EMG/SPI-B/TWEG: Mitigations to reduce transmission of the new variant SARS-CoV-2 virus, 22 December 2020
Updated 26 October 2021
Mitigations to Reduce Transmission of the new variant SARS-CoV-2 virus SAGE-EMG, SPI-B, Transmission Group, 23 Dec 2020
1. Executive summary
-
A new variant of the SARS-CoV-2 virus (VOC-202012/01, variant B.1.1.7 - ‘new variant’) has been identified in the UK. It is increasing rapidly in London, the East and the South East of England. While levels are currently low in other parts of the country there is a high likelihood that the new variant will spread rapidly in these areas unless stringent control measures are applied (medium confidence).
-
Previously identified personal, procedural, engineering and societal mitigations to reduce transmission of SARS-CoV-2 virus all continue to apply to the new variant, but are likely to require a step change in rigour of application given that the new variant is likely to represent a significantly increased transmission risk (high confidence).
-
It is essential to reinforce the core principles of a hierarchy of control measures to reduce physical transmission through the environment by all routes – close-range, airborne, and via surfaces, given the risks that transmission of the new variant may be higher for all these routes (medium confidence).
-
Primary actions to reduce transmission including: reducing social contacts; effective testing and tracing; robust outbreak identification and control; support to ensure effective isolation and quarantine; and population vaccination remain essential. Population level approaches to further reduce contact between people are likely to be necessary, such as extending Tier 4; changing the operation of schools or universities; travel restrictions between regions and internationally; and or introducing a national lockdown (high confidence).
-
As a consequence of the uncertainty around the mechanisms for increased transmission, enhanced mitigation measures are likely to be necessary including: reconsidering the 2 metre rule and requiring that where regular interactions less than 2 metre are necessary this should include correctly worn face coverings; enhancing ventilation rates to account for possible higher viral loads; and reinforcing the importance of using face coverings, including in settings where they are not currently mandated, such as education, workplaces, and crowded outdoor spaces (medium confidence).
-
The importance of reducing the risk of transmission through rigorously applying mitigation measures needs to be communicated to the public in the context of the increased risk of transmission and the season. Communications should focus on alerting the public and organisations that:
(a) previous levels of adherence to preventive measures are unlikely to sufficiently reduce transmission of the new variant, especially in winter; and
(b) environmental and personal measures can still reduce transmission if applied more rigorously, including within the home environment (high confidence).
- A new, intensive, culturally tailored communication and support strategy should be developed, employing rapid co-design with all sectors in society (high confidence). The strategy should focus on positively encouraging and supporting the additional behaviours required to control a more infectious virus strain, particularly:
- reducing indoor contacts to the lowest level possible;
- high adherence to testing and self-isolation if symptomatic or a contact of a case;
- consistent use of high-quality face-coverings whenever indoor close contact mixing is unavoidable;
- approaches to enable effective ventilation of enclosed spaces.
2. Part 1: Evidence Summary on Implications for Mitigations
-
A new variant of the SARS-CoV-2 virus (VOC-202012/01, variant B.1.1.7) has been identified in the UK. A new variant has also been identified in South Africa. Current evidence is limited but to date there is no indication that these new variants are transmitted in fundamentally different ways from other variants of the virus (medium confidence).
-
NERVTAG’s early review of four analytical approaches suggests that this new variant could be associated with an R number that is 0.39 (95% CI: 0.24:0.55) higher than other lineages, a growth rate that could be 71% (95% CI:67% to 75%) faster per generation than other variants, a decrease in cycle threshold (CT) value of 2, a potential increase in viral load. NERVTAG have high confidence that the variant can spread faster than other variants in the UK, but it is not possible at this stage to draw conclusions on any underlying mechanisms for possible increased transmissibility[footnote ],[footnote ]. Initial analysis suggests the new variant could be becoming the dominant strain circulating in some parts of the UK.
-
Within this paper we consider the modes of transmission from infected to susceptible people and consider the implications of higher transmissibility from an environmental perspective. Despite the lack of evidence for the mechanisms, higher transmissibility suggests that for a given exposure there is a greater likelihood of infection, and hence there is a need to take further actions to reduce exposure to the virus in order to mitigate risks. Environmental mitigations form part of these actions (high confidence).
