Travel-associated infections in London: 2020, 2021 and 2022
Updated 14 August 2025
Applies to England, Northern Ireland and Wales
The data presented in this report is provisional and subject to change. The 2022 dataset covers the period from January up to 31 October.
Background
COVID-19 related travel restrictions resulted in a decrease in travel to and from the UK, and in travel-associated infections. As these restrictions are relaxed, it is expected that the number of cases of travel-associated infections will rise.
This report aims to inform public health actions that can be taken to reduce the incidence of the most common travel-associated infections. Data on the most common notifiable infectious diseases associated with travel outside of the UK by London residents are presented, with year-on-year comparisons from January 2020 to October 2022. Trends in reports of these infections throughout each year are presented, as well as the demographics of those affected and the countries to which they have travelled, with particular focus on 2022.
The data can be used to support local and regional public health messaging related to travel. Many of the infections identified in this report can be prevented either through vaccination or by taking appropriate precautions before or during travel.
Data sources and limitations
The data for this report was extracted from HPZone, the system used by health protection teams (HPTs) to record and manage reported infections. To be recorded on HPZone, cases must have been notified to the relevant HPT, either by a clinician or a testing laboratory. Only cases with infection confidence as confirmed or probable are included. Only cases with recent travel to a foreign country are included. Cases of COVID-19 and monkeypox are excluded.
The accuracy of the data in this report is dependent on the quality of data recording in HPZone. If a case had travelled recently but this was not recorded, then they will not be counted in the travel-associated infection case numbers.
In the figures below, case data has been broken down into 5 categories: common food-borne diseases; hepatitis A; enteric fever; malaria; and ‘other’ travel-associated infections
‘Common food-borne diseases’ includes only campylobacteriosis, shiga toxin-producing Escherichia coli, shigellosis and salmonellosis (excluding serotypes Typhi and Paratyphi). ‘Enteric fever’ covers infections caused by Salmonella serotypes Typhi and Paratyphi. The category ‘Others’ includes any other disease or infection recorded on HPZone associated with travel.
Travel-associated infections by year: 2020, 2021 and 2022
Travel-associated infections in London fell sharply in the first 3 months of 2020 (Figure 1). They then remained at relatively low levels for the duration of the year and throughout the early months of 2021. This likely relates to reduced travel due to COVID-19 restrictions at the time. Cases rose from August 2021, and from January 2022 there was a sustained increase in recorded travel-associated infections.
Figure 1 shows infections recorded by month between 2020 and 2022, including only confirmed and probable cases with recent travel to a foreign country. The table excludes cases of COVID-19 and monkeypox.
Figure 1. Total travel-associated infections recorded in London by month from 1 January 2020 to 31 October 2022
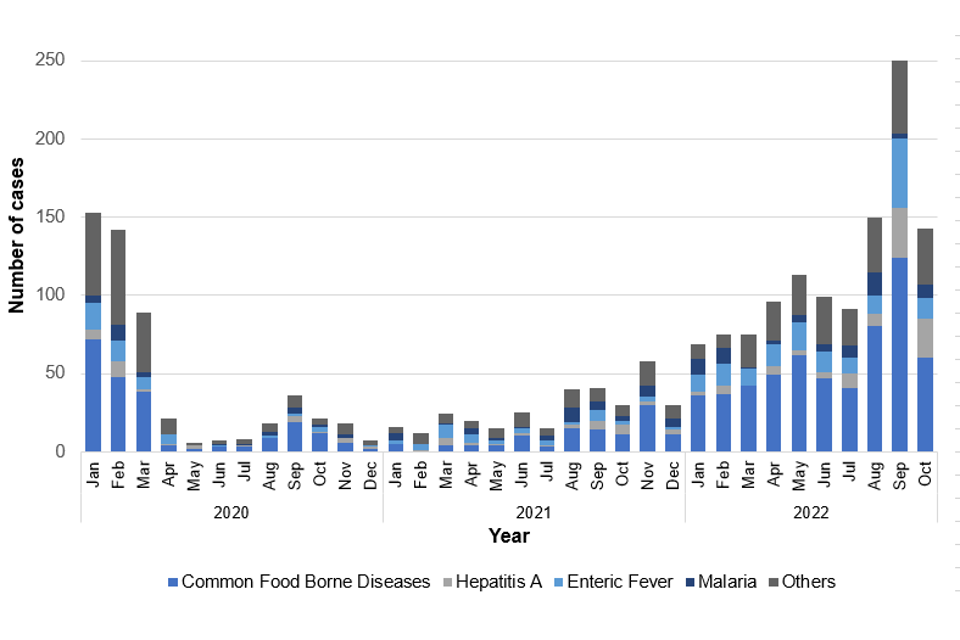
Throughout 2022 infections steadily increased until May, before initially declining in June and July. Cases then rose rapidly and peaked in September.
