Ending preventable deaths of mothers, babies and children by 2030: approach paper
Published 14 December 2021

Woman from Borana tribe holding her baby, Ethiopia
Ministerial Foreword

By Wendy Morton MP, Minister for Europe and Americas with responsibility for global health, Foreign, Commonwealth & Development Office
The UK Government is committed to working with others to end the preventable deaths of mothers, babies, and children by 2030.
This mission is now more urgent than ever, given the devastating impact of COVID-19 on healthcare services around the world.
All too often, women and babies are missing out on life-saving maternity care, and children are missing vaccinations. The economic consequences of the pandemic have also made health services unaffordable for many. Recent figures from 18 low-income countries suggest this disruption is causing 2.6 maternal and child deaths for every official COVID-19 death.
Action is required and this paper sets out our path.
More than nine out of ten maternal deaths occur in the world’s poorest countries. Every day, 7,000 newborn babies die and another 5,000 are stillborn.
The tragedy is that in most cases, with the right care, these deaths are avoidable.
Preventable deaths of women and children are fundamentally linked to the ability of women and girls to realise their right to exercise control over their own bodies, and access quality health services.
A myriad of poverty-related factors also make death more likely—such as malnutrition, anaemia, dirty water and poor hygiene.
This approach paper presents a broad approach because that is what is needed.
It reasserts the UK’s commitment to women and girls, global health, and to working with partner governments to build healthy and prosperous societies.
We have taken a leading role in these areas for decades.
Through this paper, we commit to harnessing UK innovation and using our experience and influence to improve global health and end preventable deaths.
List of acronyms
| Acronym | Meaning |
|---|---|
| AIDS | Acquired Immunodeficiency Syndrome |
| AMR | Antimicrobial Resistance |
| BEIS | Department for Business, Energy, and Industrial strategy |
| CO | Cabinet Office |
| COP | Conference of the Parties |
| CSO | Civil Society Organisation |
| DAC | Development assistance committee of OECD |
| Defra | Department for Environment, Food and Rural Affairs |
| DHSC | Department of Health and Social Care |
| DIT | Department of International Trade |
| EmONC | Emergency Obstetric and Newborn care |
| EPD | Ending Preventable Deaths of mothers, newborns and children |
| FCAS | Fragile and conflict affected settings |
| FCDO | Foreign Commonwealth and Development Office |
| Gavi | Global Vaccine Alliance |
| GFATM | Global Fund for AIDS, TB and Malaria |
| GFF | Global Financing Facility |
| GHS | Global Health Security |
| HIV | Human Immunodeficiency Virus |
| HMG | Her Majesty’s Government |
| HMIS | Health Management Information System |
| HSS | Health Systems Strengthening |
| IBRD | International Bank for Reconstruction and Development |
| IDA | International Development Association |
| LICs | Low Income Countries |
| LMICs | Low and Middle-Income Countries |
| MNCH | Maternal Newborn and Child health |
| MRC | Medical Research Council |
| NGO | Non-government organisations |
| NHS | National Health Service |
| NIHR | National Institute of Health research |
| ODA | Overseas Development Assistance |
| OECD | Organisation for Economic Cooperation and Development |
| OGDs | Other Government Departments |
| PHC | Primary Health Care |
| PDP | Product Development Partnership |
| RMNCAH | Reproductive Maternal Newborn Child and Adolescent Health |
| SDG | Sustainable Development Goal |
| SEAH | Sexual Exploitation and Abuse and Sexual Harassment |
| SRHR | Sexual and Reproductive Health and Rights |
| UHC | Universal Health Coverage |
| UK | United Kingdom |
| UKRI | UK Research and Innovation |
| UN | United Nations |
| WASH | Water, Sanitation and Hygiene |
| WB | World Bank |
| WHO | World Health Organization |
Executive summary
The UK Government is committed to ending the preventable deaths (EPD) of mothers, newborn babies and children by 2030. This Approach Paper sets out how the UK will deliver on this important ambition to 2024 and our strategic direction to 2030.
The scale of the challenge
Almost 5.5 million pregnant women, newborn babies and children under five die each year.[footnote 1] Most of these deaths occur in the world’s poorest countries and disproportionately impact the most marginalised populations. The COVID-19 pandemic has made existing health challenges worse. Huge inequities in the coverage and quality of health services needed to end preventable deaths remain. With access to quality health services, including midwifery care, a realisation of rights and gender equality, better nutrition, water and sanitation, lives would be saved.
Why ending preventable deaths matters
Every person should have the right to access the essential services needed to save their life. Investing in maternal, newborn and child health is not just the right thing to do, it is the smart thing to do. Good health, nutrition and nurturing care in early childhood can reap lifelong benefits for individuals and communities, including resilience against future health shocks. Strengthening health and rights for women is the key to their empowerment. The health systems and workers that address the needs of women and children are the same that help protect communities from epidemics, pandemics and other health threats.
We know how to save lives
Health outcomes are vastly improved through inclusive and climate-resilient health systems that can provide quality and affordable life-saving services, particularly for the most underserved and marginalised groups. We know that healthier environments and access to clean water, air and nutritious food are vital to reducing the vulnerability of women, babies and children to illness in the first place. The COVID-19 crisis has underlined the need for strong health, food and water systems to meet the challenges of today, as well as the challenges of tomorrow. We know that this means working together with countries to achieve these aims, supporting evidence-based solutions, strengthening systems and coordinating investments.
The UK has a strong track record on global health
Our work on health systems, nutrition, water, sanitation and hygiene (WASH), sexual and reproductive health and rights (SRHR), vaccines and fighting infectious diseases both at home and abroad, spans decades. We remain large investors in health globally and have strong expertise in research, development and innovation, including through our highly regarded UK institutions and charities.

We will leverage on what the UK traditionally does well to step up our efforts
We will bring together our diplomacy, development and soft power for even greater impact. We will use our voice to elevate EPD globally and harness our networks and convening power to strengthen international coordination and coherence. We will work with others to make multilateral investments go as far as they can and engage in all UK footprint countries that work on EPD related programmes to deliver the shifts outlined below.
The UK’s approach to ending preventable deaths is focused on four key pillars of action to achieve greater efficiency, equity and effectiveness in our investments through greater engagement. We will:
-
Support stronger health systems that achieve universal health coverage to end preventable deaths and enhance global health security. We will work with countries to take an integrated, inclusive and long-term approach to strengthening health systems and be a global champion for equity and quality care. We will champion the ‘backbone’ of the systems that are needed to end preventable deaths, including community and primary care, supply chains, midwifery, health financing and vaccines.
-
Support human rights, gender and equality to save and transform the lives of women, babies and children. We will continue to defend and progress sexual and reproductive health and rights but will also take a human-rights approach to all of health. We will use our voice on the world stage to defend and progress this, in all settings. We will listen to, include, and champion the needs of marginalised and inadequately served groups and work with grassroots organisations and movements that are driving change, particularly on neglected and stigmatised issues, such as Female genital mutilation (FGM) and safe abortion.
-
Support healthier lives and safe environments through improving people’s diets, transforming access to resilient water supply and sanitation services, helping to tackle the spiralling threat of air pollution and building resilient, sustainable health systems. We will promote global action on nutrition and sustainable food systems that make nutritious diets more affordable, accessible and climate resilient. We will work with countries to strengthen WASH delivery systems which we know are essential to fighting disease. We will step up our efforts to help countries tackle the increasing environmental risks to health and address the health impacts of climate change.
-
Support technology research and innovation to strengthen evidence and increase access to new health technologies such as medicines, vaccines, diagnostics and innovative service delivery. We will support research to improve the delivery of health and nutrition services at scale, and support innovation in safe technologies such as medicines, vaccines, tests, contraceptives and digital products. We will help to make sure the market is able to provide these products to high quality at affordable prices.
Progress on this approach paper will be monitored using a mix of country-level indicators, tracking overall national progress and indicators specific to UK activities and programmes.
1. Introduction
This Approach Paper lays out the UK’s contribution to ending the preventable deaths of mothers, babies and children by 2030. The paper covers an initial three-year timeframe in detail and outlines our strategic direction to 2030, linking to other key UK strategies including the Integrated Review, Health System Strengthening Position Paper, Africa Strategy, Girls Education Action Plan, Disability Inclusion Strategy and the Gender Vision.
The paper reiterates the unacceptably high numbers of maternal, newborn and child deaths. It spells out how reducing these preventable deaths is inextricably linked to achieving universal health coverage (UHC) and the Sustainable Development Goals (SDGs) 2, 3, 5 and 6. It highlights the huge inequities worldwide around the coverage and quality of health services to tackle this issue and describes how the widespread disruption of essential health services and access to other basic needs caused by the COVID-19 pandemic has made the situation much worse. It sets out how resilient, healthier populations and stronger health systems will be better able to withstand future health shocks and threats.
The paper has a central focus on achieving better maternal, newborn and child health outcomes. It encompasses the wide range of interventions needed to achieve this, across sectors with rights and system strengthening at the centre. It shows the importance of working with women, babies and children—for the health of entire populations, economic prosperity and equity.
The paper outlines four shifts in the UK’s approach to achieve greater efficiency, equity and effectiveness of investments through greater engagement. It describes how we will promote evidence-based interventions delivered as an integrated package, designed to strengthen health systems for the long term and to reach the poorest and most marginalised. In addition, it highlights a shift to system strengthening in nutrition and WASH. It outlines how we will increase the join up and coherence between our multilateral and bilateral investments and across our nutrition, food systems, hygiene, water and sanitation, gender equity, disability inclusion, SRHR, education, humanitarian, research and climate work.
It describes how we will use diplomatic levers and networks as well as our technical development expertise to work at country and global levels, across the UK government, with multilateral agencies and in partnership with others.
The paper outlines how UK efforts will focus on four key pillars of action:
- Strong Health Systems
- Human Rights, Gender and Equality
- Healthier Lives and Safe environments
- Research, Technology and Innovation
2. Global health in 2021
Every 6 seconds, a pregnant woman, newborn baby or child dies somewhere in the world.[footnote 2] The majority of these deaths are preventable and affect the poorest and marginalised the most. This scale of deaths is unacceptable and leaves us severely off track to reach the health-related SDGs 2, 3, 5 and 6, including achieving UHC.
