Heat-Health Alert action card for health and social care providers
Updated 21 March 2024
Applies to England
Who this action card is for
This Heat-Health Alert action card summarises the suggested actions that providers of health or social care should consider at each Heat-Health Alert level. This card is primarily intended for managers working in:
- hospitals
- social care, care homes and other residential settings
- organisations providing primary or community health services operating from fixed sites such as GP surgeries
- organisations delivering care to people in their homes
This card includes actions to consider:
- all year round to support summer preparedness
- for pre-summer readiness and summer preparedness
- for a yellow alert
- for an amber alert
- for a red alert
Organisations including the NHS in England, local authorities, Local Health Resilience Partnerships (LHRPs) and Local Resilience Forums (LRFs) should use these actions to develop local plans and put them in place before summer as part of wider preparedness and response to extreme heat events.
In a clinical or care setting with a patient or client, staff should exercise professional judgement and respond appropriately to that patient’s needs. Staff should be aware of the effects of severe heat on health and what they can do to protect a patient or client. When they notice a client or patient at risk of overheating, for example, from living in a home or room that is too hot, they should know what to do immediately to ensure safety, and how to make other arrangements (for example addressing housing issues) in the immediate and longer term .
Not all actions recommended in this action card will apply to managers working in all the settings listed above; the following sections separate recommended actions by setting where relevant. Managers should carefully consider if those actions apply to the settings in which they work, for the health and wellbeing of their clients or patients and staff. Managers should read this action card alongside guidance for social care, for healthcare settings, for people who sleep rough and others as appropriate.
About hot weather and health: who is at risk
While anyone can be affected by hot weather, some groups are at higher risk than others. An individual’s risk is affected by a combination of factors relating to their health, behaviours and environment.
High-risk groups include:
- older people aged over 65 years
- babies and young children under the age of 5 years
- people with underlying health conditions, particularly heart problems, breathing problems, dementia, diabetes, kidney disease, Parkinson’s disease or mobility problems
- pregnant women
- people on certain medications
- people with serious mental health problems
- people who are already ill and dehydrated (for example from diarrhoea and vomiting)
- people with alcohol or drug dependence
- people who are physically active and spend a lot of time outside such as runners, cyclists and walkers
- people who work in jobs that require manual labour or extensive time outside
- people experiencing homelessness, including rough sleepers and those who are unable to make adaptations to their living accommodation such as sofa surfers or those living in hostels
- people who live alone and may be unable to care for themselves
Air pollution combined with hot weather can also worsen symptoms for people with existing breathing problems or heart conditions.
About the Heat-Health Alert action cards
The Adverse Weather and Health Plan (AWHP), Action Cards and associated documents provide a broad framework for action, and local areas and organisations need to tailor these good practice suggestions to their local needs and ensure that these fit with wider local arrangements. Heat-Health Alerts should trigger a series of actions by different organisations and professionals as well as the public, building upon year-round planning activities to ensure hot weather preparedness. The action cards emphasise the importance of joint working across agencies including the voluntary and community sector, and highlight one of the aims of the plan, which is to ensure that there is an integrated response to severe weather events across sectors. Local areas will need to consider how recommended actions can be taken jointly across organisations and sectors.
