Abdominal wall defects: exomphalos information for parents
Updated 9 March 2020
1. Overview
This information will help if your baby is suspected of having exomphalos (pronounced ‘ex-om-fa-los’) following your 20-week scan (sometimes referred to as the mid-pregnancy scan).
This is sometimes known as an omphalocele (pronounced ‘om-fuh-luh-seel’). We hope this information helps you and your health professionals talk through the next stages of your and your baby’s care.
This information should support, but not replace, discussions you have with health professionals. Finding out there may be a problem with your baby’s development can be worrying. It is important to remember you are not alone.
We will refer you to a specialist team who will do their best to:
- provide more accurate information about your baby’s condition and treatment
- answer your questions
- help you plan the next steps
2. About exomphalos
Exomphalos is an abdominal wall (tummy wall) defect. It happens when a baby’s abdominal wall does not develop fully while in the womb.
Early in all pregnancies, the baby’s intestine develops inside the umbilical cord. It usually moves inside the abdomen a few weeks later.
For babies with exomphalos, the intestines (and sometimes other organs like the liver) stay inside the umbilical cord and do not move inside the abdomen as they should.
2.1 Causes
We do not know exactly what causes exomphalos. It is not caused by something you have or have not done. It is often linked to other medical conditions, like those affecting your baby’s chromosomes (genetic information) or heart. You will be able to discuss your individual circumstances with the specialist team.
Exomphalos happens in about 4 babies out of every 10,000 (0.04%).
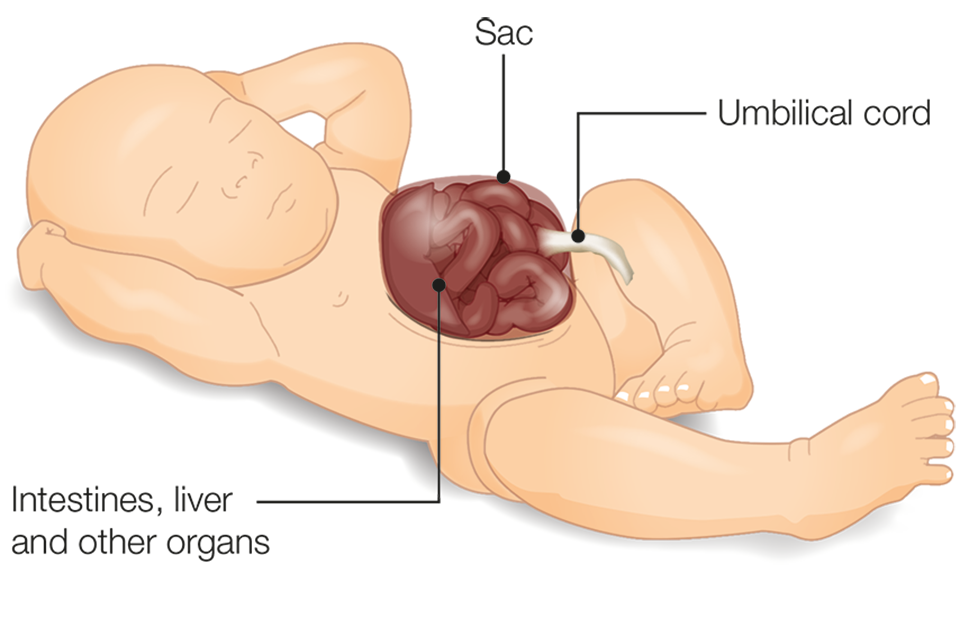
Baby with exomphalos showing intestines, liver and other organs developed outside the abdomen
3. How we find exomphalos
We screen for exomphalos at the 20-week scan (between 18+0 and 20+6 weeks of pregnancy). Sometimes we notice it during an earlier scan, usually at around 12 weeks of pregnancy.
4. Follow-up tests and appointments
As the result of the scan suggests your baby has exomphalos, we are referring you to a team of experts in caring for pregnant mothers and their babies before they are born. They may be based at the hospital where you are currently receiving antenatal care, or in a different hospital. You will need a second scan to find out for sure if your baby has the condition. The specialist team will be able to confirm if your baby has exomphalos and what this might mean.