The COVID-19 pandemic has made existing health challenges much worse. COVID-19 has caused millions of deaths directly, but the pandemic has also led to the widespread disruption of essential routine health services. In 2020, 23 million children missed out on basic vaccines[footnote 3], family planning, antenatal and postnatal care was disrupted in a third of countries and 40% of countries saw sharp declines in nutrition services.[footnote 4] The global response to malaria has dropped off and, in many countries hardest hit by the disease, cases are on the rise. During 2020, it is estimated an additional 6.7m children (14.3% increase) will have been moderately or severely acutely malnourished.[footnote 5]
The disruption to essential services have been felt most by low-income countries. Deaths from other illnesses in these countries outweigh deaths from COVID-19. The latest estimates show that, in low-income countries (LICs), for each reported COVID-19 death there has been an additional 2.6 maternal and child deaths since the pandemic began due to disruptions to essential (non-COVID-19) health services. This represents a 3.8% increase in child mortality and a 1.4% increase in maternal mortality.[footnote 6]
The most marginalised people in all countries have been hardest hit. Early evidence shows that the pre-existing inequalities in access to health services felt by women and girls, people with disabilities and other marginalised groups have worsened and the problems of poverty, HIV and humanitarian crises amplified.[footnote 7] The economic impact of lockdowns and other controls have left families unable to pay for health services and food.
Systems have been further weakened. Health facilities, already struggling with a lack of trained staff and an irregular supply of drugs and equipment, struggle even more as they try and respond to the pandemic in a health system that is pushed to the limit. Fragmented health data systems have not been able to provide the real time information needed to respond to the pandemic or make sure that everyday health services remain accessible. Disruptions to food systems have meant that an estimated 130m additional people were suffering from hunger by the end of 2020[footnote 8], and social protection systems remain stretched.
While countries had made progress towards the Sustainable Development Goals by 2019, it was clear that an acceleration of progress was needed.[footnote 9] The COVID-19 pandemic has thrown countries further off course and a decade of progress in reproductive, maternal, newborn and child health could be stalled or reversed.[footnote 10] Currently 88% of people in the world’s poorest countries still do not have access to essential health services. Once in a facility, poor quality of care is responsible for over 5 million deaths a year.[footnote 11] Even before the pandemic, closing the gap in safe water, hygiene and sanitation services for all would have required a fourfold acceleration in progress.[footnote 12]
Demographic transitions are slower in Africa, increasing the pressure on basic services and making it harder to reap the benefits of a demographic dividend.[footnote 13] In sub-Saharan Africa, unlike other regions, declines in child mortality have not been followed by falling fertility rates. Sixty percent of Africans are under 25 years old, and the population is set to double from 1.3 billion to 2.5 billion in the next 30 years.[footnote 14] A package of actions, including nurturing care of young children, expanding girls’ education and improving access to voluntary family planning as part of access to wider sexual and reproductive health and rights can accelerate progress to a demographic dividend. The use of demographic data and analysis can help prioritise where resources are targeted to reach the ‘bottom billion’.[footnote 15]
Other emerging threats to health are gaining prominence. Health, water and food systems are critical to the response to climate change but are also themselves extremely vulnerable to climate change impacts. This is felt most severely in LICs and low-middle income countries (LMICs) and there is growing evidence of a direct impact on maternal and newborn health. More countries are experiencing the double burden of malnutrition, where undernutrition coexists with obesity. The effect of air pollution on respiratory illnesses, especially in children, is spiralling upwards.[footnote 16] Changing rainfall patterns, extreme weather events and warming are affecting the persistence of microbiological hazards, driving toxic contamination of foods and increasing the incidence of foodborne diseases—which already pose as serious a burden for human health as malaria, tuberculosis and HIV/AIDS.[footnote 17] The threat of animal-to-human spread of new diseases is well-documented, and there is also an increased risk of new epidemics of existing diseases. Antimicrobial resistance, where microbes become resistant to treatments used against them, is now classed by WHO as one of the top ten global health threats.
Figure 1: Mortality progress and 2030 SDG mortality targets
Maternal deaths per 100,000 live births
2030 Global SDG target: 70
| Year | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Global mortality rates | 342 | 335 | 328 | 319 | 309 | 296 | 284 | 274 | 265 | 257 | 248 | 241 | 234 | 229 | 224 | 219 | 214 | 211 |
| Average Low and lower middle income economies mortality | 639 | 620 | 604 | 584 | 561 | 534 | 510 | 488 | 471 | 455 | 438 | 423 | 411 | 399 | 389 | 377 | 366 | 357 |
Neonatal deaths per 1,000 live births
2030 Global SDG target: 12
| Year | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Global mortality rates | 30 | 29 | 29 | 28 | 27 | 26 | 25 | 24 | 24 | 23 | 22 | 21 | 21 | 20 | 20 | 19 | 19 | 18 | 18 | 17 |
| Average mortality rates in low and lower middle income countries | 41 | 40 | 39 | 38 | 37 | 36 | 35 | 34 | 33 | 32 | 32 | 31 | 30 | 29 | 28 | 28 | 27 | 26 | 26 | 25 |
Under 5 deaths per 1,000 live births
2030 Global SDG target: 25
| Year | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Global mortality rates | 76 | 73 | 70 | 68 | 65 | 63 | 60 | 58 | 55 | 53 | 51 | 49 | 47 | 46 | 44 | 43 | 41 | 40 | 39 | 38 |
| Low and lower middle income economies | 120 | 116 | 112 | 107 | 103 | 99 | 95 | 91 | 87 | 84 | 81 | 77 | 74 | 72 | 69 | 67 | 64 | 62 | 60 | 58 |
We must accelerate action if we are to get the world back on track and build back better. Unlike most recent crises, every country has been touched by COVID-19 and this affects how we each can respond. However, current constraints present opportunities to improve and to do things differently. We know that global health support is fragmented, often focused on one disease or issue rather than on strengthening whole systems. We know that, too often, we have not worked across sectors to address the underlying drivers of deaths and disease, including those resulting from poor animal and environmental health. We know that the right types of investment can lead to longer term, sustainable changes. We know that countries need to be in the driving seat and that grassroots organisations and the communities they support play an invaluable role in demanding quality services. We know that we can achieve more in partnership with others than alone. Now is the time to sharpen our focus, innovate and accelerate action.
3. Why ending preventable deaths matters
Saving lives is the right thing to do. Maternal, newborn and child deaths shine a light on global inequality. Most causes of death are preventable and the solutions are well established. It is the right of every person to access the essential services needed to save their life.
Maternal and newborn health outcomes act as proxies for the strength of a health system and are important to achieve universal health coverage.[footnote 18] To save a mother and a baby requires almost every part of the health system to be working well. Whilst the common causes of deaths are known, their occurrence is often unpredictable and require fast action. For example, bleeding after delivery of a baby remains the most common cause of maternal death in LICs. To overcome this, a woman has to first feel welcome to go to a facility for childbirth, be able to get there on time and afford the cost of any fees. Once there, managing the bleeding requires a trained health worker to be present, who acts within minutes to give fluids to rehydrate and drugs to stop the bleeding. It requires equipment to resuscitate a stressed newborn and a way of transferring the mother, if needed, for surgery or a blood transfusion. Each part of the system needs to be functioning and handling this situation without clean water and good hygiene is unthinkable.
The health systems that address the needs of women and children are the same as those needed for global health security. Each building block of the system (health workers, drugs and supplies, data, finance, leadership and quality service delivery) that is needed to end preventable deaths will also improve global health security. In many settings, the health facilities that deal with both (and often the health workers) are the same, especially the community and primary health systems. Strong health systems will help us achieve universal health coverage (UHC), where all people and communities receive the quality health and nutrition services they need, have their rights respected, and do not experience financial hardship. Ending preventable deaths is in all our interests.
Benefits will reach the poorest, most vulnerable and women and girls. Preventable deaths disproportionately affect poor and marginalised groups.[footnote 19] Children from the poorest of households are nearly twice as likely to die before their fifth birthday compared to children in the richest households.[footnote 20] More than nine in ten of all maternal deaths occur in the world’s poorest countries.[footnote 21] Large inequities in the coverage of services and health outcomes are often linked to the amount people have to pay for care, with women, children and adolescents worst affected.[footnote 22] Vulnerabilities often compound one another in a cycle of poverty, disability and ill health.
Figure 2: Newborn deaths by country’s income group, in 2019
| World Bank Income Group | Number of neonatal deaths |
|---|---|
| Low Income Economies | 608,502 |
| Lower-Middle Income Economies | 1,516,037 |
| Upper-Middle Income Economies | 279,697 |
| High Income Economies | 36,227 |
Data Source: United Nations Inter-agency Group for Child Mortality Estimation. https://childmortality.org/data, 2020
Figure 3: Number of women dying of childbirth related causes by country’s income group, in 2017
| World Bank Income Group | Number of Maternal Deaths |
|---|---|
| Low Income Economies | 114,988 |
| Lower-Middle Income Economies | 162,184 |
| Upper-Middle Income Economies | 15,800 |
| High Income Economies | 1,666 |
Data Source: WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, “Maternal mortality: Levels and trends 2000 to 2017”. https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/, 2019.
Investing in women’s, children’s and adolescents’ health is affordable and the benefits are high. An additional $4.80 per person annually in LICs and LMICs would meet all women’s needs for essential sexual and reproductive health services.[footnote 23] Every $1 invested in reproductive, maternal, newborn and child health in the countries with the highest burden of preventable deaths can create an economic benefit of $8.70.[footnote 24] Good health, nutrition and nurturing care in early childhood will reap lifelong benefits in terms of attainment at school and ability to work.[footnote 25] Around one quarter of economic growth between 2000 and 2011 in LMICs is estimated to have resulted from the value of improvements to health.[footnote 26]
Tackling preventable deaths also drives wider agents of change. Many of the causes of premature mortality also relate to the societies and environment within which we live. Access to good nutrition, safe food, hygiene, sanitation, clean water and air, and the empowerment of all people to make choices over their bodies and take decisions that will shape their lives, are just some of the wider foundations for a healthy life. Strengthening health, water and food systems to be resilient in the face of climate change will be essential.
