Barriers to Accessing Health Support for PIP, NS ESA, and UC Claimants
Published 7 October 2024
A report of research carried out by Basis Social on behalf of the Department for Work and Pensions.
DWP research report no. 1058
Crown copyright 2024.
You may re-use this information (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence.
To view this licence, visit the National Archives website.
Or write to:
Information Policy Team
The National Archives
Kew
London
TW9 4DU
Email: psi@nationalarchives.gov.uk
This publication is also available on our website at: Research at DWP.
If you would like to know more about DWP research, email socialresearch@dwp.gov.uk
First published October 2024.
Views expressed in this report are not necessarily those of the Department for Work and Pensions or any other government department.
Executive summary
This report presents findings from an in-depth qualitative research study exploring the experiences of Personal Independence Payment (PIP), New Style Employment and Support Allowance (NS ESA), and Universal Credit (UC) Health Journey claimants in accessing health support. It provides evidence to inform the design of future health signposting and support to claimants, as well as wider health and disability policy reform. The research was conducted as part of DWP’s Health Transformation Programme.
The research looked to understand the existing health support claimants access and the barriers they face in accessing health support, the relationship between accessing and using health support and a claimant’s benefit journey, what health support claimants feel would improve their prospects of becoming (or increasing) their economic engagement, and claimants’ openness to DWP in providing this (including levels of trust).
It involved 76 in-depth interviews with a range of claimants (according to type of claim and stage in the claims journey), including a small number of appointees, between December 2022 and March 2023.
Key findings and recommendations are as follows:
- participants were receptive to receiving health support signposting from DWP – none who participated in the research felt they had all the help they might need. There was no indication of mistrust regarding DWP’s motivations here. However, DWP is not seen as a health ‘expert’, and health support and signposting should be understood in this context
- four key principles have emerged that should be considered when implementing a broader health support programme: support must feel personal and tailored to the individual health and personal circumstances of claimants – this includes accounting for lifestyle needs and preferences, such as caring responsibilities or practicalities of needing to travel; support must have no strings attached – it should be entered into voluntarily and should not impact a claimants’ claims status; support must account for the skills levels and cognitive abilities of claimants, which can vary; and, support information may need to be shared with others in claimants’ support network
- it is important to consider individual and contextual needs for effective health support, as participants’ disabilities and health conditions are diverse and influenced by multiple factors
- there is a clear unmet health support need around mental health beyond any support managing claimants’ ‘primary’ disability and/or or health conditions
- health support would be strengthened by including broader support. For example, support in managing wider life challenges (e.g. housing or relationship breakdown) and practical administrative assistance for navigating the claims journey (particularly the application process, which can be challenging and exacerbate feelings of stress and anxiety for claimants)
- local charities and support organisations can be an important source of support for those aware of them. The presence of a strong interpersonal support network is associated with more successful health management and uptake of existing health support among claimants. Whilst those with a weaker interpersonal support network often have less successful health management
- participants described a diverse range of health support styles which could best meet their needs: from lower intensity ‘self-serve’ style signposting to more ‘high-involvement’, more personalised and intensive support for those with more acute needs. Accessibility and inclusion needs should also be actively considered (e.g., whether online or face-to-face contexts are more suitable)
- frontline staff and informal conversational settings are likely to offer the most suitable routes through which to offer health support, since they are experienced positively in the main for those in the claims journey
- this research was conducted against the backdrop of the new White Paper, Transforming Support: The Health and Disability White Paper[footnote 1]. It is encouraging to note that several research findings reinforce some of the new policies being proposed, including the offer of more personalised support to claimants
Acknowledgements
This research was commissioned by the Department for Work and Pensions in October 2022.
The authors would like to express their gratitude to the Department for Work and Pension’s Social Research team for their management of the project and their valuable input and support. We extend our thanks to Ailsa Redhouse, Dr Ashley Overton-Bullard, and Salma Afzal for their project leadership and contributions throughout the process.
This project was conducted by independent researchers, Basis Social, in partnership with disability research specialists, Open Inclusion, who helped to ensure the research was sensitive to the subject matter and the nature of the participants engaged.
Finally, we would like to thank all the claimants and appointees who gave up their time to participate in this research and share their experiences with us.
Author details
Rebecca Faulkner is an Associate Director at Basis Social.
Victoria Harkness is a Senior Director at Basis Social.
Cathy Rundle is a Research Manager at Open Inclusion.
Glossary
| Term | Explanation |
|---|---|
| Appointee | Someone formally appointed to act on behalf of a claimant who may face difficulties managing their own affairs. An appointee is responsible for handling the individual’s benefit claims, receiving payments, and ensuring that the benefits are used for the individual’s best interests. |
| Assessment stage interview | In this context, a research interview with a participant who had recently attended a DWP health assessment interview, but the result of this had not been communicated to them. |
| Condition management | Strategies used by an individual to actively address or minimise the impact of their disability and/or health conditions on everyday life and to improve wellbeing. This may involve the use of medical treatments, lifestyle modifications, and self-care practices. Used interchangeably with ‘health management’ (below). |
| Conversational settings | An informal or casual environment where people engage in dialogue or discussion. In the context of this research, conversational settings often refer to discussions with DWP work coaches or Jobcentre Plus staff, where claimants can share their views, ask questions, and receive support or guidance. |
| Disability and/or health conditions | A term used in the report to collectively describe the underlying reasons for a claimant receiving a disability benefit. It encompasses a range of physical, mental, sensory, or cognitive differences or challenges that may impact an individual’s day-to-day behaviour. This term has been chosen to acknowledge that the distinction between a disability and a health condition can be subjective and personal to each participant. |
| Fit note | Healthcare professionals issue fit notes to people to provide evidence of the advice they have given about their fitness for work. They record details of the functional effects of their patient’s condition so the patient and their employer can consider ways to help them return to work. |
| Healthcare professional | A healthcare professional is an individual who is trained and licensed to provide medical care, diagnosis, treatment, and support to patients. This term includes doctors, nurses, dentists, pharmacists, physiotherapists, psychologists. |
| Health assessment | This is a process conducted by DWP to assess an individual’s disability and/or health conditions in relation to their eligibility for certain benefits or support. The purpose of the assessment is to understand how an individual’s illness or disability affects their daily life. After the assessment, DWP has the information needed to decide on an individual’s benefits claim. |
| Health management | Strategies used by an individual to actively address or minimise the impact of their disability and/or health conditions on everyday life and to improve wellbeing. This may involve the use of medical treatments, lifestyle modifications, and self-care practices. Used interchangeably with ‘condition management’ (above). |
| Life-limiting conditions | Illnesses that have no known cure and are expected to significantly reduce a person’s lifespan. These conditions may progressively worsen over time and ultimately limit a person’s ability to carry out everyday activities. The focus of care for individuals with life-limiting conditions is often on improving their quality of life and managing symptoms rather than seeking a cure. |
| Medically complex | Refers to individuals who have multiple and/or severe medical conditions that require specialised care and coordination. These conditions may involve intricate diagnostic evaluations, extensive treatment plans, or the need for multiple healthcare providers from different specialties to manage the individual’s health effectively. |
| New Style Employment and Support Allowance (ESA) | A social security benefit for individuals unable to work due to a health condition or disability. Unlike the older form of ESA, it is based on National Insurance contributions rather than income. It provides financial assistance and additional support to help individuals meet their basic needs and access necessary services while they are unable to work. |
| NHS Talking Therapies | A form of NHS psychological treatment that involves engaging in conversations with a trained mental health professional to address emotional and psychological difficulties. These therapies aim to help individuals understand and manage their thoughts, feelings, and behaviours and are effective in treating conditions such as anxiety, depression, and stress. |
| Personal Independence Payment (PIP) | Is a social security benefit that provides a financial contribution to help individuals with long-term disabilities and/or health conditions to meet the additional costs related to their condition. PIP is based on the needs arising from a long-term health condition or disability rather than the condition or disability itself. PIP is not means-tested, is tax free and can be paid in addition to most other benefits received. Assessments for PIP involve a thorough evaluation of the individual’s ability to perform various tasks and activities. |
| Post-assessment stage interview | A research interview with a participant who attended a health assessment interview and who is aware of the result. This includes individuals in receipt of benefits or undergoing an appeal process. |
| Pre-assessment interview | A research interview conducted with a participant who had applied for a disability benefit but had not yet attended an assessment interview. |
| Trauma-informed approach | This is an approach to research which recognises and considers the potential impact of psychological trauma on participants and seeks to create a safe and supportive environment for them. It involves designing and conducting research with sensitivity to the potential triggers of retraumatisation that participants may experience. |
| Universal Credit | A welfare benefit that supports individuals and families with their living costs, including those who have health conditions or disabilities. It is designed to replace several existing benefits, making the application and payment process more streamlined. For individuals with health conditions, Universal Credit considers their specific needs, and they may receive additional support or allowances based on their circumstances. |
| White Paper | In this context, a White Paper is a concise, authoritative report issued by a government department. It outlines policies, proposals, or legislative plans on a specific topic and serves as a formal document to communicate government intentions and provide a basis for future legislation or policy changes. |
| Work coach | A DWP professional who supports individuals in their employment journey. They provide guidance, assistance, and personalised advice to jobseekers, helping them develop job search skills, explore opportunities, and create tailored action plans for finding suitable employment. Work coaches may also facilitate access to training, education, and support programmes to enhance employability. |
Abbreviations
| Abbreviation | In full |
|---|---|
| ADHD | Attention deficit hyperactivity disorder |
| CBT | Cognitive behavioural therapy |
| COPD | Chronic obstructive pulmonary disease |
| DWP | Department of Work and Pensions |
| GP | General practitioner |
| HIV | Human immunodeficiency viruses |
| HTP | Health Transformation Programme |
| IT | Information technology |
| ME/CFS | Myalgic encephalomyelitis/chronic fatigue syndrome |
| NHS | National Health Service |
| NS ESA | New Style Employment and Support Allowance |
| PIP | Personal Independence Payment |
| UC | Universal Credit |
Summary
Overview
This report provides findings from an in-depth qualitative research study with claimants applying for or receiving a range of health and disability benefits, exploring their experiences in accessing health support. Specifically, it has looked to understand the views of claimants of Personal Independence Payment (PIP), New Style Employment and Support Allowance (NS ESA), and Universal Credit Health Journey (UC). It provides evidence to inform the design of health signposting and support to claimants in the future, as well as wider health and disability policy reform. The research was conducted as part of the Health Transformation Programme (HTP), which aims to enhance customer experience and trust in DWP services and improve overall efficiency of the claimant process. The HTP includes the development of a new Health Assessment Service and the long-term transformation of the PIP service.
Research aims
This research was commissioned to address evidence gaps regarding where DWP could further strengthen claimant engagement and offer timely and targeted health related support as part of the Health Transformation Programme (HTP)[footnote 2]. To understand this, the research aimed to explore the following key areas:
- what health support (clinical and non-clinical) do claimants have access to and use?
- what is the relationship between accessing and using health support and a claimants’ benefit journey?
- what health support do claimants on disability-related benefits feel would help improve their prospects of increasing their economic engagement?
- do claimants on disability-related benefits feel, and want, DWP to have a role in signposting to health support?
- would claimants trust DWP to support them with accessing health support (and would this lead to them trusting DWP in work orientated conversations)?
In practice, pursuing these objectives has required an adaptable and flexible approach. The participants in this study, some of whom were highly vulnerable, have meant it was important to adopt a practical, sensitive, and open line of questioning when delving into personal and potentially challenging subject matter.
Methodology
In-depth interviews were chosen as the best method for investigating claimants’ access to and engagement with health support, as they allowed for a detailed exploration of experiences, perceptions and attitudes, and a better understanding of contextual constraints.
Between December 2022 and March 2023, a total of 76 approximately 60-minute interviews were conducted by members of the Basis Social team with claimants, including 4 with appointees. Participants were carefully chosen to ensure a diverse representation of individuals claiming Personal Independence Payment (PIP), New Style Employment and Support Allowance (NS ESA), and Universal Credit (UC) Health Journey to understand how experiences and views differed between the different benefit types, if at all. A range of demographic characteristics was also captured to ensure diversity in the sample. The research team also spoke to claimants at different stages of their claims journey. All research was conducted in a sensitive and trauma-informed way in close collaboration with disability research experts.
key findings
The research has revealed a range of significant insights important to consider as part of any future approach to delivering health support for individuals claiming disability-related benefits.
To begin with, it has highlighted a clear and genuine desire among claimants to receive health support signposting from DWP. There was no indication of mistrust or doubt regarding the Department’s motivations in providing this assistance. No claimant felt they had all the help they could need, and thus welcomed additional information. Participants without strong support networks described finding the idea of proactive support particularly appealing. However, it is important to note that the participants in this research did not necessarily see DWP as a health expert. Therefore, it is essential to understand signposting and support within this context. This might include considering the involvement of specialists (who may or may not be medical practitioners) that those with more complex disabilities and/or health conditions might require.
Four key principles have emerged through the research that should be considered when implementing a broader health support programme. First, support must feel personal and tailored to the individual health and personal circumstances of claimants. This in turn will help them feel more confident in accessing it. This includes accounting for lifestyle needs and preferences, such as caring responsibilities they may have, or the practicalities of needing to travel to receive health support. Second, support must have no strings attached – it should be entered into voluntarily. Claimants want to know their claims status will not be impacted. Third, support must account for the skills levels and cognitive abilities of claimants, which can vary. Fourth, support information may need to be shared with others in claimants’ support network.
When asked about the actual types of health support that could enhance their wellbeing, claimants described a diverse range of support styles, spanning from lower intensity, light-touch ‘self-serve’ style signposting to more ‘high-involvement’, personalised and intensive support among individuals with more acute needs. Accessibility and inclusion needs should be actively considered in providing support, for example, the extent to which claimants can and would prefer to access health support online or in a face-to-face context.
The research also highlights how participants often apply for benefits during disruptive periods in their lives. Connecting them to support for managing broader life challenges like housing or relationship breakdown, as well as providing practical administrative assistance for navigating the claims journey, would aid in better condition management by reducing stress.
Poor mental health emerged in this research as the issue that claimants have most in common, and is the biggest apparent unmet health support need for this group. For some this has the potential to become the condition with the greatest impact on an individual’s life if left unaddressed. Since claimants described mixed levels of understanding about, and paid mixed attention towards, their mental health, the true extent of claimants’ struggles here is likely to be being under-reported to the Department during the benefits assessment process.
The research has also highlighted those aspects of the claims journey that might adversely impact claimants’ health. It is important that approaches designed to improve the health of claimants are not solely limited to the policy of health support signposting. Support should consider the elements of the claims journey which are inadvertently impacting claimants’ health in a negative way too. For example, difficulties participants described around the complexity of the application form.
Linked to this, claimants stressed that they would not want any support offer to increase the complexity of the application process or add additional stages to the journey, which was already felt to be cumbersome. Frontline staff and informal conversational settings for those that experienced them could potentially play an important role in health support delivery.
The quality of a claimant’s support network has also been shown to significantly influence an individual’s ability to manage their health needs and access available support. Claimants who had a strong support network of family, friends, and supporters not only had access to greater levels of ad hoc assistance when needed, but they also reported better mental health and increased motivation to engage with health services and overcome barriers to accessing care. Charities and third sector organisations are an important part of this support network for those claimants who are aware of them. They not only introduce health management ideas, but also help with administrative tasks required to access support. In contrast, claimants without reliable support networks reported challenges in managing their health effectively and had reduced capacity or motivation to contact known services, or to conduct independent research on health support. These difficulties were associated with lower overall levels of mental health among this group.
Participants’ experiences of NHS services varied significantly. Some instances of satisfactory care were described, with other claimants found to have experienced significant challenges in accessing timely and effective NHS healthcare. Indeed, many participants hoped that a key benefit of any future DWP health support might be its ability to connect them more effectively with the NHS services they were currently struggling to access.
