Heat-Health Alert action card for the voluntary and community sector
Updated 21 March 2024
Applies to England
Who this action card is for
This Heat-Health Alert (HHA) action card summarises the suggested actions that the voluntary and community sector should consider to prepare for and respond to each HHA alert type:
- actions to consider all year round to support summer preparedness
- actions to consider for pre-summer readiness and summer preparedness
- actions to consider for a yellow alert
- actions to consider for an amber alert
- actions to consider for a red alert
The actions are illustrative and organisations including the NHS, local authorities, Local Health Resilience Partnerships (LHRPs) and Local Resilience Forums (LRFs) should ensure that local plans are developed and in place for the coming summer as part of wider preparedness and response to extreme heat events.
In a clinical or care setting with a patient or client, staff should exercise professional judgement and respond appropriately to that patient’s needs. Staff should be aware of the effects of severe heat on health and when they notice a client or patient at risk of overheating, for example, from living in a home that is too hot, that they know what immediate actions to take to ensure safety and that there are clear guidelines for them to make other necessary arrangements (for example, addressing housing issues) in the immediate and longer term.
Other resources
Sector specific and more detailed guidance can be found on GOV.UK:
- Hot weather and health: supporting vulnerable people
- Hot weather advice: planning events and mass gatherings
- Beat the heat guidance
- Weather-Health Alerting System: user guide
About HHA action cards
The HHA action cards have been updated to reflect the new impact-based HHA warning systems, which have been developed in tandem with the Adverse Weather and Health Plan (AWHP). The AWHP, HHA action cards and associated documents provide a broad framework for action, and local areas and organisations need to tailor these good practice suggestions to their local needs and ensure that these fit with wider local arrangements. HHAs should trigger a series of actions by different organisations and professionals as well as the public, building upon year-round planning activities to ensure hot weather preparedness.
The action cards emphasise the importance of joint working across agencies including the voluntary and community sector, and highlight one of the aims of the plan, which is to ensure that there is an integrated response to severe weather events across sectors. Local areas will need to consider those actions indicated in the relevant section which will need to be taken jointly across organisations and sectors.
The action cards cover the core elements of heat-health action plans recommended by the World Health Organization (WHO):
- longer-term development and planning
- preparation before the summer
- prevention during the summer
- specific responses to hot weather
- monitoring and evaluation
Using the HHA action cards
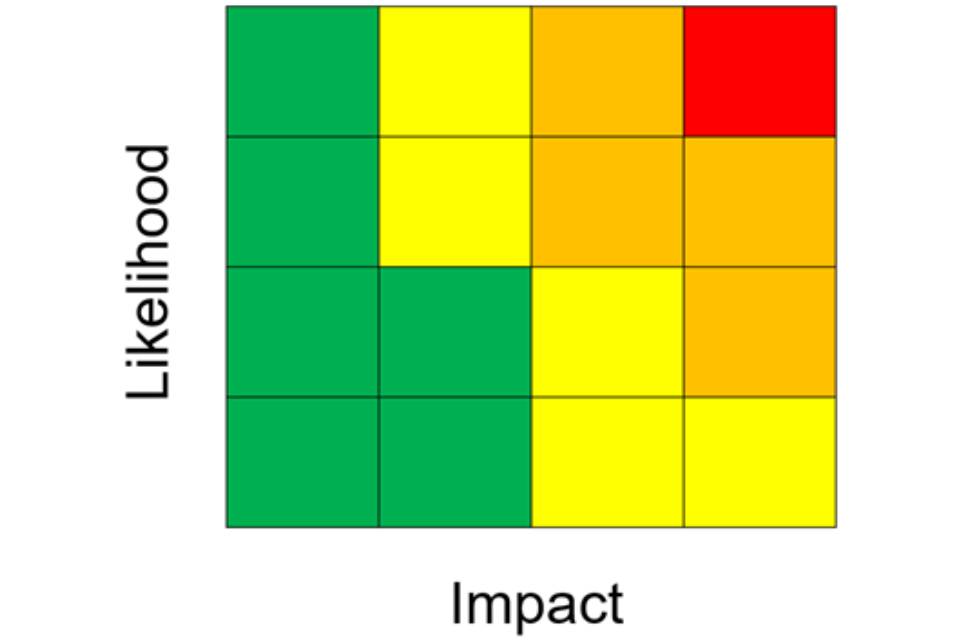
In line with other weather warning systems in operation within England (and the UK) warnings will be issued when the weather conditions have the potential to impact the health and wellbeing of the population. The alerts will be given a colour (yellow, amber or red) based on the combination of the impact the weather conditions could have, and the likelihood of those impacts being realised. These assessments are made in conjunction with the Met Office when adverse weather conditions are indicated within the forecast.