Over the period 1 January 2020 to 31 October 2022, the most marked rises in case numbers were as follows:
- common food borne disease cases rose by 165%, from 218 to 578 cases
- hepatitis A cases rose by 203% from 31 to 94 cases
- enteric fever cases rose by 214% from 51 to 160 cases
Travel-associated infections by type: 2022
As at 31 October 2022, the most common travel-associated infections have been GI illnesses and malaria.
Common food-borne diseases accounted for the greatest number of cases (50% of the current yearly total), followed by enteric fever (10% Salmonella serotype Typhi and 4% serotype Paratyphi), hepatitis A (8%) and malaria (6%).
Cases of common food-borne diseases initially peaked in May, followed by a larger peak in September. Enteric fever cases peaked in February, May and September. There was greater variation in case numbers for hepatitis A, with peaks in February, April and July, followed by the highest peak in September which was sustained into October.
Travel-associated infections by age: 2022
Figure 2 shows how the age of cases (that is, confirmed and probable cases with recent travel to a foreign country) varied depending on the infection.
Figure 2. Cases of each travel-associated infection recorded in London by age from 1 January to 31 October 2022

Children aged under 5 years accounted for more cases of common food-borne diseases than any other age group, with 14% of the total cases for the year. The next most common age group affected were those aged 26 to 30, with 13% of total cases.
The number of enteric fever cases rose steadily in the under-15s, with most cases seen in those aged 11 to 15 (15% of the yearly total). The next most common age group affected was 26 to 30 year-olds, with 12.5% of total cases.
Cases of hepatitis A infection were highest in those aged under 5 years (at 16% of the total). Cases were generally higher in those aged 30 or less, with 83% of the total hepatitis A cases seen in this age group.
The number of cases of malaria generally increased with age, peaking in the 51 to 55 years age group which made up 16% of the total cases.
Travel-associated infections by country of travel: 2022
Total case numbers for each infection category are shown in Table 1.
Table 1. Cases of travel-associated infection by country of travel from 1 January 2020 to 31 October 2022*
| Country of travel | Common food-borne diseases | Typhi | Paratyphi | Hepatitis A | Malaria |
|---|---|---|---|---|---|
| Pakistan | 47 | 38 | 28 | 25 | <10 |
| Turkey | 47 | <10 | <10 | <10 | <10 |
| Mexico | 32 | <10 | <10 | <10 | <10 |
| Spain | 31 | <10 | <10 | <10 | <10 |
| India | 29 | 43 | 13 | 13 | <10 |
| Portugal | 26 | <10 | <10 | <10 | <10 |
| Morocco | 20 | <10 | <10 | <10 | <10 |
| Egypt | 20 | <10 | <10 | <10 | <10 |
| Ghana | 17 | <10 | <10 | <10 | <10 |
| Thailand | 16 | <10 | <10 | <10 | <10 |
| Indonesia | 11 | <10 | <10 | <10 | <10 |
| Greece | 11 | <10 | <10 | <10 | <10 |
| Colombia | 10 | <10 | <10 | <10 | <10 |
| Somalia | 10 | <10 | <10 | <10 | <10 |
| Bangladesh | <10 | 14 | <10 | <10 | <10 |
| Sierra Leone | <10 | <10 | <10 | <10 | 23 |
| Nigeria | <10 | <10 | <10 | <10 | 21 |
*Includes only confirmed and probable cases. Not all countries with <10 infections are shown on this table. If there were no cases associated with a country, this is recorded as <10. Country case numbers have not been adjusted for the total number of visitors from the UK to each country.
Most enteric fever cases were associated with travel to India, Pakistan and Bangladesh; with 89% of Salmonella serotype Typhi cases and 94% of Salmonella serotype Paratyphi cases having visited at least one of these countries.
Of all travel associated hepatitis A cases, 43% were associated with travel to either Pakistan or India. A further 10% had recently visited Lebanon, the third biggest group. The remaining cases were associated with travel from a broad range of countries, with the majority of these outside of Europe (with only 10% having travel to a European country recorded).
Travel to continental Africa was identified in 93% of malaria cases, including 23 cases (37% of recorded cases) travelling to Sierra Leone and 21 cases (35% of recorded cases) having visited Nigeria.
Acknowledgements
This report was produced by Health Protection Operations London, UK Health Security Agency (UKHSA) London.
