Coronavirus (COVID-19): scaling up our testing programmes
Updated 6 April 2020
Ministerial foreword
One of the most challenging things about coronavirus is the uncertainty, not knowing who has the infection or when it’s safe to return to normal life. Good quality testing can help provide us with certainty. It’s a big part of how we’re going to defeat this disease.
Public Health England (PHE) has already done world-beating work on testing, working with key international partners to design and deliver the first UK COVID-19 diagnostic test, rolling it out faster than any other novel UK test in recent history. We are ahead of most European countries for testing at this point, and we have undertaken one of the highest number of tests in Europe, after Italy, Spain and Germany. But our testing efforts face big challenges that we now need to overcome. This strategy sets out how.
Here are the challenges. First, we are starting from a lower base. Unlike some countries, we did not go into this crisis with a major diagnostics manufacturing industry to call on. There is also huge international demand for crucial testing materials like kits, swabs and chemical reagents.
Given that finite capacity, we’ve had to prioritise. I completely understand that NHS staff want to get tested so they can return to the frontline as fast as possible. But early on I took the decision that seriously ill patients had to come first. For them, a test can mean the difference between life and death. My overriding goal is to protect life and I stand by that decision.
We also have to ensure that any new test products are up to the job. Our experts are clear that having no test is better than an unreliable test, and several of the tests we’ve already checked have been too inaccurate to be used in this crisis. I will not send NHS staff back onto the wards with the false comfort of a false negative result.
Our ultimate goal is that anyone who needs a test should have one. We will get there through a phased approach, starting with patients who need the test, expanding to NHS workers and their families as we are now doing, then other critical key workers as we ramp up further, and then expanding to the wider community over time. Our testing strategy has five pillars, which this document sets out in full.
The first pillar is boosting swab testing – testing to find out if you have the virus – by PHE and NHS labs for patients and frontline workers in the NHS. We have already reached our ambition of 10,000 tests per day by the end of March as we committed. We are now committed to reaching 25,000 tests per day by the end of April at the latest.
The second pillar is the creation of brand-new swab testing capacity delivered by commercial partners. Again, this is swab testing to tell if people have the virus. The biggest part of this pillar is the partnership with universities, research institutes and companies such as Amazon and Boots, to build a network of new labs and testing sites across the UK. This new service has just launched and is ramping up rapidly. We are also working with other testing companies to expand Pillar 2 so that over time we have many different commercial companies delivering mass swab testing.
The third pillar is antibody tests, which are designed to detect if people have had the virus and are now immune. These could potentially be done at home with a finger prick and deliver results in as little as twenty minutes. We are currently working with several companies who are offering these tests and are evaluating their effectiveness. Antibody tests offer the hope that people who think they have had the disease will know they are immune and get back to life as normal. But crucially, they have to be proven to work.
The fourth pillar is surveillance. We are conducting some of the biggest surveys in the world to find out what proportion of the population have already had the virus. This is done using a high accuracy antibody test operated by Public Health England at their Porton Down science campus. We will use these tests to help strengthen our scientific understanding and inform us all on the big choices we have to make about social distancing measures and how we exit from this crisis.
The fifth pillar is the most ambitious. We want to build in a short space of time, the large diagnostics industry that this country currently lacks. Just as our top end manufacturers have joined the national effort to build ventilators, so our life sciences companies will do the same for testing. UK pharmaceutical giants which do not have a tradition of diagnostics, are now working with our world leading but smaller diagnostics companies, to build a British diagnostics industry at scale. This new national effort for testing will ensure we can get tests for everyone who needs them.
Taken together, I’m setting the challenge across all five pillars, of 100,000 tests per day, by the end of April. To drive this forward, I’m delighted that Professor John Newton will be taking on a new role to co-ordinate this national effort for testing.
These 5 pillars represent a comprehensive strategy to put in place the testing that is mission critical as we fight this battle against COVID-19.
There will be problems, like those that we have already overcome. There will be bumps in the road and criticisms made – some justified. But we have some of the best minds and science in the world at our disposal and, having recovered from the illness myself, I am more determined than ever to take the fight to this disease.