Action cards cover the core elements of heat-health action plans recommended by the World Health Organization (WHO) heat-health action plans guidance:
- Longer-term development and planning
- Preparation before the summer
- Prevention during the summer
- Specific responses to hot weather
- Monitoring and evaluation
Using the Heat-Health Alert action cards
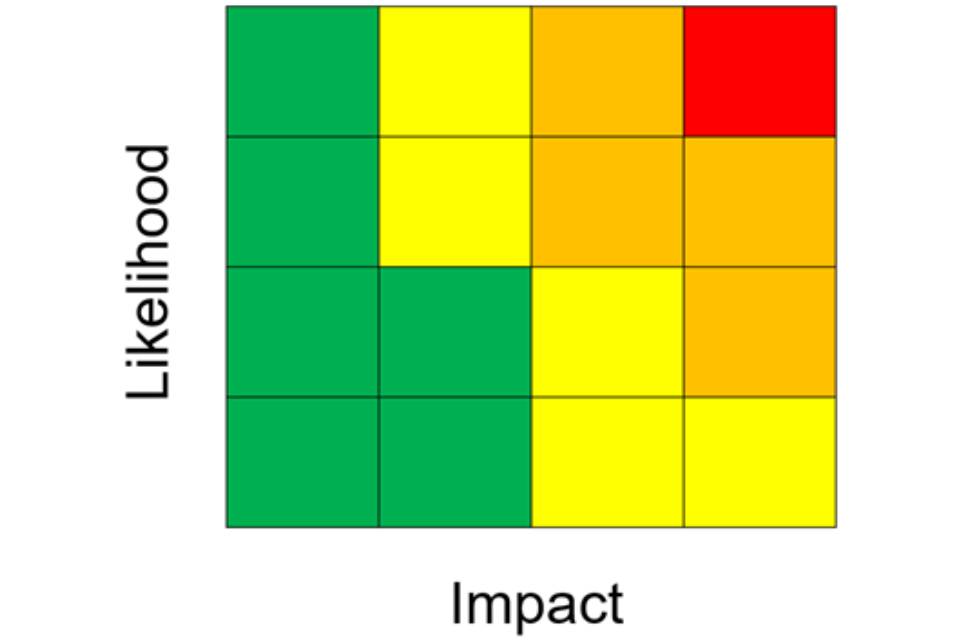
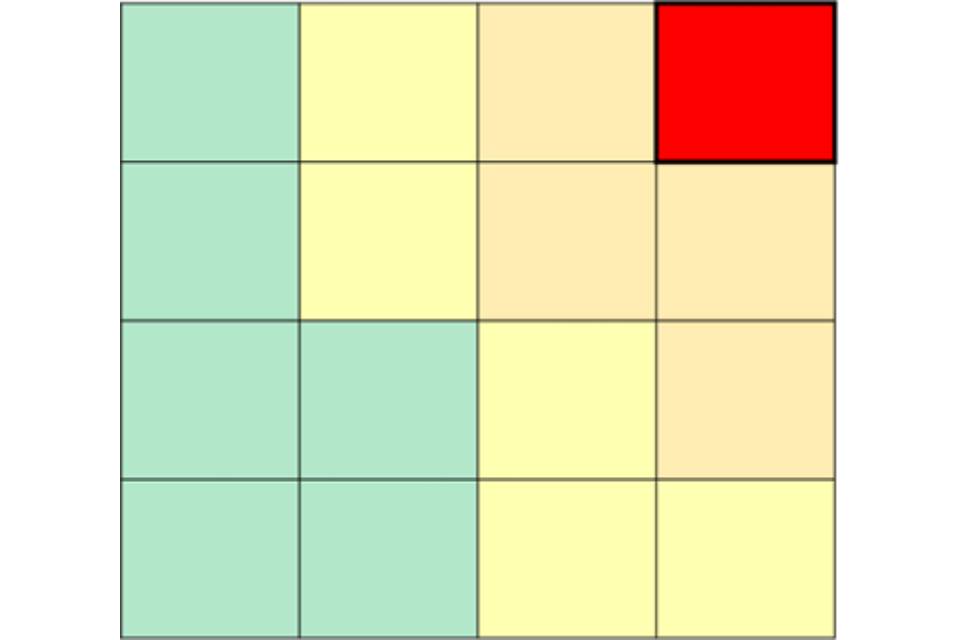
In line with other weather health warning systems in England (and the UK), alerts are issued when the weather conditions have the potential to impact the health and wellbeing of the population. The alerts are given a colour (yellow, amber or red) based on the impact the weather conditions could have on health, and the likelihood of those impacts occurring. These assessments are made with the Met Office when adverse weather conditions are forecast. Within each alert, the combination of impact and likelihood will be displayed within a ‘risk matrix’ grid as illustrated below (Figure 1).
Figure 1. Impact and likelihood risk matrix
Once the decision is made to issue an alert (yellow, amber, or red), these are sent to those registered to receive the alerts and made available on the Weather Health Alerts web platform. Alerts are issued with as much time before the weather event as is possible, to allow users to make local risk assessments and to take action to reduce harm to health. The Heat-Health Alert system operates during the summer season, from 1 June to 30 September. However, alerts may still be issued outside of this period if impacts from heat are expected.
