Young people's substance misuse treatment statistics 2020 to 2021: report
Published 27 January 2022
Applies to England
1. Main findings
1.1 Trends in young people’s treatment numbers
There were 11,013 young people in contact with alcohol and drug services between April 2020 and March 2021. This is a 23% reduction from the previous year (14,291) and a 55% reduction in the number in treatment since 2008 to 2009 (24,494).
1.2 Trends in young people’s substance use
Cannabis remains the most common substance (89%) that young people come to treatment for.
Around 4 in 10 young people in treatment (41%) said they had problems with alcohol, 12% had problems with ecstasy and 9% reported powder cocaine problems.
The proportion of young people seeking help for heroin was the same as last year, at 0.4%. However, the proportion of those with codeine problems has doubled from 2018 to 2019 (0.6% compared to 1.2% this year).
Following a 19% decrease between 2018 and 2020, this year saw a small increase in young people reporting a problem with benzodiazepines. This proportion (3.7%) was over 5 times the proportion in 2013 to 2014 (0.7%).
1.3 Vulnerabilities among young people in treatment
The most common vulnerability reported by young people starting treatment was early onset of substance use (73%), which means the young person started using substances before the age of 15. This was followed by poly-drug use (53%).
Proportionally, girls tended to report more vulnerabilities than boys, particularly self-harming behaviour (46% compared with 15%) and sexual exploitation (12% compared with 2%).
1.4 Mental health treatment need
Over two-fifths (43%) of young people starting treatment this year said they had a mental health treatment need, which continues the rising trend of the last 2 years (37% in 2019 to 2020 and 32% in 2018 to 2019). A higher proportion of girls reported a mental health treatment need than boys (58% compared to 36%).
Most young people (68%) who had a mental health treatment need received some form of treatment, usually from a community mental health team.
1.5 Treatment exits
Of the young people who left treatment, 79% left because they successfully completed their treatment programme, which is slightly lower than the previous year’s proportion (82%). The next most common reason for leaving treatment (15%) was leaving early or dropping out, slightly higher than the previous year (12%).
1.6 The effect of COVID-19
The coronavirus (COVID-19) pandemic is likely to have contributed significantly to the reduced number of young people starting substance misuse treatment in 2020 to 2021, compared with the previous year. In particular, school closures and reduced face-to-face contact across all children and young people’s services meant there were fewer opportunities for young people to be referred to substance misuse services.
2. Age and sex of young people in treatment
There were 11,013 young people in contact with drug and alcohol services between 1 April 2020 and 31 March 2021. Two-thirds were male (66%), similar to the previous 2 years. The median age was 16 years old for both boys and girls. The number of younger children (under 14) in treatment remained relatively low (740, 7%).
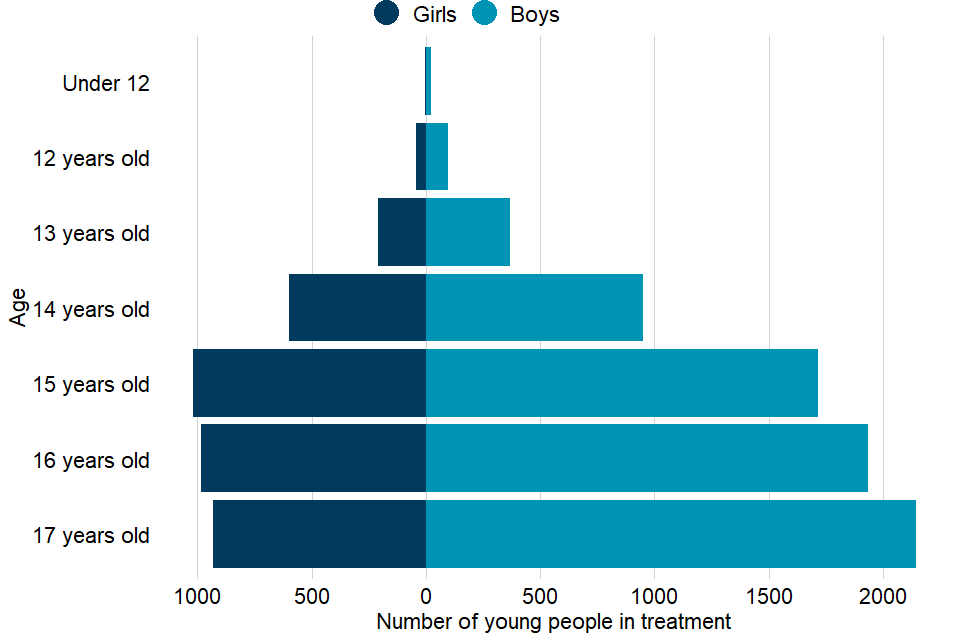
Figure 1: age and sex of young people in treatment
3. Substances used by young people
When young people enter treatment, they can record up to 3 substances that they have a problem with. Numbers in this section are based on all substances recorded during their treatment.