Finally, we note how this research was conducted against the backdrop of the new White Paper, Transforming Support: The Health and Disability White Paper[footnote 3] It is encouraging to note that several research findings reinforce some of the new policies being proposed, including the offer of more personalised support to claimants. For example, recent proposals to improve direct Work Coach support for ESA and UC Health Journey claimants outlined in the White Paper are to be welcomed in the context of offering health support, as are proposals to increase Work Coach understanding of mental health conditions and building connections between employment advice and NHS Talking Therapy services.
Recommendations
The research highlights a number of considerations that the Department may wish to reflect on when developing any future health support and signposting initiatives.
- the health support offered needs to account for the needs, capabilities, and preferences of claimants. The wide range of disabilities and health conditions among claimants, along with the impact of contextual factors on health management, suggests the need for a highly personalised and individualised approach to designing and delivering health support. In defining high-quality health support, claimants themselves stressed the importance of ideas and information being directly relevant to their lives
- extra consideration should be taken when thinking about how best to offer support to claimants with complex needs. The design and delivery of support for this group may require input from specialists to ensure its suitability
- mental health support should be a priority, even where no mental health issues are known. The impact of condition management can be detrimental to mental health, whilst declining mental health can make it difficult to maintain condition management
- health support should include offering signposting to a wider range of support services, including housing, counselling, and application assistance. This approach could serve to help claimants free up more mental ‘headspace’ to focus on their own healthcare needs
- some of the challenges and stress participants reported about the claims journey itself might be relieved through better communication and education from DWP about what they can expect from the process upfront. Further, providing practical administrative assistance for navigating the claims journey (particularly the application process, which can be challenging for some) for those who need it might also be considered (whether directly or by signposting to relevant third party organisations)
- extra support to those claimants with poorer support networks or who may be experiencing isolation should be considered. Support organisations can play an important role for more isolated claimants and should be part of future signposting activity. That said, it should not be assumed that claimants who report stronger support networks do not need health support, as this may inadvertently place unfair pressures on those providing that support (family, friends, etc.)
- future health support should consider the appropriateness of directing claimants to support beyond NHS services. There may be a potential benefit of providing claimants with signposting information about general health resources and support organisations beyond the NHS. For example, locally available free talking therapies
- further research would be beneficial for understanding how best to use conversational settings as a route through which to deliver future health support. The positive impact of face-to-face contact with frontline staff during the claims process has emerged as a notable finding in this research, and warrants further exploration as a way in which to offer health support
- to enhance trust in future health support promoted by the Department, the offer of support needs to be framed appropriately. To foster trust and confidence in the health support offering, communications should make clear that engagement with DWP health support is voluntary, and that failure to take support up will not impact claimants’ benefit claims. The emphasis participants place on attaining financial stability as a motivator for applying for benefits (over and above getting back into the job market) should also be borne in mind when thinking about how to frame and present health support signposting to claimants
1. Introduction
1.1 Overview
This report presents findings from an in-depth qualitative research study with claimants applying for or receiving a range of health and disability benefits about their experiences of accessing health support. Specifically, it has looked to understand the views of claimants of Personal Independence Payment (PIP), New Style Employment and Support Allowance (NS ESA), and Universal Credit Health Journey (UC). It provides the Department for Work and Pensions (DWP) with insights to inform the design of health signposting and support to claimants in the future, as well as wider health and disability policy reform.
1.2 The context for this research
This research has been conducted as part of the research and evaluation activities being undertaken to inform the Health Transformation Programme (HTP). The HTP is modernising benefit services to vastly improve customer experience, build trust in the services and the decisions the Department takes, and create a more efficient service for taxpayers. The Programme is developing a new Health Assessment Service and transforming the Personal Independence Payment (PIP) service over the longer term[footnote 4].
The Programme’s key strategic outcomes are as follows:
- increased trust in services and decisions
- a more efficient service with reduced demand for health assessments
- increased take up of wider support and employment
- improved customer experience with shorter journey times
- transformed in-house data and IT infrastructure that is secure
Of particular relevance to this research, the Programme is transforming the entire PIP service, from finding out about benefits and eligibility through to decisions and payments. The transformed PIP service will deliver a simpler application process for customers with more information and support available to those who need it, including helping them decide whether applying for PIP is right for them. Improved evidence gathering will also enable the Programme to better tailor the service to the customer’s circumstances. For example, they will only have a face-to-face assessment if this is the most appropriate method, and it may be unnecessary for the customer to have an assessment at all.
The programme is also creating a single new Health Assessment Service for all benefits that uses a functional health assessment. This will eventually replace the different services DWP and its assessment providers use to undertake health assessments across all benefits, including new IT and processes.
The Health Assessment Service will be fully integrated with other systems, including the transformed PIP service, to create a seamless customer experience. By improving how DWP gathers evidence and by enabling the reuse of information, the new integrated service will provide DWP agents and healthcare professionals with easier access to relevant information. This will reduce the burden on customers to provide complex information and reduce the need for them to provide it more than once.
In March 2023 DWP also published its Transforming Support: The Health and Disability White Paper[footnote 5]. This sets out in further detail proposals to improve the benefits process for people with disabilities and/or health conditions. Key proposals here include removing the Work Capability Assessment and offering more personalised support to claimants, testing an Enhanced Support Service for the most vulnerable claimants, and testing an Employment and Health Discussion.. Its content and recommendations touch on several findings uncovered through this research, which are reflected upon in the substantive chapters of this report.
1.3 Research objectives
Independent researchers, Basis Social, were commissioned to run an in-depth qualitative research study which aimed to understand more about the barriers that claimants with a disability and/or health conditions face in accessing health support. The participants in this research included a cross-section of PIP, NS ESA, and UC Health Journey claimants at different points in their journey. It also included four claimant appointees (those formally appointed to support claimants, such as family members) to understand potential needs from their point of view.
The aim of the research was to understand what role DWP could play in helping disability-related benefit claimants access health support. By improving health support to claimants, the hope is that DWP can help improve claimant Health Journeys, their quality of life and, where appropriate, move them closer to the labour market, specifically supporting the third of the HTP’s five strategic outcomes: that of “increased take-up of wider support and employment.”
The research aimed to explore the following key areas:
- what health support (clinical and non-clinical) do claimants have access to and use?
- what is the relationship between accessing and using health support and a claimant’s benefit journey?
- what health support do claimants on disability-related benefits feel would help improve their prospects of increasing their economic engagement?
- do claimants on disability-related benefits feel, and want, DWP to have a role in signposting to health support?
- would claimants trust DWP to support them with accessing health support (and would this lead to them trusting DWP in work-orientated conversations)?
In practice, pursuing these objectives has required an adaptable and flexible approach. The participants in this study, some of whom were highly vulnerable, have meant it has been important to adopt a practical, sensitive, and open line of questioning when delving into personal and potentially challenging subject matter. This approach is reflected in the main findings of the report. For instance, some participants found it challenging to describe what health support they needed from DWP. This could be because their medical needs were very specific, and they required targeted medical support. Additionally, some participants found it difficult to explain how DWP could best support them, especially given the relative complexity of the claims journey being discussed.
The report is organised to focus on the most important findings that help answer the main objective: understanding how DWP can assist people receiving disability-related benefits in accessing health support in the future.
1.4 Methodology
In-depth interviews were chosen as the best method for investigating claimants’ access to and engagement with health support, as they allowed for a detailed exploration of experiences, perceptions and attitudes, and a better understanding of contextual constraints. One-on-one interviews have also enabled sensitive handling of the subject, ensuring claimants’ voices have been heard and their perspectives fully understood.
Between December 2022 and March 2023, a total of 76 interviews were conducted. The participants were carefully chosen to ensure a diverse representation of individuals claiming PIP, NS ESA, and UC Health Journey. Additionally, the selection aimed to include participants at various stages of their engagement with DWP support, reflecting different points in their support ‘journey’. This involved conducting interviews with individuals at different stages of the process, including those who had not yet undergone assessment, those currently undergoing assessment, and participants who had already completed their assessments (see Appendix 1 for further details). The aim was to examine claimants’ experiences at various stages of their claims journey to gain a detailed understanding of potential support opportunities associated with each stage. As the researchers went on to discover, participants often struggled to identify their precise stage in this claimant journey, which has meant this aspect has been more challenging to investigate and call out during the research.
Qualitative sample design: an overview of the interviews achieved and with whom
The sample was a good mix of pre-assessment, assessment, post-assessment (and demographics) per claimant group
| Number of interviews | |
|---|---|
| Personal Independence Payment only | 30 |
| Universal Credit only | 21 |
| New Style Employment and Support Allowance only | 20 |
| Universal Credit and Personal Independence Payment | 5 |
| Total research sample | 76 |
Figure 1: Qualitative sample design
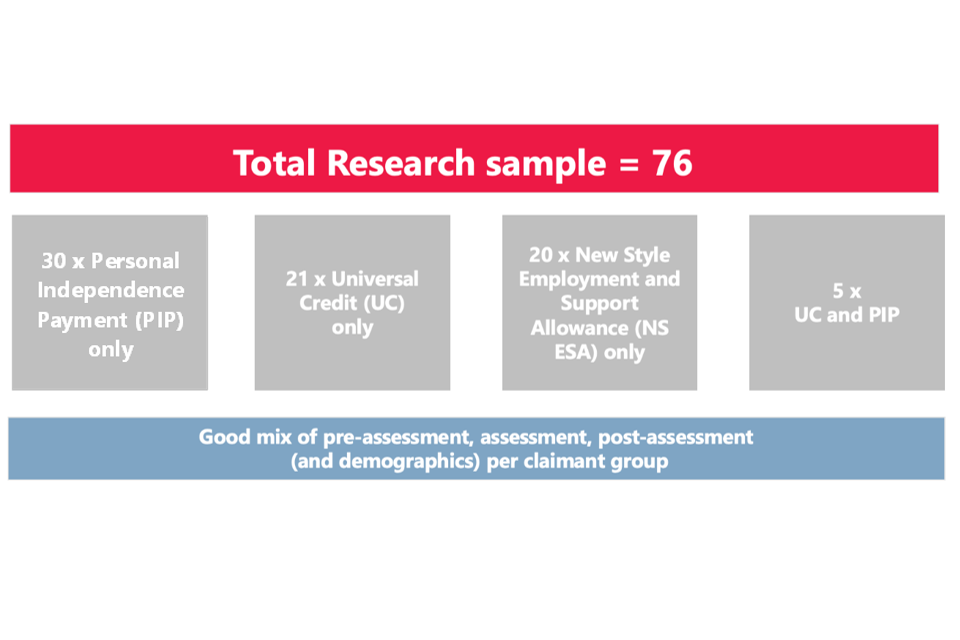
Whilst no ‘hard quotas’ were set for ethnicity, gender, and location, these factors were closely monitored during the recruitment process to ensure that a diverse range of profiles was included in the study. A breakdown of the final achieved quotas, including monitored quotas, can be found in Appendix 2.
To obtain a comprehensive understanding of the support requirements of all claimant groups, the final achieved interviews included four appointees (three for UC and one for PIP). As people formally appointed to support claimants, such as family members, this was an important viewpoint to capture.
The research team would suggest that this approach has allowed them to reach saturation point[footnote 6] This is the point in qualitative data collection when no additional issues or insights are identifiable. Repetition of themes in qualitative data signifies that an adequate sample size is reached and that further interviews across the various claimant groups is unlikely to have elicited any further insights.
Basis Social was provided with a claimant sample by DWP. To ensure the secure handling and management of data, best practice guidelines in accordance with GSR were followed. Within each quota cell, participants were randomly selected to approach for interviews from eligible batches of the sample, using the profile data available in DWP records. Most participants were contacted via post; however, email was used where an email address was on DWP records.
Telephone calls were then conducted to verbally screen participants and arrange an interview, ensuring overall quotas were achieved as far as possible. The approach taken to screening was based on disability research best practices, ensuring participation from claimants with diverse experiences. This approach enabled the researchers to accurately identify and include a wide range of claimants (based on demographic profiles and health conditions), ensuring their perspectives were fully represented. It also enabled them to check against the information provided about individual claimants in the DWP supplied sample, so the team could feel confident in who they were speaking to.
Participants were also screened to assess how their health condition impacted their daily lives. Their responses were then coded into three disability categories: ‘sense differently’ (e.g. visual impairments or hearing loss), ‘move differently’ (e.g. mobility or dexterity conditions), and ‘think differently’ (e.g. neurodivergent or mental health conditions). The disabilities and/or health conditions of the participants spoken to were complex and multifaceted, often involving comorbidity. These factors influenced their attitudes and behaviours regarding accessing health support and navigating the DWP claims journey. As a result, the reporting has focused less on describing these subjective sense categories in detail (focusing instead on the conditions in question).
The 76 participants encountered in this research experienced over 100 different conditions, with support needs as diverse as mobility differences, speech limitations, addiction, paranoia, and agoraphobia. Many participants had multiple conditions, which made their health needs more complicated. Additionally, the sample included individuals with medically complex conditions, as identified by the NHS or their healthcare providers. These conditions had a significant and long-term impact on their wellbeing, requiring substantial support. A more detailed breakdown of the range of disabilities and health conditions experienced by participants in this research can be found in Appendix 3.
In designing the research, careful consideration was given to the standard ethical guidelines for social research in government. It was acknowledged that some participants may find the topic of health in relation to their benefit status difficult to discuss. To mitigate stress, anxiety, and harm Basis Social adopted a communication and screening approach that made it clear to participants that the research was not connected to their DWP claim. All participants received materials in advance that provided detailed information about the nature of the research and that it was voluntary. The team ensured that participants felt comfortable discussing their experiences while understanding their rights and the guarantee of anonymity. Participants were also offered further signposting to health support after the interview. This approach aimed to create a safe and supportive environment, fostering trust and respect throughout the research process.
A standardised topic guide was created for use with participants from all benefit groups (see Appendix 4). To help them articulate their own benefit journey, participants were shown a range of exemplar benefit journeys that matched different pathways for PIP, NS ESA, and UC Health Journey claims, though it is worth stressing this was only limited to those conducting the interviews online (see Appendix 1). As noted previously, this made conversations related to the claims journey, including what this might mean for health support and signposting, more challenging since the researchers were unable to use these visual prompts.
Basis Social partnered with inclusive research experts, Open Inclusion, to develop the research and consent materials to ensure the lines of questioning were trauma informed[footnote 7].
Interviews lasted up to 60 minutes, building in flexibility for longer or shorter interviews depending on individual ability. Interviews were carried out online via Microsoft Teams or over the telephone, depending on participant preference (many participants did not have a working email address and/or were less comfortable using digital technology). Out of the total 76 interviews, 23 were conducted via Microsoft Teams, while 53 were conducted via telephone. All participants were given the option of having an advocate or appointee present for their interview, which a number took up[footnote 8]. To encourage participation, interviewees were provided with a £40 Love to Shop voucher as a thank you for giving their time to take part in the research.
The research team employed framework analysis, a common method in qualitative research, to structure and analyse the resulting data. This involved developing a thematic framework or coding scheme based on the research objectives and evolved lines of questioning, and the data itself. Relevant data segments were systematically coded and organised in matrices to facilitate comparison and synthesis. Through analysis and interpretation, patterns and relationships were identified, leading to well-supported conclusions. Framework analysis provides a structured and transparent approach to qualitative data analysis, enabling a systematic exploration of the research topic across diverse data sources and participant profiles. This was supplemented by regular brainstorms with members of the field team to identify and sense check the core themes emerging.
1.5 A note on interpretation
It is important to note that qualitative research is designed to be illustrative, detailed, and exploratory. It offers insights into the perceptions, feelings, and behaviours of people rather than quantifiable conclusions from a statistically representative sample. This has been reflected in the evidence presented in this report.
Verbatim quotes have been used throughout this report to help to illustrate points made in the main narrative. These have been labelled according to the disability and/or health conditions included in the supplied claimant sample and supplemented with any additional conditions that it emerged participants had during interviews (and which may or may not have been formally captured as part of their claim). This has been important to demonstrating the range and complexity of participants’ conditions. Also included are several short ‘pen portraits’, drawing anonymously on the individual participants spoken to, which have been designed to help bring the findings to life.