Read the Weather-Health Alerting System guidance for more information and to register.
Green (summer preparedness)
No alert will be issued as the conditions are likely to have minimal impact and health. However, during periods where the risk is minimal it is important that organisations ensure that they have plans in place and are prepared to respond should an alert (yellow, amber, or red) be issued.
Yellow (response)
These alerts cover a range of situations. Yellow alerts may be issued during periods of heat in which would be unlikely to impact most people. However, those who are particularly at risk (see the list above) are likely to struggle to cope and action may be required within the health and social care sector specifically. A yellow alert may also be issued if the confidence in the weather forecast is low, but there could be more significant impacts if the worst-case scenario occurs. In this situation the alert may be upgraded as the confidence in both the weather forecast and the likelihood of observing those impacts improves.
Amber (enhanced response)
An amber alert represents a situation in which impacts are likely to be felt across the whole health service, with potential for the whole population to be at risk and where other sectors apart from health may also start to observe impacts, indicating that a coordinated response is required. In some circumstances an amber National Severe Weather Warning Service (NSWWS) Extreme Heat warning may be issued in conjunction with and aligned to the UKHSA Heat-Health Alert. This would indicate that significant impacts are expected across multiple sectors .
Red (emergency response)
A red alert would indicate significant risk to life for even the healthy population. A red warning would be issued in conjunction with and aligned to a red NSWWS Extreme Heat Warning. Severe impacts would be expected across all sectors, and a national response would be coordinated across government, which may lead to additional guidance being issued.
Actions to consider all year round to prepare for summer
Identify those at risk
Establish methods to identify, alert and monitor individuals most at risk of heat-related illnesses on your caseload (whether for clinical or social reasons, see list above). Consider seeking clinical advice if you are unsure whether someone is at risk.
Business Continuity Plans (BCPs) and hot weather plans
Working with partner agencies, commissioners, providers, and businesses to coordinate BCPs and hot weather plans, ensuring those most affected by heat related illness are appropriately supported . This may include developing and maintaining a register of the most vulnerable individuals to ensure they can be offered appropriate support where required.
Updating care records
Develop approaches to include risk in care records and consider whether changes might be necessary to care plans in the event of hot weather (for example, initiating daily visits by formal or informal care givers for those living alone). Ensure plans are in place to be able to monitor room temperature, and, in clinical settings, body temperature, pulse rate, blood pressure and hydration levels.
Training plans
Develop a training plan to ensure that staff are aware of the local hot weather plans and prepared for hot weather.
Workplace champions
Consider identifying individuals to be workplace champions to increase staff awareness of the potential risks of adverse weather and climate change and to encourage staff to embed best practice mitigation against, planning for and responding to adverse weather.
Data-sharing agreements
Ensure appropriate data-sharing agreements or protocols are in place to allow organisations to share data or intelligence, including details of those most vulnerable to heat-related illness where appropriate. For example, for the care sector, having these in place with local authorities could be particularly important.
Surveillance and monitoring
Consider surveillance and monitoring so you can evaluate the effectiveness of any hot weather interventions that are established locally, including locally relevant indicators and metrics.
Environmental improvements
Consider environmental improvements that need to be made to provide a safe environment during hot weather. For example, checking that windows can be opened safely and shaded, preferably by curtains with pale, reflective lining rather than by metal venetian blinds and curtains with dark linings, which can make conditions worse. Consider outside shading as this can aid cooling.
Identify the local and national support available to make environmental improvements and help individuals you care for to access such support.