Matt Hancock
Secretary of State for Health and Social Care
Testing matters
Testing is a key pillar of our strategy to protect the NHS and save lives. We are focused on 2 types of tests:
- ‘swab tests’ for people with symptoms to see if they have coronavirus, and
- ‘antibody tests’, which test for the presence of antibodies that will demonstrate whether you have had the disease
The government is committed to mass testing. Our overall ambition is to provide enough swab tests for everyone that needs one. In the ‘contain’ stage, our focus was on testing to support contact tracing and investigating outbreaks. At present, whilst we seek to ‘delay’ the spread of the virus through social distancing, this means:
- continuing to provide tests for patients who need them
- providing tests for NHS, social care and then wider critical key workers and their families who are in self or household isolation, to support them to return to work as soon as possible, if they are well enough to do so
We are working with partners to expand swab testing to critical NHS and social care staff and their families (details under Pillar 2), so they can stay in work if they test negative and keep themselves and others safe if they test positive. Once widespread testing is available, we will test critical key workers regularly, to keep them safe and ensure they do not spread the virus. Over time, we hope to make testing available not just to NHS staff, and other critical key workers, but ultimately to the whole population, as needed. Should antibody tests prove to be effective, our strategy will then evolve to also help identify those who have had the disease.
This is an evolving document that will develop as we learn more about the virus, and as we progress the work under the 5 pillars, set out below.
The government is setting the challenge to itself and to the whole system – industry, academia, the NHS – to immediately scale up our testing levels to 100,000 tests a day from all 5 pillars of the strategy, across the UK by the end of this month.
This is a huge ambition. Currently, we are delivering around 10,000 swab tests per day. And we will continue to scale up our ambition beyond this to 250,000 tests a day from all 5 pillars.
We will work collaboratively with each nation, allocating targets and tests to meet their specific needs.
Challenges
Accuracy and reliability of tests
As with everything we are doing to tackle coronavirus, we need to be led by the science. An unreliable test is worse than no test.
We need to make sure that all the tests we use are validated, reliable and provide an accurate result. We also need to understand the quality of new tests such as the antibody test before we start using them in order to avoid putting people at risk by suggesting they are no longer susceptible to coronavirus.
We are working with a number of companies to evaluate tests and this validation is ongoing – but the science is new and uncertain. This shows the importance of having a rigorous process in place and checking every step for accuracy and reliability.
Getting the right supply of people, lab space, equipment and chemicals
Specialist labs are needed to analyse each sample with the right diagnostic machines and skilled professionals. We are fortunate to have a significant number of these highly specialised machines (extraction and PCR) across the country (over 500 in NHS labs alone, nearly 100 more in Public Health England labs, and more available through universities and research institutes).
The challenge is the global shortage of materials needed to run the end-to-end testing process at full capacity, particularly the reagents that help to ensure high levels of sensitivity and specificity for these tests, the swabs with which they have been validated, and the challenge of matching specific materials to the different machines available.
Most of these high-tech testing platforms are ‘closed’, which means that these materials can only be supplied by the same manufacturer as the machine. We are therefore dependent on global manufacturers to very rapidly increase the quantity of their specific reagents and kits. We are working in partnership with them to increase supply of these proprietary reagents, maximising the UK’s global allocation, and creating a sustainable supply of these components, including setting up local manufacturing bases here in the UK. Where possible, we are ‘opening up’ the closed platforms to make use of alternate suppliers of suitable reagents.
Where we have open platforms, we are rapidly expanding local supplies of components and identifying innovative alternatives. Making use of our world-class research institutes here in the UK, we have been developing alternatives to traditional methods, trying to overcome rate-limiting steps like RNA-extractions. We are also rapidly investigating how to bring on board the capacity and skills available to us in universities, research institutes and private labs, particularly where their platforms are open, working through the consequent implications for patient data using emerging models of success (such as the Crick Institute).
Labs across the country are prepared to scale up testing. Some have already deployed specialist staff on shifts covering 7 days a week, 24 hours a day, working in partnership with local universities and across departments; others are ready and waiting to do so as soon as their supply of reagents and other materials matches their capacity.
Logistics
With a highly contagious virus it is important to put in place robust plans for safe access to testing facilities, storage and transportation of diagnostic swabs. We want everyone who is tested to find out their results as quickly as possible.