There were 9,832 young people who said they had a problem with cannabis (89% of all in treatment) and 4,459 (41%) said they had a problem with alcohol.
Twelve per cent (1,333) said they had a problem with ecstasy and 9% (976) reported a problem with powder cocaine. Twelve per cent (1,368) reported a problem with nicotine use.
Other substances reported include ketamine, benzodiazepines, solvents, codeine, amphetamines, new psychoactive substances (NPS), crack, heroin and other opiates.
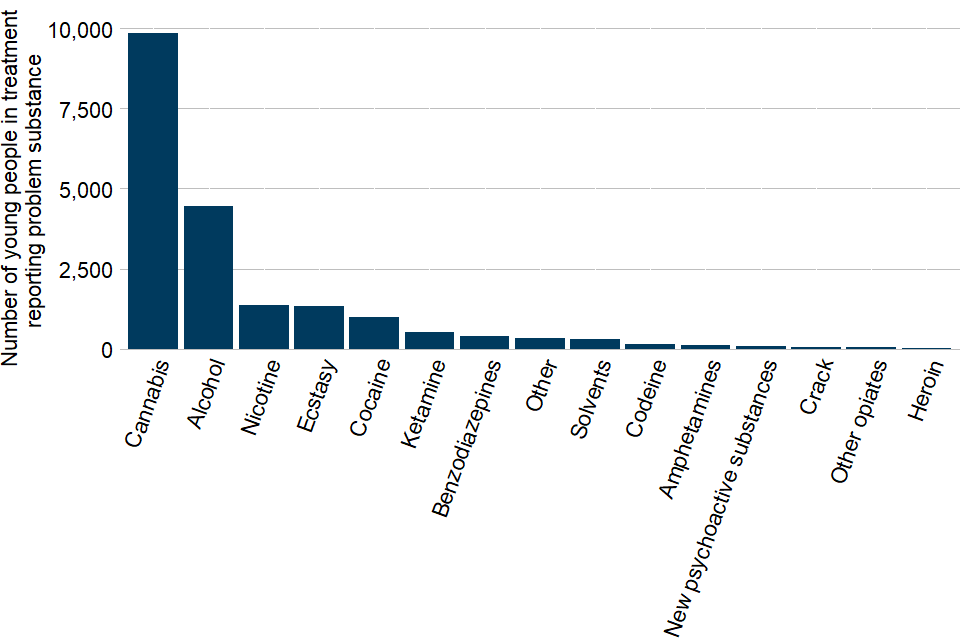
Figure 2: problem substances reported by young people
Section 10.2 of this report shows the numbers of young people in treatment broken down by substance since 2005 to 2006.
4. Referral routes into treatment
The most common route for young people to get into specialist treatment services was a referral from social care services. The proportion of people entering treatment this way was higher than the previous year (25% compared with 18% in 2019 to 2020), despite the number remaining stable (1,748 in 2019 to 2020 and 1,743 in 2020 to 2021). This is because of a large fall in referrals from other sources, likely because of the COVID-19 pandemic.
Referrals from the youth justice system were the second largest source of referral (25%, 1,705). Education services (such as mainstream education or alternative education) accounted for 19% of referrals, but the number of these referrals (1,284) dropped by 60% from the previous year. Other routes included referral by self, family or friends (12%, 867), health services (12%, 863) and other substance misuse services (5%, 333).
| Referral source | Number of young people |
|---|---|
| Social care | 1,743 |
| Youth criminal justice | 1,705 |
| Education | 1,284 |
| Health services | 863 |
| Self, family and friends | 867 |
| Substance misuse services | 333 |
| Other | 148 |
Figure 3: referral routes into treatment
5. Vulnerabilities of young people in treatment
Young people often enter specialist substance misuse services with a range of problems or vulnerabilities related to (or in addition to) their substance use. These include:
- using multiple substances (poly-drug use)
- having a mental health treatment need
- being a looked after child
- not being in education, employment or training (NEET)
Other wider risk factors can also affect or be associated with young people’s substance use, such as:
- self-harming behaviour
- sexual exploitation
- offending
- domestic abuse
Vulnerabilities are reported here only for young people who entered drug and alcohol treatment services during 2020 to 2021.