Hot weather preparedness (green)
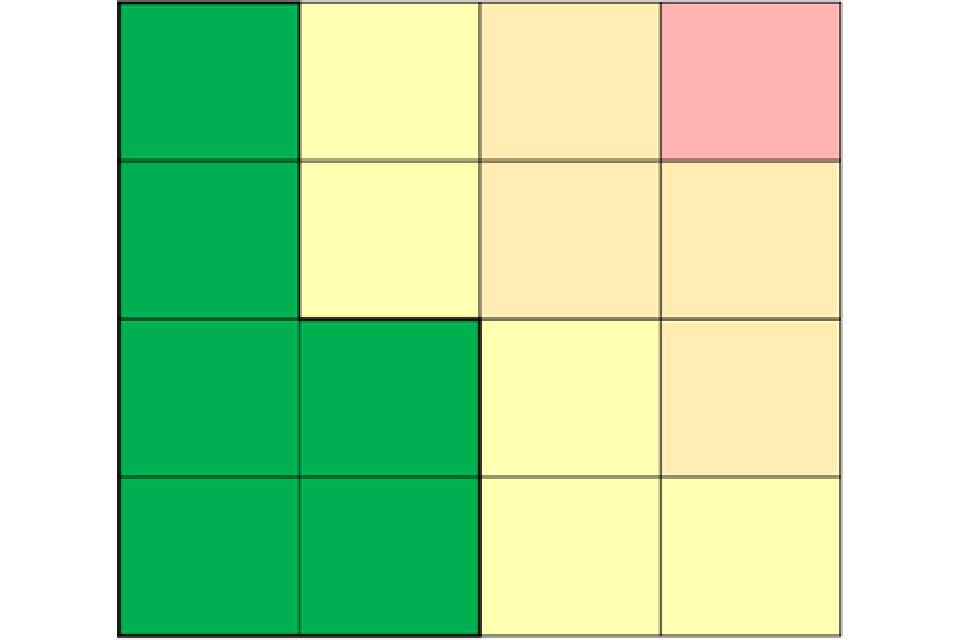
Figure 2. Impact and likelihood risk matrix: green
Suggested activities you can take before summer to prepare for hot weather include:
Alerts
Test out and ensure that local systems for sharing Heat-Health Alerts are fully operational and effective and that staff understand what actions to take. Review and update relevant distribution lists for information and weather alert cascades. Sign up to the Weather-Health Alerting System here.
Audit
Complete an audit of organisational business continuity plans and hot weather plans to ensure that these are up to date, including reviewing the Adverse Weather and Health Plan and relevant guidance to adapt suggestions for local circumstances.
Locations
Identify locations for cool rooms or areas (able to be maintained below 26°C) that could be established during a period of high temperatures. Ensure that staff:
- are trained in how to operate thermostats
- know which rooms are the easiest to keep cool and which are the most difficult
- review the distribution of residents or patients according to those most at risk
Get staff to check the status internal and external shading around buildings, considering measures to increase shading from the Beat the heat: keep cool at home checklist. Preferably, curtains will have pale, reflective lining. Where possible, avoid the use of metal venetian blinds and curtains with dark linings which absorb heat.
Thermometers
Install thermometers where vulnerable individuals spend substantial time (for example, bedrooms, living and eating areas for care settings, or wards and waiting areas in clinical settings). Ensure relevant staff know how to check, and record temperatures, and follow internal procedures if a cause for concern is identified.
Ensure staff visiting vulnerable individuals have access to a thermometer or means of measuring temperature. Ensure relevant staff know how to check, and record temperatures, and follow internal procedures if a cause for concern is identified.
Communication
Ensure staff and stakeholders are aware of hot weather guidance and are engaged in preparing for hot weather. Ensure staff are familiar with this action card, any relevant guidance, and your local plans before 1 June each year. Plan how you will share guidance reminders and any Heat-Health Alerts when they are issued, for example using email, messaging services and in person staff briefings.
Training
Ensure relevant staff members are aware of and understand BCP and/or hot weather plans, including ensuring relevant staff have received training where applicable.
Risk assessment of events
Providers should assure themselves that organisers of large-scale events for the summer period have taken appropriate risk assessment and mitigation of heat risks. Consult specific guidance on this Hot weather and health: events and mass gatherings if required.
Contact information
Ensure appropriate contact details are provided to local authority/NHS emergency planning officers to facilitate transfer of emergency information.