We will continue to harness traditional logistical capabilities, including assistance from the military, alongside new digital solutions, for example to issue kits and communicate results, whilst providing people with clear information about what is happening throughout the process.
The international context Testing rates differ across countries depending on what stage the infection is at, how it is spreading and existing testing capacity.
Other countries are also aiming to conduct 100,000 tests per day – Germany by mid-April, the UK by the end of April and France by the end of June.
We have undertaken one of the highest number of tests in Europe behind Italy, Spain and Germany. But we want to go further. Other countries, such as South Korea and Germany, have higher testing rates than the UK and we can learn from how they have achieved these goals. For example, Germany has been able to take advantage of the existing technology and infrastructure in its large diagnostics industry, with over 100 cutting edge testing labs.
The UK is a world leader in life sciences, and we can harness this capacity to help us scale up rapidly. We have seen many examples of innovative UK companies offering their support to tackle this crisis, both to move into diagnostics and to scale up testing capacity.
Scaling up our testing programmes
The government is working with the best minds in science, industry and logistics across the world to scale up our testing capacity. Our strategy has 5 pillars.
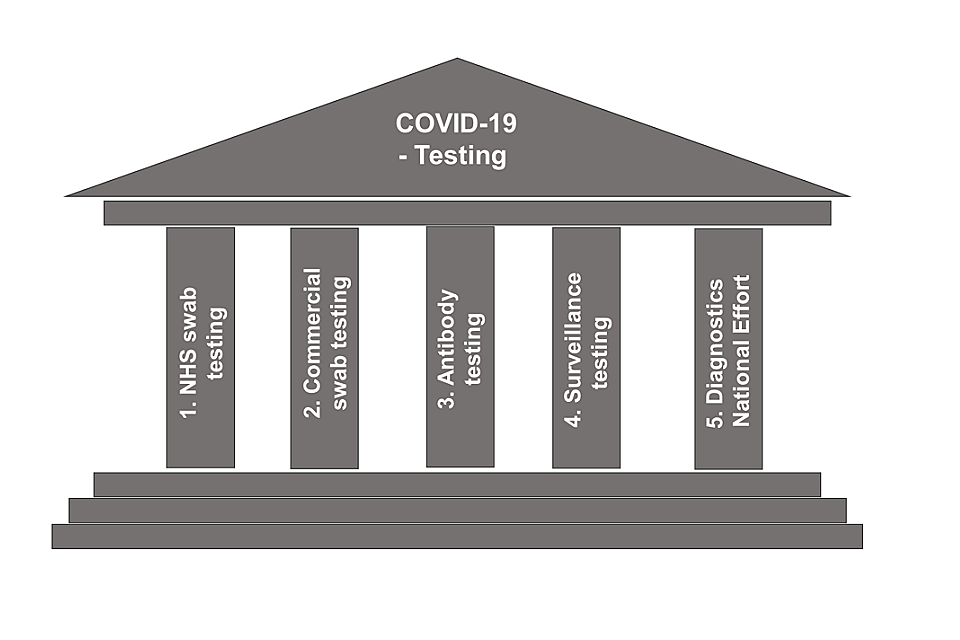
The 5 pillars of testing shown as a building
Pillar 1: Scaling up NHS swab testing for those with a medical need and, where possible, the most critical key workers
This type of testing allows the NHS to identify and effectively care for those who are most seriously ill – saving lives by helping clinicians decide the most effective treatment options. These swab tests are largely delivered through Public Health England’s regional laboratory network and, since the beginning of March, NHS laboratories across the country.
Since the crisis began, we have conducted around 200,000 tests across the UK and over the last fortnight the number of tests done by Public Health England and the NHS has doubled from 5,000 a day to 10,000 a day, by scaling up our lab capacity, boosted by additional trained staff and securing improved access to key supplies, consumables and staff. This puts us ahead of most other European countries at this stage of the outbreak.
But we need to go further, as fast as possible. Public Health England and NHS England / Improvement are committed to increasing their capacity to 25,000 swab tests per day by the end of April, including through a public and private partnership with Roche to bring on line new testing capability that uses their high-throughput real-time PCR machines. The first partnership went live last weekend, based primarily in the NHS, with more sites coming on stream each week during the course of April. We also want to see the UK getting its fair share of proprietary test kits to deliver the full capability that we are making available. The first call on these will be for this pillar.
