Health matters: preventing Type 2 Diabetes
Published 24 May 2018
Summary
This professional resource outlines how to optimise the NHS Diabetes Prevention Programme (NHS DPP) in order to identify those already found to be at risk of developing Type 2 diabetes and offer support that will help them reduce their risk of developing the disease.
Scale of the problem
Diabetes is a non-communicable disease (NCD) where the amount of glucose in the blood is too high. Type 1 diabetes is an autoimmune disease whereby the body is unable to produce any insulin, and Type 2 diabetes develops when the body stops producing enough insulin or the body’s cells stop reacting to insulin produced.
Type 2 diabetes is associated with lifestyle factors – being overweight or obese is the major modifiable risk factor for Type 2 diabetes. The onset of Type 2 diabetes can be delayed or prevented through support to change behaviour around lifestyle choices. Type 1 diabetes is not related to lifestyle issues, and at this point cannot be prevented.
The global burden of diabetes
Globally, an estimated 108 million adults were living with diabetes in 1980, and by 2014 this figure had almost quadrupled to 422 million adults; an increase in global prevalence from 4.7% in 1980, to 8.5% in 2014. This is largely due to the rise in Type 2 diabetes, which is estimated to account for 90% of all diabetes cases in the UK. The growing overweight and obesity epidemic is a major driver behind this rise in Type 2 diabetes.
According to the World Health Organisation (WHO), diabetes was the sixth highest cause of global death in 2015. There were an estimated 1.6 million deaths from diabetes in 2015, which included deaths from complications and other diseases that arose from high blood sugar.
The national burden of Type 2 diabetes
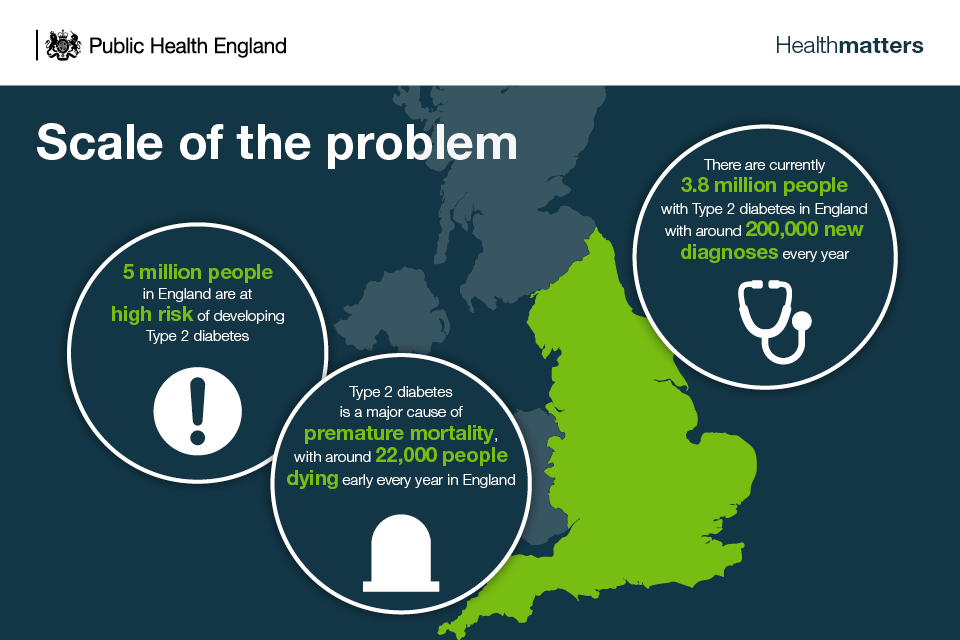
Type 2 diabetes is a major cause of premature mortality, with around 22,000 people with diabetes dying early each year in England. It is often not Type 2 diabetes itself that causes death, but complications of the disease, including cardiovascular disease (CVD).
The condition is progressive, requiring action at the population and individual level to support changes in lifestyle, particularly diet and physical activity. It also requires oral drugs and insulin for most people over time.