It may be useful to write down any questions you want to ask before you see the team.
The specialist team may offer you extra tests, such as chorionic villus sampling (CVS) or amniocentesis.
If your baby has exomphalos, they will offer you extra ultrasound scans to monitor your baby. They may also offer you more detailed monitoring of your baby’s well-being before they are born. Mothers of babies with exomphalos usually have a normal birth, but the specialist team may discuss a caesarean section with you if the exomphalos is very large.
5. Treatment
The team looking after you and your baby will involve specialists such as neonatologists and paediatric surgeons, who will care for your baby.
Babies with an exomphalos may need an operation after they are born. This depends on the size of the exomphalos.
If the gap in the abdominal wall is small (sometimes called ‘exomphalos minor’) it usually contains only some of the intestine and can be repaired easily by a single operation. The intestine is put inside the tummy and the gap in the skin is closed.
If the gap is very large (sometimes called ‘exomphalos major’), the cord may also contain some or all of the liver. This is sometimes called ‘the sac’. About 75 out of 100 babies (75%) have this repaired in an operation almost straight after they are born. If the sac is large and the contents will not fit back in the baby’s tummy, the surgeons will talk to you about different ways of treating this. Options include an early operation to place it in a plastic covering (called a ‘silo’) or treating it with special dressings and allowing the skin to slowly grow over the sac. Babies treated in this way will need an operation later to close the gap in their tummy muscles.
Some babies with exomphalos cannot feed in the same way babies usually feed after birth, and will need to be fed using a special tube to begin with. For mothers who wish to breast-feed, you can store expressed milk to give to your baby when they are ready to feed.
The length of time your baby needs to spend in hospital depends on the baby, and varies from days to months. It depends on things like the kind of operation the baby needs, the recovery time, if there are any complications or associated conditions, how the baby is feeding and whether they need any extra help with their breathing. The specialist team will be able to give you more information depending on your individual circumstances.
6. Longer term health
Exomphalos is a wide and varied condition. It can be straightforward to treat, or complicated (and more serious) if there are other health issues as well. The possible outlook for you and your baby will depend on your individual circumstances. The specialist team will support you whatever the situation.
For babies that only have exomphalos, more than 9 in 10 (over 95%) make a full recovery.
Most babies make a good recovery but the chances of a full recovery are lower if:
- the exomphalos is very large
- your baby has other physical or genetic conditions
- your baby is born significantly before their due date
Ongoing problems related to exomphalos can include feeding problems and breathing problems, most of which will improve as the child gets older.
The specialist team looking after your baby will do their best to:
- answer your questions
- help you plan the next steps
7. Next steps and choices
You can talk to the team caring for you during your pregnancy about your baby’s exomphalos and your options. These will include continuing with your pregnancy or ending your pregnancy. You might want to learn more about exomphalos. It can be helpful to speak to a support organisation with experience of helping parents in this situation.
If you decide to continue your pregnancy, the specialist team will help you:
- plan your care and the birth of your baby
- prepare to take your baby home
If you decide to end your pregnancy, you will be given information about what this involves and how you will be supported. You should be offered a choice of where and how to end your pregnancy and be given support that is individual to you and your family.
Only you know what the best decision for you and your family is. Whatever decision you make, your healthcare team will support you.
8. Future pregnancies
If you decide to have another baby, they are unlikely to have exomphalos.
9. More information
Antenatal Results and Choices (ARC) is a national charity that supports people making decisions about screening and diagnosis and whether or not to continue a pregnancy.
Gastroschisis Exomphalos Extrophies Parental Support Group (GEEPS) is a support group run by parents for parents. It is based in the UK, but welcomes parents from anywhere in the world.
Find out how Public Health England and the NHS use and protect your screening information.
Find out how to opt out of screening.
Public Health England (PHE) created this leaflet on behalf of the NHS.