The UK is well placed to respond. We have a strong track record spanning decades in health, both within the UK and in supporting countries. We have a tradition of working in partnership with a range of organisations to support countries with their objectives. Our well-respected public health institutions, leading universities, strong equitable health system and health professionals in the NHS makes us a source of world class expertise. The Foreign, Commonwealth and Development Office (FCDO) also has deep country knowledge and experience across health, nutrition, water and sanitation, agriculture and food systems, gender equality and human rights.
4. The scale of the challenge
‘Before COVID-19 the world was making progress towards global health goals—but not fast enough.’[footnote 27]
Pregnancy, childbirth and the early years of life remain a dangerous time in many developing countries. Despite maternal, newborn and child deaths falling since 2000 globally, rates remain high in poorer countries, especially those in humanitarian crises or vulnerable to famine.[footnote 28] A child born in sub-Saharan Africa or in Southern Asia is 10 times more likely to die in the first month than a child born in a high-income country.[footnote 29] A woman’s lifetime risk of maternal death in high income countries is 1 in 5400, compared to 1 in 45 in LICs.[footnote 30] If current trends persist, 48 million children under the age of 5 will die between 2018 and 2030—half of them newborns.[footnote 31] Currently one in eight children in Somalia dies before the age of five years[footnote 32], and one in 87 women in South Sudan dies in circumstances related to childbirth.[footnote 33] These numbers are unacceptably high.
The major causes of preventable death for women relate to pregnancy, including unsafe abortions and complications prior to, during and after childbirth. Women and girls are still dying from bleeding after delivery, infection and obstructed labour. Pregnant women and their babies are also at greater risk of dying from diseases such as malaria. Malnutrition increases their risks and nearly half of pregnant women go into labour with anaemia.[footnote 34] Deaths are highest in the most marginalised, including adolescents, women with HIV and women with disabilities, who are also more likely to have pre-term births and low birthweight babies.[footnote 35]
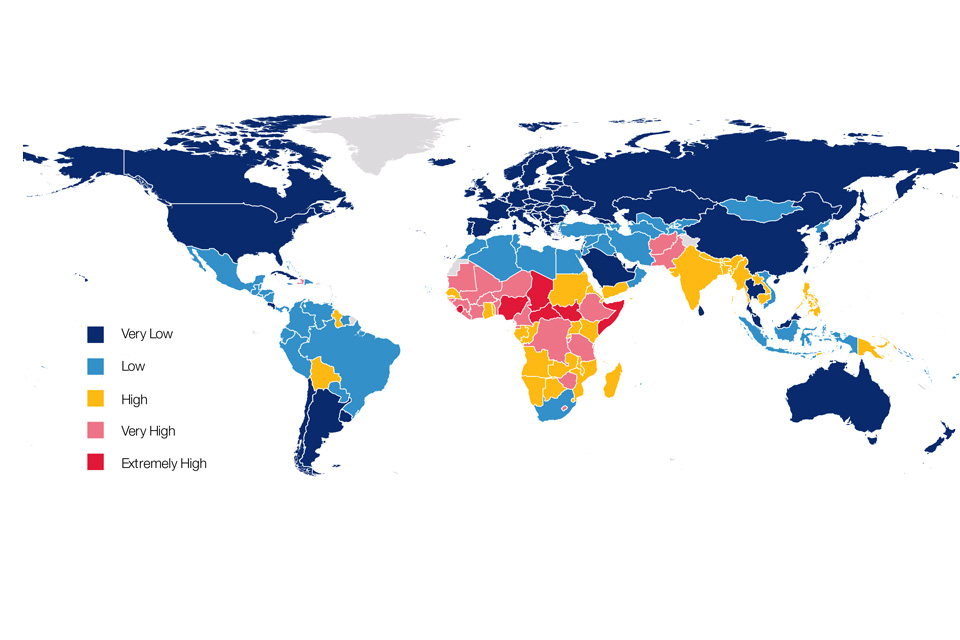
Figure 4: Levels of maternal, newborn and children under 5 mortality across the world 2017-2019
The major causes of child deaths are infectious diseases, including pneumonia, diarrhoea and malaria, premature birth and labour-related complications. Children need a healthy start in life, including a safe newborn period, breastfeeding, vaccinations, tools like bednets to prevent malaria and treatment for childhood infections. More than 1 in 4 child deaths are attributable to unhealthy environments, including 570,000 deaths from respiratory infections, attributable to indoor and outdoor air pollution; 361,000 deaths due to diarrhoea as a result of poor access to clean water, sanitation, and hygiene; and the 200,000 deaths from malaria that could be prevented through environmental actions.[footnote 36] Undernutrition contributes to almost half of all child deaths through weakening of the immune system.[footnote 37] Children with disabilities are more likely to be malnourished and die from malnutrition.
Figure 5: Causes of childbirth-related death in women
| Causes of childbirth related deaths in women | Percentage |
|---|---|
| Indirect* | 27.5% |
| Haemorrhage | 27.1% |
| Hypertension | 14.0% |
| Sepsis | 10.7% |
| Unsafe Abortion | 7.9% |
| Embolism | 3.2% |
| Other direct | 9.6% |
*Indirect causes include death resulting from previous existing disease or disease that developed during pregnancy and not due to direct obstetric causes but were aggravated by the physiologic effects of pregnancy.
Data Source: Say L et al., ‘Global causes of maternal death: a WHO systematic analysis’ Lancet Global Health. http://dx.doi.org/10.1016/S2214-109X(14)70227-X, May 6, 2014.
Figure 6: Causes of death in newborns
| Causes of newborn deaths | Percentage |
|---|---|
| Preterm birth complications | 35% |
| Intrapartum-related complications | 24% |
| Sepsis | 15% |
| Congenital abnormalities | 11% |
| Pneumonia | 6% |
| Tetanus | 1 % |
| Diarrhoea | 1% |
| Other | 7% |
An estimated 218 million women of reproductive age want to avoid or delay pregnancy but are not using modern contraception.[footnote 38] Sexual and reproductive health and rights, including family planning, are fundamental to ending preventable deaths. This is through fewer maternal deaths but also by enabling women to complete their education, take up better opportunities and contribute to the growth and prosperity of their families and countries. Not being able to choose the number and spacing of children is both a cause and consequence of low women’s empowerment. Adolescent girls face particular social barriers to negotiating their own sexual and reproductive health and rights and their levels of ‘unmet need’ for contraception are much higher than the average for all women (43% vs 24%).[footnote 39] Women continue to face legal and social restrictions on safe abortion and even on post-abortion care.
Health systems struggle to tackle the scale of the challenge. The world is currently facing a shortage of 1.1 million health workers for reproductive, maternal, newborn and child health. This includes 900,000 midwives, a third of the required global midwifery workforce.[footnote 40] Supply chain systems are not strong enough to ensure essential drugs and equipment are reaching those in need. For example, 10.6 million children per year do not receive even a single dose of basic routine vaccinations.[footnote 41] Two of every three cases of diarrhoea are caused by unsafe water and sanitation[footnote 42] yet 22% of health facilities in LICs do not have any water and sanitation facilities.[footnote 43]
The quality of care is as important as the quantity.[footnote 44] Approximately 5 million deaths each year in LICs and LMICs are due to poor quality care within health facilities.[footnote 45] High-quality health systems could prevent 1 million newborn and half of all maternal deaths each year.[footnote 46]
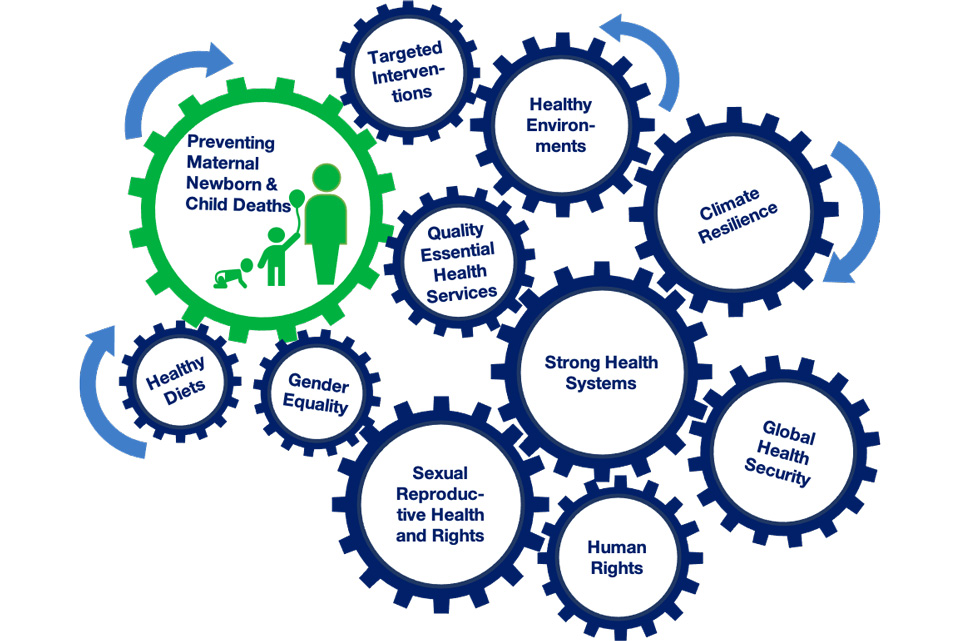
Figure 7: The interconnectedness of health interventions, systems and environments needed for healthy mothers, babies and children under 5.
Food systems need to be transformed to address the burden of malnutrition in all its forms and ill health. Poor quality diets affect 1 in 3 people worldwide and are a key driver of global disease. They also constrain growth and reduce resilience to climate change and pandemics. Unsafe food causes around 600 million illnesses and 420,000 premature deaths annually—with children under 5 years old accounting for 40% of the total health burden and 30% of the deaths.[footnote 47] Reforms to food systems are therefore a key pathway to ending preventable deaths and building resilience to climate change. The food system is central to global food security, and prosperity, with billions depending on it for jobs and livelihoods.
