Adult social care provider information provisions: guidance for providers on data collection
Updated 4 April 2024
Applies to England
Background
The COVID-19 pandemic exposed challenges in bringing together data needed to effectively manage outbreaks and ensure that emerging risks and issues could be identified at all levels and appropriate action taken. This has highlighted the importance of having robust data flows in the adult social care (ASC) sector to provide assurance that local and national government have the data and local intelligence to provide oversight and national support where it is needed in the longer term.
We need quality and timely ASC data that is collected to high standards and is transparent and accessible to all who need it to support high-quality commissioning, systems assurance and the management of risks at local, regional and national levels. This will help to ensure that nationally, regionally, locally and at provider-level, ASC data is used to benefit the system and support people who draw on care and support to make informed choices about their care.
Many bodies currently collect information but there is little standardisation in how it is collated, shared and used. The current aggregated data collected by local authorities shows a significant gap that needs to be addressed to include people drawing on privately funded care and support. Doing so will help ensure a fuller picture and enable improved outcomes for all people receiving care and support.
In the government’s health and social care data strategy, Data saves lives: reshaping health and social care with data, we set out our vision to transform adult social care data so that people who draw on support have access to information and can make more informed choices about their care, and for their carers to have timely data so that they can provide the best possible care.
As outlined in the People at the Heart of Care white paper, access to reliable data is key to underpinning the government’s ambition for social care reform. The COVID-19 pandemic has brought into sharp focus the need for high-quality data and information to be shared and used well. Prior to the pandemic, the Department of Health and Social Care (DHSC) had no comprehensive national source of data from providers on capacity, workforce status or numbers of people in receipt of care and most data was captured through aggregate annual returns from local authorities.
Emergency data measures taken in response to COVID-19 have given us near real-time data to manage the pandemic and shown us the benefits of using data to respond to emerging risks and issues.
Data from social care providers has been critical to the government’s COVID-19 response and will continue to be crucial to help us to understand capacity and risk in the care system, to judge when and how to target support to providers and ultimately to help facilitate the care of individuals across the care system.
Through technology and data strategies, and the Data Alliance Partnership, we are working to ensure the most efficient methods of data collection and improvement in the interoperability of systems. We have committed to ensuring that the data architecture underpinning the health and care system can easily work together to make more effective and efficient use of data.
The Health and Care Act 2022 received Royal Assent in April 2022. It includes:
1. A power for the Secretary of State for Health and Social Care to require adult social care providers to provide information relating to themselves, to their activities in connection with the provision of ASC in England or to persons to whom they have provided such care (section 99).
This power commenced on 31 July 2022 and applies to all ASC providers regulated by the Care Quality Commission (CQC). These are providers required to be registered under the Health and Social Care Act 2008 in respect of the carrying on of a regulated activity involving, or connected with, the provision of ASC in, or in relation to, England.
2. A power to make regulations enabling the Secretary of State for Health and Social Care to impose a financial penalty on private providers that do not comply with an information request or provide false or misleading information without reasonable excuse (section 100).
The Adult Social Care Information (Enforcement) Regulations 2022 were made on 10 November 2022 and came into force on 1 December 2022. Enforcement regulations apply to all private ASC providers regulated by CQC.
Data collection
Information required from 31 July 2022
From 31 July 2022, we mandated a core subset of the data which providers have already been submitting through the Capacity Tracker (CT). This is gathered on a monthly basis. Providers are required to update the CT with the required data within a designated 7-day reporting window. This window will open at the start of the 8th day of each month and run until the end of the 14th day of each month, or the next working day where the 14th day falls on a weekend or public holiday. This is shown in the graphics below.
Figure 1: data collection reporting windows
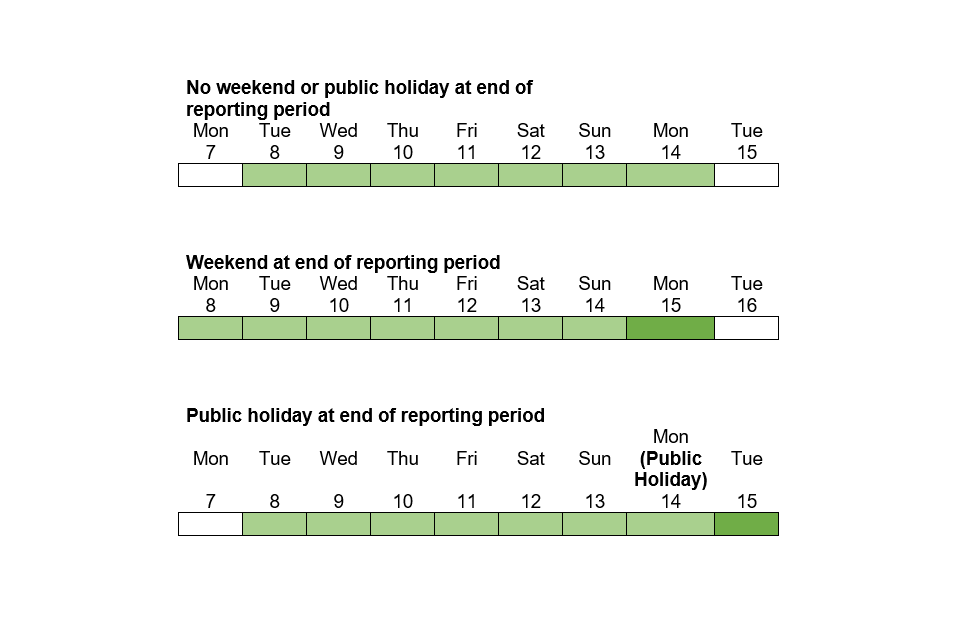
Figure 1 shows 3 graphics of the reporting windows:
- graphic 1 shows the reporting window if the 14th day falls on a weekday. The window is highlighted as being between the 8th and the 14th inclusive (both dates included)
- graphic 2 shows the reporting window if the 14th day falls on a Sunday. The window is highlighted as being between the 8th and the 15th inclusive (both dates included), which is the next working day from the Sunday
- graphic 3 shows the reporting window if the 14th day falls on a Monday and it is a public holiday. The window is highlighted as being between the 8th and the 15th inclusive (both dates included), which is the next working day from the Monday
Full dates to March 2025 are in Annex A.
Updates for this data will need to be made via the CT using the same method as at the time of this guidance’s publication – by providers either updating each mandated field individually or by the bulk update functionality. The data must be reviewed within the reporting window of each month, and, even if there are no changes to be made, the page is saved so that it is marked in the system as having been updated.
In November 2022, the Capacity Tracker Data Advisory Group (CTDAG) was replaced by the Provider Data Advisory Group (PDAG). As we did with CTDAG, DHSC will regularly engage with and consult the PDAG on:
- ways to make it clearer how data is being used centrally
- improvements to the wording and content of specific data items based on feedback received from ASC providers and data users
This is intended to ensure that any changes improve data quality and relevance, while also managing data burdens on providers.
PDAG membership includes representatives from:
- Association of Directors of Adult Social Services
- Care Software Providers Association
- CQC
- DHSC
- Department for Levelling Up, Housing and Communities
- Digital Social Care
- Local Government Association
- National Institute for Health and Care Excellence
- NHS England
- Professional Records Standards Body
- Skills for Care
The following provider groups are also PDAG members:
- Associated Retirement Community Operators
- Care Association Alliance
- Care England
- Care Provider Alliance
- Homecare Association
- Learning Disability England
- National Care Association
- National Care Forum
- Registered Nursing Home Association
- Think Local Act Personal
Other data items in CT are often key for local operational support and providers will be asked to provide more regular updates to these items – for example, confirmed and suspected COVID-19 cases in staff and residents, daily bed vacancy updates and workforce data. Such data requests are separate to the mandated list but are essential to continue to support you as providers, and health and social care partners, such as discharge teams, to keep people and staff as safe and healthy as possible. The daily vacancy data is useful when more frequent because it supports people to be in the right place for their specific needs.
Data items that form part of the mandatory collection are clearly marked in the CT system during the reporting window period.
