Screening in pregnancy: CVS and amniocentesis information for parents
Updated 31 October 2021
Public Health England (PHE) created this information on behalf of the NHS. In this information, the word ‘we’ refers to the NHS service that provides screening.
Chorionic villus sampling (CVS) and amniocentesis are diagnostic tests. Diagnostic tests can tell if your baby definitely has a serious condition by checking their chromosomes for genetic information.
CVS and amniocentesis are both invasive tests. Invasive tests involve taking a sample from within the woman’s body.
1. Who this information is for
You are reading this information because you have been offered a CVS or amniocentesis test. It can help to talk through possible results and outcomes with your doctor or midwife before deciding whether or not to have one of these tests.
The decision is yours.
We offer you a CVS or amniocentesis if:
- there were unexpected findings at the time of your ultrasound scan
- you have a higher chance screening-test result for Down’s syndrome or Edwards’ syndrome and Patau’s syndrome
- you have had a previous pregnancy/baby with a genetic condition
- you or your baby’s father have a family history of another genetic condition, such as sickle cell disease, thalassaemia major or cystic fibrosis
2. It is your decision
This information should support, but not replace, the discussions you have with your healthcare professional. Your healthcare professional will help you make the decision that is right for you and support you in that decision.
They should give you enough time to talk through your options. You can ask for more information and do not have to decide straight away. It is your decision. You can choose to have:
- no further testing
- an invasive test (CVS or amniocentesis)
Your healthcare professional should discuss with you:
- the conditions that CVS or amniocentesis can detect
- the chance of miscarriage from CVS or amniocentesis
- which test (CVS or amniocentesis) would be more appropriate for you
- how we test CVS or amniocentesis samples in the laboratory, the possible results of those tests and their reliability
- the chance that we will need to offer you a repeat diagnostic test
- when and how you get the results of a CVS or amniocentesis test
- your options if you have a test and your baby is found to have a chromosomal or genetic condition
3. If you decide to have the test
If you decide to have a CVS or amniocentesis, most hospitals suggest you bring someone with you, but you should not bring children. Most hospitals say it is safe to eat and drink as normal before and after the procedure. You may need to have a full bladder when you come for the appointment. Your doctor or midwife will let you know before you come. If you are not sure, you can ask them. Your hospital will give specific instructions. Both procedures usually take around 10 minutes to perform. Your appointment may be longer to allow time to discuss the procedure beforehand and to rest afterwards.
4. If you decide not to have the test
If you decide not to have a CVS or amniocentesis, you can still have all other parts of your routine antenatal care. Your midwife will explain what this means for you.
5. Chorionic villus sampling (CVS)
If you have a CVS, we take a tiny sample of tissue from the placenta (placental tissue) for testing. The sample contains some of your baby’s cells which contain genetic information (DNA).
CVS is usually done from weeks 11 to 14 weeks of pregnancy but can be done later. If the doctor decides it is not safe to do the procedure, for example due to the position of the placenta, they may offer you another appointment 7 to 14 days later when the placenta will be larger and easier to reach. Very occasionally, you may be offered another diagnostic test (amniocentesis) after 15 weeks of pregnancy if a CVS cannot be performed.
CVS can be performed:
- through the abdomen (tummy) – transabdominal
- through the cervix (neck of the womb) – transcervical
The transabdominal method is more common because it is often easier to carry out. Transcervical CVS is also more likely to cause vaginal bleeding immediately after the procedure, which occurs in about 10 in every 100 women who have this procedure.
There is no difference in the risk of miscarriage between the 2 methods. Transcervical CVS may be preferred to transabdominal CVS if it is easier to reach your placenta this way.
After taking the needle out, your baby is observed for a short time on ultrasound.
5.1 CVS after a higher chance result for Down’s syndrome, Edwards’ syndrome or Patau’s syndrome
You will get a rapid CVS result in about 3 days.
If the rapid CVS result shows one of the conditions screened for and there are relevant findings on ultrasound scan, your doctor will discuss your options with you.