Climate change is the biggest public health issue of the 21st century. Health systems are critical in protecting populations from the impacts of climate change but are themselves highly vulnerable to its impacts. Examples include the increased risk of diseases such as malaria and increasing evidence of preterm births caused by sudden high temperatures. The health system is also a substantial source of carbon emissions and local air pollution, through health service delivery, manufacture, and supply chain activities. Health systems must be developed to be sustainable and resilient to climate change in order to protect the health of the population and contribute positively to global efforts.
Box 1. SPOTLIGHT: The neglected toll of newborn deaths and stillbirths
Globally 2.4 million newborn babies die each year, a further 1.9 million babies are stillborn and 1.3 million babies survive childbirth but with major disabilities. Most deaths of newborn babies occur in the first 24 hours and 80% result from three preventable and treatable conditions: infection, breathing difficulties and complications due to prematurity. If current trends persist, more than 60 countries will not meet the 2030 SDG for reducing neonatal mortality or the global target for reducing stillbirth. This could be far higher as the pandemic related health disruptions and reduced access to quality care continues. (https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(20)30456-3/fulltext).
Box 2. SPOTLIGHT: Respectful maternity care
The issue of disrespect and abuse of women during maternity care is gaining global attention. Mistreatment can manifest itself in many ways including physical, sexual and verbal abuse, non-consented clinical care, abandonment during childbirth itself and poor facility conditions. Forty percent of women experience physical or verbal abuse during labour with higher rates among adolescents, people with disabilities and in fragile and conflict settings. Sixty percent of pregnant women are subject to vaginal examinations they have not consented to, with rates 4.6 times higher in the young and unmarried. These are huge disincentives to accessing care. (WHO)
5. We know how to save lives
We need strong, inclusive and climate-resilient health systems. We need health systems that can provide affordable, life-saving services for all women, adolescents, babies and children. These services should be part of a package based on the latest scientific evidence of what works to target scarce resources (Box 3). We also need better planning, sustainable and predictable financing, strong coordination, governance and accountability for health.
We need women, babies and children to be able to access services when they need them. This includes making services affordable and reaching the most underserved and marginalised groups who are at higher risk of preventable deaths, particularly people living in poverty, in fragile or conflict affected settings, people with disabilities and those with HIV. It also means addressing the social, legal and policy barriers which prevent women and girls from making their own informed decisions about their health, including about sex and childbearing.
We need services to be high quality and respectful of the rights of women, girls and other marginalised groups. This includes communities, and especially marginalised groups, having a voice in decisions about health services and demanding what they need. It also means having trained, paid and motivated health workers and outreach workers both in the community but also in facilities with midwifery skills. They need to have the means of referring women to the care they require and, once there, they need to have the necessary equipment and drugs. Weneed to have the necessary equipment and drugs as well as water and sanitation to avoid infection.
We need women, babies and children to be less vulnerable to illness in the first place. This includes ensuring access to healthy and sustainable diets through strong food systems to prevent malnourishment and access to effective treatment for malnutrition if it does arise. It also means ensuring environments are clean and hygienic to prevent diarrhoea and other infections and that air pollution is reduced to prevent respiratory illnesses. A shift towards supporting food systems will deliver greater combined benefits for health, climate and environment, and prosperity.
We need to work better to support countries to achieve these aims. This means helping countries to have evidence-based health plans in place and supporting these in good coordination with others. This means ensuring the majority of our investments strengthen government health, food and water systems for the long term. This also means raising our voice to advocate for the things we know are needed.
Box 3: Some examples of evidence-based health interventions and ‘Best Buys’ (DCP3 | (dcp-3.org))
Maternal and newborn health
- management of labour and delivery by skilled attendants, including basic neonatal resuscitation
- in high malaria transmission settings, intermittent preventive treatment in pregnancy
- early detection and treatment of pneumonia in newborns with oral antibiotics
- provision of kangaroo care for newborns
Reproductive health
- provision of condoms and hormonal contraceptives, including emergency contraceptives
- post-gender-based violence care, provision of emergency contraception
- insertion and removal of long-lasting contraceptives
- surgical abortion
Child health
- childhood vaccination series (diphtheria, pertussis, tetanus, polio, BCG, measles, hepatitis B, HiB, rubella)
- detection and treatment of childhood infections (iCCM)
- education on handwashing and safe disposal of children’s stools
- among all individuals who are known to be HIV positive, immediate ART initiation with regular monitoring of viral load for adherence and development of resistance
Nutrition
- breastfeeding and complementary feeding promotion
- treatment of severe acute malnutrition
- vitamin A supplementation
- iron and folic acid supplementation to pregnant women
Water, sanitation and hygiene
- hand hygiene behaviour change interventions and access to hand washing facilities
- safe (quality) and reliable water supply and sanitation in the home/compound, and the safe disposal of children’s stools
- water, sanitation, hygiene and waste management facilities in health care facilities and schools
6. What has the UK done to date?
The UK has been a leader on health systems, SRHR, nutrition, WASH, vaccines and fighting infectious diseases for decades, working in partnership with country governments, other donors, multilateral agencies and civil society organisations (CSOs). Examples include our steadfast defence of SRHR in the face of increasing attempts to rollback women’s rights; our increased influence on food systems to deliver a triple win for people, the planet and prosperity; and our placing of health firmly on the COP26 agenda. We have used our funds to bring in others through malaria matched funding and market shaping initiatives, for example. We have a robust research, development and innovation track record, including building on strong existing UK institutions and charities. We have championed the coordination and alignment of these health investments in countries and have a strong history of working with countries on their priorities to achieve common aims.
Box 4: Key achievements of UK aid in recent years
- supported immunisation of an estimated 74.3 million children, saving 1.4 million lives (2015—2018)
- supported 25.4 million women and girls to use modern methods of family planning, preventing: 8.8 million unintended pregnancies; 2.9 million unsafe abortions; saving 8,100 women’s lives; and preventing the trauma of 81,900 stillbirths and 48,300 newborn deaths (April 2019—March 2020)
- supported 55.1 million women, adolescent girls and young children with nutrition services in 25 countries (2015-2020)
- supported 62.6 million people to gain access to clean water and/or better sanitation (2015—2020)
- supported the Global Fund in 2019 to provide over 700,000 HIV-positive mothers with medicine to keep them alive and prevent them from transmitting HIV to their babies In 2019, Global Fund distributed 160 million mosquito nets, protected 8 million structures with anti-malarial indoor sprays and provided 11 million women with preventative treatment for malaria
- supported the development of 7 new drugs for malaria, more than 20 diagnostics for faster and more reliable detection of tuberculosis, malaria and sleeping sickness, a novel child friendly treatment for tuberculosis and new vaccines for rotavirus (diarrhoea)
- since 2010, FCDO’s market shaping work has contributed to huge cuts in the prices of life-saving products, such as vaccines, treatments for HIV, malaria and TB, as well as contraceptives. These price cuts have generated extra value for money of over £1 billion
- between 2011 and 2019, the UK supported 191 health partnerships and trained over 93,000 health workers across 30 countries
- we reached over 14 million people, including 2.7 million people with disabilities, with disability-inclusive public health radio messages about the risks of COVID-19 for people with disabilities and how they could protect themselves (April—December 2020)
7. Our approach
The UK will focus on four pillars of action to end the preventable deaths of mothers, babies and children—strong health systems, human rights, gender and equality, healthier lives and safe environments, and research, technology and innovation (section 8). Through each pillar, we will look to shift our approach to further increase the efficiency, equity and effectiveness of our interventions (Box 5).
We will increase our engagement, using our wide diplomatic networks and more focused technical assistance to countries. We will step up our influence of multilaterals, promoting an integrated approach aligned to country priorities and other partners. We will also work across other UK government departments on shared global health agendas and initiatives.
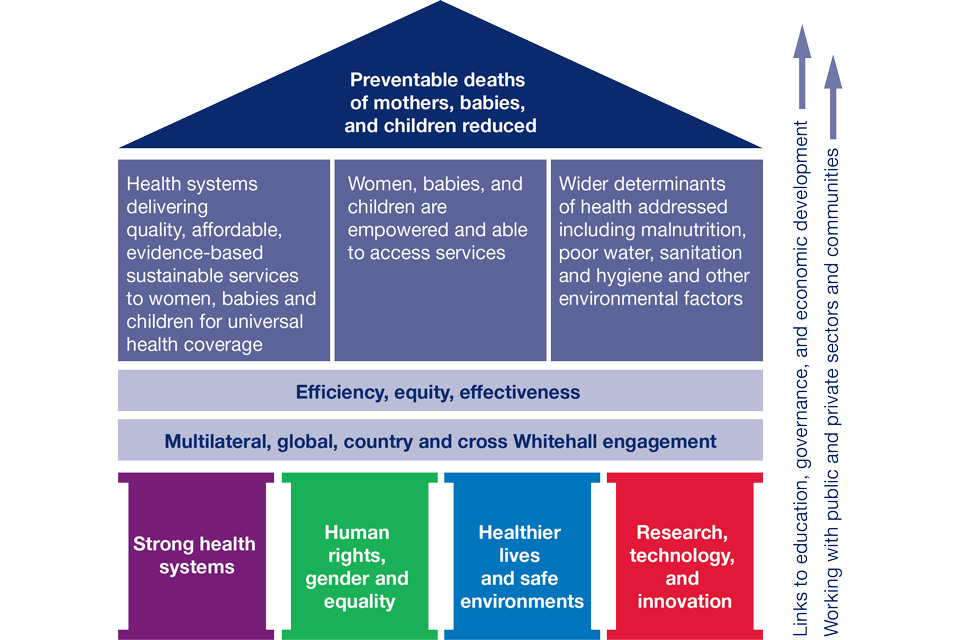
Figure 8: Theory of change for the prevention of the deaths of mothers, babies and children under 5.