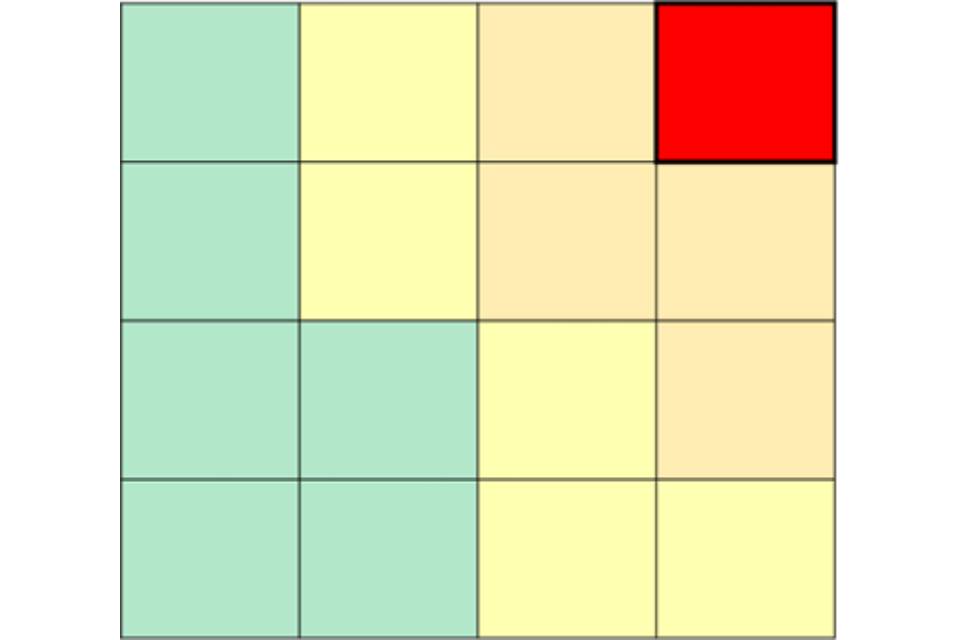
Yellow and amber alert assessments cover a range of potential impacts (for example impacts on specific vulnerable groups (such as rough sleepers) through to wider impacts on the general population) as well as the likelihood (low to high) of those impacts occurring. This additional information should aid making decisions about the appropriate level of response during an alert period. Within the alert that is issued, the combination of impact and likelihood will be displayed within a risk matrix as illustrated below.
Once the decision is made to issue an alert (yellow, amber, or red), these will be cascaded to those registered to receive the alerts and made available on the new dedicated web-platform. Alerts will be issued with as much lead time to the event as is possible to allow users time to make their local assessments and to initiate all appropriate actions to reduce harm to health. Users should review every alert when issued to ensure they fully understand the potential impacts and how likely they are to occur.
Figure 1. Impact and likelihood risk matrix
Green (summer preparedness)
No alert will be issued as the conditions are likely to have minimal impact and health. However, during periods where the risk is minimal it is important that organisations ensure that they have plans in place and are prepared to respond should an alert (yellow, amber, or red) be issued.
Yellow (response)
These alerts cover a range of situations. Yellow alerts may be issued during periods of heat in which would be unlikely to impact most people, but those who are particularly vulnerable (for example . the elderly with multiple health conditions and on multiple medications) are likely to struggle to cope and where action is required within the health and social care sector specifically. A yellow alert may also be issued if the confidence in the weather forecast is low, but there could be more significant impacts if the worst-case scenario is realised. In this situation the alert may be upgraded as the confidence in both the weather forecast and the likelihood of observing those impacts improves.
Amber (enhanced response)
An amber alert would represent a situation in which the expected impacts are likely to be felt across the whole health service, with potential for the whole population to be at risk and where other sectors apart from health may also start to observe impacts, indicating that a coordinated response is required. In addition, in some circumstances a National Severe Weather Warning Service (NSWWS) Extreme Heat warning may be issued in conjunction and aligned with the UK Health Security Agency (UKHSA) HHA. This situation would indicate that significant impacts are expected across multiple sectors.