In line with our strategy, the majority of this testing has been for those with a medical need – for example, identifying coronavirus sufferers amongst the most unwell people in hospital to allow clinicians to separate them from other vulnerable patients and provide the best possible clinical care; or for investigating specific outbreaks.
Within these numbers, some critical NHS key workers in these hospitals have already been tested for COVID-19, where there has been spare capacity based on the decision of local trusts. As capacity increases, it is now possible to also ramp up the volume of critical staff testing. This week, as NHS trusts had created further additional capacity, NHS England instructed that any spare capacity can be focused on testing critical key workers, prioritising those who are in household quarantine because a member of their household is symptomatic, allowing them to return to work as soon as possible if the test is negative.
Further details on swab testing NHS staff, and other critical key workers, is set out in the next pillar, which will add to our capacity in this area of testing.
Pillar 2: Mass swab testing for critical key workers in the NHS, social care and other sectors
As of 4 April, nearly 4,500 NHS workers have been tested in the pilot stage across five new testing sites. Over the coming weeks and months, we want to increase the scale of testing at much greater rates – to reach thousands more health and care staff – and to also cover critical key workers in other sectors. We will confirm the exact list as soon as possible. This will allow us to release more staff, who are well enough to work but currently self or household isolating, back to the frontline, boosting capacity at a time when public services are under pressure.
To help deliver this expansion in testing, last month we began a partnership with universities, research institutes and companies such as Amazon and Boots to create a mass testing infrastructure in the UK through the creation of a network of new labs and testing sites across the UK.
New testing laboratories have been set up in Milton Keynes, Alderley Park and Glasgow using Thermo Fisher Scientific test machines loaned by universities across the country and public sector research establishments, such as The Pirbright Institute. Industry are also actively helping to establish these laboratories and we are working with Boots and other partners to set up over 50 regional test centres around the country by the end of April, starting in some of the main hotspots of the virus, such as London and the Midlands. And we are urgently working on standing-up a home-testing service for critical key workers, supported by Amazon’s logistics network and other commercial partners.
As part of this national effort, we have also partnered with Randox in Northern Ireland, to establish a major laboratory in the Province to strengthen the UK-wide testing capacity for health and care staff and other critical key workers. Randox have also led in the development and production of sample self-collection kits, distributed through Amazon, to enable testing of critical key workers throughout the UK whilst they remain at home. Randox will roll out this service during April.
We are already working in many partnerships to maximise testing capacity and are keen to explore all options including:
-
encouraging innovators that are producing promising new types of tests. Examples include DNANudge that has been used at Imperial and Samba at Addenbrookes, which provide fast turnaround point-of-care testing
-
working with universities and with Universities UK. For example, through the creation of a new online portal, supported by Reed employment. This has been launched and allows university staff with laboratory skills to volunteer to assist with the testing programme. Some specialist labs in universities are already supporting the validation of new consumables and tests and providing lab technicians, equipment and consumables (for example reagents) to the programme. We will be working with Universities UK and others to provide further guidance on how our university sector can help the mass testing effort
-
working with colleagues at the Department for Environment, Food and Rural Affairs (DEFRA), who are already supporting the COVID-19 testing programme and have provided specialist laboratory equipment (PCR and robots) and expert personnel to support Public Health England and government labs. In addition, DEFRA and other scientists, and Department of Health and Social Care colleagues, are committed to working together to agree how best to use the remaining capacity of three major animal testing labs to further support this pillar of the testing effort (the Animal and Plant Health Agency, Fera Science, The Pirbright Institute)
Pillar 3: Mass antibody testing to help determine if people have immunity to coronavirus
Antibody tests could tell people whether they have had the virus and are now immune. Such tests are done by taking a blood sample and looking for the presence of the right COVID-19 antibodies. Once proven in a laboratory setting, this testing could potentially be done at home with a finger prick and deliver rapid results – maybe in as little as 20 minutes.
These antibody tests are brand new. In fact, they are still being developed and there is not yet one that has been proven to work as we would require. No government in the world has yet rolled out a full COVID-19 antibody testing programme.
