JUNIPER: Control options for mitigating a rapid rise in infection, 12 October 2021
Updated 13 May 2022
- Matt Keeling1,2
- Jonathan Read 1,3
- Edward Hill1,2
- Thomas House1,4
- Louise Dyson1,2
- Mike Tildesley1,2
- Rob Challen1,5
- Joint UNIversities Pandemic and Epidemiological Research
- The Zeeman Institute for Systems Biology & Infectious Disease Epidemiology Research, School of Life Sciences and Mathematics Institute, University of Warwick, Coventry, UK.
- Lancaster Medical School, Faculty of Health and Medicine, Lancaster University, UK.
- Department of Mathematics, University of Manchester, UK.
- College of Engineering, Mathematics and Physical Sciences, University of Exeter, Exeter, Devon, UK.
Here we consider 3 potential causes of a steep rise in infections, hospital admissions and deaths, and the merits of a range of control options that could be enacted to control the rise. We first summarise methods of control, before thinking how these could be effective against a steep rise in cases. For relatively moderate needs, the government has already set out Plan B – which includes the potential use of vaccination certification, the reintroduction of masks in specific settings and working from home. All of these will reduce the spread of infection, but are unlikely to overcome a rapid increase. We therefore focus on other measures and consider their action over different time-scales and when faced with different causes of a spike in infections.
Methods of control
Below we consider 7 methods of reducing COVID-19 disease, and rank these in order of time-scales, with processes that will take longer (but have a lasting impact) listed first, with measures that are more immediate (but less sustainable) listed last.
1. Improved ventilation in schools and workplaces. For infections where there is a significant amount of airborne transmission, good ventilation is known to help reduce the transmission risk [footnote 1] - thereby reducing R within the workplace. Although providing adequate ventilation in enclosed areas of the workplace is a legal requirement of employers, large-scale improvements to ventilation are not a rapid solution to increasing cases – although they could form part of a longer-term control initiative, and have the advantage that they are likely to reduce the transmission of many respiratory pathogens.
2. Improved public awareness. The historical response of the general public to the COVID-19 pandemic has shown that the behaviour of individuals can have a profound impact on the transmission of infection (Figure 1). Avoiding crowded areas, 2 metres distancing, proper mask use, and good hand hygiene all contribute to reducing onward transmission; similarly, isolating at the first signs of feeling unwell can also play a major role by reducing contact between symptomatic and susceptible individuals. It is likely that improved public behaviour will arise spontaneously if there is a spike in cases, but it is difficult to predict the scale of any behavioural response. Similarly, it is difficult to forecast the likely impact of renewed public-health advice. Increased public awareness of hospital capacity status, including non COVID-19 pressure, rate of cancelled operations, ITU bed occupancy and so forth, is also likely to play a role in modifying people’s attitude to infection risk.
3. Boosters and increased vaccine uptake. Ultimately, the only long-term pharmaceutical solution against COVID-19 is to generate sufficient immunity in the population, especially within groups that are most vulnerable, via boosters to combat waning vaccine efficacy (VE) or measures targeted at increasing vaccine uptake in particular socio-demographic groups where there may be increased vaccine hesitancy. Spatial variation in vaccine uptake is likely to lead to pockets of persistent infection that have the potential to general local epidemic spikes as control measures are relaxed. While vaccination is an effective long-term solution, the time-scales involved are often relatively long given the logistical issues involved in the mass-vaccination of the population - the Autumn 2021 booster campaign is likely to last around 100 days.
4. Test, Trace and Isolate (TTI) has remained a constant part of the pandemic response, with both empirical studies and theory making it clear that this can have substantial impact on transmission dynamics. This is illustrated by the ‘pingdemic’ (Figure 1), which although not fully understood was probably due to a high percentage of ‘mixers’ being required to isolate coupled with a population reaction to the preceding rise in cases, leading to a substantial decline in infection rates over a very short time-scale. Being able to recreate this effect would have substantial epidemiological impact. It is likely that returning to a 5-day (rather than 2-day) notification window in which tracing occurs would lead to a drop in infection if compliance could be maintained. Other factors that could be altered to increase the impact of TTI strategy include frequency and breadth of uptake of regular asymptomatic testing via LFD (or in some cases qPCR), which symptoms are used to trigger a test, and whether isolation requirements follow a positive LFT or only a positive PCR test.