Box 5: Shifts in approach
Increased efficiency:
- integration—promoting an integrated approach and prioritising interventions that lead to multiple outcomes
- alignment and coherence of all our EPD investments around government plans, encouraging other partners to do the same
- more join up across sectors and with research programmes. Work with public and private sectors and communities
Increased equity:
- more deliberate focus on reaching the poorest, women and girls, people with disabilities, the most marginalised including those living in fragility, conflict and humanitarian crises
- work with the community-based health system and grassroots organisations to increase reach, community voice and empowerment and drive accountability
Increased effectiveness:
- focus on system strengthening in all that we do on health, food and nutrition, SRHR, climate and WASH for greater sustainability, accountability and increased quality of care
- focus on evidence based, cost effective ‘Best Buy’ activities with maternal, newborn and child health outcomes. Increased use of demographic analysis to inform programmes
- shift in results measurement from attribution of short-term results to contribution to long term impact in countries
Increased engagement:
- country engagement: We will engage in all countries where the UK government has a presence and EPD-related programmes, working through others as appropriate. We will have more intensive partnerships with a small set of ‘EPD Flagship Countries’, likely to be in sub-Saharan Africa and Asia, that will be chosen dependent on need, the UK footprint, the country’s interest in engagement and the ability for this effort to catalyse change
- global engagement: We will use our voice and influence in global fora, to raise EPD’s profile and reinvigorate action. We will use our diplomatic networks and convening power to strengthen international structures and support greater coordination and coherence
- multilateral engagement: We will work with others to maximise the impact of multilateral investments on supporting sustainable, long term system strengthening and increasing equity
- cross UK government department engagement: We will be coherent and joined up in our approach with other UK government departments, especially on health systems, WHO reform, patient safety (Department for Health and Social Care (DHSC)), climate and One Health (Department for Environment, Food and Rural Affairs (Defra), Cabinet Office (CO), Department for Business, Energy, and Industrial strategy (BEIS)). We will collaborate on relevant cross government initiatives. Our research collaboration is outlined under Pillar 4
8. Four pillars of action
Pillar 1: Strong health systems
Objective: Strengthen fragile health systems to mitigate the impacts of COVID-19, deliver results at scale, and end the preventable deaths of mothers, babies and children.
Headlines
We will:
- support countries to strengthen their health systems taking an integrated, inclusive, long-term approach
- champion equity and quality in health systems, including respectful maternity care
Summary of key actions:
- influence all our health investments towards health system strengthening
- implement ending preventable death/health system strengthening focused country programmes with outcomes for mothers, babies and children
- support focused technical assistance
- explore innovative financing for health system strengthening
- champion equity and quality of care
We will work across the UK government (at the global, regional and national level) to drive a more coordinated, integrated and long-term approach to building stronger health systems to achieve Universal Health Coverage and deliver the twin aims of an end to the preventable deaths of the most vulnerable women, babies and children and enhancing global health security.
This pillar builds on decades of UK expertise and learning in supporting health systems. It will ensure our systems work meets the needs of mothers, babies and children and is rights-based, creating a strong foundation to tackle other global health issues and achieve universal health coverage. It links to and complements the FCDO Health System Strengthening (HSS) Position Paper.
We will support countries to strengthen their health systems taking an integrated, inclusive, long-term approach.
In doing this, we will reinforce the core systems needed to provide all essential health and nutrition services, manage communicable and non-communicable disease and build resilience to humanitarian crises and climate change. We will support the six building blocks of the health system (see FCDO HSS Position Paper) and the interconnections between these, focusing in particular on community and primary health care, the first port of call for many women and children.
We will support critical health workers including midwives, nurses and community health workers, focusing on training, supervision and sustainably strengthening local institutions for the long term. We will strengthen national supply chains to increase access to essential supplies and equipment needed for safe pregnancy and deliveries, care of the newborn, modern contraception, safe abortion (within national laws), HIV testing and treatment, nutrition and vaccines (see Pillar 4).
We will continue our support to the large-scale delivery of vaccines to children through Gavi and the prevention and treatment of HIV, TB and malaria through the Global Fund. We will increase efficiency by ensuring our approach to health systems strengthening within these initiatives is coherent with our bilateral and other central programmes, including through the World Health Organisation (WHO), ensuring our investments add up to more than the sum of their parts. We will look to the Global Financing Facility, other partnerships and our own technical assistance to promote greater collaboration and alignment between agencies in support of government-led health plans.
To maximise the alignment of health finance, we will encourage the streamlining of our funding with that of government and other donors, for example through pooled funds that bring together multiple partners around common aims and mechanisms. We will improve the allocation, use, efficiency and sustainability of financing through support to public financial management systems. We will also work with international finance institutions and the private sector to explore innovative finance options for health.
We will take an integrated approach, ensuring vertical programmes, that focus on tackling specific health issues and diseases including malaria, TB, HIV, polio, nutrition and family planning also support broad health system efforts to maximise the efficiency and impact of our investments on mothers, babies and children. We will adopt a multi-sectoral approach that promotes coordination and collaboration across sectors—focusing in particular on the integration of nutrition services and health, and accelerating access to climate-resilient water supply, hygiene and sanitation and low carbon services in health care facilities. We will strengthen the links between our research work on health systems and our development programmes.
We will especially advance the integration of public health functions that focus on preparing, preventing, detecting, and responding to public health threats. Data is central to this and we will advocate for one, integrated data management system at country level that includes surveillance for all infectious diseases.
Box 6. The Global Financing Facility
The Global Financing Facility (GFF) works in 36 LMICs to improve the health of women, babies, children and adolescents, through support to country owned plans or ‘investment cases’. Investment cases are prioritised according to the funding available from the GFF, other donors, private sector and domestic resources and contain key health system reforms needed to drive change. The GFF, a trust fund run through the World Bank Group (WBG), aims to increase the amount and efficiency of funding to health through strong links to and influence on the WBG and their International Development Association (IDA) as well as coordinated action and alignment with other partners. FCDO has supported the GFF since its inception. The GFF has also focused on mitigating the indirect impacts of the COVID-19 pandemic and is currently implementing a number of essential health service grants to strengthen both health systems for vaccines and for essential health service delivery. It has a strong gender focus including a SRHR acceleration plan and a gender roadmap.
Since 2015, the GFF has seen some significant results. These include an increase of 20% in uptake of antenatal care and 30% in institutional deliveries in Guinea; an increase of 30% in new users of family planning in Sierra Leone; an increase of 40% in coverage of institutional deliveries in regions within Tanzania implementing Results Based Financing; and an increase of 20% in antenatal care coverage in Mozambique. (GFF annual report, 2021).
Box 7: The Global Fund and HSS
The UK has supported the Global Fund since its establishment in 2002. Focused on ending AIDS, TB and Malaria, the Global Fund invests over $1bn per year in health systems. The new Global Fund strategy 2023-2028 sets out key changes that will further strengthen investments aligned with UK priorities, including a greater emphasis on:
-
prevention with the aim of cutting new infections including among key and vulnerable populations
-
addressing inequality and inequity that underpin the epidemics through rights-based approaches and investment in community systems and community-led approaches
-
integrated people-centred health services including support around agreed national health plans and packages of care and moving beyond processes that are disease specific.
-
sustainability in all its forms including financial (catalysing increased domestic resources), programmatic (focusing on prevention) and institutional (integrating Country Coordination Mechanisms and other specific Global Fund entities into national structures, ensuring sustainable financing of community structures)
-
resilient and sustainable systems for health with all activities strengthening broader systems where possible, as well as having benefits on HIV, TB and malaria, recognising the role of both private and public aspects of the system..
-
data and innovation to support effective decision-making with a focus on strengthening national systems for sustainable impact
-
partnership for impact, recognising the critical importance of coherence between the activities of the Global Fund and those of other global health initiatives (particularly at country level)
We will champion equity and quality in health systems, including respectful maternity care.
We will advocate and support the integration of quality of care into our bilateral and multilateral health programmes and be a global champion for quality of care. A key part of quality is ensuring respectful maternity care and we will work with others to promote this within the countries where we work.
Among the most marginalised groups are the poorest, adolescents, people with disabilities and affected by HIV and those living in fragile and conflict affected settings. We will champion their rights and increase their visibility and voice to enable powerful engagement with decision making at all levels of the health system. We will promote greater disaggregation of data to provide information on who and where these groups are and what their needs are. We will support Gavi, Global Fund and the GFF’s approach to improving equity, the former including focusing on reaching unvaccinated (zero-dose) children to find families most left behind.
In fragile and conflict affected settings and humanitarian crises, where mortality rates are some of the highest, we will work harder to reach the women, adolescents, babies and children most affected. This will mean increasingly covering humanitarian needs through longer-term health systems strengthening interventions, helping systems flex in response to displacements of populations and to prevent and treat severe acute malnutrition, whilst enhancing local capability to anticipate and prepare for new shocks such as cholera outbreaks. We will advocate for the scale up in the use of the minimum initial service package of SRHR interventions in acute crises and will support the efforts of Global Health Initiatives such as Gavi and GFF to find innovative ways to deliver in these settings, using non-state providers.
Box 8: Strengthening health systems in Kenya
The FCDO Maternal and Newborn Health programme in Kenya aims to sustainably improving the quality of maternal, newborn and child health (MNCH) services. The programme takes a health systems strengthening approach with emphasis on improving the quality of human resources for health through pre- and in-service training and mentorship on Emergency Obstetric and Newborn Care (EmONC), enhancing essential MNCH commodity security and promoting the use of appropriate low-cost high impact technologies. In the last two years, the programme has supported legislative processes in several counties (sub-national governance units) aimed at securing domestic funding for health services. The Facility Improvement Fund Acts aim to ringfence health revenue for use by the generating facilities and also facilitates engagement between health facilities and the national hospital insurance fund (NHIF) to address bottlenecks in the disbursement of claims—a key source of revenue for public and private health facilities. The programme is on course to train 11,500 health care workers in EmONC by March 2023 and enhance pre-service training in 42 nursing colleges.