Risk factors for Type 2 diabetes
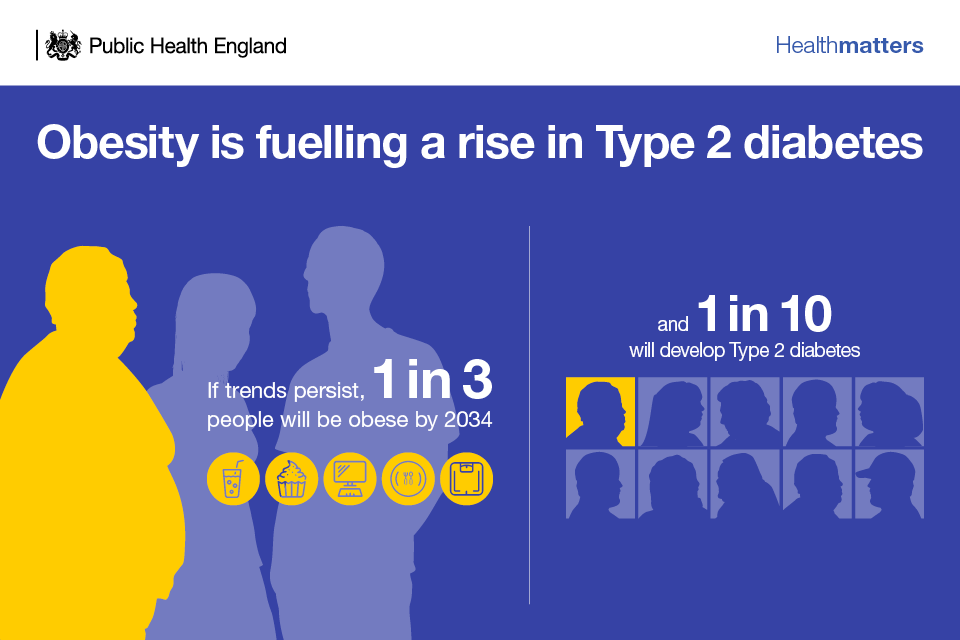
The obesogenic environment and associated lifestyle risk factors
The increasingly obesogenic environment we live in makes it harder for individuals to avoid unhealthy lifestyle choices. The obesogenic environment can be considered to be at the root of the prevention challenge in Type 2 diabetes.
From childhood, people are exposed to ultra-processed, energy-dense, nutrient-poor foods, which are cheap and readily available. Opportunities for physical activity, both in and out of school and the workplace, have been reduced and more time is spent on screen-based and sedentary leisure activities. As a result, high proportions of children and adults have increasingly been defaulting to unhealthy lifestyle choices including unhealthy diets, low levels of physical activity, and sedentary behaviour. These all give rise to higher risk of Type 2 diabetes:
- overweight or obesity with a body mass index (BMI) of 25 or more
- a large waist circumference – more than 80cm or 31.5 inches in women and 94cm or 37 inches in men
Therefore, being overweight or obese is the main modifiable risk factor for Type 2 diabetes, with the likelihood of developing the disease and the risk of complications being closely linked to BMI. There is a 7 times greater risk of diabetes in obese people compared to those of a healthy weight, and a threefold increase in risk for overweight people. Severely obese people, with a BMI of 40 or over, are at an even greater risk than obese people with a lower BMI ranging from 30 to 39.9.
Whilst it is known that body fat distribution is an important determinant of increased diabetes risk, the precise mechanism of the association between obesity and Type 2 diabetes remains unclear. It is also uncertain why not all people who are obese develop Type 2 diabetes, and why not all people with Type 2 diabetes are obese.
A large waist circumference is also a preventable risk factor, which often coincides with obesity. Men with an increased waist circumference are 5 times more likely and women are over 3 times more likely to have diagnosed Type 2 diabetes than those without a raised waist circumference.
Deprivation
Individuals from more deprived backgrounds face greater challenges in making healthier lifestyle choices.
Deprivation and low socioeconomic status are closely associated to heightened risk of obesity. Data from the Health and Safety Executive shows that in 2014 in the most deprived quintile compared to the least, obesity was 13% and 50% higher for men and women, respectively.
Prevalence of Type 2 diabetes is 60% more common among individuals in the most deprived quintile compared with those in the least deprived quintile in England.