We are currently engaged with several companies and are urgently testing the quality, accuracy and effectiveness of potential tests with scientific experts and regulators. We have bought some antibody testing kit stock on the basis of minimum initial volumes to enable clinical testing. If the outcome of this is that the antibody tests do not work, no further tests will be purchased and, where possible, orders will be cancelled.
Our experts are clear that an unreliable test is worse than no test. We need to be led by the evidence. Hence, the Chief Medical Officer discourages in the strongest terms organisations from buying their own unvalidated antibody tests.
Should our clinical testing prove successful, we hope to deploy antibody testing kits in their millions. In time, and subject to clinical advice, they could even be used to inform the use of social distancing measures in the future. However, this is some way off. In the meantime, we will keep the public updated on progress.
Pillar 4: Surveillance testing to learn more about the disease and help develop new tests and treatments
Robust population surveillance programmes are essential to understand the rate of infection, and how the virus is spreading across the country. They help us to assess the impact of measures taken so far to contain the virus, to inform current and future actions, and to develop new tests and treatments.
Since the end of February, we have established a national surveillance programme for population blood testing, using a high accuracy antibody test operated by Public Health England at Porton Down, to find out what proportion of the population have had the virus.
Public Health England is testing samples of the population and is in the process of analysing the first 800 samples collected. We are expanding this programme during April so that we have the potential to test around 5,000 samples per week.
We will also roll out a national mass population sample over the coming months. Participants will be invited to take part in a study involving at-home immunity testing every 4 weeks over a 6 to 12-month period. The aim is to enrol 16,000 to 20,000 people who will undergo repeat testing. This will add to the population data, as well as telling us about immunity and how long it lasts.
Pillar 5: Spearheading a Diagnostics National Effort to build a mass-testing capacity at a completely new scale
Britain has an innovative, but relatively small diagnostics industry. We now need to grow it, substantially and quickly. We are calling on all British life science companies to turn their resources to creating and rolling out mass testing at scale. In the short term, this will help meet the supply outlined in the other strands in this strategy, and then help us develop resilient, diagnostic capability in the UK capable of meeting the testing demands over the coming months and years.
We are therefore asking industry to work with us on how this can best be achieved. We want proposals for new national industrial capability that meets a set of clear principles:
- It must be flexible, able to quickly adapt both the tests themselves and the delivery of those tests as the virus and our response evolves over time. We want to explore increasingly decentralised models of testing, moving away from central labs to testing in local hospitals, at work or in the home
- The solutions must enable testing at huge scale, but with extremely high levels of accuracy and sensitivity. An unreliable test is worse than no test
- It needs to be resilient - the end to end supply chain for the test should be domestically based as far as practically possible, with a clear and deliverable plan for the capacity and capability to deliver the scale of testing we need
- It must be as open source as possible with the ability for components, consumables, chemicals and digital components to be produced by a range of manufacturers – quickly and easily. And it should be clear how new companies can join and contribute to the approach
We have already asked industry to tell us if they can manufacture testing equipment or consumables; or if they have new or existing complete tests. We are particularly focused on local manufacturers who can offer reagents and other consumables, and these offers will be prioritised. We will continue to issue calls over the coming days and weeks – these will be asks on specific areas where we need current capability to be ramped up. We will also issue more detail on how we are working with industry to grow our national diagnostic industry.
We are already working with our multinational companies; small, innovative manufacturers; and industry bodies. Over the coming days, we will ramp up this engagement further, working with many others to develop this national effort.
Next steps
This is an evolving strategy to put in place the testing we need to fight this battle against COVID-19:
-
From this week the NHS will be using all their spare capacity to test critical key workers at the frontline of health and care
-
We will complete the pilot of our new commercial swab testing programme and are aiming to offer tens of thousands of swab tests per day by the end of April
-
In early April, we will complete our evaluation of the antibody test kits we are working with and share the results; committing to further develop any promising tests for clinical and then potential home use
-
Over April we will continue our programme to survey the population, to learn more about this virus so we can develop new tests and treatments and, hopefully, vaccines
-
We are going to continue rapidly building a diagnostics industrial strategy that will develop our manufacturing capabilities, to secure the stable supply of the tests, equipment and consumables we need for mass-testing at scale over the immediate and medium term
