for Virgin Atlantic, IAG, TUI, Heathrow, MAG, Collinson, Airlines UK and IATA.
Pearson, C., Russell, T., Eggo, R., Kucharski, A., and Edmunds, J., n.d. Preliminary analysis of novel South Africa SARS-CoV-2 variant 501Y.V2 and importation risk in UK. [Unpublished]
Public Health England (Gent N). Modelling note: pre-departure testing effectiveness. [Unpublished]
Russell, T. W., Wu, J. T., Clifford, S., Edmunds, W. J., Kucharski, A. J., and Jit, M., 2020. Effect of internationally imported cases on internal spread of COVID-19: a mathematical modelling study. The Lancet Public Health, 6 (1).
Smith, P., 2020. Covid-19 in Australia: most infected health workers in Victoria’s second wave acquired virus at work. The BMJ [online].
UK Government, 2021. Coronavirus (COVID-19): testing for people travelling to England [online]. GOV.UK.
UK Government, 2021. Multidisciplinary Task and Finish Group on Mass Testing- Behavioural Considerations [online]. GOV.UK.
TTI Modelling Group. Comparison of quarantine and testing strategies to prevent onwards infection from infected travellers returning to the UK from abroad. [online] GOV.UK.
Lai S, Floyd J, and Tatem A. Preliminary risk analysis of the spread of new COVID-19 variants from the UK and South Africa. [online].
Wells CR, Townsend JP, Pandey A, et al. Optimal COVID-19 quarantine and testing strategies. Nat Commun. 2021;12(1):1-9. doi:10.1038/s41467-020-20742-8
-
www.who.int/bulletin/volumes/92/12/14-135590/en/ ↩
-
ONS, 30 September - 8 October 2020, n=1,191. ↩
-
ONS, 23 to 25 September, n=1060 GB adults. ↩
-
TFMS: Behavioural paper supporting the consensus statement on mass testing, 27 August ↩
-
WHO. Antigen-detection in the diagnosis of SARS-CoV-2 infection. ↩
-
WHO. COVID-19 diagnostic testing in the context of international travel ↩
-
Protective Effect of Maritime Quarantine in South Pacific Jurisdictions, 1918–19 Influenza Pandemic ↩
-
Early dynamics of transmission and control of COVID-19: a mathematical modelling study ↩
-
Genomic characterisation of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings ↩
-
Protective Effect of Maritime Quarantine in South Pacific Jurisdictions, 1918–19 Influenza Pandemic ↩