The research approach was designed to see if and how views and experiences differed according to the type of benefit individuals were claiming. Through this research it has been challenging to consistently draw out distinctions between benefit types – there has been significant consistency in terms of experiences, though the researchers have aimed to draw out difference where they can be confident doing so. There are a variety of reasons for this. First, it became apparent during interviews that the severity of a participant’s disability and/or health conditions did not always align with the specific type of benefit they were claiming, likely due to other influences at play such as financial status. Second, participants clearly varied in their understanding of the benefits system, which is likely to have been influencing their choice of benefit.
A note on language: Throughout the writing of this report, the research team has been acutely aware of the sensitivity surrounding discussions on health and disability. Linguistically, this is an area where best practices are constantly evolving. Open Inclusion has reviewed the language used in this report to ensure that it is suitably sensitive and free of stigma. The report also aims to reflect as best as possible the sorts of language and tone employed by participants themselves in discussing their specific disabilities and/or health conditions. All quotations used are verbatim, taken from interview transcripts and detailed moderator notes.
1.6 Report structure
This report is divided into four main chapters that address the project’s core research objectives, followed by a set of conclusions.
- Chapter 2 focuses on understanding how participants manage their health and the support they currently use. It looks at various factors that influence their approach to health and identifies any gaps in support based on their views
- Chapter 3 provides more detailed information on the health support available to participants and what drives them to use or not use it. It also explores the barriers they face in accessing this support currently
- Chapter 4 examines the connection between using health support and a participant’s journey through the benefits system. It explores if there are specific moments or ways support could be provided to them effectively
- Chapter 5 captures the opinions of participants about receiving health support as part of their benefits journey. It looks at the role DWP might play and about levels of trust in DWP offering this kind of support
- Chapter 6 summarises the main learnings from the research and the key factors to consider in providing health support going forward
2. How claimants experience and manage their health
This chapter explores the contextual factors influencing participants’ perceptions and management of their health, as well as the challenges posed by specific disabilities and health conditions. It provides insights into participants’ access to and need for health support, including their awareness, interest, and preferred types of support. The findings underscore the complex and personal nature of claimants’ health needs. Additionally, it highlights that when referring claimants with complex needs to health support, consideration should be given to involving specialists in the design and delivery. Furthermore, there is an apparent unmet need for mental health support among claimants and their appointees.
2.1 Multiple factors affect claimant health management
Participants, regardless of their specific disability and/or health conditions, or the type of benefit they had applied for, consistently highlighted to the researchers the highly personal and individualistic nature of their disability and/or health conditions. The unique aspects of their situation strongly influenced how they coped with their condition, their ability to identify relevant health support, and their willingness to access it. Participants commonly emphasised to the research team the importance of considering a variety of personal and contextual factors related to their experience and situation which they felt were key to understanding how they managed their disability and/or health conditions.
For some participants, the very nature of their condition was described as making health management challenging. For instance, they described their medical conditions’ symptoms as highly unpredictable and difficult to anticipate, with varying levels of intensity over time. To provide an illustration, the researchers received accounts from individuals with conditions such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) who emphasised that while they could manage certain basic tasks independently through energy planning and conservation, flare-ups in their condition or unexpected disruptions to their routine occasionally necessitated significant additional support, which was challenging to predict. Meanwhile, participants with degenerative conditions such as Alzheimer’s disease and osteoarthritis described experiencing highly personal changes to their physical and cognitive abilities.
Other participants in this research described being given specific medications as part of their treatment which exacerbated their existing symptoms in a way they felt was not commonly associated with the primary condition they were receiving treatment for. For example, one participant described how statins for a heart condition had on occasion impacted their memory. Another claimant with alcohol dependency described how this made them more prone to infection which impacted their management of bladder disease.
Participants who encountered personal challenges unrelated to their disability and/or health conditions often expressed difficulties in managing their health. To illustrate, claimants who faced literacy issues, language barriers, or difficulties in using and accessing digital technology described how these challenges affected their ability to identify and access relevant support. For example, by impacting their ability to proactively access information or communicate with medical experts online. Other participants highlighted broader environmental challenges, such as living in unmodifiable properties or areas with limited or inaccessible health services.
A number of participants in this project were also at pains to emphasise the role their own personality and life philosophy played in managing their disability and/or health conditions. This included life experiences which had required them to develop highly personal strategies to cope with the world. For example, highly negative experiences might have encouraged them to avoid strangers of a particular gender, or to conceal vulnerability from others. For others, this meant having a strong set of personal ‘rules’ surrounding their health management, such as a desire for autonomy or independence (“I can’t rely on others, so I need to rely on myself” – UC claimant, heart and kidney condition). These ‘rules’ influenced the types of support individuals went on to describe as feeling appropriate for their disability and/or health conditions, and when they felt this support would be best needed.
Case study 1: Meet Roy. Roy has had a difficult past, serving in the army and after this experiencing periods of homelessness. As a result, he highly values his independence and believes that seeking care is a sign of weakness. Prior to his heart attack, he served as a caregiver for a neighbour. However, he rejects the idea of being a care recipient himself and sees himself as someone who helps others, not someone who needs help. This mindset caused him to initially resist having home visits from a heart failure nurse after his release from hospital, until one day he fainted in the street, and it was clear he could no longer cope on his own. Due to his aversion to seeking help, he keeps his struggles hidden from his friends and family.
Whilst it is important to note that a small number of participants did not necessarily overtly call out the uniqueness of their disability and/or health conditions, this was typically because of their uncertainty about how their condition or situation compared to others. However, when describing how their condition affected their lives, it was apparent to the researchers that these participants still shared highly personal challenges that they believed were crucial to consider for effective condition management.
It is clear from speaking to participants that the factors that shape an individual’s relationship with their health and health management, as well as the symptoms they need to manage, are highly personal, varied, and will depend on their specific circumstances. This strongly points to the need for a more personalised approach to health support and signposting. And to ensure successful uptake of such support, it is necessary to fully understand and consider the broad range of factors at play.
2.2 Disabilities and health conditions can be complex and severe
Understanding claimant health needs and their barriers to accessing support is made more complex by the sheer variety of conditions which can lead people to claim disability benefits, as was very evident from the participants spoken to. Across this project’s 76 participants, participants described experiencing over 100 distinct conditions (see Appendix 3 for a list of the conditions encountered), with support needs as diverse as mobility differences, speech limitations, addiction, paranoia, and agoraphobia). It was common for participants to also experience more than one condition, which increased the complexity of their health needs.
Additionally, the sample included participants who described having conditions which are formally classed by the NHS or their healthcare provider as ‘medically complex’[footnote 9], meaning they have a substantial impact on their wellbeing that require significant and often long-term support. Examples here included individuals with schizophrenia (who may sometimes struggle to distinguish their thoughts and ideas from reality), participants with severe learning difficulties (introducing at times some challenges understanding complex information), and individuals with life-limiting conditions such as chronic obstructive pulmonary disease and cystic fibrosis (limiting their movement and breathing).
Claimants with severe conditions expressed that the scale of their health challenges would mean they would need a more sensitive approach when it came to identifying and accessing health support. They emphasised that even basic changes to how they managed their health should be made in consultation with a medical expert who would be best placed to understand the degree or risk involved. Following ‘generic’ or ‘off-the-shelf’ advice and guidance which might be offered through the claimant journey had the potential to risk causing harm for these participants since it was not rooted in a nuanced understanding of their condition. This concern was particularly pertinent for participants with multiple health conditions. They expressed concern about whether an intervention targeting one aspect of their health could end up adversely impacting or complicating another comorbid condition they had. Participants with a disability and/or health conditions which they themselves considered complex or sensitive were clear that they would not want to make substantial changes to their health management without medical advice.
Whilst support is always nice, there’s also the concern in the back of your mind that it might not be right for you or [DWP may not] have fully understood your condition. Well-meaning suggestions could in fact make matters worse which would be the worst outcome of all.
(PIP claimant, bladder cancer and lupus)
The big question I have with health advice is always whether this will be right for me. You’d want to check with a doctor to be safe.
(UC claimant, anxiety and depression)
The wide range of disabilities and health conditions experienced by claimants, and the complex ways in which these can intersect, suggests that extra care will need to be taken when considering the health support needs of those with more complex need. This might include the need to engage specialists in the design and delivery of health support for claimants with these more complex conditions and/or needs.
2.3 Life challenges can worsen conditions
For some participants, the need for benefits was described as accompanying significant periods of disruption in their lives. Participants explained that when navigating these periods of volatility, it often shifted their focus away from health management, resulting in less optimal care practices and challenges in establishing healthy routines. Among our sample, these challenges were more commonly reported by participants in the UC Health Journey group compared to other benefit groups.
Case study 2: Meet Linda. Linda, a claimant on Universal Credit, used to work as a cleaner at her local hospital, but had to give up her job due to the impact of Long Covid and a heart condition. The loss of her income has made it difficult for her to afford the rent, so Linda has spent the past month searching for new housing. She describes the entire process as stressful and overwhelming. The fear of eviction, combined with the physical energy required to view properties, has worsened her symptoms. Linda does not feel like she can focus on her health and rest until this issue is resolved. Since she does not live in council housing, she does not think there is anyone she can speak to about her situation and describes feeling alone.
Researchers also heard from several claimants with substantial caring responsibilities – on top of managing their own health conditions they were caring for others, some of whom also had a disability and/or health conditions. The pressure and exhaustion involved in managing this alongside their own health made it hard to plan effectively or put their own needs first.
Case study 3: Meet Adam. Adam is a PIP claimant who has recently suffered a spinal injury that has forced him to reduce his work hours. This has left him feeling financially stressed, especially with two autistic children who require a lot of support. He is worried about his ability to physically care for them and feels guilty for putting his own needs first. The lack of support for childcare and the need to advocate for his children’s needs is taking a toll on his mental and physical health. Adam currently relies on his mum to help with childcare when she can but knows this is not sustainable. Currently he feels too overwhelmed with his day-to-day responsibilities to find the time to contact health services. Getting more help with childcare would allow him to focus more on his own health management.
Claimants who faced such disruptive life events typically thought that targeted support aimed at reducing stress, such as housing assistance, counselling, and aid with administrative tasks, would be beneficial. This support was expected to help provide the necessary ‘headspace’ to focus on their own health and wellbeing.
However, unless they were already connected to third sector support organisations, many of these claimants faced challenges in identifying the appropriate channels to access such support. Those participants who actively engaged with support often mentioned relying on assistance from friends, family, or pre-existing relationships with support organisations established during previous stages of their lives. They also described receiving signposting from other services they were in contact with, for example, social services.
Another source of disruption and instability participants described, was deteriorating health conditions. In these cases, it was apparent that participants found it challenging to develop effective coping strategies, namely because they did not have enough time or opportunity to experiment with different lifestyle adaptations before their condition changed. Participants here described how the changing nature of progressive illnesses could make it hard to predict how a condition might be experienced in the future, making long-term accommodations more difficult to plan for. Whilst some described managing their condition well – typically those with robust support networks and good access to local health services – others reported difficulty in getting access to regular support conversations, including from the NHS, as their condition changed. As such, this group was open to the kind of health support and signposting which might help them better understand how their condition is likely to progress, and what this means for how they can plan for future health management.
The influence of broader life challenges on health management, and the extent to which claimants currently utilise services to address these challenges, indicates a potential benefit to claimants in signposting to wider support services where relevant.
2.4 Poor mental health is common, but not always formally recognised
Poor mental health can complicate the management of an individual’s disability and/or health conditions. In discussions with participants, the topic of poor mental health frequently came up without any prompting, although this was by no means the case for all participants. Spontaneous discussion of mental health was less common among those who had strong support networks and established care routines. However, some participants who described experiencing social isolation felt this exacerbated their symptoms. Other participants who had limited connections to family and friends felt this made it harder to manage their mental health and establish consistent care practices.
Some participants who were facing mental health issues had received formal diagnoses and treatment for conditions such as depression and anxiety. However, others had not received a formal diagnosis or treatment. Within this group, some shared their experiences of reaching out to their GP for support but had faced challenges with long waiting lists. Others admitted that they had not sought medical assistance due to the overwhelming demands of managing their primary health conditions, which left them with little energy or motivation to address their mental wellbeing.
The researchers also heard from participants who found it difficult to express their mental health challenges using medical terms, but who nonetheless were clearly struggling (describing periods of feeling low and hopeless, for example).
Some participants described how the deterioration of their physical health linked to their disability/health condition had led to anxiety. For example, one PIP claimant with Parkinson’s disease explained how they felt they were losing control and expressed concerns about how their condition was affecting those around them. Specifically, they worried about the increased burden placed on their loved ones, who had to take care of them.
I think about the future, and it all seems to be bleak. I just sit on my bed and cry.
(PIP claimant, Parkinson’s disease)
For others, deteriorating health was described as leading to a loss of identity. One NS ESA claimant who had left employment due to back pain and mobility issues, reported that they felt they had lost their ‘purpose in life’. Others who had left employment due to their deteriorating health described how a lack of day-to-day structure was now causing them low mood.
My whole life has been dedicated to my job. Now I have nothing.
(NS ESA claimant, chronic back pain)
Shame was a sentiment expressed by those who were used to “paying into the system” (NS ESA claimant, depression). For them, claiming benefits was interpreted as a loss of pride and status.
It makes me feel down that I’m reduced to this. It makes me feel small.
(UC claimant, rheumatoid arthritis)
Another way poor mental health manifested was because of participants feeling less able to participate in social activities, in turn leading to isolation. One PIP claimant explained that they avoided going out for fear of having a manic episode in public. We also heard examples of how medications claimants took could cause embarrassing side effects, such as sweating, flatulence, involuntary urination, brain fog, and fatigue.
I take a pain medication for my back which is a relaxant. This means I can sometimes soil myself. I’ve lost all my confidence and don’t want to go outside.
(PIP claimant, chronic pain and depression)
During interviews, it was not unusual for claimants to discuss their mental health in a way that indicated it was being ‘normalised’, and just part of their daily life. When asked if they had informed DWP about their mental health conditions, or had discussed it at their Health Assessment, several participants explained they were more focused on telling DWP about their physical conditions, since they understood this to be the Department’s primary concern. Others could not remember if they had brought up mental health at all.
Several claimants within our sample mentioned that the deterioration of their mental health occurred to such an extent it became the main challenge for them ahead of the original health condition which motivated them to apply for benefits in the first place. To cope with their circumstances, the researchers heard a small number of instances where participants were adopting behaviours they felt shameful of, including substance abuse. This in turn made it hard to convey the full extent of their health concerns to DWP.
At the start the main issue was my eyesight but now I would say it’s the drinking and the loneliness. That’s the first thing I need help with.
(PIP claimant, macular degeneration and alcohol dependency)
The idea of receiving support with their mental health was received positively by participants in the main. For those with less interest, this was more down to a desire to manage their own health independently without the involvement of a non-NHS organisation. But, again, participants here wanted to know that any support would account for their unique circumstances, including the disability and/or physical health conditions they are living with. In short, it was important mental health support aligned with their wider health management needs.
A lot of mental health support out there wants you to increase your exercise or talks about getting out in the world, which for me isn’t going to work. I barely have enough energy to get out of bed.
(PIP claimant, Scheuermann’s disease)
The repeated mention of mental health challenges among participants, and the observed lack of understanding in managing them, indicate a potential role for future health support to provide mental health signposting. Increasing awareness and take-up of mental health support is likely to make a substantial difference in motivating claimants to seek wider health support. Furthermore, these findings suggest the important role wider health support could play in preventing the deterioration of health conditions and thus the onset of poor mental health in the first place. Support needs to be cognisant, however, that mental health challenges can result in behaviours that are embarrassing for the claimant and which they may not wish to disclose. For example, the use of alcohol or illegal substances to manage low mood. When developing future support, the Department may wish to involve medical experts who can adapt solutions based on the needs of claimants with more complex conditions and communicate this clearly to claimants by way of reassurance.