-
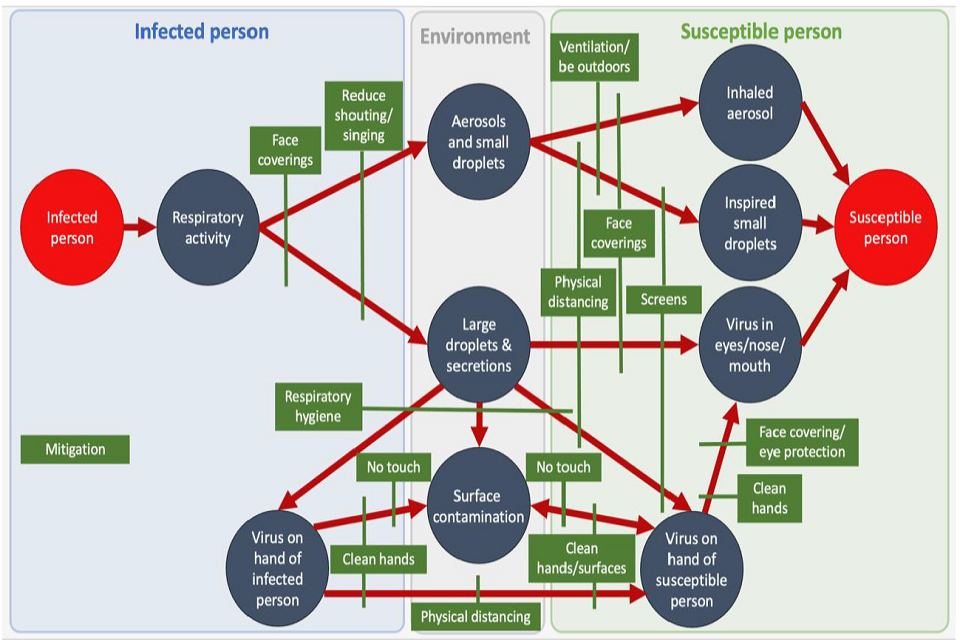
The SARS-CoV-2 virus is transmitted via direct physical contact, close range aerosols and droplets (greatest risk at less than 2 metre), longer range fine aerosols (which can pose a risk beyond 2 metre) and contaminated surfaces. Figure 1 illustrates how the virus can spread between infected and susceptible people via the environment they share. It is possible that the viral load is higher in those with the new variant, which could increase the amount of virus generated by respiratory activity. This would impact on all transmission routes. It is likely that close range interactions will remain the highest risk for transmission for the new variant; however it may be the case that all routes of transmission are enhanced, which could change the balance of their importance in some settings.
-
A hierarchy of control measures should continue to be applied to establish the right measures to mitigate transmission of the new virus variant in a particular setting. Actions that limit people’s interactions (for example online rather than face to face; reducing the size of groups; travel restrictions) which can reduce, or if possible prevent, exposure to the virus are the most effective (high confidence). Where individuals and organisations can do this, they should prioritise these actions. Providing support to enable individuals to maintain quarantine or isolation is an important mechanism for promoting adherence to rules.
-
Where interactions between people are unavoidable, then engineering, procedural and personal controls are essential for reducing transmission. It is important that these measures are applied rigorously to ensure they are effective (high confidence). Organisations and individuals should reassess their environments in the light of new evidence about transmissibility of the new variant to consider whether they have maximised all the steps they can take to reduce the probability of transmission.
-
Transmission of the virus can occur in most settings[footnote ]. It is important that every effort is made to implement effective mitigation measures in all settings where people interact (high confidence). This includes the home environment.
Figure 1: Schematic showing potential routes of transmission for all SARS-CoV-2 variants, together with where personal, procedural and engineering mitigation measures can disrupt the transmission pathway.
8. There is good evidence from multiple studies that the number of interactions and the duration of exposure are risk factors for SARS-CoV-2 transmission (high confidence). Reducing the number and duration of any interactions between people is likely to mitigate all transmission routes (medium confidence). There is no evidence yet to quantify the relationship between risk of transmission and duration of exposure for the new variant, but given the possibility of increased transmissibility it may be that even more stringent reductions in duration of transmission are required (medium confidence).
- Face coverings and face masks control the source of the virus and provide important mitigation against all routes of transmission. They also provide a degree of protection against exposure, as shown on the right hand side of Figure 1. The effectiveness of face coverings improves with quality of design (multi-layer masks are better than single layer), a snugger fit on the face, and correct usage with both nose and mouth covered (high confidence). A better level of mitigation could be achieved through specifying higher performance face coverings and masks, and this should particularly be considered in settings where people are more vulnerable to the consequences of the disease and or are more likely to be infectious. It may be necessary to extend the use of face coverings to a wider number of settings (for example workplaces and education) where they are not currently mandated. This is important even when people are more than 2 metres apart, as correctly worn face coverings also reduce the emission rate of small aerosols.