If the rapid CVS result shows one of the conditions screened for and there are no relevant findings on ultrasound scan, a further test on the original CVS sample may be needed. If this further test is needed, it can take about two weeks to get the results and you will be advised to wait for these if you are considering ending the pregnancy.
This is because of a rare condition called confined placental mosaicism (CPM) in which the DNA in the placenta is not the same as the baby’s DNA. In a very small number of cases, you may be offered another diagnostic test (amniocentesis) to test the DNA of the baby.
6. Transabdominal CVS
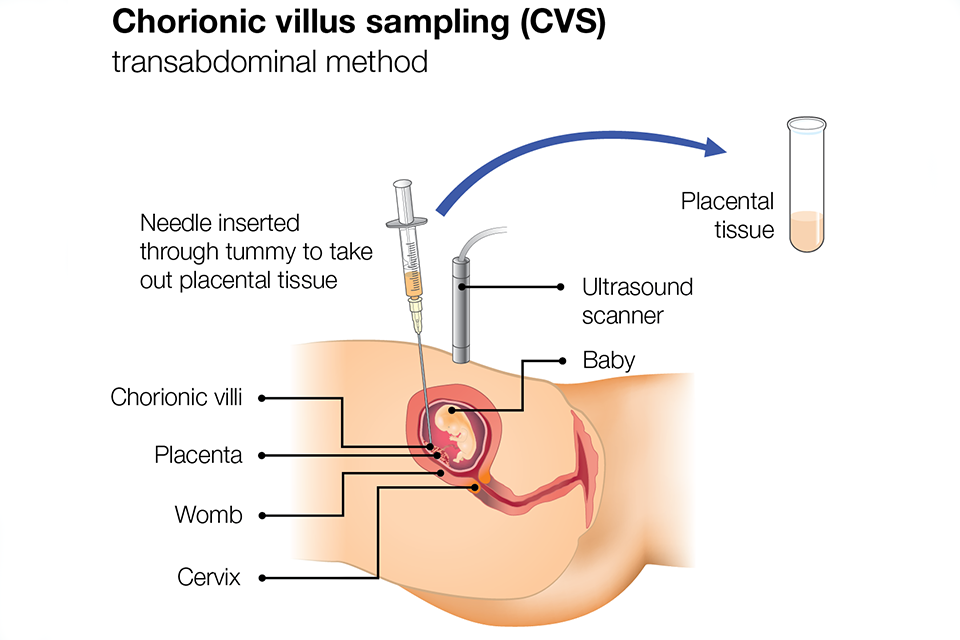
We clean your abdomen (tummy) with antiseptic and may use a local anaesthetic injection to numb a small area. We insert a fine needle through your abdomen and into your uterus (womb) to take the sample. We use an ultrasound probe to guide the direction of the needle.
7. Transcervical CVS
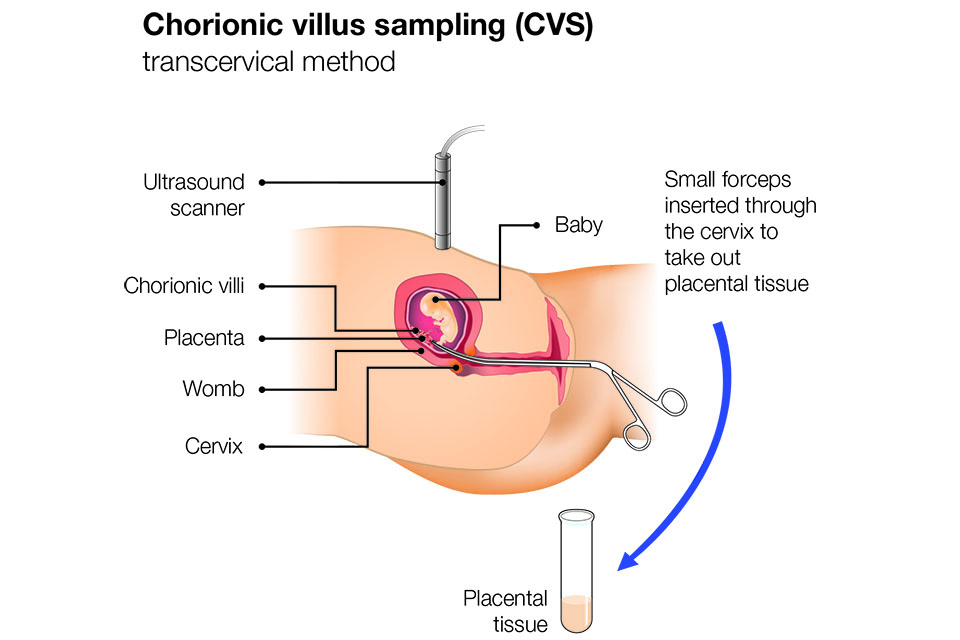
We insert small forceps through your vagina and cervix and guide it towards the placenta using the ultrasound scan. We collect a tiny sample of placental tissue through your cervix.
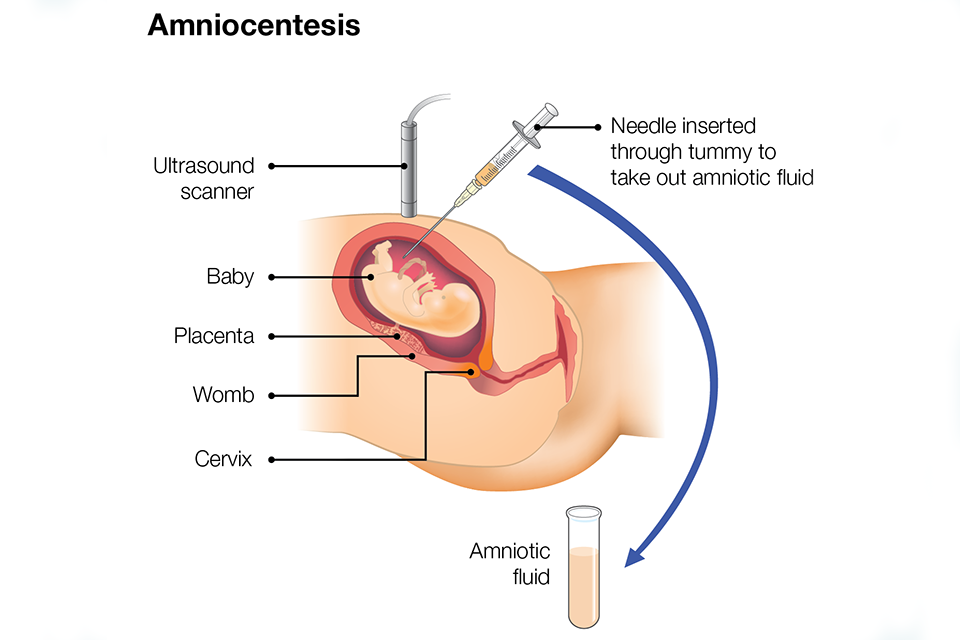
8. Amniocentesis
If you have an amniocentesis, we take a small amount of amniotic fluid (the water around your baby inside your uterus) for testing. The sample contains some of the baby’s cells, which contain genetic information.
Amniocentesis is usually done between 15 and 20 weeks of pregnancy, but it can be done later.
We clean your abdomen with antiseptic and may use a local anaesthetic injection to numb a small area. We insert a fine needle through your abdomen and into your uterus to take the sample. We use an ultrasound probe to guide the direction of the needle.
Occasionally, for fewer than 7 in every 100 women, we cannot take enough fluid at the first attempt and have to re-insert the needle. This is usually due to the position of your baby.
If a second attempt fails, we will offer an appointment to have the amniocentesis again on another day.
After taking the needle out, the baby is observed for a short time on ultrasound.
Amniocentesis results are usually available in around 3 days. They are a true reflection of the baby’s DNA.
9. Possible risks of CVS and amniocentesis
Most women say that CVS or amniocentesis is uncomfortable rather than painful. Some say it feels something like period pain.
You may feel anxious before and after the test. You may notice some cramping for a few hours afterwards. This is normal. You can take paracetamol for any discomfort. You do not need to rest or stop driving after the procedure.
It is not always possible to get a result from the first CVS or amniocentesis. Up to 6 in 100 women (6%) will be offered a second procedure.
About one in 200 women who have a CVS or amniocentesis will miscarry. We do not know why some women miscarry after these procedures. Most miscarriages happen within 3 days of the procedure, but they can happen up to 2 weeks afterwards. There is nothing you can do to prevent a miscarriage after a CVS or amniocentesis.
There is a risk of less than 1 in 1,000 that CVS or amniocentesis will cause a serious infection. You should call your midwife or doctor, or the hospital where you had the test, straight away if you experience any of the following symptoms:
- constant or severe pain
- a high temperature of 38°C (100.4°F) or more
- chills or shivering
- heavy vaginal bleeding
- discharge or clear fluid from the vagina
- contractions
10. Testing women who are pregnant with twins
You can have a CVS or amniocentesis if you are pregnant with twins.
CVS or amniocentesis in twin pregnancies is more complicated and should be performed in a specialist unit. The doctor may need to insert the needle twice to get samples of placenta or fluid from each baby. With CVS there is a small chance of getting 2 samples from the same baby, which could give misleading results.
The risk of miscarriage when having CVS and amniocentesis with twins is about twice as high as in single pregnancies. If this occurs, it may lead to the miscarriage of both babies.
11. Other considerations
If your blood group is Rh (rhesus) negative, it will be recommended that you have an injection of anti-D immunoglobulin after the procedure to prevent you from developing antibodies against your baby’s blood cells.
If you are HIV positive, CVS or amniocentesis might increase the risk of passing HIV on to your baby. You should talk to your obstetrician to decide what is best for you and your baby.
If you have hepatitis B or hepatitis C viruses, CVS or amniocentesis might increase the risk that you pass this on to your baby. The specialist team caring for you will be able to offer further advice.
12. Possible results
The hospital will send the sample of tissue from your placenta (CVS) or amniotic fluid (amniocentesis) to a laboratory for testing.
Depending on the type of laboratory test, you will usually receive 2 results, the first after 3 days and the second after 2 weeks.
You can usually choose whether to receive the results by phone or come into the hospital again and receive the results face-to-face.
In most cases the result will let you know, one way or the other, whether your baby has the condition the test was looking for.
Most CVS or amniocentesis results show babies do not have the condition the test was looking for.
Some women will be told their baby has the condition the test was looking for.
Very occasionally, women have a CVS or amniocentesis test to detect Down’s syndrome, Edwards’ syndrome or Patau’s syndrome and the test detects a different condition.
A CVS or amniocentesis test result which shows a baby does not have the conditions tested for, rules out most conditions, but not all. You can discuss this with your healthcare professional if you need to.
If the result shows your baby has the chromosomal or genetic condition being tested for, your doctor or midwife will talk to you about what this may mean for you and the baby.
If the result shows that your baby has a condition, you should be able to talk to a consultant paediatrician, consultant geneticist or genetic counsellor.
You might choose to:
- continue with your pregnancy
- end the pregnancy (have a termination)
13. Continuing support and care
Deciding whether or not to continue with the pregnancy will be very personal to you. If you decide to continue with your pregnancy, your doctor or midwife will discuss your care and how best to care for your baby during pregnancy and after birth.
If you decide to end your pregnancy, you will be given information about what this involves and how you will be supported. This will include the choices you have about the method of termination.
Whatever decision you make, your healthcare professionals will support you.
14. More information
NHS.UK has information on:
The NHS Screening Programmes use personally identifiable information about you to ensure you are invited for screening at the right time. Public Health England also uses your information to ensure you receive high quality care. Find out more about how your information is used and protected, and your options.
Antenatal Results and Choices (ARC) is a national charity that provides support for people making decisions about screening and diagnosis and whether to continue a pregnancy. You can contact them via their website or call 020 713 7486.
15. Reusing this information
PHE created this leaflet on behalf of the NHS.
You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