The most common vulnerability was early onset of substance use (73%), which means the young person started using substances before the age of 15. Girls reported this more than boys (77% and 71% respectively). This was followed by young people reporting poly-drug use (53%). Again, girls tended to report this more than boys (62% and 49% respectively).
Proportionally, girls tend to report more vulnerabilities than boys, particularly for self-harming behaviours (46% compared with 15%) and sexual exploitation (12% compared with 2%).
Other vulnerabilities that were commonly reported by young people include:
- antisocial behaviour (33%), which was more common for boys than girls (41% compared with 19%)
- being affected by domestic abuse (23%)
- being affected by others’ substance use (23%)
Less commonly reported vulnerabilities include:
- opiate or crack use (3%)
- being pregnant or a parent (4%)
- housing problems (1%)
- injecting (less than 1%)
Being involved with social services as a looked after child (13%), a child in need (14%) or having a child protection plan (9%) were also recorded as vulnerabilities.
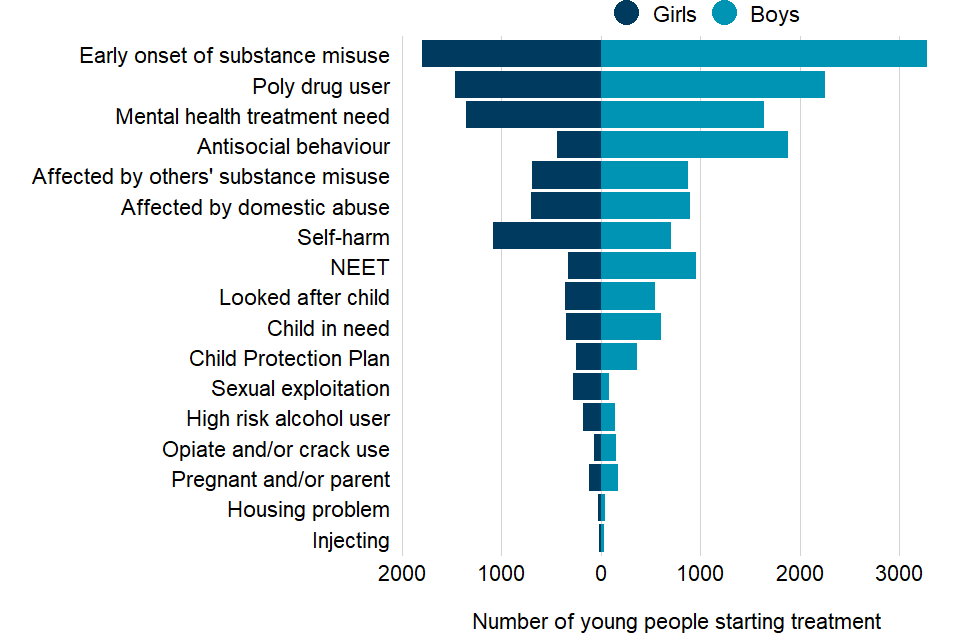
Figure 4: vulnerabilities among young people starting treatment
6. Sexual exploitation
The Department for Education has published guidance that defines child sexual exploitation (CSE):
Child sexual exploitation is a form of child sexual abuse. It occurs where an individual or group takes advantage of an imbalance of power to coerce, manipulate or deceive a child or young person under the age of 18 into sexual activity (a) in exchange for something the victim needs or wants, and, or (b) for the financial advantage or increased status of the perpetrator or facilitator. The victim may have been sexually exploited even if the sexual activity appears consensual. Child sexual exploitation does not always involve physical contact; it can also occur through the use of technology.