2.5 Appointees’ mental health can suffer too
In seeking to understand health support needs, the research has also shown that mental health issues can occur among appointees too. Whilst the researchers only spoke to four appointees through this research, amongst this group all described challenges to their own mental health and wellbeing in supporting the person they acted on behalf of. This is relevant because it appears to be having an impact on the functioning of the claims process itself. The researchers heard examples of appointees struggling with poor memory or lack of concentration causing errors in paperwork. Lack of energy had caused challenges in securing key documentation in a timely manner, slowing down the claims process. One appointee described how depression had reduced their ability to perform care behaviours or advocate for health support on behalf of the claimant they represented.
These appointees would welcome support from DWP that helped them with their own wellbeing and health management, which in turn could benefit those they are caring for.
Case study 4: Meet Claire. She is a busy mother of three children and acts as an appointee for her 16-year-old son, Josh, who requires round-the-clock care due to a rare genetic disorder. She describes her life as grueling and exhausting. Due to Josh’s night seizures, Claire rarely gets any sleep and spends most of her waking hours managing his care or advocating for support from medical professionals. She describes experiencing periods of very low mood, which can be debilitating and, at their worst, impair her ability to care for her son including dealing with his paperwork. She identifies isolation as the biggest challenge she faces, as she is effectively confined to her home. She strongly believes that DWP should provide more support for appointees and would welcome assistance that helps her connect with other adults or provides signposting to organisations that could offer help. The pressure of her caring responsibilities means she has no time for health research herself.
To ensure effective advocacy for claimants, it may be beneficial for DWP to also offer support and signposting to appointees, particularly in relation to mental health and wellbeing.
2.6 Summing up
In this chapter, the report has explored the factors that influence how claimants perceive and manage their health and what this means for potential health support and signposting. It has found the following:
- the factors that shape an individual’s relationship with their health and health management, as well as the symptoms they need to manage, are highly personal and varied. This points to the need for a more personalised approach to health support and signposting
- given the potential risks identified by participants in signposting claimants with more complex needs to health support, any support offer should consider the extent to which specialists should be engaged in the delivery and/or design of support
- given what we have heard about broader life challenges in health management, there appears to be a role for offering signposting to wider support services where relevant (housing support, counselling, and help with administrative tasks, etc.)
- the repeated mention of mental health challenges among participants (and appointees), and the observed struggles in managing them, suggests mental health support and signposting will be important to consider as part of any future support offer
3. Access and engagement with health support
This chapter explores the factors influencing the availability and accessibility of health support for claimants, as well as the factors shaping these interactions. We have found that the strength of a claimant’s social network significantly impacts their ability to manage their disability and/or health conditions. Claimants who were more isolated with weaker social ties struggled more with their health condition. Some participants felt current pressures on the NHS were impacting their ability to access timely and high-quality treatment, while organising care beyond the NHS could be seen as challenging. Charities and support organisations play a crucial role in providing health management support for those participants who were aware of them. This again underlines the potential benefits of a strong social network to good health management.
3.1 Social connections impact how claimants access health support
When comparing participants who appear to be effectively managing their health to those who are not, the presence of strong social and support networks was identified by the research team during the analysis as a critical differentiating factor. Participants who had a reliable support system consisting of friends and family described more successful management of their disability and/or health conditions compared to those who lacked close relationships. Some participants explicitly mentioned the importance of their support networks, while in other cases, the research team inferred its significance from their descriptions of care practices and health management behaviours.
There were several key factors which participants attributed here.
First, participants reported that family and friends were often in the best position to recognise any changes in their health status. The individuals surrounding the claimant can detect and proactively suggest extra support needs early, before an individual’s condition deteriorates (and where the individual may not recognise they need support themselves).
After I first got diagnosed, I was working too many hours and really struggling. My husband took me aside and said you can’t go on like this, you look terrible, we need to make some big changes at home.
(NS ESA claimant, back pain and leg ulcer)
Secondly, many friends and family members were described as actively meeting claimants’ support needs themselves, often with significant self-sacrifice and expense (a fact mentioned by both claimants and appointees). Support can vary from personal care, such as washing and dressing, to managing household affairs, and from providing transportation to offering financial assistance to access privately funded care.
Case study 5: Meet Ken. Ken is a recipient of Universal Credit (UC) and Personal Independence Payment (PIP) due to his heart and kidney condition. Following a recent health scare that required hospitalisation, his youngest son, Patrick, decided to move back in to provide monitoring and support for his father’s condition. The specific tasks Patrick assists with vary from day to day, depending on Ken’s wellbeing. They include shopping, gardening, running errands, picking up medication, and taking Ken to a local social club. Although Ken feels guilty that Patrick invests so much time in his care, he finds it difficult to envision how he would manage such flexible support without his son’s help.
It is noted earlier in section 2.5 the pressure and stress that providing this support to claimants can have on those providing care, specifically for those appointees spoken to through the research. Whilst not the target audience for health support, this is relevant for DWP to consider given the potential impacts here.
Family and friends were reported to help broaden participants’ horizons by sharing new information, including treatment options and health management tips. Their role here was described as particularly important by participants who face mobility or mental health challenges which can limit their interaction with the outside world.
When my sister visits, she also shares ideas I can try. For example, sitting on a stool when I cook.
(UC and PIP claimant, arthritis)
Other interviewees described how receiving support from family and friends also eased the burden of engaging with health services and advocating on behalf of the claimant – for example, questioning treatment plans and pressing for additional support.
It’s been a struggle to get the NHS to take this serious[ly] and get my therapy, but mum has been with me all the way, on the phone, really pushing.
(UC claimant, depression and ADHD)
Importantly, participants with solid support networks often described how the love and care of friends and family had helped to boost their mental health during difficult periods. This increased their motivation to problem solve, ask for help, or experiment with new care practices.
My family are keeping me sane and encourage me to keep going and look for new solutions.
(UC claimant, anxiety and diabetes)
In stark contrast, participants with weaker social connections described less successful health management. While some explicitly mentioned the detrimental effect of social isolation on their health, the impact of poor social networks could also be inferred when considering the challenges this group was facing in accessing care they might need.
For example, the researchers heard from participants who described how they struggled with performing self-care behaviours at home, such as washing, dressing, or eating. This then impacted their energy levels and their ability to dedicate time to positive health management behaviours.
It takes me hours to get ready in the morning. Even putting on a shirt in the morning takes my breath away. All I can do is sit on the bed and wait until I have more energy. My son used to help with this when he lived here.
(UC claimant, angina and chronic pain)
Other participants described difficulties in leaving the house on their own, which would impact their ability to access healthcare resources and care options. This was attributed to factors such as mobility issues or limited transportation options (e.g. inability to drive or limited access to public transport) but was also an issue for those with social anxiety or mental health conditions.
For this group, social isolation was described as having a negative impact on their mental health. They reported symptoms such as low mood, decreased energy levels, and an increased sense of helplessness. These factors were explained as combining to decrease their ability to connect with healthcare services or support organisations which may help manage their condition. Low mood was also described as decreasing their motivation to find ways around these barriers.
I am very ready and desperate for any kind of support. If I had someone to speak to, even a cat, I think I would be coping with it all so much better. I might feel more positive.
(PIP and UC claimant, eye melanoma)
Case study 6: Meet Emily. She experiences agoraphobia and severe anxiety, which greatly restrict her ability to leave her house. Her fear of venturing outside has had a profound impact on her daily life, making simple tasks like visiting the doctor or seeking health support extremely challenging for her. Emily’s anxiety is triggered by the thought of being in crowded or unfamiliar places, leading to panic attacks and overwhelming feelings of fear and dread. Due to her condition, Emily has become increasingly isolated, as she avoids social gatherings and public spaces. Even leaving the house to attend medical appointments becomes a daunting prospect, causing her significant distress. This results in delayed or neglected healthcare, as she struggles to access the necessary support and treatment for her physical and mental wellbeing. Emily used to have a cousin living close by who would accompany her on short trips outside or run errands when she was not able to. However, since she recently moved away, Emily has stopped experimenting with going outside. Emily longs for a life free from the grip of agoraphobia and anxiety, where she can comfortably navigate the outside world and receive the healthcare she needs.
The research has revealed a clear association between effective care management and strong support networks among participants. As a result, the Department may wish to consider extra support to those claimants with poorer support networks or who may be experiencing isolation. The report already notes the impact on appointees, and by inference wider care givers, in supporting claimants in managing their health, so this is not to say that claimants who have support networks would not also benefit from health support.
3.2 NHS pressures are impacting accessible health support
The participants in this research either currently or previously received medical care as part of their condition management. The majority of participants received care from the NHS, while there were a few instances where participants mentioned receiving treatment from private medical care providers.
Participants’ experiences of NHS care and support varied. Some described receiving positive, proactive, and continuous care. This often corresponded with having regular appointments to monitor their health and identify additional support needs through NHS frontline services. However, for others, the healthcare system to them was felt to be ‘badly organised’, ‘distant’, and ‘disinterested’. One participant expressed that their interactions with the NHS and the difficulty getting an appointment made them feel like healthcare professionals had little interest in the daily challenges arising from their conditions.
In the main, participants had received targeted health treatment after diagnosis. Although, it is worth noting several individuals with mental health issues reported delays in treatment. In addition, following initial treatment, some participants felt like they had been left to navigate their ‘day to day’ on their own, without much guidance on practical steps they could take to enhance their quality of life or what to do if their health did not improve. This included a lack of advice or guidance from healthcare professionals about how their disability and/or health conditions might impact on their ability to work in the future.
It is worth noting that the researchers also heard examples of positive experiences with aftercare from the NHS. Interestingly, the differences in aftercare experiences did not appear to be strongly connected with the type of health condition the participants had. This indicates that variations in experiences may be influenced by specific hospitals or care trusts.
Case study 7: Meet Lauren. Six months ago, Lauren experienced a medical emergency and was urgently hospitalised due to cirrhosis of the liver. Since then, she has been dealing with physical weakness and chronic fatigue. During the emergency, she had positive impressions of the NHS staff and their care. However, after her surgery, she was discharged from the hospital quite swiftly and received minimal information about post-operative care or guidance on how her condition could improve. Although her GP has subsequently organised a follow up appointment, she feels uncertain about the specific circumstances in which she should reach out to them or the questions she should ask regarding her health.
A perception expressed was that this was the result of ‘service rationing’ by the NHS and that this in turn was affecting individuals’ ability to manage their care effectively.
When I was first signed-off the NHS gave me a course of CBT therapy. But this was very short. Only six sessions. I think it was obvious to everyone it wasn’t enough. And I asked for more and so did my therapist and it was just ‘nope that’s all you get’.
(NS ESA claimant, anxiety, depression and autism)
For a small proportion of participants who reported that they had been denied NHS care, it was apparent that they struggled to know how to challenge this decision or advocate for themselves. As such, they expressed a strong sense of frustration and helplessness in navigating the system.
The researchers also heard examples of where NHS medical practitioners had recognised and recommended additional care, such as hip operations or physiotherapy, however, extended waiting lists were causing delays to participants accessing treatment. Gaps in receiving timely care was felt to be causing the wellbeing of these participants to deteriorate, exacerbating anxiety and low mood disorders where these existed.
Finally, there was a view among some participants that pressures on the NHS had affected the style and quality of the GP care they had received. To illustrate the point, there were examples of participants having to show persistence in order to schedule regular appointments. Those with chronic or changeable conditions with low energy levels found this particularly challenging. There were also instances cited of being given less time with their GP to discuss their symptoms. Several participants described negative interpersonal interactions that had hindered the development of trusting relationships with their doctors. As a result, they felt less comfortable opening up about the difficulties they were facing, as illustrated in the case of Angela below.
Case study 8: Meet Angela. Until recently Angela was a seamstress in a local factory. She loved her job, but felt she was unfairly sacked due to her arthritis, which made it difficult for her to work efficiently. Angela never finished school, which impacts her self-esteem and confidence when dealing with those she sees as in a position of power. Angela’s old doctor was warm and sympathetic and encouraged her to open about her struggles. However, when Angela visited the surgery recently, she encountered a new GP who, seemingly under stress, was rude and abrupt with her. This attitude made Angela feel small and insignificant and she interpreted it to mean that her condition was not believed. She now vows to avoid the doctors at all costs.
One participant expressed that their interactions with the NHS and the difficulty getting an appointment made them feel like healthcare professionals had little interest in the daily challenges arising from their conditions.
The reported challenges faced by some research participants in accessing NHS care provides important context when considering what a future health support offer might look like. Future health support may wish to be mindful, for example, of signposting claimants to NHS services that people report finding difficult to access. As some individuals reported experiencing long waiting times for NHS treatment, providing guidance and support to claimants on how to maintain their physical and mental wellbeing in the interim may be beneficial.
3.3 Accessing health support beyond the NHS can be challenging
In addition to some of the challenges participants described in accessing NHS healthcare and support, they also expressed difficulty in finding alternative forms of support that they might organise independently. During the interviews, only a small number of participants described actively engaging in independent research on health solutions or care practices. A commonly expressed view by participants was that they assumed healthcare professionals would inform them about any available choices or care practices, should they exist.
To understand the barriers in accessing non-clinical health support, it is crucial to acknowledge that many participants perceived their health difficulties as lacking a clear path to resolution. They faced challenges in finding appropriate solutions or guidance for their specific concerns. This was especially true for challenges or concerns that did not appear to neatly fall within the scope of NHS care, but still required some degree of medical involvement. Participants cited challenges such as making adjustments to their clothing, diet, transportation needs, or modifying their living space to accommodate their health or disability needs.
So at the moment I can drive, but will this be the case in the future?
(PIP claimant, degenerative disc disease)
The arthritis in my ankles is getting worse and I wonder if I could be better wearing different shoes.
(UC claimant, arthritis and back pain)
Case study 9: Meet Sam. Sam claims UC and lives alone. Sam struggles with a heart condition and arthritis. She receives care from the NHS at arm’s length: scheduling appointments is down to her. Sam would like to make her home more accessible and ergonomic, but she is unsure who to speak to for advice. Although home improvements do not seem like an NHS issue, Sam is uncertain about what accessibility needs she will require in the future and feels it would be risky to make changes without some medical expertise. She finds it impossible to get a doctor’s appointment, so she just leaves it.
Participants’ challenges in identifying health support options beyond the NHS highlight the potential benefits of providing claimants with signposting information about general health resources and support organisations. Additionally, offering guidance on when to proactively contact the NHS, particularly in relation to lifestyle changes or everyday care practices, may be beneficial for claimants (notwithstanding the potential tensions and pressures this might cause, as stated above).
3.4 Third sector organisations provide important support
Third sector organisations and charities clearly play a crucial role in supporting participants in managing their health. Citizens Advice (mentioned most commonly), Mind, UK COPD, The Trussell Trust, and local grassroots charities aimed at supporting local residents are just some examples of organisations that participants mentioned accessing regularly.
Participants described how charities and third sector organisations provide help both with the emotional and administrative aspects of health management, making the care feel person-centred and comprehensive. Tasks which participants described charities assisting them with included administrative tasks such as form-filling or complaint writing, signposting to local support groups or alternative care practices, providing guidance on accessing extra funding to support health needs such as PIP or NS ESA, and sharing contextual information about others in similar positions.
However, the participants spoken to differed considerably in both their awareness of these organisations and their confidence in contacting them. Based on the participants’ descriptions of their interactions with these services, the research team has deduced that this is primarily influenced by claimants’ social networks and the extent to which they engage with other services that play a role in providing guidance and referrals. Participants who had been in contact with support organisations tended to become aware of them and/or received encouragement to reach out to them through others in their network or through support workers, such as housing officers or social workers. Conversely, individuals who had fewer social connections, were socially isolated, or had limited engagement with services beyond their immediate health needs appeared to be less aware of and actively accessing these kinds of resources. For those who struggled with social interaction due to conditions such as anxiety or mental health disorders, seeking this kind of support required extra encouragement. For instance, one participant with severe anxiety shared an example of how she required her sister’s presence to dial the phone number of Citizens Advice and gather the confidence to speak to them.