Red (emergency response)
A red alert would indicate significant risk to life for even the healthy population. A red warning would be issued in conjunction with and aligned to a red NSWWS Extreme Heat Warning. Severe impacts would be expected across all sectors with a coordinated response essential.
Suggested actions to consider all year round to support summer preparedness
Long-term, strategic actions would seek to address the 9 areas of action outlined in the AWHP, as appropriate locally, including:
- service delivery
- capacity building
- organisational arrangements
- communication
- risk management
- early warning systems
- research and data analysis
- quality assurance
- policy development and accountability
Within these 9 areas of action, consideration should be given to:
Identify those at risk
Establish methods to identify, alert and monitor individuals most vulnerable to heat-related illnesses on your caseload.
Business Continuity Plans (BCPs) and/or hot weather plans
Working with partner agencies, providers, and businesses to coordinate BCPs and/or hot weather plans, ensuring vulnerable and marginalised groups are appropriately supported. This may include developing and maintaining a register of the most vulnerable individuals to ensure they can be offered appropriate support where required.
Workplace champions
Consider identifying individuals to be workplace champions to increase staff awareness of the potential risks of adverse weather and climate change and to encourage staff to embed best practice mitigation against, planning for and responding to adverse weather.
Training plans
Develop a training plan to ensure that staff are aware of the local hot weather plans and are engaged in preparing for hot weather.
Data sharing agreements
Ensure appropriate data-sharing agreements or protocols are in place to allow organisations to share data or intelligence, including details of the most vulnerable people where appropriate.
Monitoring
Consider ways to monitor interventions to manage the risk of hot weather to enable evaluation of the effectiveness of any hot weather interventions that are established locally.
Environmental improvements
Identify the local and national support available to make environmental improvements and help individuals you care for to access such support.
Pre-summer readiness and summer preparedness
Figure 2. Impact and likelihood risk matrix: green
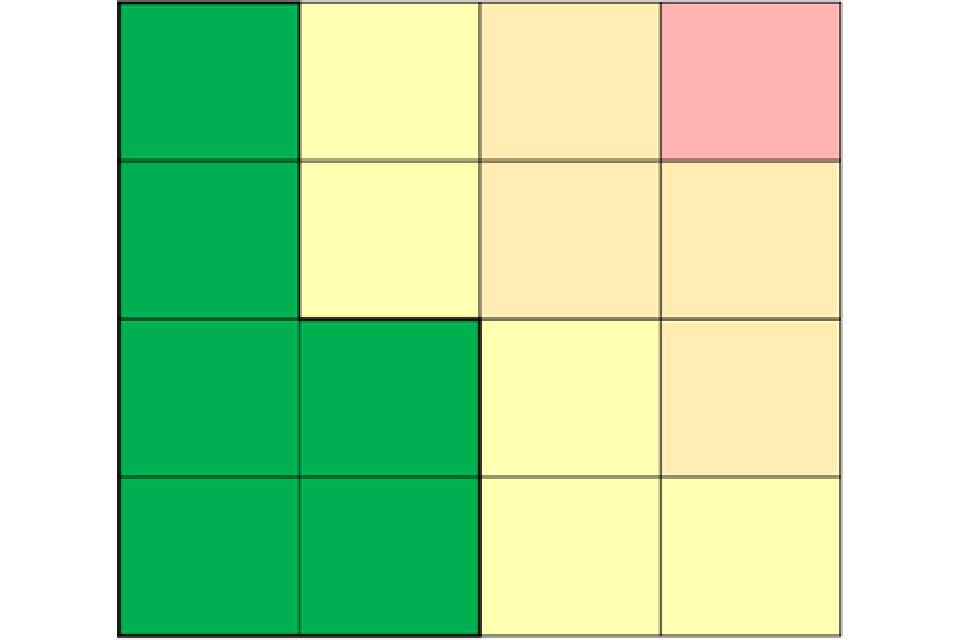
Suggested areas you can support preparedness are:
Alerts
Test out and ensure that local dissemination systems for heat health alerts are fully operational and effective and that staff understand what actions to take. Review and update relevant distribution lists for information and weather alert cascades.