Actions to consider for a yellow alert
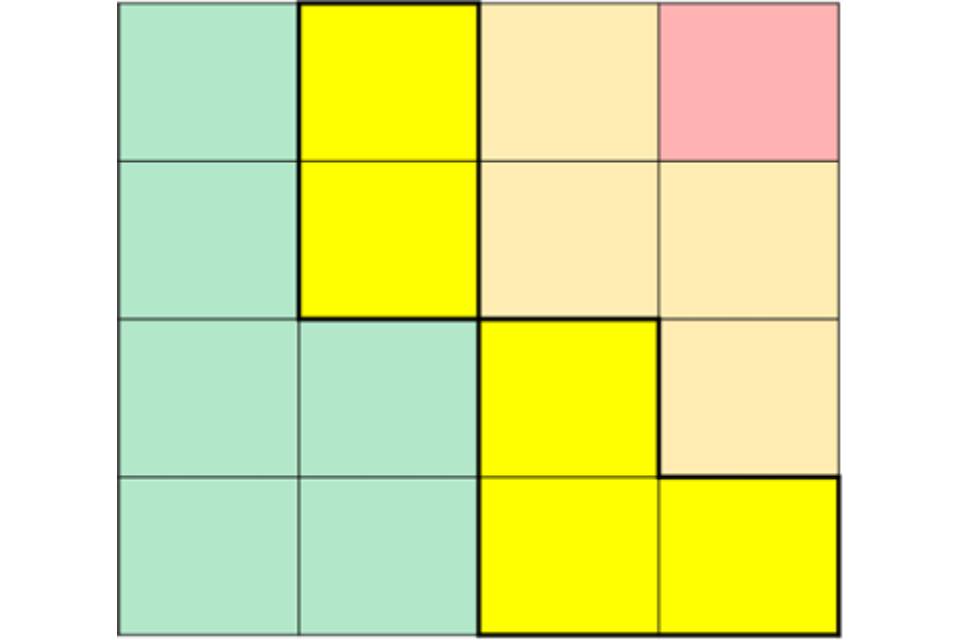
Figure 3. Impact and likelihood risk matrix: yellow alert
Suggested actions once an alert is issued
All settings
Ensure relevant staff members are aware of and understand the business continuity plan and/or hot weather plans, including sharing plans with relevant members of staff.
Conduct a local risk assessment for hot weather, using the Heat-Health Alert impact matrix (Figure 1, above) and the relevant guidance to understand the specific impacts of the hot weather on your service.
Raise awareness about heat illnesses and how to prevent them among staff, patients, clients and carers, for example by sharing Beat the heat messages
Encourage staff and partners to share Beat the heat messages far and wide, especially to high-risk groups and underserved populations.
Ensure organisers of large events take account of possible heat risks.
Fixed sites
Keep certain rooms or areas below 26°C, giving people a place to cool down.
Check thermometers are installed and working where vulnerable individuals spend substantial time and ensure relevant staff know how to check, record, and follow internal procedures if a cause for concern is identified.
Services delivering home care
Ensure staff visiting high-risk individuals have access to a thermometer or means of measuring temperature and ensure relevant staff know how to check, record, and follow internal procedures if a cause for concern is identified. During hot weather, indoor temperatures should be monitored regularly, and steps taken to keep the home cool.
Suggested actions once alert is in effect
All settings
Repeat key public health messages to patients, service users and staff, such as from the Beat the heat guidance.
Assess staffing levels, recognising possible increased care needs of clients and patients during hot weather.
Monitor the local and national weather forecast.
Keep stocked with food and medication.
Review storage of medicines. Most medicines should be kept below 25°C, so they should be stored somewhere cool, dry, out of direct sunlight and away from windowsills. Medicines should only be stored in the in fridge if specified. The NHS Specialist Pharmacy Service has further guidance on storing medications.
Ensure staff promote hydration, encouraging patients and service users to drink and offering cold water regularly.
Encourage and enable staff to carry water and stay hydrated, and report concerns about their own health promptly.
Fixed sites
Ensure staff check and record indoor temperatures regularly during the hottest periods for all areas where patients or clients reside and ensure they follow internal procedures if a cause for concern is identified.
Ensure designated cool areas are below 26°C.
Reduce indoor temperatures through shading or covering windows, turning off unnecessary lights or equipment, and opening windows when the air is cooler outside (for example at night, if it is safe to do so).