The latest list of data items can be found in the formal notice of a mandate for all adult social care providers.
Purpose of collecting this information
Availability of good quality and timely data from ASC providers is essential to:
- supporting efficient commissioning and systems assurance
- managing national, regional and local risks
- assisting with evolving situations, like COVID-19
- ultimately, helping to facilitate the care of individuals
Data mandation will build on the stronger data sharing practices we have built during the pandemic where providers have shared data and information via the CT tool. This has highlighted the importance of having robust data flows in the ASC sector to ensure that the right level of capacity and support is available for service continuity. It will support a consistent and transparent approach to the processing of data across privately and publicly funded care to support improved safety and quality of provision.
Data is needed to:
- continue to support COVID-19 recovery
- monitor vaccination levels
- understand capacity and risk in the care system more generally
- understand the impact of winter pressures
- determine when and how to target support to providers
- ultimately, help facilitate the care of individuals across the care system in the long term
For example, during the pandemic, provider data-sharing facilitated:
- flagging a need for a visit from a COVID-19 vaccination team – vaccination teams also used data to arrange visits directly
- highlighting issues with accessing flu vaccinations
- flagging PPE shortages
- receipt of targeted support from regional teams, using data from the workforce RAG status
- visualising and benchmarking your own provider data against local authority, regional and national data to understand how it compares
Emergency data measures taken in response to COVID-19 gave us near real-time data to manage the pandemic and showed the benefits of using data to respond to emerging risks and issues – for example, in outbreak management and prioritising PPE supplies for providers in highest need.
Currently, providers are able to view their data in the CT and use this for benchmarking purposes, comparing against the local authority, regional and national aggregate. This provider view will be reviewed and improved to better meet provider needs and support them to realise the full value of their data, noting such needs will differ depending on provider characteristics. We will be seeking feedback from providers on how to improve this view using the PDAG member organisations. Furthermore, we are keen to explore what wider data sources we can add to this view, to offer a richer source of data to providers that they would not be able to access without it.
Data also helps us to identify issues at an early stage and provide an evidence base for central government funding discussions. For example, CT data on staff absence in January 2021 showed the need for support with recruitment and that additional staff hours were needed, one of the drivers of the £120 million Workforce Capacity Fund being established.
With more and better data, we can plan the future care of our population and will have the potential to generate significant health and care benefits such as increased independence, improved quality of care, higher satisfaction for people drawing on health and care support, and more efficient use of funding. Improved data on the ASC workforce can also benefit recruitment, retention and equality policies.
We have carried out an impact assessment in relation to the financial implications of mandatory completion of the CT.
Engaging on future changes
The burden on ASC providers in providing data is a key consideration in all changes and our aim is to reduce the burden overall where possible, while also improving the information data gives. If the data needs of DHSC or other ASC partners evolve or issues with data arise, wherever possible, we will give at least 3 months’ notice of any change to the mandated data listed above or to the frequency of collection before making it a legal requirement. If DHSC receive feedback on the usefulness or burden of the above listed data items, we will work with the sector to review and iteratively improve these as needed.
We intend to engage on changes with providers and representatives through the PDAG. The PDAG includes provider and local authority representatives.
If a change to a data item or a new data item is required by DHSC, DHSC will first consider key criteria such as whether it can be obtained elsewhere, what any output will be used for and the benefit of collecting it for providers, settings and other sector partners. If the need is clear, an example of how the data item will appear in the CT will be shared with PDAG for feedback and further iteration as part of co-building.
Depending on the scale of the change, any engagement might be solely via email feedback, representations at a PDAG meeting itself, or could involve workshop sessions. This iterative process seeks to refine the new or changed data item to a point where it is ready for development and adding to the collection. Once the process is complete, we will notify providers of the upcoming change, giving at least 3 months’ notice, where possible.
Support and guidance
Filling in the Capacity Tracker
The CT is managed by the North of England Care System Support (NECS) unit. NECS provides a dedicated support centre – Monday to Friday, 8am to 5pm – to support care providers and wider stakeholder users of the CT. If providers need support completing or updating the system, accessing or using the reports and analytics, they can reach out either by phone 0191 691 3729 or via necsu.capacitytracker@nhs.net.