A recent analysis suggests typical reductions in transmission for previous variants of the virus in real-world scenarios, which account for both physical filter performance and behaviour, are around 6 to 15% (B. Cowling and G. Leung, Eurosurveillance, 25(49), Dec 2020) but could be as high as 45% depending on the implementation strategy (Mitze T, et al. Proc Natl Acad Sci USA. 2020;202015954).
-
Close-range transmission by aerosols or droplets is primarily mitigated by physical distancing. Previous EMG papers have highlighted that the risk grows exponentially as distance reduces below 2 metres, and may be 2 to 10 times higher at less than 1 metre compared to 2 metre distancing, due to the higher concentration of virus in the immediate plume from an unmasked infected person[footnote ]. While there is no “magic distance”, beyond 1.5 to 2 metres larger droplets typically deposit on surfaces. Reconsider 2 metre as the default distance (rather than 1 metres +) to reduce the risk of close-range transmission, however there is little benefit to increasing distancing beyond 2 metres; at greater distances exposure to the virus in the air is predominantly determined by ventilation rates and airflow patterns rather than distance. The use of screens may potentially mitigate transmission through droplets and larger aerosols (Figure 1), but their impact on small aerosols is very limited (aerosols can go around a screen) and they are therefore not effective beyond 2 metres from the infected sources. Where it is essential for people to be less than 2 metres apart, it is important that mitigations consider both aerosol and droplet exposure, and it is strongly recommended that face coverings are mandated. One-way systems and floor markings may provide effective reminders to promote distancing, but are not themselves a mitigation.
-
Transmission via surfaces and fomites is primarily mitigated by good hand and respiratory hygiene and effective surface cleaningv, although face coverings may also reduce emission in the context of high viral loads and hence contamination of surfaces and hands. Frequent, focussed, cleaning of high hand-touch surfaces is likely to be more effective than cleaning surfaces where contact with hands is rare.
-
Transmission via the air is primarily mitigated by effective ventilation[footnote ]. This is most important in workplace and public settings where people interact, and is also important in the home, especially if there are visitors from outside the household, or someone within it has COVID-19. Where provision of adequate ventilation is difficult, the use of air cleaning devices may be a suitable alternative[footnote ]. Higher viral load associated with people who have the new variant could have significant implications for transmission via the air, as previous modelling suggests that viral load is a major determinant of airborne transmission risks. As a precautionary measure it is recommended that ventilation rates stated in previous EMG papers[footnote ] are adjusted accordingly to account for the increased risk (potentially 1.5 to 1.7 times higher). Application of ventilation controls is currently very variable between different settings, and it is essential to ensure that all public and workplace spaces include ventilation as part of their COVID secure risk assessment, and adopt appropriate measures to ensure it is effective (high confidence).
-
Virus survival may have some influence on transmission. Evidence for several viruses suggests that humidity may influence survival of the virus, with low relative humidity (experienced indoors in winter) leading to longer survival on surfaces and in air. Low relative humidity can also enable more evaporation of droplets, leading to a higher chance of aerosols that remain suspended for longer periods of time. Maintaining indoor relative humidity in the range 40 to 60% is recommended where possible. There is currently no evidence to suggest that persistence of the new variant in the environment is a factor in increased transmissibility, however research to understand survival of different variants should be undertaken.
-
The new variants that have emerged in the UK and South Africa are the first major cases of a mutated form of the SARS-CoV-2 virus that appear to present an increased level of risk, but they are unlikely to be the last. It is important to monitor changes to the nature of the virus over time and adapt mitigation measures, and the rigour with which they are applied, accordingly.
3. Part 2: Recommendations to Reduce Transmission of the new variant SARS-CoV-2 virus drawing on previous SPI-B recommendations on Improving Adherence to Mitigation Measures
Several SPI-B papers have made recommendations that are relevant to the need to improve adherence to all aspects of pandemic control in view of the increased transmission risk posed by the new variant. Some key relevant points are summarised below; evidence and further details are given in the original papers, which are referenced.
3.1 1. Communicating with and supporting all sectors of the population to improve their adherence to mitigation measures
- Provide positive feedback about a) the great efforts people are making to control the virus, b) the success of these efforts in helping to reduce infection rates and c) the need to now increase these efforts in order to sufficiently control the new variant[footnote ].