The programme is part of FCDO’s wider engagement on EPD—in January 2021, Kenya and UK signed a memorandum of understanding that provides for bilateral and multilateral support though initiatives like Global Financing Facility, Global Fund and Gavi aimed at strengthening the Kenyan health system to deliver universal healthcare coverage (UHC) and end preventable maternal, newborn and child deaths.
| Key actions | Shift |
|---|---|
| Advocate for health system changes for EPD through global, regional and national level political engagement using diplomatic networks and key partnerships such as the Partnership for Maternal, Newborn and Child health (PMNCH). | Country and global engagement |
| Influence the major health multilaterals and global health initiatives to align their investments with national health plans and embed a long term, integrated health systems strengthening approach, using FCDO country-based advisers where possible. | Efficiency, country and multilateral engagement, equity |
| Promote WHO’s technical leadership on EPD—including sexual, reproductive, maternal and newborn health, nutrition, health systems, quality of care, water sanitation and hygiene, and climate. | Multilateral engagement |
| Implement EPD focused programmes with a strong health systems approach in a range of low and low-middle income countries. | Country engagement and effectiveness |
| Support focused technical assistance to countries drawing on the FCDO health network, UK government expertise, central programmes and links with academia/research community. | Country engagement and effectiveness |
| Explore innovative health and nutrition financing mechanisms to strengthen health systems through the private sector, development banks and other partners. | Efficiency and effectiveness |
| Champion equity and quality of care in systems approaches globally, working through multilaterals to support national health equity and quality of care policies. Include technical assistance for quality midwifery skills and respectful maternity care. | Country and multilateral engagement, equity and effectiveness |
| Influence partners to support harmonised national health information systems to improve results measurement and continue to monitor our own programmes, including better population level data for long term planning. | Country and multilateral engagement and efficiency |
Pillar 2: Human rights, gender and equality
Objective: Accelerate progress on sexual and reproductive health and rights, gender and equalities, and human rights that are central to ending the preventable deaths of mothers, babies and children.
Headlines
We will:
- boldly defend, progress and champion universal sexual and reproductive health and rights and other rights fundamental to ending preventable deaths
- integrate a human rights-based approach into the UK’s global health effort
Summary of key actions:
- defend and advance human rights and equality, including gender equality and sexual and reproductive health and rights, through global influence and support to key partnerships
- champion and support grassroots and rights-based efforts and movements
- strengthen rights-based approaches in health systems
- promote the rights and visibility of marginalised groups, including through data disaggregation
The UK has a long history of evidence-based international leadership to defend and advance gender equality and human rights, including sexual and reproductive health and rights[footnote 48], often venturing where others are cautious to go. The UK is committed to the principle of non-discrimination on all recognised grounds, including on the basis of sexual orientation and/or gender identity.

Poverty, harmful social norms, gender relations, stigma, discrimination, laws and policies, as well as the state of the health system itself, all undermine the ability of people to enjoy their right to the highest attainable standard of physical and mental health, free from discrimination, coercion, exploitation and violence. Women, girls, people with disabilities, adolescents and other marginalised groups face the risk of preventable death and severe injury and harm when their ability to make informed decisions about their own bodies, health and lives, and to access and use quality services, is restricted. Sexual and reproductive health and rights are often particularly restricted. All this in turn also affects children’s chances of survival. These social and gender norms and power/economic imbalances also underpin various forms of abusive behaviours and practices including sexual abuse and exploitation and sexual harassment.
This cross-cutting pillar outlines the actions we will take to support human rights that are critical to saving—and transforming—the health and lives of all people, including women, babies and children. This will include but is not limited to a major focus on sexual and reproductive health and rights. We will follow the principle that our work should be intersectional, anti-racist, and endeavour to place power in the hands of local actors.
Box 9. International Commitments at the G7: Foreign & Development Communique
- We recognise universal access to quality and affordable comprehensive sexual and reproductive health services, including comprehensive sexuality education, as life-saving and critical to achieving universal health coverage. The G7 reaffirms our full commitment to the SRHR of all individuals. We further recognise their right to the enjoyment of the highest attainable standard of physical and mental health, which should be enjoyed free from discrimination, coercion, exploitation and violence. We commit to working together to prevent and address the severe impacts on SRHR from the pandemic. We commit to intensify our efforts, including by working with other countries and civil society, to accelerate progress towards the universal enjoyment of SRHR, with specific attention to the most marginalised and inadequately served groups, including adolescents, those belonging to racial and ethnic minority groups, and LGBTQI+ individuals.
Box 10. Catalysing collective action and youth engagement
The UK has supported global advocacy movements and networks such as the Partnership for Maternal, Newborn and Child Health (PMNCH), a global network of over 1,000 members, and the family planning partnership FP2030, closely linked to countries that have committed to family planning actions. Both organisations work to advocate, drive action and hold key stakeholders including governments, civil society and donors accountable for delivering change.
The voices of young people are increasingly being placed at the heart of these efforts. Through its network of youth led organisations, young people are being supported to participate in the global FP2030 processes. While PMNCH has galvanised the global community to make adolescent health a priority through its Call to Action on Adolescent Wellbeing, co-created by young people themselves.
We will boldly defend, progress and champion universal sexual and reproductive health and rights and other rights fundamental to ending preventable deaths.
Using the UK’s voice on the world stage, we will steadfastly defend human rights and promote gender equality and inclusion for all across all settings. Building on our commitments at the United Nations and G7, we will continue to promote SRHR, positive social norms and women and girls’ autonomy and physical integrity, including safe and legal abortion, and champion other neglected or stigmatised issues such as respectful maternal care, ending child marriage and female genital mutilation (FGM), menstrual health, period poverty and stigma, the health of people with disabilities, LGBT+ people, sex workers and other inadequately served populations.
Working with our valued likeminded partners, we will push for progress in the UN using global and regional moments. We will actively engage in global advocacy and accountability networks and partnerships which progress rights to save lives.
We will listen to, include and champion the voices and needs of marginalised and inadequately served groups, and all those who face stigma, discrimination and exclusion which negatively impacts their health outcomes, particularly their sexual and reproductive health. We will increase the visibility of women, young women and men, people with disabilities, LGBT+ people and their representative organisations within our advocacy and programmes, following the principle that people should be involved in decisions that concern them and their health.
We will advocate on these matters, and support human rights defenders, grassroots organisations and movements that are driving change, particularly on neglected and stigmatised issues such as safe abortion, child marriage, FGM, and key populations living with or at risk of HIV. Using our diplomatic missions and relationships in countries, we will respond to in-country and regional dynamics, and provide safe convening spaces for civil society working on these issues, particularly where civic space may be restricted.
We will continue to promote global commitment to preventing sexual exploitation, abuse and sexual harassment (SEAH) by calling on all delivery partners to adhere to international standards, the OECD DAC recommendation on ending SEAH and strengthen implementation on standards set at the 2018 (UK hosted) Safeguarding Summit.
We will integrate a human rights-based approach into the UK’s global health effort.
We will promote the human right to the highest attainable standard of health, understood as spanning the availability, affordability, acceptability, and quality of services provided by the health system, individuals’ agency and autonomy in relation to their own health, and their ability to have a voice in the system and hold providers and policymakers to account., We are guided by the International Covenant on Economic, Social and Cultural Rights, related standards, the International Conference on Population and Development and Programme of Action and the outcome documents of the review conferences, and the WHO Resolution on the Highest Attainable Standard of Health for Persons with Disabilities. This will include expanding our own understanding and application of human rights-based approaches in health.
We will also embed our approach into the refreshed FCDO Strategic Vision on Gender Equality, and across FCDO priorities, particularly open societies, girls’ education, humanitarian, and climate work. We will champion disability inclusion across FCDO’s health portfolio, underpinned by the Disability Inclusion Strategy.
We will prioritise country and global investments that adopt an evidence and rights-based approach. FCDO programmes and efforts will aim to reach the most marginalised with quality services, and tackle discrimination, restrictive social norms, laws and policies. We will support specific initiatives that apply rights-based approaches across the four EPD pillars including embedding empowerment and accountability into systems strengthening efforts for health, nutrition and WASH.
We will champion the development and use of improved data for health equity and rights-based approaches, including through the launch of the new FP2030 measurement framework as well as initiatives in other critical areas, including those which are hard to measure such as changes in social norms. UK aid programmes will continue to generate new evidence and learning across gender and rights issues including those that are critical for ending preventable deaths.
| Key actions | Shift |
|---|---|
| Advance human rights and equality, including gender equality, through the Global Disability Summit, the Adolescent Summit, Democracy Summit, the International Conference on Family Planning, the LGBT+ Rights Conference, UN convenings and other moments. | Global engagement and equity |
| Engage with partnerships, including on family planning, FP2030, PMNCH, the Sanitation and Water for All and the Equal Rights Coalition. | Country and global engagement and equity |
| Champion and support grassroots and rights-based efforts and movements on neglected issues including FGM and safe abortion, and those led by women, minorities and marginalised groups. | Country engagement and equity |
| Embed gender, equity and rights principles into the large health multilaterals and global health initiatives, including through FCDO Global Fund equity and country-based advisers where possible. | Country and multilateral engagement and equity |
| Support health systems initiatives that aim to integrate a rights-based approach e.g. the GFF SRHR accelerator. | Country and multilateral engagement and equity |
| Carry out internal training on rights-based approaches in health. | Effectiveness |
| Champion efforts to expand the evidence base on human rights, gender and equality. | Effectiveness and equity |
| Promote interventions that safeguard against SEAH in national discourse, policies and programmes. | Effectiveness |
| Promote data disaggregation, including by disability, using the Washington Group Question Sets where appropriate, to build up evidence of what works. | Effectiveness and equity |
| Advocate for the inclusion and increased visibility of people with disabilities and adolescents within UK health investments. | Global engagement and equity |
Pillar 3: Healthier lives and safe environments
Objective: Strengthen the wider systems needed to end preventable deaths—reducing malnutrition through safe, healthier and sustainable food systems; transforming access to climate resilient water supply, hygiene and sanitation services; and addressing the health impacts of climate change.
Headlines
We will:
- promote the transformation of food systems to make safe and nutritious diets accessible to women and children
- work with countries and partners to strengthen systems and institutions to deliver safe climate resilient water, sanitation and hygiene services in communities, schools and health facilities
- work with countries to understand and address the sources and impacts of air pollution on health
- support countries to implement COP26 health commitments on climate resilient and sustainable low-carbon health systems and integrate health outcomes into climate change policy and programme plans
Summary of key actions
- empower, influence and work with countries, partners and the private sector to tackle malnutrition, WASH and the need for climate resilient health systems
- integrate WASH and nutrition into other sector investments
- focus on improving nutrition and WASH in areas of fragility and conflict
- further develop the evidence base for climate resilient health systems
This pillar sets out how we will support healthier lives and safer environments. It outlines a shift in approach from WASH and nutrition direct delivery of services, to strengthening the systems underpinning these services, using strong partnerships and technical assistance driven by evidence and innovation.