Overall, 5% (362) of young people who entered treatment in 2020 to 2021 reported CSE. Broken down by age, the proportion was:
- 6% of 16 year olds (98)
- 5% of 14 year olds (44), 15 year olds (89) and 17 year olds (112)
- 4% of those under 14 (19)
Among the young people who started treatment in 2020 to 2021, girls reported CSE much more than boys, with 285 girls (12% of all girls) and 77 boys (2% of all boys) reporting CSE.
Among girls, 13% of those aged 15 or older reported CSE compared to 9% of those aged 14 or younger. For boys, the proportion reporting CSE was 3% for both these age groups.
Most girls who reported CSE were aged 15 (70, 25%), 16 (85, 30%) or 17 (83, 29%). Forty-seven girls (17%) who reported CSE were aged 14 or younger. Most boys who reported CSE were 17 years old (29, 38%). A quarter of boys who reported CSE (19, 25%) were 15 years old, 13 boys were 16 years old and the remaining 16 boys were aged 14 or younger.
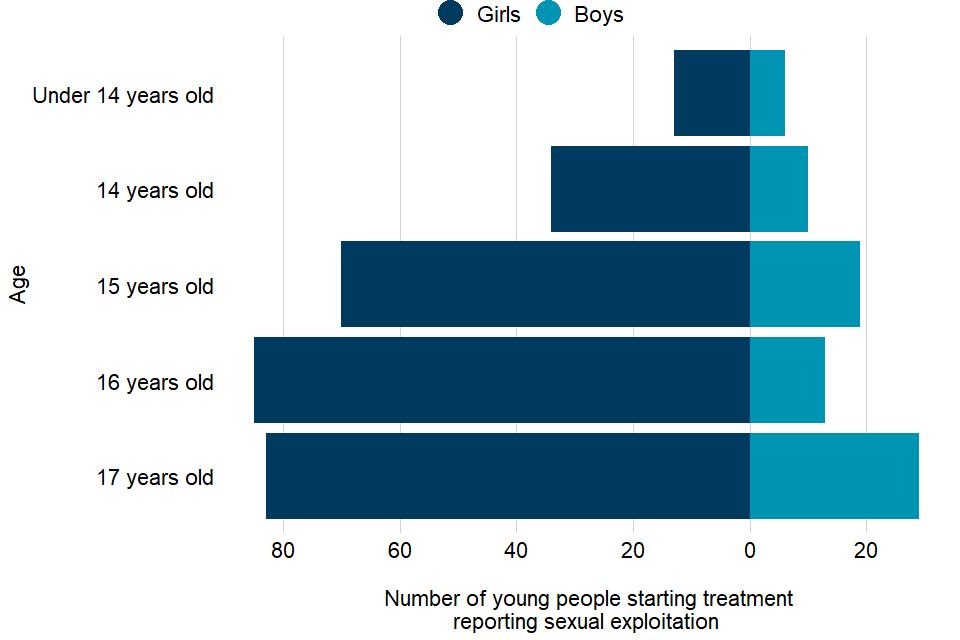
Figure 5: sexual exploitation of young people starting treatment
7. Mental health needs
Over two-fifths (43%, 3,007) of young people who started treatment in 2020 to 2021 said they needed mental health treatment.
A higher proportion of girls reported needing mental health treatment than boys (58% compared to 36%). Of those reporting a mental health treatment need, 68% were receiving some form of mental health treatment.
Overall, a slightly higher proportion of girls who needed mental health treatment were receiving a form of mental health treatment when they started substance misuse treatment compared to boys (70% compared to 66%).
The most common treatment type was from community or other mental health services (56%). Figure 6 shows that 773 girls and 895 boys were engaging with community or other mental health services while in treatment in 2020 to 2021. Smaller numbers received mental health treatment from a GP (108 girls and 110 boys) or within drug or alcohol services (40 girls and 55 boys).
Some young people also received other mental health treatment, either within a health-based place of safety (19 girls and 16 boys) or by engaging with Improving Access to Psychological Therapies (13 girls and 17 boys).
However, 412 girls and 554 boys (32% overall) had a mental health treatment need identified but either did not receive treatment or refused treatment.