Communication
Ensure staff and stakeholders are aware of hot weather guidance and are engaged in preparing for hot weather. Ensure staff are familiar with this action card, any relevant guidance, and your local plans before 1 June each year.
Audit
Complete an audit of organisational Community Emergency Plans (CEPs) and/or hot weather plans to ensure that these are up to date, including reviewing AWHP and HHA action cards to adapt suggestions for local circumstances.
Training
Ensure relevant staff members are aware of and understand the CEPs and/or hot weather plans, including ensuring relevant staff have received training where applicable.
Risk assessment of events
Providers should assure themselves that organisers of large-scale events for the summer period have taken appropriate risk assessment and mitigation of heat risks.
Additional considerations for staff working directly with vulnerable individuals:
- identify locations for cool rooms/areas (able to be maintained below 26°C) that could be established during hot weather
- consider how to monitor temperatures of places or rooms where vulnerable individuals spend substantial time and ensure relevant staff know how to check and record temperatures and follow internal procedures if a cause for concern is identified
- ensure staff visiting vulnerable individuals have access to a thermometer or means of measuring temperature and ensure relevant staff know how to check, record, and follow internal procedures if a cause for concern is identified
Suggested actions to consider for a yellow alert
Figure 3. Impact and likelihood risk matrix: yellow alert
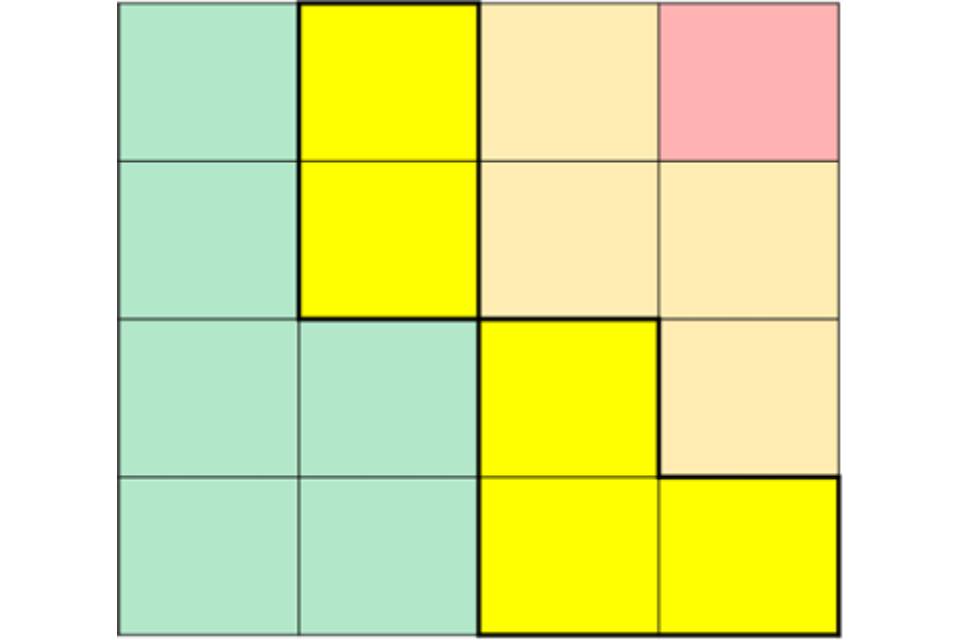
Suggested actions once alert is issued:
- ensure relevant staff members are aware of and understand CEP and/or hot weather plans, including cascading plans to relevant members of staff
- use the HHA impact matrix to inform the local risk assessment for and response to hot weather
- support the provision of information about health risks from reliable sources – especially to vulnerable groups and underserved populations
- work with partners and staff on risk reduction awareness using a variety of methods to maximise dissemination
- develop and communicate proactive evidence-based messages aimed at the public.
- ensure organisers of large events take account of possible heat risks
Additional considerations for staff working directly with vulnerable individuals are to:
- create or operationalise cool rooms or areas (able to be maintained below 26°C)
- ensure staff visiting vulnerable individuals have access to a thermometer or means of measuring temperature and ensure relevant staff know how to check, record, and follow internal procedures if a cause for concern is identified
- monitor temperature in places where vulnerable individuals spend substantial time and ensure relevant staff know how to check, record, and follow internal procedures if a cause for concern is identified
Suggested actions once alert is in effect are:
- use the HHA impact matrix to inform the local risk assessment for and response to hot weather
- check individuals most vulnerable to heat-related illnesses have appropriate arrangements in place
- reaffirm key evidence-based public health messages, especially to vulnerable groups and underserved populations
- ensure sufficient cold water and ice are available to minimise risks from dehydration.