Of all the individuals spoken to in this research, participants claiming PIP were most vocal about their dependence on support from third sector organisations. Many shared their experiences of living with long-term and chronic conditions, which had brought about significant changes in various aspects of their lives. Participants were drawn to the support provided by these organisations because of their ability to assist with various aspects of their lives. Because PIP claimants do not receive interpersonal support during their claim, such as access to a Work Coach, they have fewer personal interactions through which to ask for advice or guidance. Without third party support, the experience of applying for benefits can therefore feel overwhelming and lead to feelings of isolation for this group.
At one point I even thought about going into the Jobcentre [Plus] to speak to someone there because I had no idea what I was doing and there really wasn’t anyone to talk to. The whole process [of applying for PIP] felt stressful. I felt very alone.
(PIP claimant, anxiety and ADHD)
Third party support is clearly playing a critical role for those claimants accessing it. Yet awareness and access were quite variable among the participants spoken to through the research. This suggests a valuable role could be played in signposting claimants (particularly PIP) to local organisations from the outset of their claims journey. This is likely to be especially valuable for those more isolated individuals.
3.5 Summing up
In this chapter, the report has examined the factors influencing the availability and accessibility of health support for claimants, as well as the factors shaping these interactions. It has found the following:
- there is a clear association between effective care management and strong support networks. As a result, extra support should be considered for those claimants with poorer support networks or who may be experiencing isolation
- some claimants are clearly facing challenges in accessing NHS care, which will be critical to understand from a health support signposting point of view (particularly in terms of the types of NHS services or support claimants might be directed to)
- participants’ challenges in identifying health support options beyond the NHS highlight the potential benefits of providing claimants with signposting information about general health resources and support organisations, for example, locally available free talking therapies
- in particular, the research has illustrated the contribution that third party organisations such as charities can play in supporting claimants, suggesting the valuable role health support could play in signposting them (particularly PIP claimants) to local organisations from the outset of their claims journey
4. How health support intersects with claiming benefits
This chapter explores the relationship between accessing health support and a claimant’s benefit journey. How the two interact is relevant to thinking about how signposting to health support might be delivered. The research has highlighted that claimants find touchpoints in conversational settings to be particularly positive, and as such offer potential moments where signposting to health support could be well targeted and received. By attempting to understand more about participants’ experiences of the claims process it is apparent that elements of the journey itself can exacerbate poor health. Negative experiences related to the application and assessment processes in particular, have the potential to significantly influence claimants’ relationship with DWP and their trust in any health support signposting offered.
4.1 Claimants struggle to pinpoint specific moments in their DWP journey
When asked to reflect on their DWP claims journey, many participants found this challenging. It was common for participants to struggle to visualise a clear journey, or to recall the specific sequence of events they had encountered. As such, it has been challenging through the research to explore the relationship between the claim journey and accessing health support.
To be honest I find it difficult to answer this question [of what if any health support would have helped]. It’s a hard thing to get my head round and to describe.
(UC Health Journey claimant, chronic back pain)
Participants identified several factors that contributed to this challenge. One group of participants attributed their difficulty in visualising the system to the challenges they faced in dealing with a complex or deteriorating health condition. It was felt that experiences of disorientation and distress during their claims process could make it difficult to understand and recall their journeys accurately. For example, one participant recounted how stress connected to a period of ill health had resulted in memory problems around the time of her application. Participants who described memory challenges connected to their disability and/or health conditions included those with Parkinson’s disease, anxiety disorders, schizophrenia, learning disabilities, and participants with alcohol dependency.
Everything at the time was a blur. I remember talking to a woman at the Jobcentre [Plus] and then there was an interview but that’s it. Everything has gone from my mind.
(UC Health Journey claimant, ADHD)
Other participants attributed these difficulties to a lack of knowledge about the benefits system at the time of their application. This limited understanding led to confusion and uncertainty during the process. For instance, one claimant shared her experience of applying for one benefit, only to be redirected to another by the system, causing confusion about which aspects of the process belonged to which benefit. Research participants who understood the system better tended to be receiving support via third party organisations.
After I applied I don’t know what happened next. I was just waiting and seeing what they would say. I don’t really know what was going on.
(PIP claimant, heart and kidney failure)
The whole process was very confusing! Initially I was told I should apply for PIP and then the next person I spoke to said, ‘Well because you get sick pay from work, it’s ESA you need.’ But then it turned out that was wrong, but the form I was given was actually for PIP anyway.
(PIP claimant, macular dystrophy and glaucoma)
However, for participants receiving help with the application process, from friends and family or third parties such as Citizens Advice, this could also mean they felt removed from the process, making it challenging for them to articulate the elements of their journey.
My husband was a godsend and helped with everything. Because of how sick I was at the time I had to be quite hands-off. He took over the online application for me as well because I’m not so good with computers.
(UC Health Journey claimant, schizophrenia)
Conversely, participants who spoke more positively about their overall claims journey experience tended to have a clearer understanding of the process. This included understanding roles and responsibilities between claimants and DWP, feeling more confident about their eligibility and what information was needed to support their claim, and feeling informed about how to obtain necessary documentation, such as fit notes, and the proper submission procedures.
For those who described positive experiences, they may have also had previous experience with the benefits system or had family members who had gone through the process, which gave them a better understanding. Others emphasised that they received valuable support and guidance from third party organisations who specialised in assisting individuals with the application process, or more general support from organisations such as Citizens Advice.
Participants in the research faced challenges in comprehending and navigating their benefits journey for a variety of reasons. This makes pinpointing where signposting to health support might be best placed difficult. However, through further exploration the researchers have been able to infer where support may be more effectively received, as described below in section 4.2.
The difficulty claimants face in visualizing and comprehending their journey implies that improved communication and education regarding what to expect from the process might alleviate some of the stress reported by claimants during the claims process. Certainly, the research has found that those with a better grasp of the process tended to report a more positive experience.
4.2 Positive ‘touchpoints’ could be used to deliver effective support
Many participants had difficulty understanding their journey and how it would affect their interaction with DWP health support. However, the research has revealed several positive associations with the claims journey which may be useful to thinking about the optimal timing for targeted support.
One major focus was on frontline staff, who were clearly valued by the participants we spoke to – as one NS ESA claimant put it, “real people.” Participants generally spoke positively about frontline staff when discussing them. However, it is important to acknowledge that there was some variation in these perceptions. While the majority of interviewees expressed positive experiences, some mentioned encountering less positive interactions. For instance, some mentioned frontline staff who were clearly time pressured and less attentive, while others highlighted personality differences as contributing factors.
Participants who spoke highly of frontline staff really valued these forms of interactions. They described a feeling of empathy and valued the opportunity to establish a personal connection which helped to ensure their needs were understood. Specifically, for NS ESA and UC Health Journey claimants this comes from their Work Coach. These participants found conversations with their Work Coaches beneficial as they offered a chance to share their story, describe the impact of their condition on their lives and discuss the challenges they were facing. The conversational setting facilitated question-and-answer exchanges and offered more personalised advice and solutions tailored to their specific health needs.
The ladies [at the Jobcentre] were wonderful, and you really got the sense that they cared. One even offered to attend a job fair on my behalf as she could tell it would be too much for me.
(UC Health Journey and PIP claimant, fibromyalgia)
The researchers also heard about positive experiences with Disability Employment Advisers from NS ESA claimants. One participant in this group described how advisers took the time to get to know them and their condition. What is more difficult to discern is the extent to which these positive associations with the journey are down to the system or the individual adviser and how they apply their role.
During the application process I really felt I had a supporter in my corner. She is the reason I completed [the application]. One day she phoned me to follow-up on a conversation we’d had and asked how I was doing. When I told her I was struggling with the form, she did it with me on the phone, right there and then.
(NS ESA claimant, chronic fatigue)
The positive sentiment associated with face-to-face contact – empathy, trust, patience – suggests that ‘touchpoints’ involving frontline staff could offer a way through which to channel signposting to health support. DWP Work Coaches in particular, are clearly highly valued and may be well placed to carry out health-related discussions. For claimant journeys that do not currently contain interpersonal touchpoints (such as PIP), there may be value in introducing these styles of interaction for those who wish to access it.
4.3 Offering health support feels at odds with those exiting the journey
It is important to also recognise that some people will not be successful in their claims application. A small number of participants we spoke to spontaneously mentioned they felt that ‘refusing’ to financially support an individual, yet providing health information, which by implication acknowledges they have health needs, feels confusing.
It’s all well and good if you’re successful but I was initially turned down for PIP and it would have felt like a kick in the face.
(PIP claimant, degenerative disc disease)
As the Department determines eligibility based on a functional assessment and not on the basis of having a disability and/or health conditions, someone may be found not eligible for a health-related benefit whilst also being in a position where health support would be beneficial. It is important that any signposting to health support for people in this position is managed carefully to avoid distress and protect the reputation of DWP.
4.4 Aspects of the claims journey can impact claimant health
Whilst some participants reported broadly positive experiences with the claims journey, it was common to hear examples of where the process had proved challenging for participants. This was not universal across the claims journey, though appeared particularly relevant to the application and assessment aspects of it, and in respect of how claimants came to understand their eligibility for benefits.
It is worth noting that during interviews, participants who faced challenges with the system often focused on discussing enhancements to the claims process when asked about potential health support and guidance within the benefits journey. They felt that if DWP wanted to promote health improvement then this was not just about health signposting; it could also involve tweaks to the claims process itself, with the aim of making their lives simpler and less stressful.
With regards to eligibility, it became evident through discussions that many claimants reported learning of their potential entitlement to benefit by chance, either through word of mouth from family, friends, or local networks. This was particularly evident among UC claimants, as several of them mentioned being encouraged to apply by individuals in their network who had either experienced unemployment or had specific health support needs.
Both NS ESA and PIP participants commonly reported learning about potential benefits they might be eligible for through more focused guidance from Jobcentre Plus staff (who often responded to general inquiries about benefits) and third sector organisations such as Citizens Advice. However, participants who were experiencing social anxiety, mental health difficulties, or mobility issues found connecting to support organisations for help in this regard more challenging.
The application process itself was highlighted as lengthy and complex. This posed significant challenges, particularly for participants experiencing fatigue, poor mental health, memory difficulties, and learning disabilities. They described completing the form as physically and mentally exhausting, which for some led to heightened anxiety and, in some cases, had triggered periods of ill health.
Case study 10: Meet Caroline. She suffers from severe arthritis and chronic fatigue, which significantly impacts her writing ability, energy levels, and ability to focus. She recently discovered she was granted PIP on her second application for the benefit. In her earlier attempt, Caroline had been initially turned down due to insufficient evidence showing the impact of her condition on her daily life. She attributes these challenges to the overwhelming amount of information she felt she was expected to submit. Specifically, she found the PIP form to be excessively long, taking her days to complete. The experience of being denied support despite the profound difficulties she faced had a severe impact on Caroline’s mental health at the time. She felt disheartened and frustrated by the initial rejection, as it failed to acknowledge the extent of her struggles. She strongly feels the claimant process needs to be adjusted to better reflect the needs of people like her, that struggle with completing forms, especially if they do not have anyone in their life to help.
When it came to the assessment process, the researchers heard from participants with mobility challenges as well as anxiety who explained they found the requirement to attend face-to-face interviews distressing. While assessment processes are intended to consider whether claimants require a remote option, it became apparent that not all participants felt that their needs had been taken into account during this process. In fact, the researchers encountered a handful of instances where participants explained that they had been denied the opportunity for a remote assessment despite their expressed need for it. They reported how the stress of attending in person could set back their wellbeing for days, leading to periods of depression and low mood.
My anxiety was through the roof days before. I couldn’t sleep. That morning I was in so much pain I had to fork out for a taxi. I kept thinking ‘why do I need to do this?’. It’s all on the doctor’s note. Is it because they don’t believe me?
(PIP claimant, anxiety and depression)
It is important that efforts aimed at enhancing claimants’ health should not solely concentrate on health support signposting. Components of the claims journey that may unintentionally have a negative impact on claimants’ wellbeing may also wish to be addressed. This research has found that elements of the application process itself may be exacerbating some people’s health conditions. It also sets the tone for a claimant’s relationship with DWP, including their expectations around understanding, empathy, and trust. This is likely to impact how receptive or otherwise claimants might be to receiving health support and signposting in the future.
4.5 Claimants apply for benefits primarily for financial stability
One of the ultimate benefits of providing health support to claimants is to improve their health management so that those who are able may eventually move closer to the labour market or stay in work for longer. So, it is important to reflect on where, at the time of making a claim, participants in this research were focused in terms of their motivations for applying for benefits.
Participants commonly described undergoing periods of significant upheaval in their lives. Changes to their health caused some to have substantially increased expenses and outgoings. This made financial security – as opposed to other drivers, such as getting (back) into employment – the main motivator for applying for benefits. This view was expressed across all benefit types. The researchers did encounter a few instances where individuals were motivated to apply for benefits as a passport to other forms of support. For instance, to obtain blue disability badge to make parking easier.
You’re applying for benefits because your life is falling apart. You’re struggling and need help. It’s not time to find a new job, but maybe later down the line when things are a bit clearer. I’d be okay to have a conversation [about health support] if it’s based on a genuine understanding of your health.
(UC Health Journey claimant, rheumatoid arthritis)
This is not to say that claimants were not motivated to move (back) into employment or were not thinking about getting back into work at some point in time. There were instances where participants demonstrated a strong attachment to work. For example, the researchers encountered individuals claiming PIP and NS ESA who strongly wished to remain in the workforce via reduced hours. Some described a strong attachment to their work, finding deep fulfilment in their professional roles. Others – a view commonly expressed amongst younger participants – explained they were still in the process of building their careers and so wished to remain actively engaged in work for the future. For others, their ill health was unexpected, such as following an accident or a recent diagnosis, and not something they had factored into their career plans. As a result, they sought workplace adjustments like altered hours or working patterns rather than leaving the labour market altogether. By opting for reduced working hours, these individuals hoped to strike a balance between addressing their health needs and fulfilling their work commitments.
For unemployed NS ESA claimants, whilst there was an expectation that they may need to return to work in the future, if possible, this was causing anxiety for some about what might happen to them when financial support stops – would they be expected to find a job when they might not be fit to?
I’m not sure how long I get the help for, but I know that it doesn’t last forever, so either I need to get better or be moved on to something else.
(NS ESA claimant, shoulder pain)
While improvements in their health management may eventually help some claimants move towards employment, it is important to understand that it is financial stability that is front of mind for claimants when seeking benefits. This finding is important to consider in terms of when health support is offered during the journey and how it is framed and promoted to claimants.
4.6 Summing up
In this chapter, the report has explored the relationship between accessing health support and a claimant’s benefit journey. How the two interact is important to understanding the ways in which signposting to health support might be offered. It has found the following:
Since many participants struggled to comprehend a clear claims ‘journey’ this makes pinpointing where signposting to health support might be best placed difficult. The positive sentiment associated with face-to-face touchpoints and experiences with frontline staff make conversational settings a clear route through which health support and signposting could be explored.
- further, improved communication and education about what claimants can expect from the process might also help to address some of the challenges and pressures described by claimants during their journey
- care should be taken in how health support is offered to claimants who are not found to be eligible for benefits. Offers of support to this group, whilst potentially still helpful, may cause distress or damage to DWP’s reputation
- it is clear from the research that elements of the claims process can cause challenges for claimants, which can have an impact on their health. It is important that approaches designed to improve the health of claimants are not solely limited to health support signposting. Support could also extend to elements of the claims journey which may be inadvertently impacting claimants’ health in a negative way too; namely the application process and the assessment itself. It is important to note that work on this issue is already underway as part of the Health Transformation Programme
- the emphasis participants place on attaining financial stability when applying for benefits should be borne in mind when thinking about how to frame and present health support signposting to claimants during their journey
5. Claimant views on receiving health support from DWP
This final chapter examines whether claimants want and trust DWP to connect them with health support, and what form of support would be most valuable. The research has found genuine appetite for this among claimants. Whilst trust does not appear to be an issue, support needs to feel tailored and suitable to individuals’ circumstances and health needs, including around accessibility. This points to a range of different solutions being offered, from light-touch ‘self-serve’ support to more ‘high-involvement’ support for particularly vulnerable claimants.