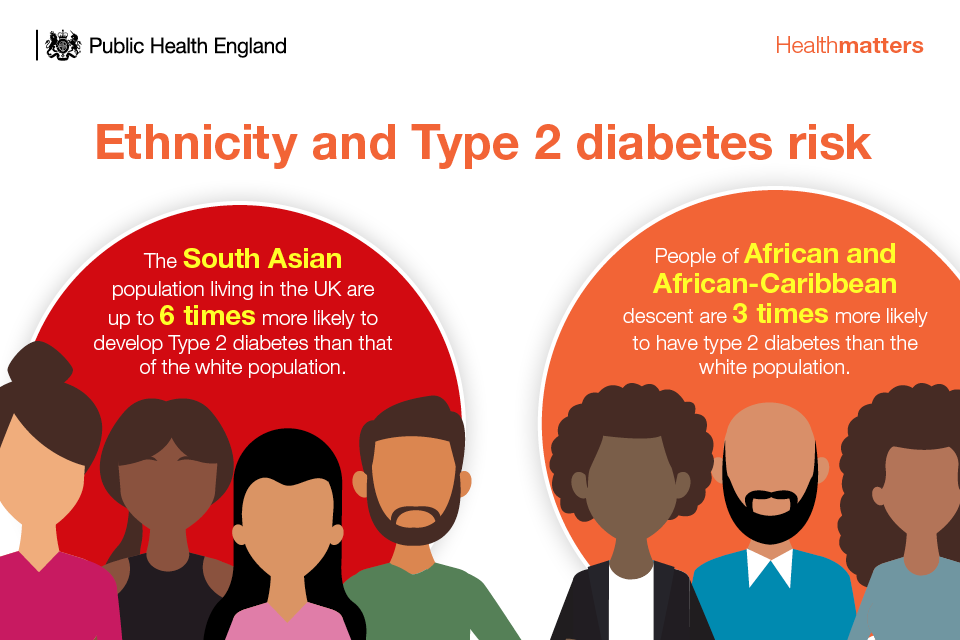
Demographic and medical history risk factors
In addition to modifiable risk factors associated with the obesogenic environment and associated lifestyles, there are risk factors related to ethnicity and medical history, which cannot be controlled or prevented, including:
- a family history of Type 2 diabetes
- age – being older than 40 or older than 25 for some black and minority ethnic (BME) groups
- certain ethnicities
Health impact of Type 2 diabetes
Those who develop Type 2 diabetes are subsequently at greater risk of developing complications from the disease:
Macrovascular complications
- CVD including heart attack and stroke – Type 2 diabetes leads to a 2 fold excess risk of CVD
Microvascular complications
- blindness – diabetic retinopathy is the leading cause of preventable sight loss among people of working age in England and Wales
- nerve damage
- kidney disease and failure
- peripheral neuropathy
- diabetic foot disease
Mental health and social consequences
A Type 2 diabetes diagnosis can also negatively impact quality of life and social contact, which can have an adverse effect on mental health. Depression is more prevalent among people living with Type 2 diabetes, compared with those who are not. This, as well as many other complications of Type 2 diabetes, increases their risk of premature death.
A survey conducted by Diabetes UK also found that:
- 3 in 5 people (64%) living with diabetes experience emotional or mental health problems as a result of their condition
- just 3 in 10 people living with diabetes said they definitely felt in control of their condition
- nearly a third of people living with diabetes had at some point relied on self-help materials
- one in 5 people living with diabetes had used support or counselling from a trained professional to help them manage their diabetes
There is also evidence that minor psychological morbidities lower adherence to Type 2 diabetes treatment, which can have knock-on effects on patients’ health.
In addition to mental health and quality of life, the important social consequences of Type 2 diabetes include impacts on individuals’ family life, education and employment. Whilst these factors are typically under-recognised in health research, from a public health perspective they are wider consequences that are just as important as health outcomes. They also tend to be highlighted as important by people living with Type 2 diabetes, as they have far-reaching impacts.
Diabetic foot disease
Diabetic foot disease is a potential consequence of the microvascular complication of peripheral neuropathy and the macrovascular complication of peripheral vascular disease.
Latest figures show that between 2014/2015 and 2016/2017, there were 132,114 hospital spells for diabetic foot disease. The median length of stay in hospital was 8 days and the total number of days spent in hospital for diabetic foot disease was 1,730,072.
There were 7,305 major amputation procedures performed, giving a directly age and ethnicity standardised rate of 8.2 major amputations per 10,000 population-year. This is one of the lowest amputation rates worldwide.