There is concern among some members of the public that their considerable efforts to help control the spread of the virus have had no success. It is important to recognise the sacrifices made and emphasise that the efforts the public have made have already had success in keeping infection rates much lower than they would have been while going back to work and other activities – but that because of the greater threat of infection posed by the new variant we need to build on and extend these efforts in order to save lives and reduce the need for lockdown.
Communications should avoid giving visibility to non-adherence (which undermines social norms for adherence[footnote ]) or suggest the ineffectiveness of preventive behaviours[footnote ]. Focusing on failure leads to reduced self-confidence and lower motivation to try, whereas positive feedback about coping efforts leads to further effort[footnote ], particularly if combined with feedback that further effort is needed to reach the desired goal[footnote ]. More positive messaging about the positive impact of the many ways in which members of the public are acting safely and the effectiveness of the measures they are taking when implemented fully should help to increase confidence in the value of these efforts and the ability of everyone to make them.
- When introducing any changes to guidance for infection control it is crucial to provide a credible rationale for new guidance and changes, and the new guidance should be precise and consistent[footnote ],[footnote ].
Resources should include clear and convincing explanations, detailed guidance and effective behaviour change techniques to motivate and support people to adhere to the guidance. The messaging should be transparent about uncertainty where present, in order to earn trust.
In the context of the new variant, messages should focus on encouraging and supporting the additional behaviours required to control a more infectious virus strain, particularly (as recommended by EMG):
- reducing indoor contacts to the lowest level possible;
- consistent use of high-quality face-coverings whenever indoor close contact mixing is unavoidable;
- approaches to enable effective ventilation of enclosed spaces[footnote ];
- high adherence to testing and self-isolation if symptomatic or a contact of a case.
Communications should also include the clear message that actions that pose only a low risk at an individual level may nevertheless lead to major increases in risk at population level when many individuals are doing them[footnote ].
- Help members of the public to identify situations where they find it difficult to avoid risky behaviour and work with them to create acceptable solutions
- Target more intensive information and practical support for adherence to the specific behaviours, settings and populations that need it
- Provide appropriate communications and support for people from communities with different cultural backgrounds
Once the specific knowledge gaps and barriers to target have been identified, rapid participatory co-design[footnote ] can be used to develop acceptable and feasible solutions, effective support for each solution, and persuasive new messages. Co-creation involves working with diverse members of all target user groups and multidisciplinary experts in supporting behaviour change to develop engaging and accessible resources suitable for different user audiences, including persons of all genders, age groups, racial, ethnic and social backgrounds and different levels of health risk. This process can be undertaken as rapidly as necessary. Information and guidance should be developed, disseminated and implemented in collaboration with opinion leaders from all target communities[footnote ].
Resources should identify and address concerns and barriers, suggest positive solutions, maintain social cohesion and support, and promote a shared sense of responsibility for infection control. Fear-inducing messages should be avoided as, even when health messages are adhered to, stressors remain in the physical environment that are not within the control of individuals; if a health message induces fear, it may result in denial or avoidance as a coping mechanism due to low control over external factors, such as working in frontline roles.
Detailed advice on how to communicate with young people is given in a previous SPI-B paper[footnote ]. Wellbeing in young people may impact their ability to adhere. Online, NHS and settings-based interventions to support young people’s mental health and wellbeing should be increased, as well as practical support and opportunities for education, training and employment.
Detailed advice on how to communicate with communities with different cultural backgrounds is given in a previous SPI-B paper[footnote ]. Translation of guidance into a range of suitable languages is necessary, but not sufficient. It is important to understand differences within and between minority groups, identify trusted, credible messengers and media channels to reach these groups and ensure health messages reflect salient aspects of ethnic identity and experiences.
3.2 2. Reducing transmission within households and during permitted household mixing
Families and groups must be made aware of the increased risk of infection when they are considering household mixing. Messaging in the context of Christmas and other celebrations should be accompanied by information about the risks of traditional behaviours, opportunities to create and engage in alternative forms of celebration and make environmental changes to enable safer household visits, and the effectiveness of decreasing infection risks by changing behaviour.
There is evidence that behaviours such as handwashing, surface cleaning and use of face coverings in the home can reduce (although not eliminate) transmission of infection, including of COVID-19. There is also evidence that currently most people do not implement these as thoroughly as they could, and that providing in-depth, personalised advice on how to implement infection control in the home can reduce infections in household members.
The risks posed by social interactions can be reduced through reducing the numbers of people involved; the sizes of their networks; minimising the numbers of overlapping networks (for example through reducing connections to different households); reducing the duration of events; and maximising mitigation measures affecting the physical environment and the types of activities that take place[footnote ].