We will focus on the specific needs and vulnerabilities of the most marginalised women, adolescent girls, babies and children within their communities, places of work, institutions and their environments. To do this, we will promote equitable access to nutritious diets through safe and sustainable food systems to reduce malnutrition in all its forms and strengthen climate resilience; transform access to safe and resilient water supply and sanitation services and improve people’s hygiene; establish a new global trajectory to help tackle the spiralling threat of air pollution; and increase our focus on addressing the health impacts of climate change and build resilient, sustainable health systems.
We will promote the transformation of food systems to make safe and nutritious diets accessible to women and children.
We will maximise the impact of FCDO investments in areas such as agriculture, economic development, climate and social protection to build sustainable food systems that make safe and nutritious diets more affordable, accessible and climate resilient.
We will continue to contribute to impactful global action on nutrition including through the advocacy of the Scaling Up Nutrition Movement[footnote 49] and by promoting the implementation of commitments made at global events such as Nutrition for Growth.
We will increase the share of UK food systems investments that contribute to safe and nutritious diets by promoting nutrition as a core objective of these investments. We will work together with others, empowering and supporting their actions to strengthen the resilience of food systems and prevent famines. We will support government policy and multi-sectoral plans in partner countries that help improve diets and enable greater investment in sustainable food systems that make nutritious foods more affordable and available. We will promote more responsible business practices, among others by enabling effective accountability mechanisms.
We will promote, support and advocate for better coherence in a fragmented financing landscape and foster innovative and creative approaches to enable financing and funding solutions to malnutrition.
Box 11. The Access to Nutrition Initiative
The food industry has a major role to play in enabling women and children to access safe, nutritious diets, yet less than a third of the world’s leading food manufacturers’ products can be considered healthy. Holding companies to account for their practices is an important means to incentivise greater action on nutrition. FCDO has been supporting the Access to Nutrition Initiative (ATNI) to promote greater business transparency and accountability.
By assessing and ranking the world’s largest food manufacturers on their nutrition-related commitments, practices and performance globally, ATNI aims to encourage companies to increase consumer access to nutritious and affordable foods and beverages through actions related to product formulation, pricing and distribution. ATNI also aims to responsibly exercise their influence on consumer choice and behaviour through actions in areas such as marketing, labelling and promoting healthy diets and active lifestyles. ATNI’s global and national company benchmarks and its engagement with businesses and investors are important instruments to influence improvements in company performance. The ultimate goal is to facilitate improved diets and a reduction in the serious global problems of both obesity and undernutrition.
We will work with countries and partners to strengthen systems and institutions that enable the delivery of safe water, sanitation and hygiene services in communities, schools and health facilities.

Building on our experience of large-scale programming and long-standing strategic partnerships, including across UK academia, private sector, charities and government departments, we will shift our focus to work with countries to strengthen water, sanitation and hygiene systems, ensuring that these are inclusive, reliable and resilient to the impacts of climate change. We will do this by strengthening accountability, collaboration and partnerships, providing bespoke technical assistance to strengthen key components of WASH delivery systems, introducing new technologies and attracting new finance. Our areas of focus will include providing WASH in healthcare facilities, enable handwashing and hygiene practices, and establishing durable, climate-resilient solutions in water-scarce fragile and conflict affected states, where reaching the most vulnerable requires us to bridge the divide between humanitarian and development programmes.
Box 12. WASH in healthcare facilities, Mozambique
Clean water, sanitation and hygiene are critical for quality of care in health care facilities. Clean delivery kits together with hand washing facilities save the lives of mothers and babies. The UK has worked closely with the national and local authorities in Mozambique, through its partnership with UNICEF, to improve WASH services in communities, schools and healthcare facilities. Clean and renewable energy through solar panels provides electricity to run facilities and provide water. As a result of technical support national standards and norms for WASH in health care facilities were developed to be applied progressively across the country. Maintenance and operation funds for the WASH and waste management facilities are now included in annual district budgets. Mozambique also tracks progress through its national health information system, and on the WHO WASH in Health Care Facilities global tracker, following recommendations published in 2020 and in line with resolution 71.2 (2019) to accelerate progress on WASH in health care facilities.
We will support countries to understand and address the sources and impacts of air pollution on health.
Building on our existing work on promoting clean cooking and clean energy, we will work across sectors to deepen our understanding of the causes and human impacts of poor air quality in LICs and LMICs and the policy and programmatic responses to address these. We will support global knowledge, evidence and expertise sharing through mechanisms such as the UK-Chaired Forum for International Cooperation on Air Pollution.
We will support countries to implement COP26 health commitments on climate resilient and sustainable low-carbon health systems and integrate health outcomes into climate change policy and programme plans.
We will support the integration of climate resilience and sustainability into our work on health system strengthening through FCDO’s bilateral and multilateral initiatives, and through our global and local partnerships. We will use these mechanisms to ensure that health systems are included in wider climate change mitigation and adaptation planning.
| Key actions | Shift |
|---|---|
| Empower and influence governments and private business to roll out appropriate, cost-effective, responsible solutions to tackle malnutrition, strengthen food systems, improve healthy diets and enable safe and sustainable agriculture and land use practices. | Country engagement and effectiveness |
| Integrate nutrition objectives into UK investments and influence others externally to do the same, promoting increased accountability to this. | Effectiveness |
| Work with international partners and country governments to increase and broaden global commitment and financing to ending malnutrition in all its forms. | Global and country engagement |
| Strengthen the resilience of services to prevent and treat wasting in fragile contexts through strengthened government services and co-ordinated UN services. | Country engagement and effectiveness |
| Improve WASH governance, collaboration and accountability through Sanitation and Water for All, the WHO/UNICEF Joint Monitoring Programme; WHO’s work on norms, standards and regulation, the WASH in Health Care Facilities taskforce and the Global Water Partnership. | Global engagement |
| Catalyse action to accelerate the provision of climate-resilient WASH services in countries facing increasing water insecurity, including in fragile contexts. | Country engagement and effectiveness |
| Advance the evidence and collaboration on hygiene behaviour change, building on previous partnerships between academia, global initiatives and the private sector. | Global engagement and effectiveness |
| Mobilise partners to provide specialised support to countries on tackling air quality, including from WHO, the UK Met Office and Defra. | Country engagement and effectiveness |
| Strengthen our engagement with the Risk Informed Early Action Partnership[footnote 50] ensuring that health is integrated into an all-hazard approach to climate related disaster preparedness and response. | Global engagement |
| Ensure an evidence-based focus in work on climate change mitigation and adaptation, maximising sustainable and resilient health outcomes through work with development banks and other development institutions. | Global engagement and Effectiveness |
Pillar 4: Research, technology and innovation
Objective: Build on UK support for science, research and innovation to build the best available evidence and increase access to new health technologies such as medicines, vaccines, diagnostics and innovative service delivery for mothers, babies and children and to tackle the most serious infectious diseases.
Headlines
We will:
- support research to improve the delivery of health and nutrition services at scale
- use research and innovation to improve equitable access to safe, affordable technologies such as medicine, vaccines, tests, contraceptives and digital products
Summary of actions:
- support research, product development and market shaping partnerships
- support the evaluation, synthesis and dissemination of evidence
- implement innovation for climate resilient food systems
The UK has a robust reputation for science, research and development, and innovative market shaping initiatives. We will continue to play a leading role in supporting innovation and access to new products, technologies and services for mothers, babies and children, including better diagnostic tools and new vaccines. Through our investments into key product development partnerships (PDPs), the UK has helped to develop novel diagnostics and treatments for infectious diseases and vaccines for meningitis and rotavirus. Through working with partners to pool purchasing or to bring new low-cost suppliers to market, we have accelerated access to new products. Since 2010, these have delivered at least a halving in the price of key childhood vaccines, medicines for HIV, malaria, tuberculosis and long-acting contraceptives. These are global public goods that can enable a step-change in our ability to tackle preventable deaths.
The Integrated Review highlights the critical importance that the UK assigns to science and technology, research and development and generating evidence of what works. Three HMG departments bring complementary strengths to the UK research offer to end preventable deaths: FCDO, DHSC through the National Institute of Health Research (NIHR) and BEIS through the UK Research and Innovation-Medical Research Council (UKRI-MRC).
Box 13. Working together on research saving lives
UK funded joint research grants are addressing preventable deaths in low-income countries. These include the Joint Global Health Trials (JGHT) supported by DHSC, FCDO, UKRI/MRC and Wellcome and the Joint Health Systems Research Initiative supported by FCDO, UKRI/MRC, Wellcome and the ESRC. For example, infection with malaria in pregnancy can have severe consequences for both mother and baby but recommended interventions were based on findings from sub-Saharan Africa. JGHT funded the first trial in the Asia-Pacific region to determine the effectiveness of several strategies to prevent malaria in pregnancy and was able to identify the best combination of antimalarial prevention in Indonesia.
We will support research to improve the delivery of health and nutrition services at scale.
We will continue to support a range of important applied health research mechanisms that include Research Programme Consortia, as well as research platforms and partnerships. This support enables us to focus on specific research gaps in ending preventable deaths of mothers, babies and children, as well as research on health systems that underpin health services for mothers, babies and children. Some of this research is jointly funded by a number of UK government and academic departments.
We will focus on evidence synthesis, dissemination and policy uptake of best practices for reproductive, maternal, newborn and child health, health systems, neglected tropical diseases, WASH and nutrition. This includes engaging with policy makers and health programme implementers throughout the research cycle as well as dissemination through academic journals. Programmes have strong links with country-based research institutions and we will further increase our engagement with our own FCDO country posts to maximise policy influencing and scale up. We will also explore ways to support countries to identify their research needs and develop their own coherent, prioritised research agenda ensuring stronger links between research and policy.