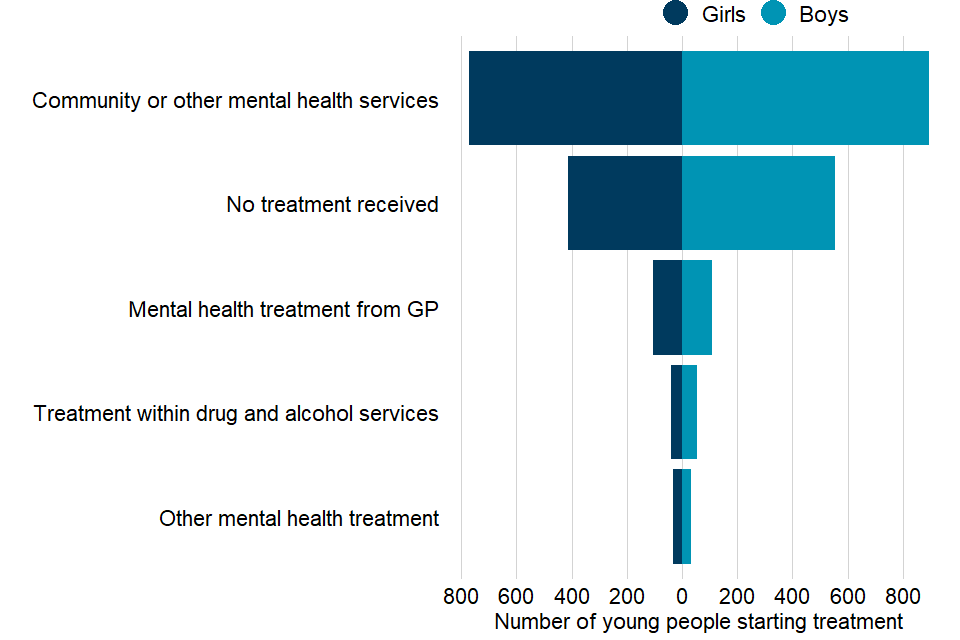
Figure 6: mental health treatment received by young people in alcohol and drug treatment
8. Treatment types
Most young people in treatment received a psychosocial intervention (10,881 of 11,013, 99%). The small number who did not receive an intervention probably entered treatment at the end of the time period covered by this report, and so had not started their intervention yet. Psychosocial interventions (also known as talking therapies) use psychological, psychotherapeutic and counselling skills to encourage behaviour change.
Structured harm reduction interventions are a type of psychosocial intervention. They involve support to manage risky behaviours associated with substance misuse. This might include behaviours that can cause overdose or accidental injury, for example injecting and poly-substance use. In 2020 to 2021, 7,174 young people (66% of those receiving an intervention) received a harm reduction intervention.
Only 28 young people in treatment (less than 1%) received a pharmacological intervention during treatment. These interventions involve medication prescribed by a clinician and can include detoxification, stabilisation, relapse prevention, and substitute prescribing for opiates.
Almost all interventions were delivered in a community setting (98%). A small number of young people received interventions in other settings, such as at home, in residential rehab, or in an inpatient unit.
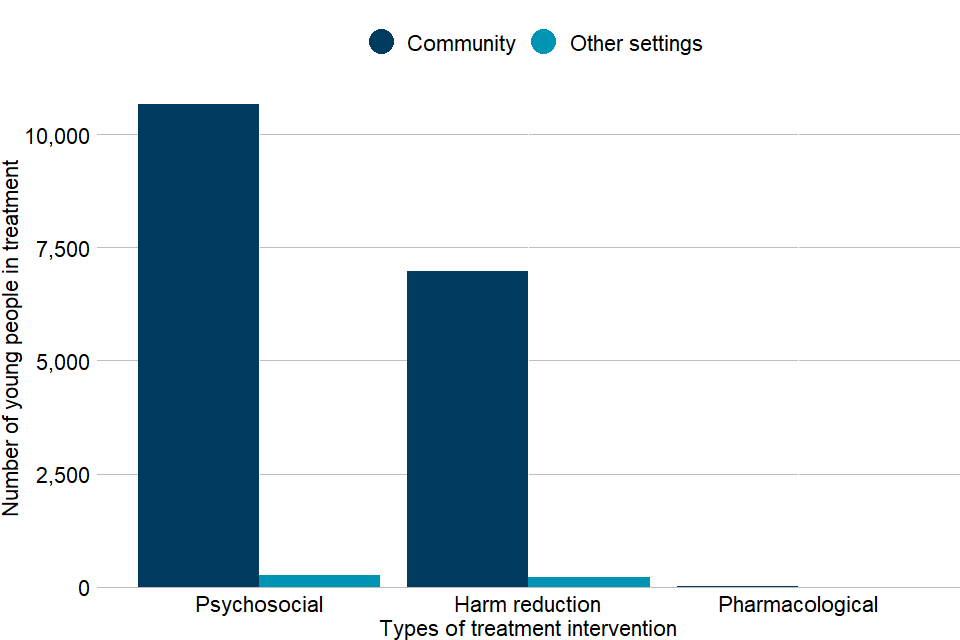
Figure 7: treatment types received by young people
9. Treatment exits
There were 7,237 young people who left treatment in 2020 to 2021. Of those who left, 5,725 (79%) successfully completed their treatment and 1,088 (15%) dropped out. A further 3% were referred to another provider for treatment and 2% declined the treatment offered.
| Treatment exit reason | % |
|---|---|
| Completed | 79.1 |
| Dropped out or moved away | 15.0 |
| Transferred to another substance misuse service | 3.5 |
| Treatment declined by client | 1.8 |
| Other | 0.4 |
| Prison | 0.2 |
Figure 8: treatment exit reasons
10. Trends over time
10.1 Trends in age and numbers in treatment
The number of young people attending specialist substance misuse services has fallen year-on-year since a peak of 24,494 in 2008 to 2009. The number of young people attending treatment services during 2020 to 2021 is 55% lower than this peak and 23% lower than the number in treatment in the previous year.
Data from the Smoking, Drinking and Drug Use among Young People in England survey showed a long-term decreasing trend in the proportion of school pupils reporting lifetime drug use until 2014. However, there was a significant increase in this proportion in 2016 and it remained similar in 2018.
Figure 9 shows the trends in the numbers and ages of young people in treatment since 2005 to 2006, split into 3 age groups:
- under 14 years old
- 14 to 15 years old
- 16 to 17 years old
The total number of young people coming to treatment increased from 17,105 in 2005 to 2006 to a high of 24,494 in 2008 to 2009. Since then, the numbers in treatment have steadily fallen until 2019 to 2020, which saw 14,291 young people in treatment. This year, we saw a slightly steeper fall to 11,013 young people in treatment.
The 3 age groups shown have largely followed these trends since 2005 to 2006 with the largest proportion being 16 to 17 year olds, followed by 14 to 15 year olds. The under 14 years old group makes up the smallest proportion year on year.
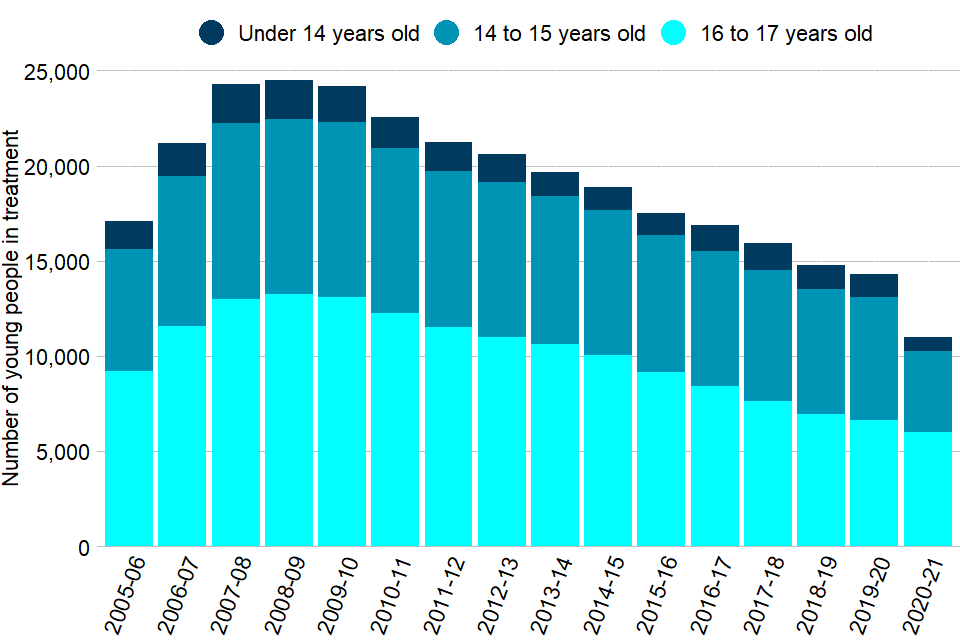
Figure 9: trends in age and numbers in treatment
10.2 Trends in recorded substance misuse
The proportion of young people in treatment who said that they had problems with cannabis has been between 85% and 90% since 2013 to 2014. The proportion who reported having alcohol problems has fallen steadily from a peak of 68% in 2008 to 2009 to 41% in 2020 to 2021. The proportion of young people in treatment whose main problem substance was something other than cannabis or alcohol has consistently been around 10% for the past 10 years of reporting.
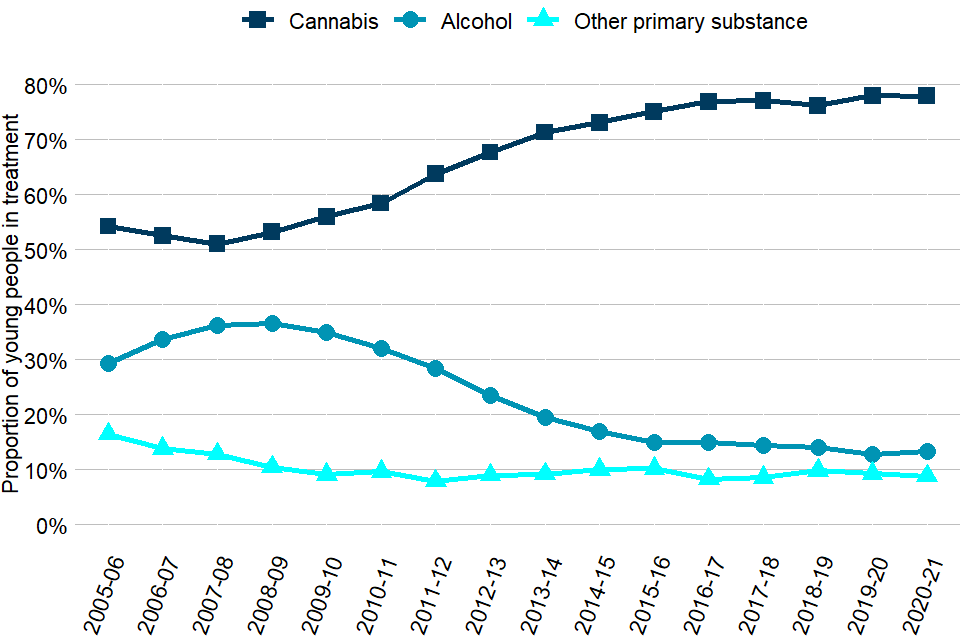
Figure 10: trends in primary substance
The proportion of people treated for ecstasy has fluctuated from around 10% between 2005 and 2008, decreasing to 4% between 2010 and 2012 before rising to a peak of 14% between 2017 and 2019. In 2020 to 2021, the proportion decreased to 12%.
The proportion of young people in treatment for amphetamine use decreased slightly between 2005 and 2010 before increasing quickly to a peak of 12% in 2012 to 2013. Since then, there has been a trend of decreasing proportions of young people in treatment for amphetamine use (1.1% this year).
Cocaine use among young people in treatment peaked in 2008 to 2009 (13%), falling to 7% in 2012 to 2013. Since this point, the number has remained similar year-on-year (8.9% this year). The number of young people reporting NPS has continued to fall. This was first reported on in 2013 to 2014 and rose to a peak of 6% in 2015 to 2016 before falling to under 1% in 2020 to 2021.
The number of young people in treatment for ketamine problems was consistently low (under 2%) between 2005 and 2018. It has since increased from under 1% in 2015 to 2016 to 5% in 2020 to 2021.
The proportion of young people who reported benzodiazepines as a problematic substance was also consistently low (under 1%) between 2005 and 2017. In 2020 to 2021 the proportion increased to 4% from 3% in the previous year. This was more than 5 times the proportion in 2013 to 2014 (less than 1%).
The proportions of young people seeking help for heroin has remained stable since 2017 to 2018. However, there have been recent increases in young people getting help for codeine (another opiate), with 1.2% this year, up from a low of 0.1% in 2014 to 2015.
The number of young people reporting solvent use has decreased by 0.5% this year compared to the previous year (from 3.3% to 2.8%).
The data tables for this year’s young people’s substance misuse treatment statistics also contain trends by the primary substance. This is the main substance that the young person reported problems with when they entered treatment.
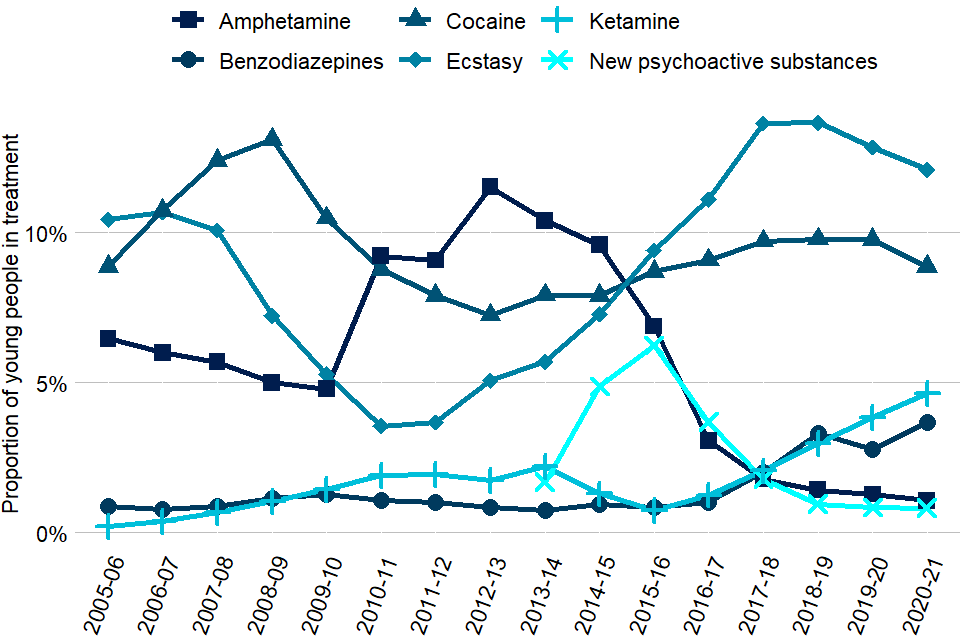
Figure 11: trends in substance misuse
11. Background and policy context
11.1 Background to the data
This report presents statistics on the availability and effectiveness of young people’s alcohol and drug treatment in England and the profile of those accessing treatment.
The statistics in this publication come from analysis of the National Drug Treatment Monitoring System (NDTMS). The NDTMS collects data from sites providing structured substance misuse interventions to young people in every local authority in England.
The data collected includes information on the demographics and personal circumstances of young people receiving treatment, as well as details of the interventions delivered and their outcomes.
You can find more details on the methodology used in the report in the NDTMS annual statistics quality and methodology information paper.
11.2 Policy context
Specialist substance misuse services for young people are normally separate from adult treatment services because young people’s alcohol and drug problems tend to be different from adults’ and need a different response. This includes:
- being child-centred
- considering the age and maturity of young people
- acting on safeguarding concerns
- making sure the young people do not mix with adults who use drugs
These services support young people, help them to reduce the harm their alcohol or drug use causes them and try to prevent it from becoming a bigger problem as they get older. Services should be part of a wider network of local prevention services that support young people with a range of issues and help them to build their resilience.
Young people’s alcohol and drug treatment in England is commissioned by local authorities using the public health grant. They are responsible for assessing local need for treatment and commissioning a range of services and interventions to meet that need.
The public health grant conditions make it clear that:
A local authority must, in using the grant: have regard to the need to improve the take up of, and outcomes from, its drug and alcohol misuse treatment services based on an assessment of local need and a plan which has been developed with local health and criminal justice partners.
The Office for Health Improvement and Disparities works with local authorities and provides them with bespoke data, guidance, tools and other support to help them commission services more effectively.
Guidance for alcohol and drug treatment is available in the Alcohol and drug misuse prevention and treatment guidance collection.
A wide range of NDTMS data is available on the NDTMS website, including some data reports that are only available to local authority commissioners (via login).
The government recently published its 10-year strategy for drug treatment and prevention, which included actions and funding for young people’s treatment.
Young people’s substance misuse services need to ensure that they are responding appropriately to child sexual exploitation. Public Health England published guidance on how public health leaders can prevent and intervene early in cases of child sexual exploitation.