5. Changes to restrictions and potential lockdowns. Restricting social mixing is known to change the epidemic growth rate, from national lockdowns, to limits on social gatherings, to encouraging working from home where possible. Both of the main lockdowns of March to April 2020 and January to February 2021 were associated with less mixing (Figure 1) which pushed an increasing epidemic into decline . We therefore know that implementing broad restrictions on social mixing is an effective solution – though ultimately a short-term one. For more limited measures, we expect there to be considerable hysteresis in the system; for example, the rate of population mixing that occurred after 12 April when moving into Step 2 from Step 1, may not necessarily be the same as the mixing that would happen if Step 2 regulations were reintroduced as a control measure in the future. As common with all epidemiological systems, there are substantial benefits from reacting quickly and strongly, reducing measures later if needed.
6. Antivirals [footnote 2] and pharmaceuticals. During the pandemic there have been a number of pharmaceutical improvements in the treatment of COVID-19 and the reduction of the most severe symptoms [footnote 3]. It is unknown if the currently available antivirals could also block infection or limit transmission, and it is too early to consider using these prophylactically - but future strategies could utilise antivirals in a similar manner to pandemic influenza if deemed cost effective. The most recent antivirals could be used to suppress the number of ICU admissions and deaths following a detected wave of cases.
7. Travel restrictions. Tighter border restrictions are unlikely to have a significant impact once cases have begun to noticeably increase in the UK. Such restrictions would only be highly effective before the event, if a novel variant of concern was identified elsewhere in the world. Although travel restrictions can at best buy some time before a novel variant arrives in the UK, this time could allow for vital preparations.
Increase due to novel variant
Novel variants pose a major risk to the UK and could easily lead to an abrupt increase in cases. Two scenarios are of greatest concern:
(i) the emergence of a new variant with greater transmission potential than Delta. The spread of first Alpha and then Delta was due to an increased transmission advantage (see Figure 2), and there is no reason to assume that the SARS-CoV-2 virus has reached its theoretical limit – other variants could arise with even higher basic reproductive ratios.
(ii) the emergence of a new variant with (partial) vaccine escape properties (Figure 3). Much of the UK’s current population immunity comes from vaccination; a variant that could overcome this immunity would have a fitness advantage and could spread rapidly through the population. As the UK continues to vaccinate and individuals return to pre-COVID-19 rates of mixing there is an increased evolutionary pressure for vaccine escape variants to emerge. Very high prevalence in schools combined with partly vaccinated 12- to 16-year-olds in a highly mixing population provides ideal conditions for vaccine escape emergence.
Non-pharmaceutical interventions, NPIs, (from ventilation to restrictions) are likely to be effective against all future variants, as they operate at fundamentally blocking infection. LFD tests target the N protein, which has so far not been subject to sufficient mutation to cause problems, and while we have seen the PCR S protein target fail, since most PCR machines use multiple targets (for example N and ORfab as well as S) it is also not expected that significant evasion of testing will be a problem for new variants. However pharmaceutical measures (including vaccination) may need to be adjusted to account for differences - this is likely to be a time-consuming process and hence NPIs will be needed until other solutions can be developed. For the UK, the emergence of a vaccine escape mutant is potentially the worst-case scenario, reversing the gains from vaccination over the last 10 months.
Increase due to waning immunity
There is now good evidence of waning vaccine efficacy, especially in older individuals due to their weaker immunity and the longer time that has elapsed since they were vaccinated. Although the vaccine efficacy against severe disease remains high, it should be noted that a small change can generate a major shift in hospital admissions (for example, a change from 95 per cent to 90 per cent VE against hospitalisation would lead to doubling of admissions). Similarly, there is also some evidence of waning immunity from natural infection, although this is less readily quantified and may be due to partial immunity between variants. The UK is already introducing booster vaccines to offer increased protection to the elderly and vulnerable age groups.
A substantial rise in infection or hospital admissions could be due to one of 2 sources:
(i) reduction in protection of the most vulnerable placing them at greater risk of severe disease
(ii) reduction in protection of the general population, leading to a greater transmission risk to the most vulnerable. These would require different targeting of vaccine boosters
Non-pharmaceutical interventions are likely to be effective in controlling waning immunity, on the basis they were effective in 2020 before vaccination began.
Increase due to behaviour change
Population behaviour is the main driver of epidemiological transmission, and has varied throughout the pandemic due to regulations (such as lockdown restrictions) and reaction to the epidemiological situation. As such, changes in population behaviour are the most likely cause of a new rise in cases (with a subsequent rise in hospital admissions and deaths).
The greatest risk is as we enter colder winter months (as natural ventilation becomes less appealing); a decrease in working from home, greater mixing within school cohorts and university student age-groups (and where vaccination uptake is relatively low), less physical distancing, less mask-use, a decline in testing and the opportunity to redress the restrictions of last Christmas season could all generate the perfect storm. Our model predictions suggest that a complete return to pre-pandemic behaviour could increase R by around 75% (Figure 2).
While all control measures should work well against changes in behaviour, such changes are capricious in nature. A sudden rise in hospital admissions or deaths may catalyse a greater public reaction than government advice could produce; therefore spikes in cases due to changes in public behaviour may be ‘self-limiting’ and short-lived - although this should not be relied upon..
Summary table
Drivers of epidemic growth
| Control Measure | Driver of epidemic growth: Novel variant | Driver of epidemic growth: Waning immunity | Driver of epidemic growth: Behaviour change |
|---|---|---|---|
| Ventilation | A long-term measure that can have a lasting impact against multiple infections. Increased ventilation could drive down transmission, but is unlikely to get substantial uptake in the colder months. | A long-term measure that can have a lasting impact against multiple infections. Increased ventilation could drive down transmission, but is unlikely to get substantial uptake in the colder months. | A long-term measure that can have a lasting impact against multiple infections. Increased ventilation could drive down transmission, but is unlikely to get substantial uptake in the colder months. |
| Public behaviour | Effective but difficult to influence, may be an emergent property of a response to increasing infection. | Effective but difficult to influence, may be an emergent property of a response to increasing infection. | Unlikely to have an immediate impact, if change is driven by behaviour. |
| Vaccination | Effective vaccine may not be available for several months. | Effective but time-scale of vaccination may take months. | Unlikely to have a major impact. |
| Test-Trace-Isolate | Can work extremely well, but efficacy depends strongly on how the system is designed and implemented. Main negative is large economic cost of infrastructure (but anticipated to be much lower than lockdown). | Can work extremely well, but efficacy depends strongly on how the system is designed and implemented. Main negative is large economic cost of infrastructure (but anticipated to be much lower than lockdown). | Can work extremely well, but efficacy depends strongly on how the system is designed and implemented. Main negative is large economic cost of infrastructure (but anticipated to be much lower than lockdown). |
| Restrictions or lockdown (see Figure 4) | A rapid, short-term and an imprecise tool. Restrictions are known to work, but are not a long-term solution. Could be used to rapidly mitigate a sudden spike in infection and ease pressure on healthcare facilities. | A rapid, short-term and an imprecise tool. Restrictions are known to work, but are not a long-term solution. Could be used to rapidly mitigate a sudden spike in infection and ease pressure on healthcare facilities. | A rapid, short-term and an imprecise tool. Restrictions are known to work, but are not a long-term solution. Could be used to rapidly mitigate a sudden spike in infection and ease pressure on healthcare facilities. |
| Pharmaceuticals | Pharmaceuticals may have reduced efficacy against novel variants. | Most likely only reduces severity, not transmission with the current antivirals. | Most likely only reduces severity, not transmission with the current antivirals. |
| Travel restrictions | Only effective if the variant is identified elsewhere in the world. | Unlikely to have any benefit. | Unlikely to have any benefit. |
Exemplar figures from the Warwick inference and model
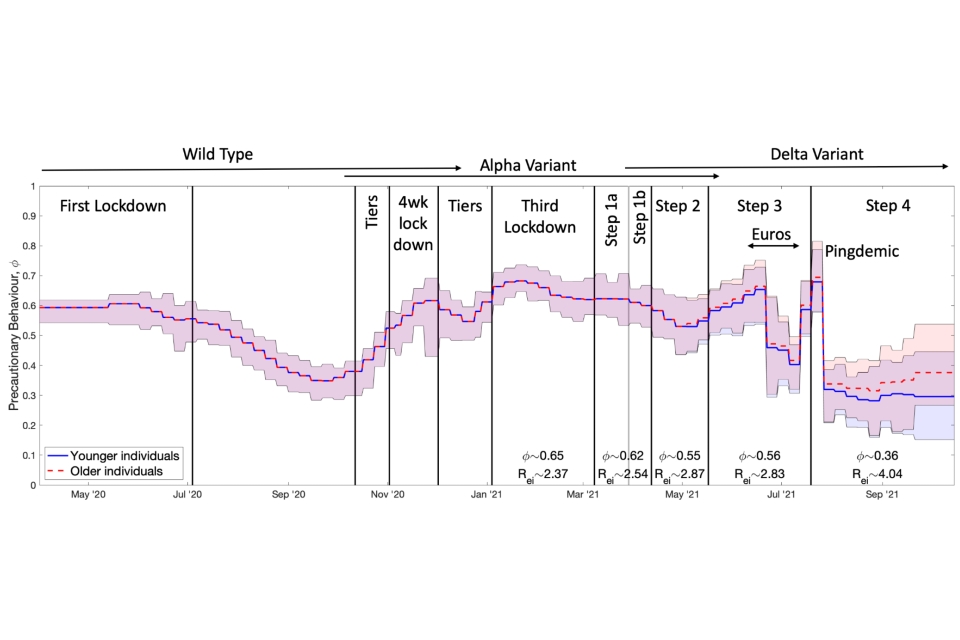
Figure 1: Inferred precautionary behaviour, phi, over time together with the different periods of restrictions and the variants in circulation. Solid lines show the mean values while shaded areas cover the 95 per cent credible intervals; mean values of phi and the associated value of Rei for the Delta variant over the different periods in 2021 are written on the lower part of the graph. Rei is the value of R excluding immunity calculated from the growth rate with a given level of precautionary mixing but assuming everyone is susceptible to infection. The blue line shows the inferred values for the younger population (less than 40) while the red dash line shows the inferred values for the older population (over 60), with both assumed equal before May 2021. Ages between 40 and 60 take values between the 2 inferred levels, increasing with age. Values of phi are generally assumed to vary slowly (exceptions are set based on observed behaviour such as during the EURO 2020 football tournament and subsequent pingdemic) and remain constant over a week.
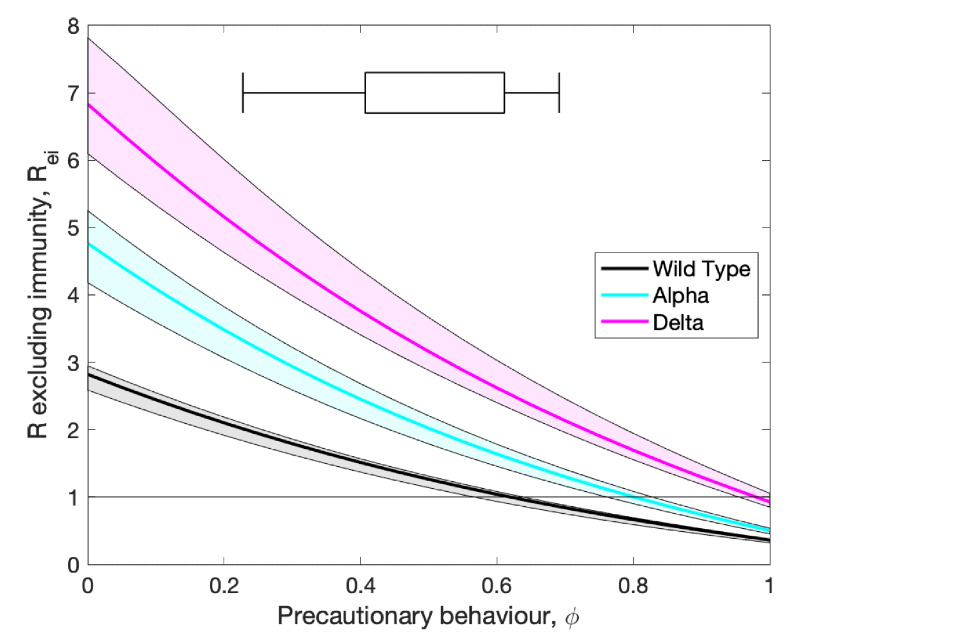
Figure 2: Inferred values of R excluding immunity (Rei) against the level of precautionary behaviour, phi, for the wild type virus and 2 main variants of concern in the UK: Alpha and Delta. The line is the mean value while the shaded regions show 95% prediction intervals. The horizontal error bar shows the 95% and 50% interval on values of phi since 23 March 2020.
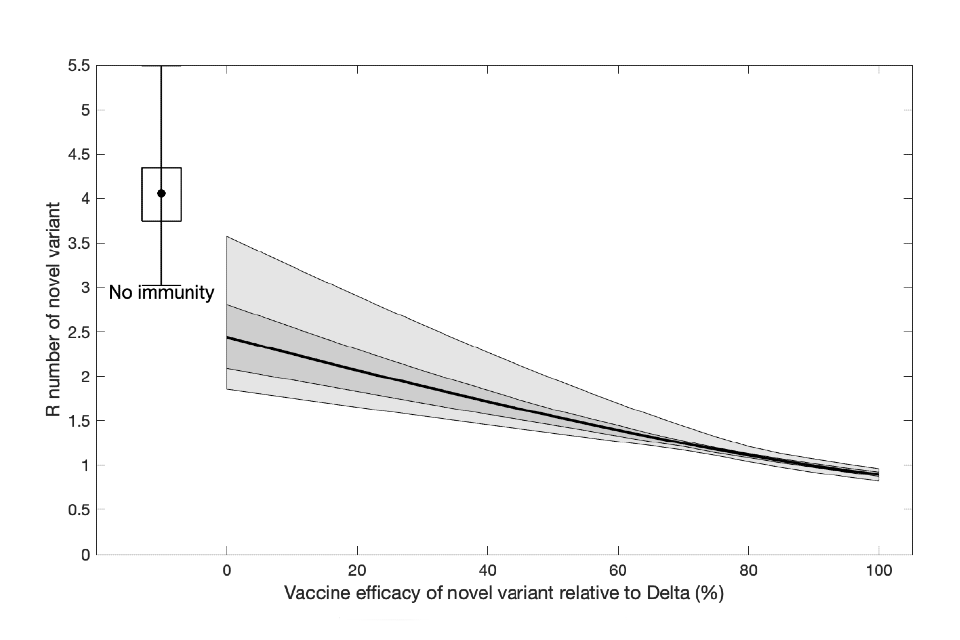
Figure 3: Implications of a vaccine escape variant on the estimated R number. Assuming a novel variant with partial vaccine escape properties invades the UK in November 2021, we calculate the reproductive number of this variant (under the assumption that there is repeated waning of immunity after boosting, and combining 3 assumptions for the asymptotic level of vaccine efficacy). The x-axis gives the level of vaccine efficacy against the new variant compared to the Delta variant. The solid line shows the mean values, while the shaded regions are the 50% and 95% prediction intervals. For comparison, the single error bar shows the implications of a variant that completely escapes both infection-derived and vaccine-derived immunity.
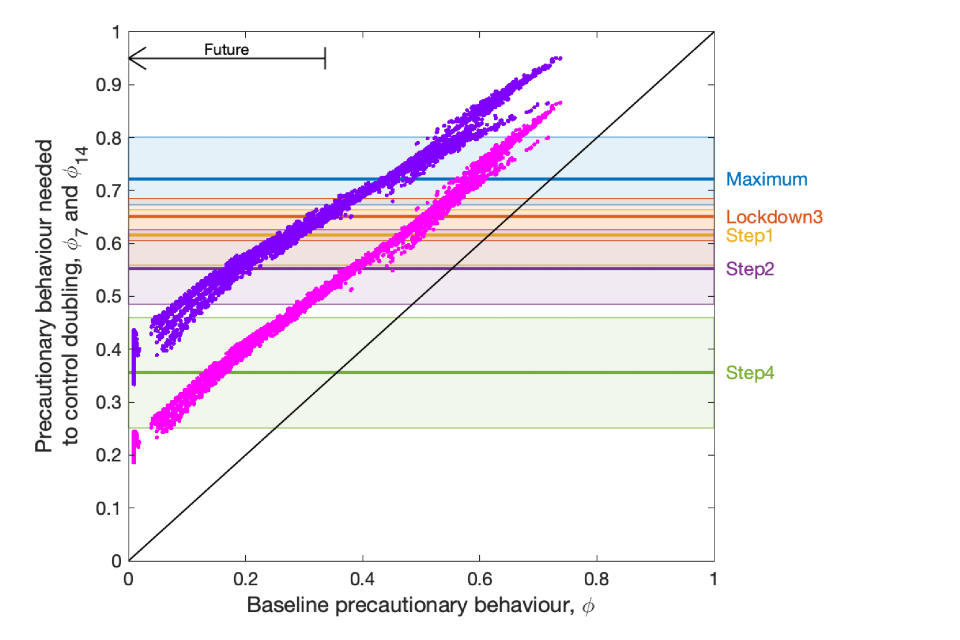
Figure 4: For a given baseline level of precautionary behaviour at each time-point in the epidemic (x-axis) we assume that a change has occurred that leads to a doubling of infection every week (purple, top set of points) or every 2 weeks (pink, lower set of points), and assess the level of precautionary behaviour needed to bring the growth rate back to zero (y-axis). The arrow indicates the values of precautionary behaviour below the current level that we expect to observe into the future. Horizontal lines (together with 95% credible intervals) correspond to values inferred for different periods of 2021.