5.1 Claimants are open to DWP health support and signposting
During the research, participants were asked directly whether they would welcome health support and signposting from DWP. The response was overwhelmingly positive. Virtually all claimants interviewed expressed openness to being offered health support and signposting by DWP as part of the claims journey, and this was regardless of which benefit they were claiming. Only two participants actively expressed disinterest in receiving support, which was primarily driven by general preference for independent management of their health – a point spoken to in section 2.1.
Participants described how having more support options to choose from can only be a ‘good thing’ even if they might decide not to take it up. They ultimately want to improve their health and day-to-day wellbeing making relevant advice from any reputable source, including DWP, welcome. No participants who discussed the issue of additional health support with the research team described receiving all the help they needed to manage their condition – there is clearly a gap to fill. Participants without strong support networks described finding the idea of proactive support particularly appealing.
Yes, I would be open to that; more information and choice is always good isn’t it.
(PIP claimant, anxiety and depression)
I think it would be a good idea. It would be nice to have things suggested. It’s not like I have all the answers today and there must be more things out there I haven’t tried.
(UC Health Journey claimant, spondylosis)
The notion that claimants might not ‘trust’ DWP to offer health support and signposting has been firmly challenged by this research. There was little evidence of participants questioning DWP’s motivations for supporting them with their health (e.g. as a way of getting them off benefits and back into work), whether spontaneously or when probed. DWP’s intentions in offering health support and signposting were seen to be good ones. Those participants expanding on the question of trust during interviews tended to accept that DWP has a responsibility to get those that are able to back into employment and understood its motivation in that light, but this did not come from a point of view of mistrust.
It was commonly acknowledged that DWP could provide a valuable perspective in health matters – they already offer financial support to individuals with disabilities and/or health conditions, which participants saw as giving the Department insight into various care solutions used by others in similar circumstances. But, they felt there needed to be a balance struck: ultimately participants did not consider DWP to be a health ‘expert’. Health support and signposting needs to be designed accordingly.
Obviously, they want people to be as well as they can be. They might not be experts, but they might have access to experts. I don’t see how it [health support] couldn’t be helpful.
(UC Health Journey claimant, chronic back pain)
I think it makes sense as they want people to be well and they do have doctors working with them as part of the process.
(NS ESA claimant, heart condition and depression)
Whilst a less common theme, it is important to note that there were participants who made spontaneous links between support from DWP that was ‘financial’ (since it was coming from a department which focuses on providing financial support) versus support that was ‘clinical’ and specific to a health support need. To illustrate, there were cases where participants thought health support meant being given money to pay for additional healthcare, such as private treatment or health classes. This suggests expectation management and clarity around the health support ‘offer’ will be important to convey (including the types of support not going to be offered).
Yes, it sounds good. If they will give me extra money to help me with my health, I am not going to say no!
(UC Health Journey claimant, glaucoma)
Additionally, it is relevant to factor in how some participants might receive the offer of support. This is especially the case for those claimants who have found the claims process challenging or distressing (as discussed in chapter 4. For those participants who described experiencing a challenging application process, for example, there was more skepticism about the offer of health support and signposting. This group wanted DWP to focus on ensuring claimants would feel better supported through the claims process itself. They suggested that if DWP truly wants to improve wellbeing, it should focus on improving its own processes first.
I’m not going to say no to extra help, but it does seem backwards when there was so much stress at the beginning. I think the design of the [application] form could be looked at first.
(PIP claimant, osteoarthritis)
For these participants (who were primarily participants with poor mental health, learning disabilities, or with weaker support networks) their feeling was that a valuable form of health ‘support’ could be to adapt the application form, so it was shorter and introduce a more person-centred application process. This would entail tailoring the processes to better accommodate the needs of the applicant, taking into account their specific health circumstances.
The research findings should offer confidence to DWP in offering health support and signposting to claimants going forward. Trust, including around motivations for offering support, does not appear to be an issue. There is also a clear demand from claimants – of the participants spoken to it was clear there were very few who felt they were receiving all the support that could be of help. However, the support offer needs to be clear on the types of support available – for example, managing expectations regarding financial support for some individuals. There is a view to be taken about the extent to which health support also extends to the claims process itself.
5.2 Claimants want tailored and personalised support where possible
The participants interviewed found it hard to imagine or articulate the range of support options that DWP might offer. Since DWP is not considered a specialist in healthcare or disability support, participants with more formed views tended to default to the assumption that the support on offer would most likely be information-based.
Opinions were mixed about what this information could look like. Participants the researchers spoke to, who captured a broad range of disabilities and health conditions, saw ‘off-the-shelf’ or ‘textbook’ advice as less helpful. Given the complexity of their needs they considered that this could pose a potential risk to their health, as discussed in section 2.2. They want information that would be clearly connected to their individual health needs and the context in which they managed their health. This view was felt particularly strongly by those with serious mental health conditions or who had conditions which required careful conservation of energy levels.
Some examples of the types of support participants suggested here included:
- targeted health support ideas based on the claimants’ individual capabilities and varying abilities
- expert advice specifically tailored to help manage their exact symptoms
- crowdsourced ideas on condition management from others who have experienced similar conditions
- contact information for specialists with whom they could discuss their individual conditions and needs
It can be really difficult to find information which you know is relevant to your specific circumstances and everything that’s going on in your life, so I would definitely be interested.
(UC Health Journey claimant, angina)
The findings show that claimants would be open to receiving information-based health support and signposting but are likely to be more receptive if they know that it is genuinely tailored to their individual needs. Adopting a more personalised approach is therefore likely to increase the perceived value of future health support and build trust in the overall approach.
5.3 Claimants are open to use of existing health data
In offering support, a common reflection from participants was that this should not result in extra mandatory assessment stages to the current process or increasing the complexity of the application. There was a view that DWP should make full use of the existing data it collects on claimants. Among the participants who engaged in discussions on this matter, none of them expressed concerns regarding the use of their data in this manner. In fact, these participants viewed it as a positive development. It is important to note that not all participants discussed this specific topic with the researchers, indicating that there may be additional nuances they have not been able to fully address.
You provide so much information … as part of assessment process already [fit notes, information about your day-to-day life], can they do something with this?
(NS ESA claimant, irritable bowel syndrome)
In this scenario, participants expected that whoever reviews and interprets their information has sufficient medical expertise to understand their condition, ensuring any health signposting recommended to them is safe and appropriate.
Are these ideas going to be developed with medical experts then?
(PIP claimant, thrombosis)
Collection of additional claimant data to inform individual health support and signposting needs to be carefully considered in terms of the additional burden it could place on claimants, some of whom already find the claims process overwhelming. Maximising utility from information already collected from claimants could be one way to address this, assuming it is done by suitably qualified staff.
5.4 There is no one size fits all – support needs are a spectrum
The researchers heard participants describe a broad range of health support which they might find of benefit. The type of support participants prioritised was very much driven by the nature of their disability and/or health conditions and how their symptoms affected their daily life. However, the research team heard a number of other factors come into play, including the quality of a participant’s living conditions (i.e. housing or the built environment), the level of care they required, or an individuals’ own unique strengths and capabilities. For example, one claimant with a condition impacting their mobility, stressed a preference for health support ideas which accommodated their ability to travel short distances independently. Other considerations included the quality of a claimant’s support network, the extent to which they could manage their health independently, and broader life challenges such as caring responsibilities.
This has led the research team to deduce that health support and signposting for claimants needs to fall within a wide-ranging spectrum: from ‘self-serve’ support that individuals can independently organise, to more ‘high involvement’ support that requires more active and hands-on involvement. The latter typically may involve collaboration with a third party. The researchers heard a range of examples of what types of support might fall within this spectrum from participants, which is summarised in Figure 2.
Figure 2 Claimant generated health support ideas
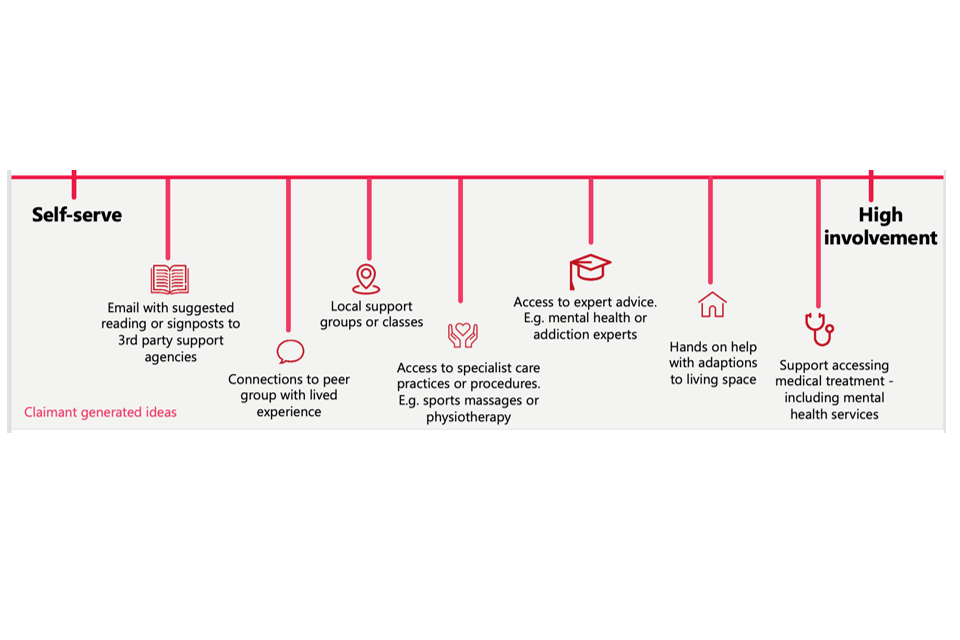
Those participants with more stable and manageable health conditions, who had good access to medical services and/or a strong support network tended to navigate more towards a ‘self-serve’ model. They typically exhibited the highest levels of independent self-care, meaning they were confident being able to seek out support themselves or get help from others from their network to do so.
Yeah, I’d be happy to sign-up to something [a class] if it was relevant to me. My husband could even drive me there!
(UC Health Journey claimant, diabetes)
For these participants, signposting via email or booklet would work well. These materials could provide recommendations for self-care practices they might not be aware of, or organisations to contact with a specialist in their health area, such as local support charities they could contact.
If you could put something down on email for me which set out things, I could try out based on my circumstance, I would definitely take a look.
(UC Health Journey claimant, cardiovascular disease)
Engagement in broader group settings, such as support groups, elicited varied responses among participants. For individuals who felt more at ease in social situations, the idea of being directed to local face-to-face support groups or health-focused classes was appealing. They saw these groups as a valuable opportunity to interact with others in a structured environment and learn support techniques from peers. However, participants with anxiety or agoraphobia expressed a strong aversion to face-to-face health support. Even in online settings, those with the most severe symptoms felt uncomfortable speaking to strangers. Participants who were socially confident, but who faced mobility and transportation challenges also wanted the option of accessing this type of support online.
I think you can learn so much from others and their experiences so if there were high quality local groups where I could meet people… I’d try.
(UC Health Journey and PIP claimant, bladder cancer)
As mentioned earlier in this report, many participants described experiencing challenges in accessing NHS care. These individuals spoke of the value they would find from facilitated access to medically trained specialists to improve their circumstances, such as advice on lifestyle changes or topics of care they may wish to discuss with their doctor.
I’m currently on the waiting list for physio, but if there was a phoneline you could call where I could ask questions and get some advice [from a medical professional] on how to make some basic changes in the meantime, that would be really valuable.
(NS ESA claimant, chronic back pain)
In contrast, those who found managing their disability and/or health conditions more difficult, or who had more complex health needs, are likely to need more ‘high-involvement’ solutions. For these claimants, there is a need for more intensive guidance to help them make changes. A common sentiment among this group was that they felt they lacked the energy to do this themselves and would find it difficult contacting relevant services or support without help.
The types of support mentioned here were varied, reflecting the range of individual circumstances participants were living with. Nor did they reflect any specific benefit type. For example, participants with poor mental health or addiction issues would welcome a direct connection to specialist services in these areas. Participants struggling with unsuitable housing would benefit from support in making alterations to their living space. Meanwhile, participants with the most complex and severe medical challenges, which are not being well managed, saw expert NHS support as a priority. In this instance, participants felt that any support DWP could provide to expedite or support them in getting access to necessary clinical care and/or medical experts would be highly valued.
I’ve tried therapy so many times, but it’s not worked, it’s not done anything. I’m on the waiting list to see a specialist psychiatrist. Could anything be done to speed that up?
(UC Health Journey claimant, anxiety and depression)
Case study 11: Meet Sue. Sue struggles with a degenerative lung condition that makes it difficult for her to breathe. As a carer for her disabled husband, she finds it hard to rest and often gets lung infections. She is not comfortable with technology, but she has a strong bond with her son, who helps her with her appointments and takes her out shopping. She expressed a desire for additional assistance at home to support her in caring for her husband, as it would enable her to prioritise her own health. Apart from Adult Social Care, she is unaware of any other organisations that could potentially offer help. She would greatly appreciate information about any relevant resources or services that DWP may be aware of.
Effective health support must also actively consider accessibility and inclusion needs. During this research (and as mentioned throughout this report), participants described experiencing a variety of challenges that impacted their approach to health management and ability to access relevant care. Participants for whom English was not their first language encountered challenges in accessing support materials in their mother tongue and communicating with medical staff. Individuals with intellectual and learning disabilities, as well as those with low literacy skills or limited access to computers and data, found it more difficult to research their health conditions. Additionally, participants with limited mobility or mental health conditions such as anxiety faced difficulties leaving their homes or interacting with strangers, which restricted their access to support. If they are to successfully take up future support, DWP needs to be mindful of claimants’ different abilities in accessing and engaging with information.
I don’t have a smart phone so there’s no point sending me stuff to look at on the internet.
(UC Health Journey claimant, heart condition)
As noted from the outset, the range and often complex nature of claimants’ disabilities and/or health conditions makes a one-size-fits-all approach to health support and signposting inappropriate. Lower intensity ‘self-serve’ style signposting will be appropriate for some claimants, but more tailored and intensive support will be needed for those with more acute needs. It is important that accessibility and inclusion needs are actively considered.
5.5 Delivering health support in conversational settings is valued
Overwhelmingly, participants advocated for a less transactional and more conversational approach to health support, both in the identification of need and in delivery of health support. They described how they would value the opportunity to explain their individual situation, needs, and preferences, and to have these considered by DWP in the design of any health support or signposting. Conversations were also expected to provide the ability to ask questions and ensure that the information provided was clearly understood and so could be acted upon quickly. The Work Coaches who came in for the most praise from participants were those already felt to be providing this type of support to claimants, whether by design or not. This makes them a good route through which to offer health support, as set out in chapter 4.
I feel really strongly that this sort of thing [discussing health needs and agreeing support options] should be done as a conversation so I can explain myself and what the challenges are.
(NS ESA claimant, HIV)
To really trust whatever they are telling you, you want to check it’s relevant to you and your experience.
(PIP claimant, liver disease)
However, for a handful of participants the notion of support conversations taking place face-to-face was uncomfortable. For some, this was because they struggled with verbal communication or were dealing with anxiety and depression. For others, they did not like the idea of discussing highly personal matters in a public setting like a Jobcentre Plus office. Some of these participants would be comfortable with a phone conversation instead, whilst others expressed a preference for communicating with DWP through less personal means, such as email.
The strong preference expressed by participants for the use of conversational settings to deliver support suggests that stages involving interpersonal interactions in the claimant journey could offer a suitable route for some claimants, though it will be important to be considerate of alternative options for those less comfortable in such face-to-face settings.
5.6 Claimants were unclear about the appropriate timing of support
Claimants in the main struggled to visualise their claims journey in a linear way (see section 4.1), making it challenging to connect support ideas to an ideal moment in their journey. Based on this, the most common view amongst participants in this research is that they did not have a strong preference about when DWP might engage them in a support conversation. Those participants who lacked a good support network were more likely to recognise the benefit of support and signposting coming earlier in their journey. Participants with less pressing needs and stronger support networks were more relaxed.
I’d be happy with anything but, soon as possible is best as obviously I’m looking to be as well as I can be. Whatever they information they could give me would be fantastic.