Costs to the NHS and wider economy
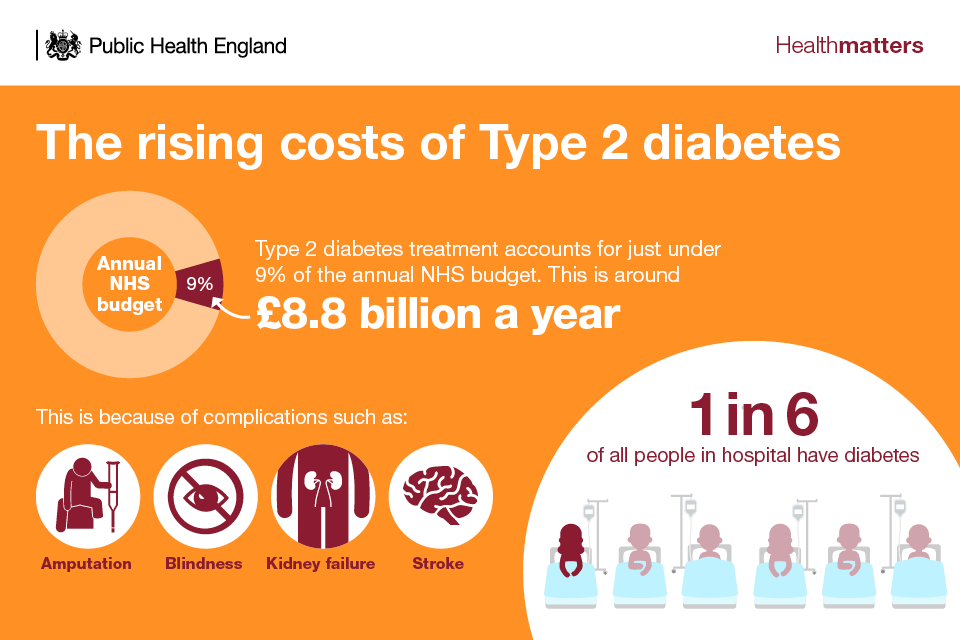
80% of the direct costs are related to the complications of Type 2 diabetes. There are also major indirect costs, such as loss of productivity due to increased death and illness and the need for informal care. It is estimated that in 2010 to 2011, indirect costs in the UK were approximately £13 billion.
The national response to diabetes prevention
The national response to diabetes prevention includes multiple different behavioural interventions that address lifestyle choices that lead to individuals being at high risk of developing Type 2 diabetes. This edition of Health matters will focus specifically on the Healthier You: NHS Diabetes Prevention Programme (NHS DPP).
Healthier You: NHS Diabetes Prevention Programme
The NHS DPP is a joint commitment from PHE, NHS England and Diabetes UK. The Programme, launched in 2015, delivers evidence based behavioural interventions at scale for individuals identified as being at high risk of developing Type 2 diabetes.
The NHS DPP is underpinned by a strong evidence base. PHE has published a systematic review and meta-analysis examining the effectiveness of diabetes prevention programmes.
The goals of the NHS DPP are to:
- reduce the incidence of Type 2 diabetes
- reduce the incidence of complications associated with Type 2 diabetes – heart, stroke, kidney, eye and foot problems related to diabetes
- reduce health inequalities associated with incidence of Type 2 diabetes, over the longer term
In the short-term, the Programme recognises that a stronger focus on identifying people who are at risk of diabetes is likely to increase recorded incidence of diabetes as more undiagnosed cases are uncovered. This is important to recognise as it is possible to live for some time with undiagnosed Type 2 diabetes; in 2015, an estimated 900,000 people had Type 2 diabetes but were undiagnosed.
There is strong international evidence that demonstrates how behavioural interventions, with a focus on supporting people to maintain a healthy weight and be more active, can significantly reduce the risk of developing Type 2 diabetes. The NHS DPP behavioural intervention reflects this evidence, as it is underpinned by 3 core goals:
- achieving a healthy weight
- achievement of dietary recommendations
- achievement of the Chief Medical Officers’ (CMO) physical activity recommendations
Dr Jonathan Valabhji outlines the aims of NHS Diabetes Prevention Programme
Dr Jonathan Valabhji outlines the aims of NHS Diabetes Prevention Programme
Who is eligible?