In addition, the CT has an integrated resource centre – all communications, user or help guides and video tutorials along with contact details for local System Champions can be found there.
NECS also utilises regional leads that are split across the 7 NHS England regions. They run regular provider engagement sessions and have set up regional forums to help support continuous improvement of the system and support our user centred design approach.
For guidance relating to how to answer specific questions, you can email capacitytracker-guidance@dhsc.gov.uk.
Providers will be contacted when they have not updated their CT data and will be offered support or advice on completing the return. This will be done via NECS as at present, or via other routes depending on the issue. Contact will normally be established via a combination of emails, telephone calls and NECS regional leads and local system champions.
For administrative amendments, account support and more, you can contact NECS directly already at: necsu.capacitytracker@nhs.net.
Data use and privacy
These provisions will not enable data to be sold to private organisations. Our intention is that data collected will be shared appropriately with organisations who need the data across the ASC sector (for example, local authorities, CQC, integrated care systems) to guide delivery, policy development and research in the area for purposes connected with the health or ASC system in England. We will continue to encourage all such partners to look to data in CT in the first instance rather than instigating separate data collections covering similar data.
The information will be subject to the UK General Data Protection Regulation (GDPR) and statutory restrictions on disclosure. This includes not sharing commercially sensitive data without taking into account both the interests of the provider (or the person to whom that data relates) and the public.
Section 277A states that the provision of information under that section:
- does not breach any obligation of confidence owed by the person providing it, but
- is subject to any express restriction on disclosure imposed by any enactment (other than a restriction which allows disclosure if authorised by an enactment)
DHSC will seek to ensure that data requests comply with these principles including UK GDPR but providers should take their own legal advice as necessary.
Enforcement powers
See Adult social care provider information provisions: data enforcement for guidance on DHSC’s enforcement powers.
Annex A: reporting window periods until March 2025
The reporting window periods are:
- 8 April 2024 to 15 April 2024 (inclusive – both dates included)
- 8 May 2024 to 14 May 2024 (inclusive – both dates included)
- 8 June 2024 to 14 June 2024 (inclusive – both dates included)
- 8 July 2024 to 15 July 2024 (inclusive – both dates included)
- 8 August 2024 to 14 August 2024 (inclusive – both dates included)
- 8 September 2024 to 16 September 2024 (inclusive – both dates included)
- 8 October 2024 to 14 October 2024 (inclusive – both dates included)
- 8 November 2024 to 14 November 2024 (inclusive – both dates included)
- 8 December 2024 to 16 December 2024 (inclusive – both dates included)
- 8 January 2025 to 14 January 2025 (inclusive – both dates included)
- 8 February 2025 to 14 February 2025 (inclusive – both dates included)
- 8 March 2025 to 14 March 2025 (inclusive – both dates included)
Annex B: operational support, non-mandatory data collection
This annex contains guidance for providers on operational support, including non-mandatory data collection.
Operational support data
Operational support data items in CT are often key for local operational support and providers will be asked to update these items daily or weekly. They fall into 2 categories:
- Those that are also part of the mandatory data collection. These must be updated monthly to comply with the adult social care provider information provisions. If they are not updated, providers may be subject to enforcement. For operational support, providers are asked to update these more frequently, though this a non-mandatory request.
- Those that are not part of the mandatory data collection but for operational support, providers are asked to provide these daily or weekly, though this a non-mandatory request.
Questions that are used for operational support purposes for care home provider locations are:
- confirmed and suspected COVID-19 cases in staff and residents
- vaccination updates that are part of an ongoing campaign, for example winter flu
- daily bed vacancy updates
- digital social care record (DSCR) software in use, if any
- knowing who is your primary care network lead
- up-to-date infection prevention and control training
- care home rounds
Such data requests are separate to the mandated data collection but are essential to continue to support you as providers, along with health and social care partners, such as discharge teams, to keep people and staff as safe and healthy as possible.