(UC claimant, depression)
It’s already quite a complicated system if you think about it, so having this conversation at a quiet point, when there’s less going on might make sense.
(PIP claimant, heart condition)
This finding reinforces the notion that a uniform approach to the timing of support delivery may not be suitable for everyone and should instead be tailored to the individual’s specific needs, which could be determined through an initial assessment. It will be important to not inadvertently overwhelm claimants with information depending on where they are on their claims journey.
5.7 Key principles to promoting engagement with health support and signposting
Finally, participants were asked to share their thoughts on what constituted effective health support and guidance from DWP and how the Department might best promote engagement and participation. Their views can be summarised into four key principles that should be borne in mind when designing health support and signposting going forward.
Support must feel personal
Participants once again reiterated that it was crucial the options presented to them were based on a thorough understanding of their disability and/or health conditions, symptoms, and personal circumstances. This included accounting for lifestyle needs and preferences, such as implications for any caring responsibilities they may have or the practicalities of being able to travel to receive health support. Support which was not grounded in a proper understanding of their unique situation was seen as risky.
Support must have no strings attached
Linked to this, participants should get a choice over whether to accept health support or not. Taking up support needs to be seen as entirely voluntary, which should be made clear upfront. In particular, it should be emphasised that taking up health support would not be part of any benefit conditionality, now or in the future.
The one thing I’d say is that it must not feel pressured. There are certain things I know won’t work for me and things I’d never do. It’s my body at the end of the day.
(UC Health Journey claimant, fibromyalgia)
Support must account for varied skills levels and cognitive abilities
Claimants should have choice not only in terms of the support being recommended, but also in how that support is accessed and delivered. For instance, participants with anxiety felt face-to-face support would be unsuitable, whilst individuals with poor literacy would prefer verbal information. Given the vulnerability of some participants, it should not be assumed that providing basic information or signposting to all will be sufficient for them to engage in health support without assistance.
Support information may need to be shared with others in their support network
While not all participants had a strong support network, some who did, wanted health information to be shared with others as well as themselves. They believed that involving friends and family would help ensure the information was retained and acted upon effectively. This was particularly emphasised by claimants with conditions like Alzheimer’s or ADHD, who described difficulties in processing and remembering information.
5.8 Summing up
In this chapter, the report has explored whether claimants want and trust DWP to signpost health support, and what form of support would be most valuable. It has found the following:
- there is a clear potential role for offering health support and signposting to claimants going forward. Trust, including around motivations for offering support, does not appear to be an issue. Few participants currently feel they are receiving all the health support they could be, and they are interested in more information
- claimants are likely to be more receptive to receiving information-based health support and signposting where it is felt to be genuinely tailored to their individual needs. Maximising utility from information already collected from claimants to inform this would be one route to consider in reducing the burden on the claimants themselves
- a one-size-fits-all approach to health support and signposting feels inappropriate given what has been learnt about this audience. Lower intensity ‘self-serve’ style signposting will be appropriate for some claimants, but more tailored and intensive support will be needed for those with more acute needs. Accessibility and inclusion needs also need to be actively considered
- any health support signposting needs to account for potential concerns raised by individuals in order to build trust in and acceptance of the policy. This includes offering support that feels personalised, is accessible, and is completely voluntary in nature
6. Conclusions and recommendations
This research has sought to identify where DWP can offer timely and targeted health related support as part of the Health Transformation Programme. Specifically, the research has aimed to understand what role the Department could play in helping disability-related benefit claimants access health support going forwards. Through in-depth interviews with 76 claimants and appointees, the research has been able to offer a number of specific reflections and recommendations on what health support for people claiming disability-related benefits could look like.
1. Through this research it has been challenging to draw out distinctions between benefit types – there has been significant consistency in terms of experiences, though where clear differences existed these have been drawn out. Therefore, whilst the research approach was designed to see if and how views and experiences differed according to the type of benefit individuals were claiming, it has actually found that health support needs are not as distinctive between PIP, NS ESA, and UC Health Journey claimants as may have at first been thought.
2. The research clearly shows that there is genuine appetite amongst claimants for further support in managing their health. There is a potential role for DWP to play here, though it should be noted that participants did not regard DWP as health ‘experts’, so signposting and support needs to be understood in this context. There was little to suggest that claimants would mistrust or question the motivations of DWP in signposting them to health support, which is encouraging. In fact, many claimants would highly welcome the support.
3. The research demonstrates that claimants’ health conditions and/or disabilities are both diverse and complex, and are highly personal to the individual. This makes simple ‘off the shelf’ or generalised support and signposting inappropriate. Indeed, it also implies a risk to both individuals and DWP. For individuals: in being assigned the wrong kind of support or being signposted to support that they might not be able to access, especially where stretched NHS services may be involved. For DWP: in terms of reputation and trust, should the support offered not be right for the claimant.
4. Through the research, four key principles have been identified that should be considered when implementing any health support programme. These should be laid out to claimants from the outset to build confidence and trust in the offer:
- support must feel personal to the individual health and personal circumstances of claimants. Accordingly, design and delivery of health support should consider the extent to which specialists need to be engaged in the process, especially for those with more complex needs.
- support must have no strings attached – it should be entered into voluntarily and not be seen to have any sway over an individual’s benefit claim
- support must account for the varied skill levels and cognitive abilities of claimants
- support information may need to be shared with others in a claimants’ support network
5. The research has also uncovered more about the types of health support that claimants are looking for. It has identified appetite for a range of possible health support that extends beyond that aligned to claimants’ original disability and/or health conditions. For example, a clear area of need that has emerged from the project relates to mental health. For some it has the potential to become the condition with the biggest impact on that individual’s life if left unaddressed, though may not always be flagged when making an initial claim. This is probably the health issue that participants had most in common and is potentially the biggest unmet health support need for this group. The research also suggests that support in managing broader life challenges (e.g., housing) and in navigating the claims journey itself would also be welcome.
Health support needs can best be summarised as falling within a spectrum: from ‘self-serve’ to ‘high involvement’. Self-serve is likely to be better for those with more stable health conditions as well as those who find their disability and/or health conditions easier to manage. This could include signposting to local support groups or health-focused classes. ‘High involvement’ is suited to those requiring more active and hands-on involvement in their health management, such as signposting to specialist services or support in making lifestyle changes. It will also be crucial to actively consider accessibility and inclusion needs – participants reported a variety of challenges that currently impact their ability to access support services.
Participants’ challenges in identifying health support options beyond the NHS also highlight the potential benefits of providing claimants with signposting information about general health resources and support organisations, for example, locally available free talking therapies.
6. The research has identified how a lack of a social network can contribute to poor health management and reduce the likelihood of claimants accessing health support. Health support should be cognisant of the potential extra help that might be needed from this group. Third party organisations such as charities can play a clear role in supporting such claimants, particularly those who may have less face-to-face interaction with the DWP process (i.e. PIP claimants). The research also heard from participants who would benefit from signposting to housing support, counselling, and administrative style support services, which these kind of third party organisations are well placed to deliver (e.g. Citizens Advice).
7. In getting participants to speak to the positive aspects of their claims experience, it is clear that frontline staff and ‘conversational settings’ have positive potential for delivering health support. Further research could be beneficial to establish who may be best placed to deliver this (such as Work Coaches, Healthcare Professionals, specialists, or third party organisations).
8. Claimants in this research were often applying for health and disability benefits at a point of significant disruption in their lives. Their applications were often being made to attain some level of financial stability. Whilst this is unlikely to influence the type of health support offered by DWP, it might affect the way in which it is positioned to claimants and at what point along the journey.
9. The open nature of conversations with claimants during the research has illustrated the impact the claims journey itself can have on individuals’ health. It is important that approaches designed to improve the health of claimants are not solely limited to the policy of health support signposting. Support also needs to account for the elements of the claims journey which may be inadvertently impacting claimants’ health in a negative way too. The application process and the health assessment were highlighted by participants in particular. It is important to note that work on this issue is already underway as part of the Health Transformation Programme.
DWP might relieve some of the challenges and stress claimants reported about their claims journey through better communication and education about what they can expect from the process. The research has found that those with a better grasp of the process tended to report a more positive experience. Further, providing practical administrative assistance for navigating the claims journey for those who need it might also be beneficial (whether directly or by signposting to relevant third party organisations such as Citizens Advice as noted above).
10. Finally, this research was conducted against the backdrop of the new White Paper, Transforming Support: The Health and Disability White Paper[footnote 10]. Where findings align with key themes in the White Paper the report has aimed to flag this. It is encouraging to note that several project findings reinforce some of the proposals, including the offer of more personalised support to claimants. For example, recent proposals to improve direct Work Coach support for UC Health Journey and ESA claimants outlined in the White Paper are to be welcomed in the context of health support, as are proposals to increase Work Coach understanding of mental health conditions and building connections between employment advice and NHS Talking Therapy services.
Based on the findings, there are several areas that would benefit from further investigation. For instance, conducting research to explore the best framework through which to have conversational settings about health support needs, and how this can work across the different health and disability benefits. This could include identifying how and where such conversations should be delivered, the necessary training requirements for staff, and any potential risks to be considered.
Furthermore, it could be valuable to conduct more focused research on mental health support needs and to further explore the benefits of providing enhanced support for claimant appointees to improve their experiences (noting only a small sample of this group was engaged through this research).
In conclusion, the research offers clear evidence of the potentially positive role DWP could play in offering health support and signposting to people claiming disability-related benefits.
7. Appendices
Appendix 1: Stimulus – claimant journeys for the different benefit types
PIP claimant journey
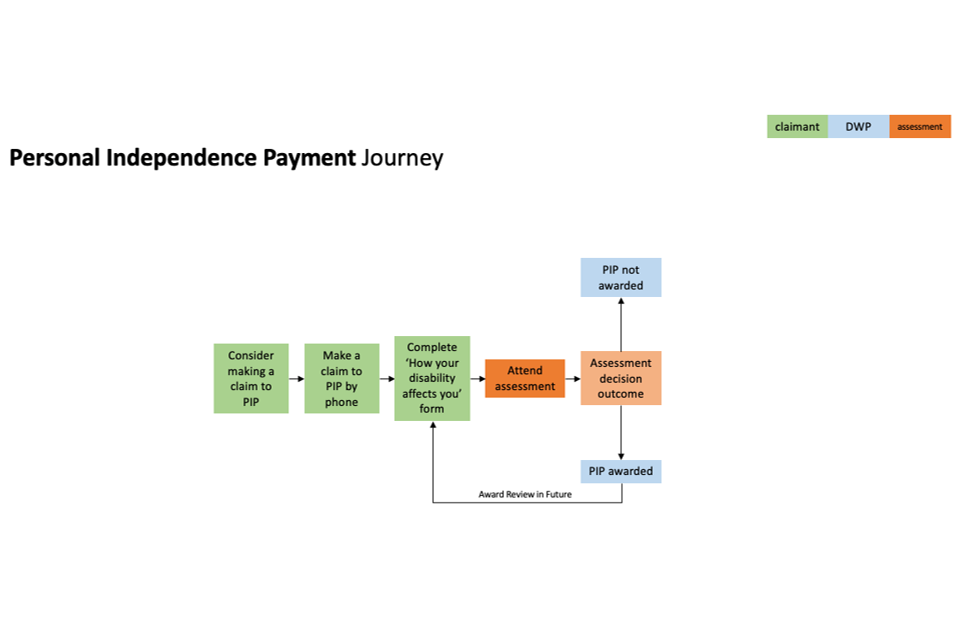
NS ESA claimant journey
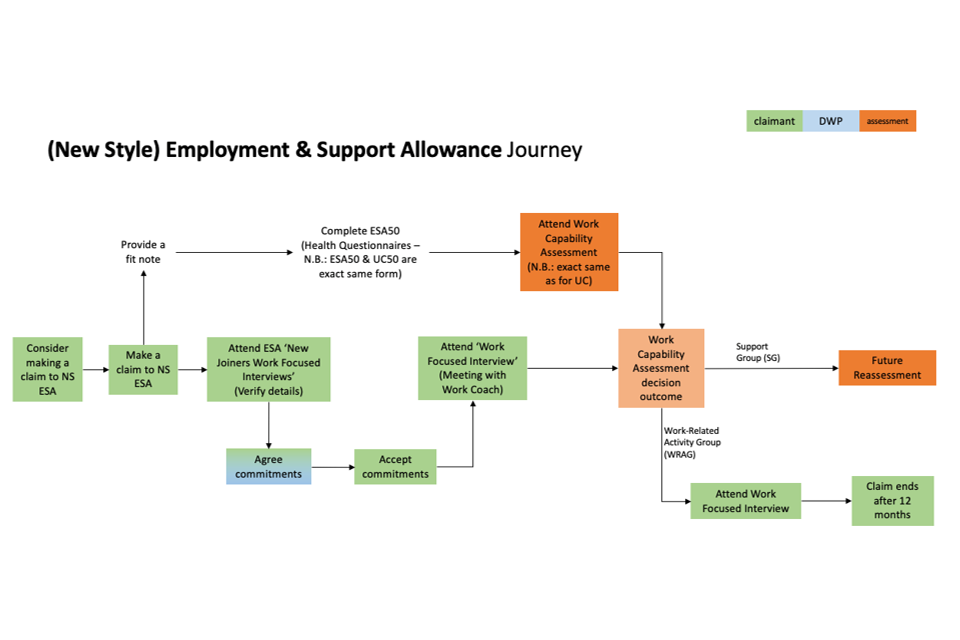
UC high-level health claimant journey
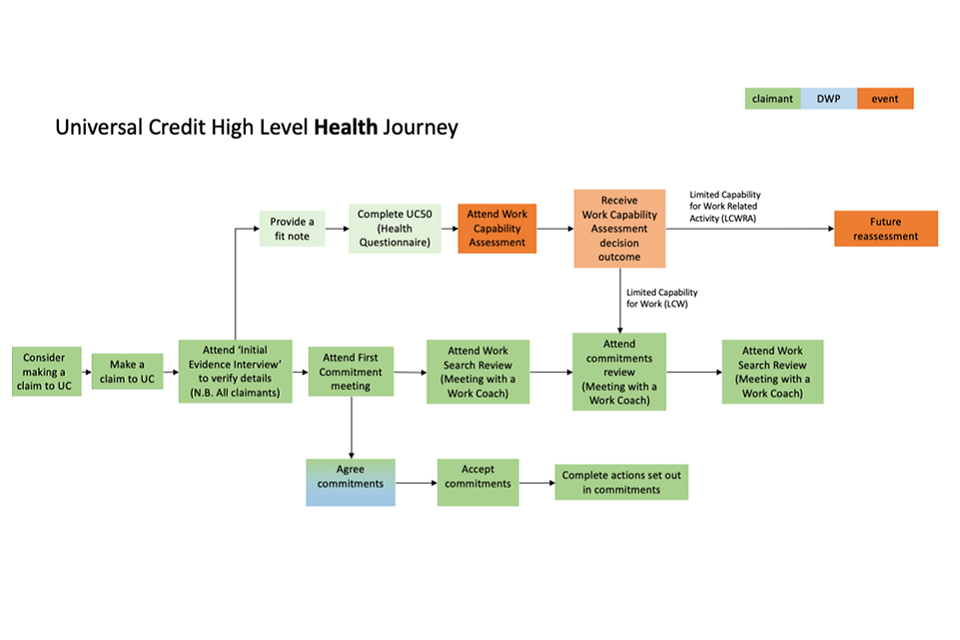
Appendix 2: Interview sample profile
Table showing interviews by benefit type
| Number completed | |
|---|---|
| Total | 76 |
| NS ESA (n20): Claimants in the assessment phase (pre-WCA) | 5 |
| NS ESA (n20): Claimants in the main phase (post-WCA) assessed as being in the WRAG | 8 |
| NS ESA (n20): Claimants in the main phase (post-WCA) assessed as being in the SG | 7 |
| Universal Credit (n20): Claimants providing valid medical evidence pre-WCA | 7 |
| Universal Credit (n20): Claimants who are post-WCA and assessed as having LCW | 7 |
| Universal Credit (n20): Claimants who are post-WCA and assessed as having LCWRA | 7 |
| PIP (n40): Pre-assessment [have submitted PIP2 but not had a decision] | 17 |
| PIP (n40): Post-assessment [who have an entitlement] | 13 |
| Multiple Benefits (n5): Universal Credit and PIP | 5 |
Tables showing monitored quotas
| Monitored Quotas: Health Conditions | Number |
|---|---|
| Move differently | 32 |
| Sense differently | 4 |
| Think or feel differently | 26 |
| Other | 7 |
| Monitored Quotas: Gender | Number |
|---|---|
| Male | 30 |
| Female | 45 |
| Monitored Quotas: Age | Number |
|---|---|
| 16-30 | 17 |
| 31-45 | 23 |
| 46-65 | 35 |
| 66+ | 0 |
| Monitored Quotas: Ethnicity | Number |
|---|---|
| White | 62 |
| Asian or Asian British | 1 |
| Black or Black British | 4 |
| Other | 8 |
Appendix 3: Health conditions in the sample
The following disabilities and health conditions were represented by participants as part of this research. It is important to note many participants experienced more than one condition.