Identify and prioritise individuals most vulnerable to heat-related illnesses. For individuals who cannot be moved to cool areas, or for whom a move might be too disorienting, take actions to cool them down (for example, liquids, cool wipes) and enhance surveillance.
In clinical settings with high-risk patients or clients, check body temperature, heart and breathing rates, blood pressure and hydration levels. Consider weighing clients regularly to identify dehydration and rescheduling physiotherapy to cooler hours.
Assess refrigeration capacity to ensure sufficient cold water and ice are available to minimise risks from dehydration.
Ensure staff promote regular cool showers, baths or body washes, and serve cold food (particularly salad, fruit and ice lollies as these contain lots of water).
Services delivering home care
Check individuals most vulnerable to heat-related illnesses have visitor/phone call arrangements in place.
Ask staff to advise clients or patients on how to keep their own homes cool, using the Beat the heat: keep cool at home checklist.
Actions to consider for an amber alert
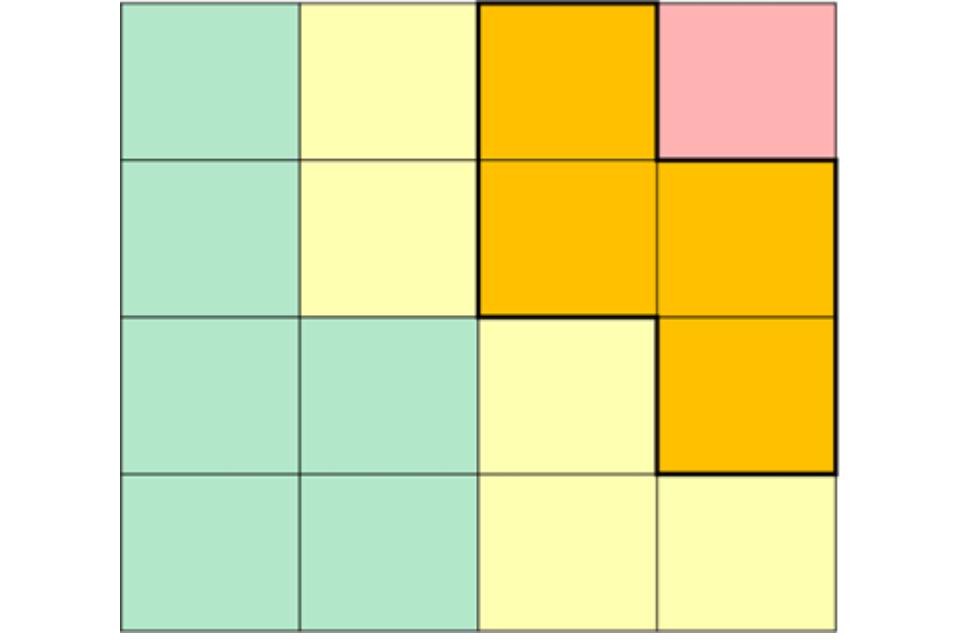
Figure 4. Impact and likelihood risk matrix: amber alert
All settings
Follow local business continuity plans and/or hot weather plans, including cascading alert to relevant members of staff and accounting for a possible surge in demand.
Conduct a local risk assessment for hot weather, using the Heat-Health Alert impact matrix (Figure 1, above) and the relevant guidance to inform the specific impacts of the hot weather on your service, and how likely they are.
Repeat key public health messages to clients and staff, such as from the Beat the heat guidance.
Assess staffing levels, recognising possible increased care needs of patients or clients during hot weather.
Monitor the local and national weather forecast.
Keep stocked with food and medication.
Review storage of medicines. Most medicines should be kept below 25°C, so they should be stored somewhere cool, dry, out of direct sunlight and away from windowsills. Medicines should only be stored in the in fridge if specified. The NHS Specialist Pharmacy Service has further guidance on medicines storage.
Ensure staff promote hydration, encouraging patients and service users to drink and offering cold water regularly.
Advise staff and carers to contact the clinical lead if they have concerns regarding the health of a patient or client.
Encourage and enable staff to carry water and stay hydrated, and report concerns about their own health promptly.
Identify and prioritise individuals most vulnerable to heat-related illnesses. For individuals who cannot be moved to cool areas, or for whom a move might be too disorienting, take actions to cool them down (for example, liquids, cool wipes) and check them more often.