3.3 3. Improving engagement with Test, Trace and Isolate
People must self-isolate immediately when experiencing any of the core symptoms of COVID-19[footnote ]. Polling data suggests that many people do not recognise all of the core symptoms of COVID-19. A belief that the symptoms of the new variant must be somehow unusual or severe may also prevent people from self-isolating promptly in response to mild symptoms. Government should pre-empt any confusion by:
- being clear that the core symptoms of COVID-19 remain the same, even for the new variant;
- spelling out explicitly that the symptoms to watch for are any (not all) of: new, continuous cough; high temperature; loss or change to sense of smell; loss or change to sense of taste;
- being explicit that people should treat even mild symptoms as COVID-19 until proven otherwise by a test, and that a large proportion of cases are asymptomatic.
Some groups are likely to have particular needs in relation to symptom recognition. This includes parents of young children, people with comorbidities, people from minority ethnic groups, people from lower socio-economic groups, and people who are receiving less information about the pandemic in general. Targeted messaging to such groups may be particularly beneficial.
Perceived and real practical barriers to accessing a test or self-isolating likely deter people from attempting to seek a test. Providing easy access to testing, and support for people who need to self-isolate, remains essential to maximising uptake of both[footnote ].
3.4 4. Maintaining adherence during vaccine deployment[footnote ]:
Indirect evidence from surveys conducted during the current pandemic as well as from previous vaccination campaigns suggest that, in the absence of any mitigation policies, some of those who have been vaccinated will show a reduction in personal protective behaviours (NPIs). These behaviours are those relating to hand and surface hygiene, use of tissues and face coverings, physical distancing and ventilating rooms.
Communication strategies should mitigate the risk of reducing adherence by communicating ongoing risk and the need to protect others. A culturally tailored communication strategy targeted and stratified by different sectors in society should be developed to ensure that people fully understand why it is vital to continue to adhere to protective behaviours, whether or not they have been vaccinated while the vaccination programme is being rolled out, until population-wide immunity is achieved.
4. References
-
NERVTAG meeting on SARS-CoV-2 variant under investigation VUI-202012/01, 18th Dec 2020 ↩
-
NERVTAG/SPI-M Extraordinary meeting on SARS-CoV-2 variant of concern 202012/01 (variant B.1.1.7), 21st Dec 2020 ↩
-
PHE: Factors contributing to risk of SARS-CoV2 transmission in various settings, 26 November 2020 ↩
-
EMG: Transmission of SARS-CoV-2 and Mitigating Measures, 4 June 2020 ↩
-
EMG: Role of ventilation in controlling SARS-CoV-2 transmission, 30 September 2020 ↩ ↩2
-
EMG: Potential application of air cleaning devices and personal decontamination to manage transmission of COVID-19, 4 November 2020 ↩
-
SPI-B Positive strategies for sustaining adherance to infection control behaviours, 22 October 2020 ↩
-
SPI-B Extended paper on behavioural evidence on the reopening of large events and venues, 21 August 2020 ↩
-
SPI-B Increasing adherance to COVID-19 preventative behaviours among young people, 22 October 2020 ↩
-
principles-for-the-design-of-behavioural-and-social-interventions-20-april-2020 ↩
-
SPI-B: Implementation and communications: harnessing behavioural science to maintain social distancing (April 2020) Available from the SPI-B Secretariat. ↩
-
EMG Simple summary of ventilation actions to mitigate the risk of COVID-19, 1 October 2020 ↩
-
SPI-B Key evidence and advice on celebrations and observances during COVID-19, 5 November 2020 ↩
-
SPI-B: Principles for the development of co-creation. Available from the SPI-B Secretariat. ↩
-
SPI-B Communicating behaviours to reduce transmissions between social networks summary, 27 May 2020 ↩
-
SPI-B Increasing adherence to COVID 19 preventative behaviours among young people 22 October 2020 ↩
-
EMG and SPI-B Mitigating risks of SARs-CoV-2 transmission associated with household social interactions, 26 November 2020 ↩
-
SPI-B: How important is symptom recognition in leading people to seek a test for COVID-19? Available from the SPI-B Secretariat. ↩
-
SPI-B Impact of financial and other targeted support on rates of self isolation or quarantine, 16 September 2020 ↩
-
SPI-B: Possible impact of the COVID-19 vaccination programme on adherence to rules and guidance about personal protective behaviours aimed at preventing spread of the virus, December 2020. Available from the SPI-B Secretariat. ↩