The NHS DPP provides a behavioural intervention for individuals aged 18 years or over with nondiabetic hyperglycaemia (NDH), which is defined as having an HbA1c of 42 to 47 mmol/l or 6.0 to 6.4% or fasting plasma glucose (FPG) of 5.5 to 6.9 mmol/l. These individuals are at high risk for progression to Type 2 diabetes. The blood result indicating NDH must be within the last 12 months to be eligible for referral.
Individuals with blood glucose levels in the normal range (HbA1c less than 42 mmol or less than 6.0%) and those with a diagnosis of Type 2 diabetes are not eligible for the NHS DPP intervention. A diagnosis requires 2 separate blood tests within the diabetic range (HbA1c greater than or equal to 48 mmol or FPG greater than or equal to 7 mmol/l).
Dr Jonathan Valabhji describes how the NHS Diabetes Prevention Programme is reaching those most at risk
What is involved?
The intervention consists of a series of predominantly group-based sessions delivered in person across a period of at least 9 months. There are at least 13 sessions, lasting between 1 and 2 hours, and at least 16 hours of contact time.
Each session covers topics geared towards the Programme’s main goals of weight reduction and improved glycaemic control through dietary improvements, and increased physical activity and reduction in sedentary behaviour. They are underpinned by behavioural theory and involve the use of behavioural techniques.
NHS DPP coverage in England
In June 2016, the process for roll out of the NHS DPP began with a first wave of 27 areas covering 26 million people, half of the population in England, and making up to 20,000 places available. In April 2017, the Programme mobilised across a further 13 sustainability and transformation partnerships (STPs), achieving 75% population coverage in England.
The programme rolled out to all remaining clinical commissioning groups (CCGs) and local authorities (LAs) in England that were not previously included in the Programme, achieving full coverage from April 2018, with referrals due to start in July 2018. There have been over 185,000 referrals and over 78,000 taking up the programme to date.
Dr Jonathan Valabhji describes the roll out of the NHS Diabetes Prevention Programme
Dr Jonathan Valabhji describes the roll out of the NHS Diabetes Prevention Programme

Early outcome data and provisional analyses suggest that over 50% of the individuals that started the intervention completed it. Completion is defined as attendance to 62% or more of the Programme sessions, which is 8 out of 13 sessions in the curricula of most providers, aligning to the financial incentives for providers to retain participants on the programme.

Digital approach
A digital pilot of the NHS DPP was launched in November 2017 and referrals to digital services commenced in December 2017.
The digital stream offers an alternative service to face-to-face programmes, with the potential to widen access to diabetes prevention. It offers similar support, assistance and guidance using technologies, including wearables and apps. An estimated 5,000 people are expected to gain access to these digital interventions over the 18 to 24 month duration of the pilot.

The 8 digital pilot sites implementing digital services are:
- Buckinghamshire, Oxfordshire and Berkshire
- Bristol, North Somerset and South Gloucestershire
- Lancashire
- Salford
- Central and West London, Hammersmith and Fulham, Hounslow and Ealing
- North East London
- Somerset
- Humber Coast and Vale
Dr Jonathan Valabhji describes the digital stream of the NHS Diabetes Prevention Programme
Dr Jonathan Valabhji describes the digital stream of the NHS Diabetes Prevention Programme
The referral routes: identifying those who can benefit from the NHS DPP
Referral routes into the Programme vary according to local case finding pathways. Three primary mechanisms for referral are:
- the NHS Health Check Programme, which should be made available to 15.5 million eligible adults aged 40-74 years of age every 5 years. These checks should include a diabetes risk assessment or filter, which should lead onto blood testing for those identified at risk. Those people identified as having NDH should be offered a referral to the NHS DPP in accordance with the local protocol.
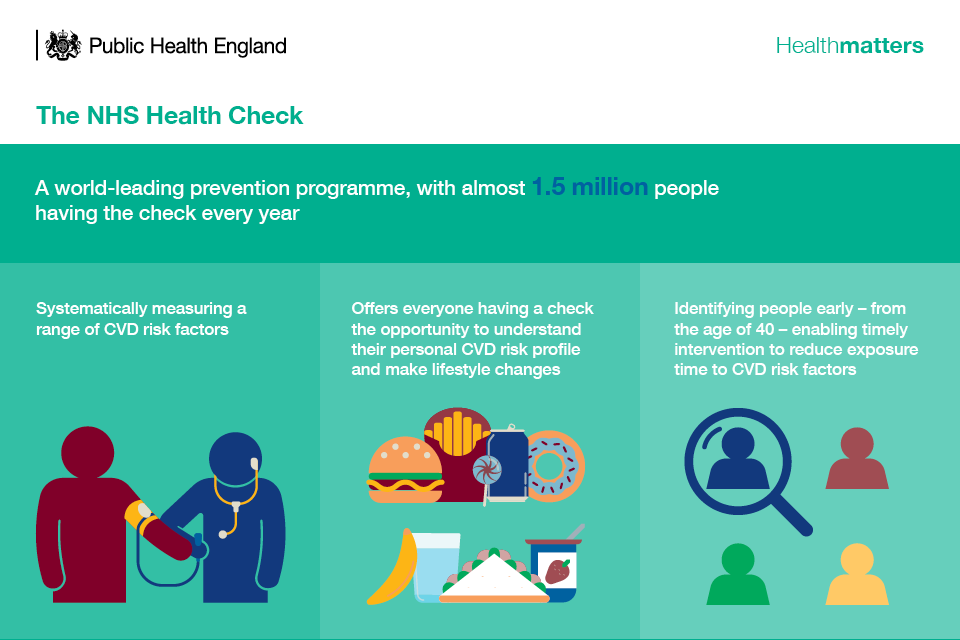
Find out more about the NHS Health Check Programme in this previous edition of Health Matters.
- those who have already been identified as having an appropriately elevated risk level (HbA1c or FPG) in the past and who have been included on a register of patients with high HbA1c or FPG
- those who are identified with NDH through opportunistic assessment as part of routine clinical care
Lifestyle interventions and national policies
National policies to tackle obesity and prevent Type 2 diabetes
The association between overweight and obesity and risk of developing Type 2 diabetes is well established. Therefore, it is crucial to tackle obesity as a means of preventing future cases of Type 2 diabetes.
The following national policies are predicated on acting on the obesogenic environment:
Calorie reduction programme
The calorie reduction programme challenges the food industry to achieve a 20% reduction in calories by 2024 in product categories that contribute significantly to children’s calorie intakes (up to the age of 18 years) and where there is scope for substantial reformulation and/or portion size reduction.
Although the programme focuses on foods consumed by children up to the age of 18 years, the programme is supporting all family members in reducing their calorie consumption, particularly with continued support through PHE’s OneYou and Change4Life campaigns. The OneYou campaign encourages adults to follow a simple rule of thumb: 400-600-600 – the number of calories to aim for at breakfast, lunch and dinner, with healthy snacks in between.
Sugar reduction programme
A broad, structured sugar reduction programme is being led by PHE to remove sugar from the products children eat most. All sectors of the food and drinks industry will be challenged to reduce overall sugar, across a range of products that contribute to children’s sugar intakes, by at least 20% by 2020, including a 5% reduction in year 1.
A soft drinks industry levy
The government’s childhood obesity plan outlined plans for a soft drinks industry levy across the UK, which was brought into law in April 2018. Sugary soft drinks provide 26% of the total sugar intakes for 11 to 18 years olds in England, according to the National Diet and Nutrition Survey. The Scientific Advisory Committee on Nutrition (SACN) recently concluded that sugar consumption increases the risk of consuming too many calories. In England, the revenue from the levy will be invested in programmes to reduce obesity and encourage physical activity and balanced diets for school age children.
PHE’s marketing campaigns
PHE has a number of national marketing campaigns that can be used at a local level to encourage people to improve their lifestyle behaviours. Downloadable content is available from the PHE Campaign Resource Centre.
Diabetes Prevention Week
NHS England, PHE and Diabetes UK launched the first Diabetes Prevention Week in April 2018. The week-long campaign raised awareness of Type 2 diabetes, the complications associated with it, high-risk groups, and how to prevent it.
A Diabetes Prevention Week toolkit was made available for GP practices and other local organisations to order for free from the PHE Campaign Resource Centre. This includes everything needed to host your own local diabetes prevention events and advertise your local NHS DPP service, from posters and leaflets, to briefing documents, videos and social media plans.
The week was a success, with nearly 5,000 toolkits ordered from practices across the country. We plan to make the week an annual event with the next Diabetes Prevention Week taking place in April 2019.
Call to action
It is important to have a smooth referral pathway that works hand in hand with the NHS DPP providers. To achieve this, the number of GP referrals must be realistic so that demand matches the providers’ supply capacity. This, in turn, can minimise waiting times and therefore minimise drop-off from the programmes.
This section outlines the specific actions that primary care professionals and local authorities can take to enable a successful referral process, and maximise the number of individuals identified as being at risk of Type 2 diabetes taking up and completing the NHS DPP.
Primary care providers
Primary care engagement is crucial for the effective implementation of the NHS DPP, as primary care professionals are required to identify individuals at high risk of developing Type 2 diabetes and refer them into the Programme. As such, their support to individuals is important to encourage take up and completion of the 9-month Programme.
There are a few simple steps primary care providers can take to ensure the Programme is successful, including:
- working closely with the diabetes clinical network and intervention providers
- making connections with NHS DPP providers to identify and promote wider community assets that can support people to achieve their goals
- considering the quality of referrals and whether individuals are sufficiently motivated to attend the Programme
- maintaining an up-to-date register of people with NDH
- conducting annual follow-ups and recording results, as per NICE guidelines, for all individuals in NDH category
- ensuring inclusion of a diabetes risk assessment in the NHS Health Check and providing follow-up blood tests for those identified as being at high risk
Application of behavioural insights
There are 3 key aspects of the NHS DPP that would benefit from the application of behavioural insights:
- uptake of diabetes prevention programmes
- retention to diabetes prevention programmes
- lifestyle change
The EAST framework, developed by PHE’s Behavioural Insights Team, is a simple framework for thinking about behaviour change that can be applied to the 3 key aspects of the NHS DPP listed above. The premise of the framework is to make the process ‘EAST’, which stands for Easy, Attractive, Social and Timely. PHE has published further advice on this.
Local authorities and Clinical Commissioning Groups (CCGs)
Identify and increase uptake to the programme
CCGs and local authority (LA) commissioners should work with their local voluntary sector to raise awareness and commission tailored lifestyle interventions to high risk BME communities.
NHS commissioners should work alongside LAs to increase uptake and identify those who could benefit from a NHS Health Check, as it includes a diabetes filter that pinpoints those at high risk of developing the condition.
CCGs and LAs will need to integrate the NHS DPP into the local care pathway, and work with providers to manage this process of referrals, including appropriate data processing and data sharing agreements where required.
NHS commissioners can use the NHS RightCare Diabetes Pathway which shows the core components of an optimal diabetes service, including risk detection using the NHS DPP.
Provide and deliver lifestyle interventions
Commissioners have a key role to play in ensuring that patients identified through the programme are offered lifestyle advice to achieve:
- a healthy weight
- dietary recommendations
- CMO physical activity recommendations
It is anticipated that the NHS DPP will encourage the uptake of other resources which should be made available in the local community such as:
- exercise classes
- walking groups
- swimming offers
- weight management programmes
PHE has a number of national marketing campaigns that can be used at a local level to encourage people to improve their lifestyle behaviours. Downloadable content is available from the PHE Campaign Resource Centre.
Population-level interventions to prevent diabetes
In the long term, it remains the case that to address obesity and therefore reduce the risk of Type 2 diabetes, local health economies (STPs, and community, voluntary and private sectors) must work together in implementing population-level approaches.
Specific guidance from NICE on approaches to working strategically on diabetes prevention at the population level is available (NICE guidelines PH35). This guidance covers specific steps to integrate local and national action, promote food and physical activity at the population level, and to target groups who9 are particularly at risk of developing diabetes.
You can also find out more about population-level interventions for obesity in the previous edition of Health matters.
Resources
Download references.
Download the Health matters infographics.
Read the Health matters blog.
Watch Health matters videos.
Download case study: Driving clinical engagement in diabetes prevention.
Download case study: Practice based nurse case finding approach.
Download case study: Marketing approaches to promote engagement.
Download case study: Targeted case finding approaches.