List of disabilities and health conditions:
- Attention Deficit Hyperactivity Disorder (ADHD)
- Alcohol dependency
- Amputated leg
- Anaemic
- Angina
- Anxiety
- Arthritis
- Asthma
- Autism
- Auto immune
- Back condition
- Benign prostatic hyperplasia
- Bipolar
- Bladder cancer
- Borderline personality disorder
- Breast cancer
- Broken limb
- Cardiovascular disease
- Cauda equina syndrome (CES)
- Chronic pain
- Chronic fatigue
- Collapsed lung
- Constant cough
- Chronic Obstructive Pulmonary Disease (COPD)
- Degenerative disc disease
- Depression
- Diabetes
- Disease affecting veins and legs
- Disordered eating
- Dizziness
- Downs syndrome
- Dipyrrin’s contracture
- Fibromyalgia
- Gallstones
- Glaucoma
- Gout
- Hearing loss
- Heart and kidney failure
- Heart condition
- Hip condition
- HIV
- Hydrocephalus cerebral palsy
- Hypermobility
- Irritable bowel syndrome (IBS)
- Liver cirrhosis
- Liver disease
- Long COVID
- Macular dystrophy
- Malignant plasma cell neoplasm
- Multiple myeloma
- Muscle degeneration
- Nerve damage - spinal cord
- No use of arm
- Osteoarthritis
- Pain in hands and shoulder
- Posterior cortical atrophy
- Prostate urinary tract infections
- Rheumatoid arthritis
- Scheuermann’s disease
- Schizophrenia
- Seizures
The research team made provisions for conducting five face-to-face interviews to accommodate individuals with specific accessibility needs, such as those requiring British Sign Language interpretation or the assistance of a translator. However, it was determined that none of the participants required these adjustments.
Appendix 4: Discussion guide
1. Welcome and consent (5 minutes)
Objectives: introduce the topic; begin to build rapport with participant; put minds at ease
Hello. My name is [xxx]. I work on behalf of Basis Social/ Open Inclusion. Nice to meet you. I really appreciate you taking the time to talk to me today.
Just to recap why we want to speak to you today… we are interested in understanding the experiences of people when applying for health or disability benefits. In particular, we want to explore any health or support needs you may have during this time, what barriers you might face in accessing such support, and your experiences of accessing support during your recent assessment journey for [PIP (personal independence payment)/ NS ESA (New Style Employment and Support Allowance)/ UC (universal credit)].
Your views – whether positive or negative – will help us to understand how people might be better supported as part of their assessment process in the future.
Interviewer – we need to capture verbal consent of the following via audio recording in case we do not have signed consent forms returned. Note that participants should have already consented to being recorded as a condition of taking part [audio recorded, not video recorded].
Before we start, I just need to make sure you are happy with the following. This should have already been explained to you by our recruiter:
- Taking part in this interview is voluntary.
- We understand this may feel like a very personal topic. We ask you to be only as open and honest as you are comfortable. There are no right or wrong answers. At the same time if there is any question you wish not to answer that is completely okay.
- Your involvement will not have any impact on your benefit claims or your dealings with the DWP, now or in the future.
- The interview will be audio recorded, and I may take some notes too. This will be for analysis purposes only.
- What you say will remain anonymous – it will not be possible for the DWP or anyone else outside of basis social or open inclusion to know that you have taken part, or what you have said. This is unless you say something that makes the team think you, or someone else you identify during the interview, might be at risk of serious harm.
- You can change your mind and withdraw from this research at any time by contacting the basis social team.
Are you okay with this? [gain verbal agreement from each participant]
Do you have any questions before we get started?
2. Claimants’ Health Journeys including access and barriers to health support (20 minutes)
Objectives: understand participant’s Health Journey/ wider context to their current situation; understand inter-relationship between work and health; understand current access to health support and role it can play in improving health and employment outcomes; identify potential further needs and barriers to accessing health support
To kick us off, I would like to hear a little more about you…
Tell me a little bit about yourself…
- What words would you / your friends use to describe you?
- When do you feel at your best? Why?
- What do you like to do with your time?
Now we are now going to speak a bit about your health condition/s or disability, how it impacts you and your live, and how you have learned to cope with and manage your condition/s/disability. As mentioned before, we recognise that this is a personal and sensitive topic, and we are not expecting you to share any details of your experiences you do not feel comfortable with.
- Could you talk me through the experience of your health condition/disability a little bit?
- Can you tell me the name of the health condition(s) or disability that you have, if you are happy to share these with me today?
- Researcher to list all and probe where relevant for comorbidities throughout Health Journey section
- When did your condition(s) or disability(ies) first begin to affect you? In what ways?
- Could you tell me a little bit about how your current health condition(s)/ disability(ies) affects you?
- How does your current condition impact your day-to-day life?
- Probe: any long-term or ongoing needs/ conditions?
- Probe: is the condition stable or does it fluctuate?
- How does it affect your overall health and wellbeing?
- [if time researcher to ask] does it stop you doing anything you would like to be doing?
- Probe: does it affect your ability to work/ work as much as you would like/ in the job you would like?
- How easy/ hard do you find managing your health condition/ disability?
- Probe: how do you find managing your condition physically? What supports do you rely on to help you live your life?
- Probe: how do you find managing your condition/disability emotionally?
- Probe: who plays a role in helping support you to manage your condition(s)/disability(ies)? And how important is their support to your wellbeing?
- Prompt: partner, family, carer, social worker, clinical staff, community group
- Probe if there is time: any changes since covid in terms of your emotional or physical health, or in terms of how able you are to manage your condition (e.g. Accessing support for health in community)?
Section 2.2 managing your condition/accessing support
- Let’s talk about the support out there to help you manage your condition(s). What support have you personally accessed to help you in managing your health condition(s) so far?
- By “support” or “health support” in this research we mean, any clinical or non-clinical support that may help you manage your condition(s)/disability(ies) and/or alleviate any personal, emotional or physical issues relating to your condition.
- Probe: clinical (e.g. GP and primary care) vs. Non-clinical support (e.g. Community networks, charity, websites, holistic care); national vs. Local
- Probe: types of support, e.g. In relation to managing condition vs. Wider issues such as managing finances or supporting wider family
- When did you decide to access this support?
- How did you find out about the support available? (e.g. Signposted by clinical staff, support group, website)
- What benefit did you hope to get from this support?
- How valuable have you found this support in terms of
- … improving your overall health and wellbeing?
- … your engagement with the workplace (e.g. Helping move towards or into more desirable employment)?
- Has it met your expectations? Why? /why not?
- What health support do you know is out there for your condition(s) / disability(ies) that you do not currently access? Why don’t you access these?
- Do you feel you are getting all the support you need at the moment in managing your health condition(s)?
- If no: What’s missing?
- Probe: physical health support vs mental health support
- What, if anything, do you think might be preventing you from accessing additional support?
- Probe on potential barriers: e.g. Not knowing what’s available, support not being accessible, cost, mistrust of information/ support, not wanting to feel a burden.
3. Claimants’ assessment journeys, and experiences of key touchpoints (10 minutes)
Objectives: understand participant’s claimant journey; understand motivations for claiming; help identify key touchpoints or challenges within the claims journey; understand high level perceptions of key DWP touchpoints (which may impact wider views about their role in providing health support)
I’d now like to understand a little more about your experience in claiming [PIP (personal independence payment), NS ESA (new style employment and support allowance), or UC (universal credit)]
[share stimulus of claimant journey map]
We understand you’re currently at [insert from screener] in your assessment process. Is this correct? [interviewer points to relevant stage of journey to crosscheck process to date resonates with participant]
- Could I ask, what made you decide to apply for [PIP/ NS ESA/ UC]?
- Was there something that happened with your health condition which made you apply?
- How did you find out about it? Who, if anyone, encouraged you to apply?
- Probe on information sources, e.g. Word of mouth, work coach, via GP or other healthcare professional, online
- When did you decide to apply? Why at this point specifically?
- What are you hoping applying for [PIP/ NS ESA/ UC] would offer you?
- Probe: extra money, peace of mind, support finding work, help managing their health condition
We’re now going to speak a bit about your experience of the application process in general. We appreciate that this can be a stressful or overwhelming experience for some, and you’ll likely have lots of things to say. I apologise in advance if it feels like I’m going through this section at speed and there is more that you would like to say. DWP are doing a lot of research at the moment to try and improve the application process for people, but this study is more about accessing health support. So while we will cover this quickly, it will not be the main bulk of our conversation today.
Speaking overall, how have you found the process of applying for [PIP/ NS ESA/ UC] (so far)? [researcher to keep high level]
- Probe overall spontaneous views, positive and negative
- Area’s participant may mention (researchers to note not probe):
- Accessibility issues filling out forms/ long forms
- Issues around jargon/ wording
- Relevance (or not) to one’s life or context
- Difficulties contacting DWP
- Mental health toll, energy toll etc.
- Are there any particulars elements of the application process/claim journey that stand out as particularly positive/ negative in terms of your experience? [interviewer we’re interested to understand if there are touchpoints or interactions that resonate more positively/ negatively to help understand where signposting might be most effectively introduced]
4. Health support needs during claims process and role of DWP in signposting to health support (20 minutes)
Objectives: understand claimants’ needs across the assessment journey; understand any current health signposting taking place via DWP; identify if claimants would be receptive to DWP signposting health support, and what this could look like.
[interviewer note: you will need to factor in running this for both PIP AND UC claims processes where participants have done both.]
I’d like you to think about your health and any support needs you had during the claims process we have just been discussing…
- Thinking about your claim journey/application process so far, can you identify any key points at which you would have liked some support relating to your health condition/ disability? [interviewer annotate on journey map and refer back to how condition/disability impacts people]
- Probe: when in the claims journey/application process and why?
- Probe: what sort of support might have been helpful in meeting this need?
- Probe on non-clinical support (e.g. Community networks, charity, online information, welfare rights organisations, telephone support or helplines, fitness or exercise, holistic therapy, social media, forums, blogs)
- Thinking generally, how do you feel about DWP signposting people to health support as part of their application process? I.e. In principle do you agree/disagree with this? Why?
Researcher to remind participants: by “support” or “health support” in this research we mean, any clinical or non-clinical support that may help you manage your condition(s)/disabilities and/or alleviate any personal, emotional or physical issues relating to your condition.
- Probe: positive/ negative – e.g. Concern about influencing their claim; how it might impact work-orientated conversations; improvements to wellbeing; suspicion or mistrust, DWP are not health experts
- Probe: what value do they think DWP could bring in playing a signposting role, if at all? (i.e. Could signposting from DWP play a positive role? How?
- Now I’d like you to think about your own personal experience, how would you feel if DWP had signposted you to support or had a conversation with you about your health needs and the range of support available to you?
- Would you have taken up support if DWP had suggested this to you? Why? Why not?
- How would that conversation have felt at these different points across the claim journey? (prompt: at the point of application, at initial meeting, at work coach meeting, at commitments meeting, at work capability assessment etc.) Interviewer work through each point on journey where support to help alleviate symptoms associated with health condition would have been welcome by participant to understand how they would feel if DWP provided signposting.
For each probe for:
- How ready /open they would have been to accepting support / having conversations about support
- Trust/ suspicion/ what do they see as DWP’s motivation for signposting support
- Positive/value-add helping them out at a time of need
- How would this support be best signposted/ who provides it
- E.g. Letter, website, work coach, assessor, case manager
- Would they want reassurances, and what would these be
- E.g. General encouragement vs specific actions that they can take up:
- Is there anything that might be important for DWP to consider if it was to encourage someone like you to seek health support?
- Probe: accessibility requirements, using simple language, providing reassurance about support not impacting their claim, other ways to build trust, DWP signposting to be seen separately to the claims process itself
5. Final reflections/close (5 minutes)
Objectives: Final reflections on the discussion; Signposting as part of further safeguarding
Thinking about what we’ve been talking about today, is there anything else you would like to add about the types of health support you feel you need, and DWP’s potential role in helping you access this?
Thank you for your time today.
- You should be happy to know that your views will be feeding into a very important piece of work for DWP, aimed at improving the support that people receive while claiming health and disability benefits.
- Just to reiterate, all you have told me today will remain confidential to Basis Social/ Open Inclusion and Basis Social.
- Signposting:
- We can send you an email with links to support services if you would find this helpful?
Any further questions – please email the Basis Social team: dwp.healthassessmentresearch@basisresearch.com
References
Dhere A. (2016) ‘Managing complex long-term conditions and multimorbidity’. Clinical Medicine (Lond) 16(6): 545–547 [online]. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6297343/
Department for Work and Pensions. (2022) ‘Employing Disabled People and People with Health Conditions’ [online]. Available at: https://www.gov.uk/government/publications/employing-disabled-people-and-people-with-health-conditions/employing-disabled-people-and-people-with-health-conditions
Department for Work and Pensions. (2023) ‘Employment of Disabled People 2022’ [online]. Available at: https://www.gov.uk/government/statistics/the-employment-of-disabled-people-2022/employment-of-disabled-people-2022
Department for Work and Pensions. (2023) ‘Health Transformation Programme Evaluation Strategy’ [online]. Available at: https://www.gov.uk/government/publications/health-transformation-programme-evaluation-strategy/health-transformation-programme-evaluation-strategy
Department for Work and Pensions (2023) ‘Transforming Support: The Health and Disability White Paper’ [online]. Available at: https://www.gov.uk/government/publications/transforming-support-the-health-and-disability-white-paper
Guest G., Brunce, A., and Johnson, L. (2006) ‘How many interviews are enough? An experiment with data saturation and variability’, Field Methods, Sage (Lond), 18(1), 59–82 [online] Available at: https://journals.sagepub.com/doi/10.1177/1525822X05279903
Office for Health Improvement and Disparities (2022) ‘Guidance: Working Definition of trauma informed practice’ [online] Available at: https://www.gov.uk/government/publications/working-definition-of-trauma-informed-practice/working-definition-of-trauma-informed-practice
-
DWP. (2023) Transforming Support: The Health and Disability White Paper ↩
-
DWP (2023). Employment of disabled people 2022. ↩
-
DWP. (2023) Transforming Support: The Health and Disability White Paper ↩
-
DWP. (2023) Health Transformation Programme evaluation strategy ↩
-
DWP. (2023) Transforming Support: The Health and Disability White Paper ↩
-
Guest, G., Bunce, A., & Johnson, L. (2006) How many interviews are enough?: An experiment with data saturation and variability ↩
-
Trauma-informed practice is an approach to health and care interventions which is grounded in the understanding that trauma exposure can impact an individual’s neurological, biological, psychological, and social development. For more information on this topic, please refer to the government’s recently published guidance. ↩
-
Note interviews with appointees in attendance are not counted in the appointee sample, as these interviews did not focus on the experience from the appointee point-of-view. ↩
-
Dhere, A. (2016) Managing complex long-term conditions and multimorbidity. ↩
-
DWP. (2023) Transforming Support: The Health and Disability White Paper. ↩