- monitor weather forecast and keep stocked with food and medication, if applicable.
- monitor temperatures regularly during the hottest periods for all areas where patients or clients reside and follow internal procedures if a cause for concern is identified; ensure designated cool areas are below 26°C
Suggested actions to consider for an amber alert
Figure 4. Impact and likelihood risk matrix: amber alert
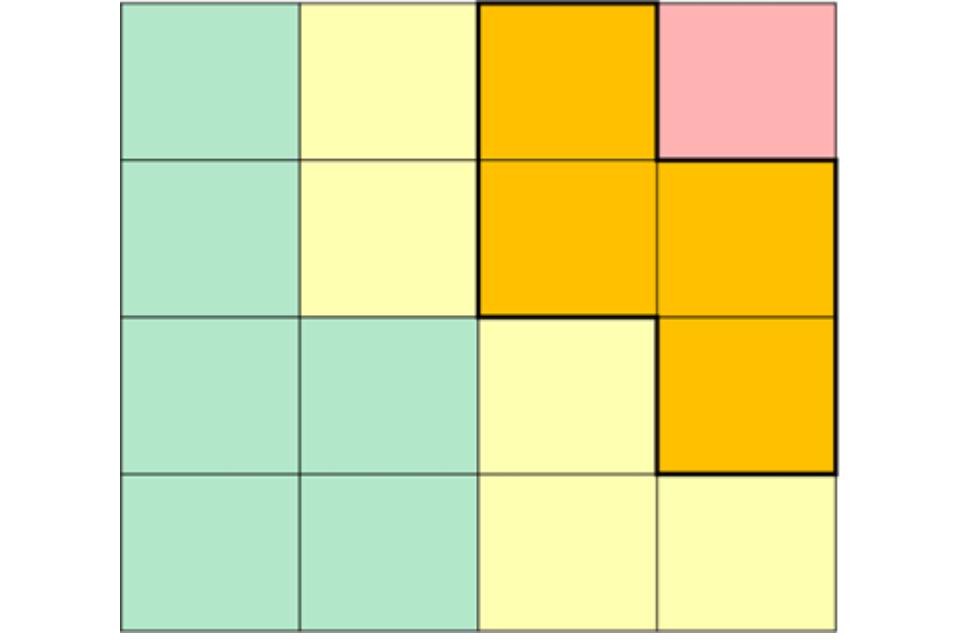
Suggested actions once alert is issued:
- invoke local CEP and/or hot weather plans, including cascading alert to relevant members of staff
- use the HHA impact matrix to inform the local risk assessment for and response to hot weather
- check individuals most vulnerable to heat-related illnesses have appropriate arrangements in place
- increase communication of key evidence-based public health messages, especially to underserved populations and vulnerable groups
- ensure sufficient cold water and ice are available to minimise risks from dehydration
- monitor weather forecast and keep stocked with food and medication
- monitor temperatures regularly during the hottest periods for all areas where patients or clients reside and follow internal procedures if a cause for concern is identified; ensure designated cool areas are below 26°C
- support organisations to reduce unnecessary travel
- review safety of public events
- mobilise community and voluntary support
Suggested actions to consider for a red alert
Figure 5. Impact and likelihood risk matrix: red alert
Central government will declare an emergency in the event of severe or prolonged hot weather affecting sectors other than health and if requiring coordinated multi-agency response.
Suggested actions once alert is issued are to:
- follow all local emergency response plans and feed into local (and, where appropriate, national) coordination and response
- use the HHA impact matrix to inform the local risk assessment for and response to hot weather
- check individuals most vulnerable to heat-related illnesses have appropriate arrangements in place
- increase communication of key evidence-based public health messages, especially to underserved populations and vulnerable groups
- ensure sufficient cold water and ice are available to minimise risks from dehydration
- monitor weather forecast and keep stocked with food and medication
- monitor temperatures regularly during the hottest periods for all areas where patients or clients reside and follow internal procedures if a cause for concern is identified; ensure designated cool areas are below 26°C
- support organisations to reduce unnecessary travel
- review safety of public events
- mobilise community and voluntary support