Our continuing research in water security, urban sanitation and smart technologies will help to end preventable deaths through new cost-effective solutions that will help poor households gain access to affordable, reliable and resilient WASH services.
We will continue to support research and innovation for sustainable agriculture and food systems that deliver healthy diets, supporting efforts across UK government agencies, including exploring ‘One Health’ initiatives focused on livestock vaccines for diseases with the potential to spillover to humans and also developing climate resilient crops and technologies.
Box 14. UK funded Product Development Partnerships are harnessing new technologies at affordable prices
Diagnostic technology: New diagnostics for faster detection of tuberculosis, with detection reduced from 6 weeks to less than 5 hours.
Medicines development: Eight new drug combinations for malaria and early treatments for children before reaching the hospital, estimated to have saved more than a million lives since 2009.
Vaccine development: Two new vaccines to treat rotavirus (that causes diarrhoeal diseases) for use in India and a new meningitis vaccine that will prevent thousands of deaths annually. The UK Vaccine Network and other partners are also supporting the development of vaccines for epidemic diseases including Zika, Plague and Ebola.
We will use research and innovation to improve equitable access to safe, affordable technologies such as medicine, vaccines, tests, contraceptives and digital products.
FCDO will support product development partnerships that harness the best of the public, private and academic sectors to develop, trial and test new technologies for use in LMICs at affordable prices and help ensure that, once developed, products are affordable and accessible in LICs and LMICs.
We will work with partners to build and shape markets for life saving drugs, nutrition commodities, contraceptives, vaccines and other new health technologies to ensure they are available in the poorest countries at lower prices as early as possible. We will also continue to bring these market shaping approaches to product areas where they can be transformative in terms of improving access, such as for assistive technologies like wheelchairs, hearing aids and prosthetics.
Competitive markets with multiple quality-assured suppliers and transparent pricing deliver more affordable prices, shorter delivery times and allow a rapid rollout of innovative health products. We will partner with others to strengthen commodity markets and work to improve equitable access to new health products.
COVID-19 accelerated the use of digital, mobile and remote technologies to reach people and the potential for expansion is huge. We will explore new opportunities to support this shift and also ensure that this is implemented in an inclusive and responsible way.
| Key actions | Shift |
|---|---|
| Support Product Development Partnerships to develop life-saving technologies, including novel diagnostics, treatments and vaccines. | Effectiveness |
| Work with market-shaping organisations to strengthen access and affordability of life-saving innovations. | Efficiency and effectiveness |
| Support applied health research partnerships, including but not limited to the FCDO Research Programme Consortia; Special Programme of Research, Development and Research Training in Human Reproduction at WHO. Programmes include filling evidence gaps on SRHR in FCAS, the newborn period and on adolescent health and wellbeing. | Effectiveness |
| Support platforms that evaluate and synthesise evidence for best possible and sustained policy uptake. | Effectiveness and efficiency |
| Implement innovation for climate resilient food systems through a new cross-HMG coordination mechanism (the ‘Gilbert Initiative’) | Effectiveness |
| Further operational research into smart technologies, business models and city-wide inclusive sanitation to transform the reliability and resilience of water supply, hygiene and sanitation services in the face of climate change. | Effectiveness |
9. Monitoring Progress
Progress on this Approach Paper will be monitored using a framework based on that shown below. This includes a mix of country level indicators that will track national progress, and indicators specific to UK activities, programmes and shifts in approach. At a high level, the aim of the approach is to decrease the mortality rates of mothers, newborns and children under five by 2030, with expected impact on SDG goals on nutrition and WASH as well. Key outcome level changes will be essential including increasing progress towards Universal Health Coverage.
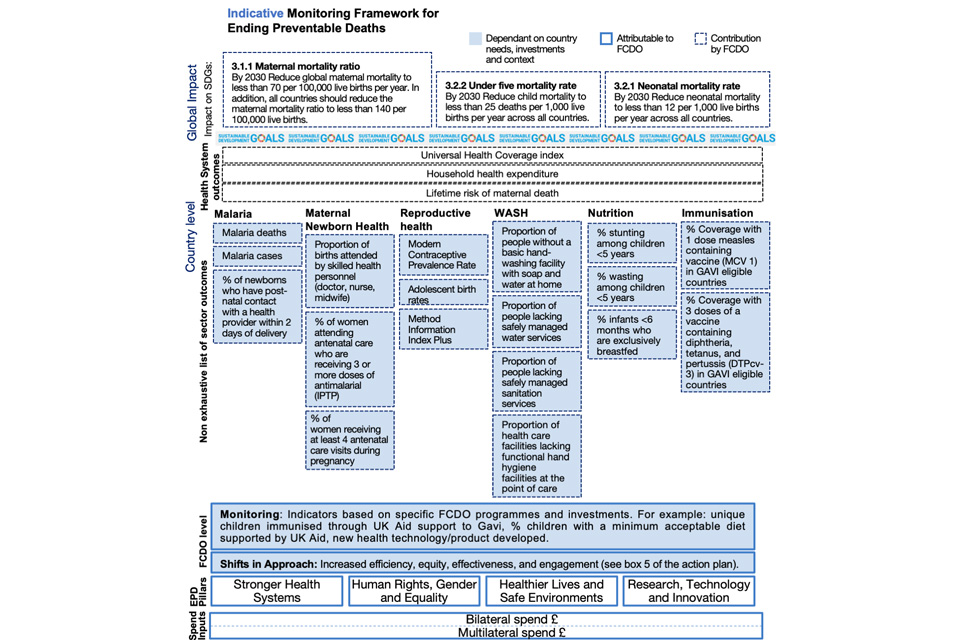
Figure 9: Indicative monitoring framework for ending preventable deaths
-
Based on https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/ and https://childmortality.org/ estimates ↩
-
Based on https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/ and https://childmortality.org/ estimates ↩
-
https://www.who.int/news/item/15-07-2021-covid-19-pandemic-leads-to-major-backsliding-on-childhood-vaccinations-new-who-unicef-data-shows ↩
-
WHO 2021 pulse survey ↩
-
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31647-0/fulltext ↩
-
Indirect Effects on Maternal and Child Mortality from the COVID-19 Pandemic: Evidence from Disruptions in Healthcare Utilization in 18 Low- and Middle-Income Countries. Lancet pre-print, 9th Sep 2021 ↩
-
https://www.medrxiv.org/content/10.1101/2021.06.08.21258546v1 ↩
-
State of Food Security and Nutrition in the World report, 2021 ↩
-
https://unstats.un.org/sdgs/report/2020/The-Sustainable-Development-Goals-Report-2020.pdf ↩
-
https://unstats.un.org/sdgs/report/2021/The-Sustainable-Development-Goals-Report-2021.pdf ↩
-
The Lancet commission on Quality of Care, 2018. ↩
-
https://washdata.org/sites/default/files/2021-07/jmp-2021-wash-households.pdf ↩
-
The economic growth potential that can result from shifts in a population’s age structure, mainly when the share of the working-age population (15 to 64) is larger than the non-working-age share of the population (14 and younger) ↩
-
UNPD, 2019 ↩
-
The Bottom Billion originated from Paul Collier, arguing there are just under 60 countries that have seen no economic growth in the last 3 decades. These are home to almost 1 billion people ↩
-
Air Pollution and Child Health, WHO, 2018 ↩
-
Food Safety, Climate Change and the Role of the WHO, WHO, 2018 ↩
-
Universal Health Coverage means that all individuals and communities receive the health services they need without suffering financial hardship ↩
-
Marginalised groups include ethnic minorities, women and girls, people with physical and mental disabilities, and Lesbian Gay Bisexual Transgender Queer and Intersex (LGBTQI) people ↩
-
https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(18)30059-7/fulltext ↩
-
https://www.who.int/news-room/fact-sheets/detail/maternal-mortality ↩
-
https://www.who.int/pmnch/knowledge/publications/PMNCH_WCAH_brochure.pdf?ua=1 ↩
-
https://www.guttmacher.org/fact-sheet/investing-sexual-and-reproductive-health-low-and-middle-income-countries ↩
-
http://dcp-3.org/chapter/1938/human-capital-and-productivity-benefits-early-childhood-nutritional-interventions ↩
-
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)62105-4/fulltext ↩
-
https://www.who.int/news-room/spotlight/the-impact-of-covid-19-on-global-health-goals ↩
-
Between 2000 and 2017, maternal deaths have reduced by 35%, child deaths by 44% and newborn deaths by 37%. ↩
-
https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality ↩
-
Lifetime risk is the probability that a 15-year old woman will eventually die from a maternal cause. Data from WHO mater-nal mortality report. ↩
-
UNICEF 2020 ↩
-
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)60937-X/fulltext ↩
-
Don’t Pollute My Future! The impact of environment on children health and Inheriting a Sustainable World : Atlas on Children’s Health and the Environment, both WHO Geneva, 2017. ↩
-
https://www.thelancet.com/journals/lancetarticle/PIISO1406736(13)60937-X/fulltext ↩
-
Adding It Up: Investing in Sexual and Reproductive Health, Guttmacher Institute ↩
-
Riley T et al., Adding It Up: Investing in Sexual and Reproductive Health 2019—Methodology Report, New York: Guttmacher Institute, 2020 ↩
-
Gavi Board approves new push to reach unvaccinated children worldwide, Gavi, the Vaccine Alliance ↩
-
WHO’s Framework on Integrated People Centred Health Services described high quality care a care that has the follow-ing domains: “safe, effective, people centred, timely, efficient, equitable and integrated ↩
-
Lancet commission on Quality of Care, 2018 ↩
-
WHO fact sheet on Quality of Care, July 2020 ↩
-
WHO FERG, 2015 ↩
-
We endorse the Guttmacher-Lancet Commission definition of sexual and reproductive health and rights. ↩
-
Since 2010, the SUN Movement has brought together a coalition of governments, civil society, the United Nations, donors, businesses and researchers to work collaboratively. to end malnutrition, in all its forms ↩
-
The Risk-informed Early Action Partnership, established with UK support and hosted by IFRC brings together stakeholders across the climate, humanitarian and development communities with the aim of making 1 Billion People Safer from disaster by 2025 ↩