In clinical settings with high-risk patients or clients, check body temperature for signs of heat exhaustion or heat stroke, heart and breathing rates, blood pressure and hydration levels. Consider weighing clients regularly to identify dehydration and rescheduling physiotherapy to cooler hours.
Fixed sites
Check and record indoor temperatures regularly during the hottest periods of the day (usually 11am to 3pm) for all areas where patients or clients reside and follow internal procedures if a cause for concern is identified.
Ensure designated cool areas are below 26°C.
Reduce indoor temperatures through shading or covering windows, turning off unnecessary lights or equipment, and opening windows when the air is cooler outside (for example at night, if it is safe to do so).
Ensure staff promote regular cool showers, baths or body washes, and serve cold food (particularly salad, fruit and ice lollies as these contain lots of water).
Assess refrigeration capacity to ensure sufficient cold water and ice are available to minimise risks from dehydration.
Ensure discharge planning takes home temperatures and potential need for additional support into account, especially for the most at-risk groups.
Services delivering home care
Check individuals most vulnerable to heat-related illnesses have visitor or phone call arrangements in place.
Ask staff to advise clients or patients on how to keep their own homes cool, using the Beat the heat: keep cool at home checklist.
Actions to consider for a red alert
Figure 5. Impact and likelihood risk matrix: red alert
The UK government will declare an emergency in the event of severe or prolonged hot weather which affects sectors other than healthcare, and if it requires a coordinated multiagency response.
All settings
Follow all local emergency response plans and feed into local (and, where appropriate, national) coordination and response.
Conduct a local risk assessment for hot weather, using the Heat-Health Alert impact matrix (Figure 1, above) and the relevant guidance to inform the specific impacts of the hot weather on your service, and how likely they are.
Identify and actively monitor high-risk individuals during hot weather episodes.
Repeat key public health messages to clients and staff, such as from the Beat the heat guidance.
Consider surge staffing and potential difficulties for staff getting to work and increased care needs of clients or patients during hot weather.
Monitor the local and national weather forecast.
Keep stocked with food and medication.
Review storage of medicines. Most medicines should be kept below 25°C, so they should be stored somewhere cool, dry, out of direct sunlight and away from windowsills. Medicines should only be stored in the in fridge if specified. The NHS Specialist Pharmacy Service has further guidance on medication storage.
Ensure staff promote hydration, encouraging patients and service users to drink and offering cold water regularly.
Advise staff and carers to contact the clinical lead if they have concerns regarding the health of a patient or client.
Encourage and enable staff to carry water and stay hydrated, and report concerns about their own health promptly.
Identify, prioritise and monitor individuals most vulnerable to heat-related illnesses. For individuals who cannot be moved to cool areas, or for whom a move might be too disorienting, take actions to cool them down (for example, liquids, cool wipes) and enhance surveillance.
In clinical settings with high-risk patients or clients, check body temperature, heart and breathing rates, blood pressure and hydration levels and escalate according to local clinical advice. Consider weighing clients regularly to identify dehydration and rescheduling physiotherapy. Consider adjusting client bedding and personal clothing.
Fixed sites
Check and record indoor temperatures regularly for all areas where patients or clients reside and follow internal procedures if a cause for concern is identified.
Maintain cool rooms or areas below 26°C. Ensure staff and patients or clients know where these are.
Assess refrigeration capacity to ensure sufficient cold water and ice are available to minimise risks from dehydration.
Reduce indoor temperatures through shading or covering windows, turning off unnecessary lights or equipment, and opening windows when the air is cooler outside (for example at night, if it is safe to do so).
Ensure discharge planning takes home temperatures and support into account.
Ensure staff promote regular cool showers, baths or body washes, and serve cold food (particularly salad, fruit and ice lollies as these contain lots of water).
Services providing home care
Check individuals most vulnerable to heat-related illnesses have visitor/phone call arrangements in place.
Ask staff to advise clients or patients on how to keep their own homes cool, using the Beat the heat: keep cool at home checklist.
Other resources
Sector specific and more detailed guidance can be found on GOV.UK:
