Childhood obesity: applying All Our Health
Updated 7 April 2022
The Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
Introduction
This guide is part of ‘All Our Health’, a resource that helps health professionals prevent ill health and promote wellbeing as part of their everyday practice. The information below will help frontline health and care staff use their trusted relationships with patients, families and communities to promote the benefits of a healthier weight and reduce childhood obesity.
The guide also recommends important actions that managers and staff holding strategic roles can take.
View the full range of ‘All Our Health’ topics.
Access the childhood obesity e-learning session
An interactive e-learning version of this topic is now available to use. The Office for Health Inequalities and Disparities (OHID) and Health Education England’s ‘e-Learning for Healthcare’ have developed this content to increase the confidence and skills of health and care professionals, to embed prevention in their day-to-day practice.
Promoting a healthier weight in your professional practice
Childhood obesity and excess weight are significant health issues for children and their families. There can be serious implications for a child’s physical and mental health, which can continue into adulthood. The number of children with an unhealthy and potentially dangerous weight is a national public health concern.
Healthcare professionals play an important role in supporting families to take action. Working alongside other professionals and public health teams, they can also influence the general population by delivering whole systems approaches to tackle excess weight, and reduce drivers of excess calorie intake and sedentary lifestyles.
Action across the child life course is essential to impact childhood obesity and enable positive behaviour change around eating and activity. The focus should be on:
- preconception and pregnancy
- infancy and early childhood
- older childhood and adolescence
- transition into independent adulthood
Obesity harms young people and children infographic
Obesity is associated with poor psychological and emotional health, and many children experience bullying linked to their weight. Children living with obesity are more likely to become adults living with obesity and have a higher risk of morbidity, disability and premature mortality in adulthood.
Using National Child Measurement Programme (NCMP) data relating to primary school children, NHS Digital states that:
In the 2018 to 2019 school year, around three-quarters, or 76.5%, of children in reception (4 and 5 years old) were a healthy weight. In year 6, around two-thirds, or 64.3% of children (10 and 11 years old), were a healthy weight. Overweight and obesity prevalence (including severe obesity) was higher in year 6 (34.3%) compared to reception (22.6%).
Obesity rates are highest in the most deprived 10% of the population, more than twice that of the least deprived 10% as shown in the graph below from the 2018 to 2019 NCMP data.
2018 to 2019 National Child Measurement Programme data
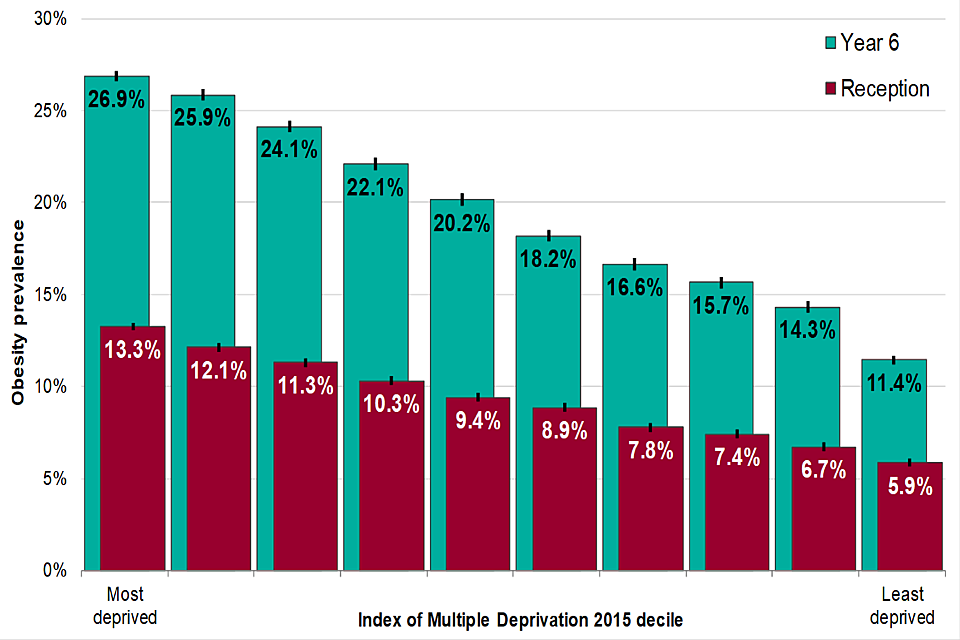
Obesity prevalence in Year 6 and Reception children
Obesity rates are higher in some ethnic minority groups of children (particularly among children from black and Bangladeshi ethnicities, though this varies by age and sex of the child).
Risk factors
The main risk factors for children, in terms of the households they are born into and grow up in, include:
- maternal health: in the 2017 Maternity Services Dataset, 49% of pregnant women attending their first appointment with a midwife were either living with overweight or obesity. Evidence shows a significant relationship between maternal obesity and the birth of babies above a normal weight range, and the subsequent development of childhood and adult obesity
- parental health: children who live in a family where at least one parent or carer is living with obesity are more at risk of growing up to be above a healthy weight themselves
In addition:
- children living with obesity are more likely to become adults living with obesity and thus increase the risk of obesity for their own children later in life
- poor diet and low levels of physical activity are the primary causal factors of excess weight
Children are currently consuming more than the recommended daily limit of sugar and this is a contributing factor to excess weight gain. The National Diet and Nutrition Survey found that sugary drinks account for 17% of 11 to 18 year olds’ daily sugar intake or 6% of 4 year olds daily sugar intake. High sugar intakes are also associated with an increased risk of dental caries. A recent report from the National Dental Public Health Team showed that children who are above a healthy weight were more likely to have dental caries in all deprivation categories.
Physical activity can help children and young people to achieve and maintain a healthier weight. The 2019 to 2020 Sport England Active Lives survey showed that only 45% of children and young people met the Chief Medical Officer’s Physical Activity Guidelines and participated in an average of 60 minutes or more of physical activity a day. Meanwhile, 31.3% did less than an average of 30 minutes a day. Boys are more likely than girls to meet the recommended levels, as can be seen in the graph below (data for children in years 1 and 2 is reported by their parents or carers).
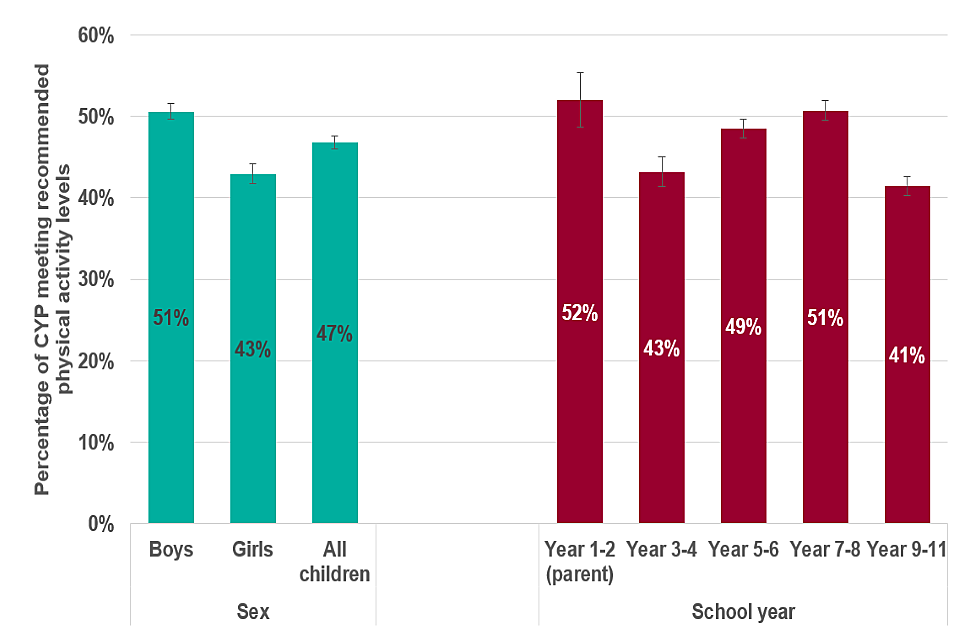
Percentage of children and young people aged 5 to 16 meeting physical activity recommendations, 2018 to 2019 [Source: Active Lives Children and Young People Survey, 2018 to 2019, Sport England]
HM Government Childhood Obesity: a Plan for Action
Building on the first chapter of the childhood obesity plan, the new measures included within chapter 2 of the childhood obesity plan focus on:
- improving the nutritional content of the food and drink our children consume
- strengthening the information available to parents about those products
- changing the way that unhealthy food and sugary drinks are promoted
Core principles for healthcare professionals
Healthcare professionals and the wider public health workforce should:
- know the needs of individuals, communities and population and the services available
- think about the resources available in health and wellbeing systems
- understand specific activities that can prevent, protect and promote
Taking action
If you’re a frontline health professional:
- remember that a healthy weight is primarily achieved through improving dietary intake, portion control and physical activity
- recognise that obesity is complex with many drivers including behaviour, environment, genetics and culture
- provide consistent evidence-based healthier weight, nutrition and physical activity messages for parents, children and young people – this includes explaining the principles of the Eatwell Guide and promoting the Chief Medical Officers’ Physical Activity Guidelines, as well as directing families to further information
- understand the specific activities and interventions that can support individuals and families to achieve and maintain a healthier weight
- use opportunistic moments to open up conversations around weight and, if appropriate, use a Royal College of Paediatrics and Child Health (RCPCH) UK growth chart or the healthy weight calculator to determine the body mass index (BMI) centile and weight status of the child or young person
- be mindful of weight bias, and use neutral, non-blaming, factual language when discussing weight with families
- encourage parents to sign up for the Start4Life information service for children from 0 to 5 years – the service provides evidence-based information for parents on pregnancy and child health development from 0 to 5 years, including important messages on breastfeeding initiation and continuation and improved nutrition
- ensure you are familiar with the local obesity care pathway and aware of the services and support available in the local system – from the NHS, local authorities and voluntary and community sectors
- promote breastfeeding uptake and duration, timing of introduction of solid food and responsive feeding practice
- think about how you as a professional are role modelling healthy behaviours – and how you can support your peers and colleagues to achieve and maintain a healthier weight
- promote and support healthy home environments to families
In addition, it is important to:
- encourage schools to register with the Change4Life School Zone, to receive new teacher packs designed to help teach curriculum-linked PSHE topics, with flexible lesson plans and engaging videos
- encourage schools to work proactively with the National Child Measurement Programme so that it is an integral element of the whole school approach to healthy weight – think about the role you can play in supporting children and young people who are identified as overweight or obese
- make use of the NCMP conversation framework for talking to parents
- offer evidence-based advice to increase activity throughout the school day such as the What works in schools and colleges publication, the school sport and activity action plan and the active mile briefings, as well as ideas for using the PE and Sport Premium
- support schools to adopt healthy eating policies
- support the development of school policies on bullying so that they include obesity and weight as possible causes – think about the role that school nurses and other professionals can play in supporting young people affected by bullying
- raise awareness among school and college staff to support positive emotional health and wellbeing
- signpost 11 to 16 year olds to Rise Above to help young people build resilience and reduce risk-taking behaviour – topics include body image, self-care, sugar and physical activity
- offer support to schools as they develop their curriculum to meet statutory requirements for the teaching of Relationships Education, Relationships and Sex Education, and Health Education from September 2020 onwards
If you’re a team leader or manager
In addition to the actions highlighted for frontline professionals, team leaders or managers can support this work by:
- standardising the approach across the service, for example, ensuring the 5 mandated health visitor reviews are offered for every family, or by ensuring all clinics have the Eatwell Guide and physical activity infographics displayed on the wall in the waiting room
- thinking about how the service can support sharing appropriate data between health, education, social care and community organisations to target prevention activity and coordinate intervention
- understanding that weight bias (PDF, 1.4MB) and stigma can negatively impact the experiences children, young people and families have with programmes and services, and consider this when communicating to teams and making decisions
- communicating up-to-date information on programmes and services including tier 2 weight management services in your local area to staff
- thinking about how you as a team leader or manager are role modelling healthy behaviours, and how you can support your peers and colleagues to achieve and maintain a healthier weight
- supporting evidence-based behaviour change training for staff through Make Every Contact Count
If you’re a commissioner or service provider:
- work with senior or strategic leaders to identify local levers and opportunities and to understand where programmes and services are working well, and where there are challenges accessing support for children living with overweight and obesity and their families
- use recommended evidence-based behaviour change techniques and involve children, young people and families when commissioning and designing services to help ensure they meet the needs of the local population
- prioritise healthy workplaces to reduce sickness absence, lower staff turnover and boost productivity – it is important not just for businesses and staff, but for the economy as a whole
- promote a ‘whole systems approach to obesity’ – this involves working closely with the many organisations, community services and networks in a local system to align and prioritise actions to address obesity and promote a healthier weight
If you’re a senior or strategic leader you can support these interventions by:
- building community capacity to enable local families to promote healthy eating and physical activity
- considering how high streets can be used as an asset to improve the overall health of local communities
- working with the community to facilitate active lifestyles, for example, through youth clubs, safe neighbourhoods, StreetPlay and outdoor play
- working with the local authority to use the planning system to achieve healthy weight environments
- working with the community and local authority to encourage the local provision of healthier food and drink options
- working closely with the local authority and other partners in the local system to take a ‘whole systems approach to obesity’
- supporting health professionals to have healthier weight conversations
Measuring impact
As a health professional, there are many reasons to measure your impact and demonstrate the value of your contribution. This could be about sharing what has worked well to benefit your colleagues and local people or to help you with your professional development.
The Everyday Interactions Measuring Impact Toolkit provides a quick, straightforward and easy way for healthcare professionals to record and measure their public health impact in a uniform and comparable way.
The childhood obesity impact pathway is recommended for healthcare professionals and the wider public health workforce to record and measure actions undertaken as part of routine care which impact on childhood obesity.
Understanding local needs
Child obesity data from the NCMP 2006 and 2007 to 2019 and 2020 is available in the online tool NCMP Local Authority Child Data Profile.
The NCMP tool:
- provides local authority level child data (underweight, healthy weight, obese, excess weight, overweight including obese) for reception (aged 4 to 5 years) and Year 6 (aged 10 to 11 years)
- presents trend data (including inequalities data) and enables easy comparison of local authority data, allowing users to compare regional neighbours and local authorities with similar characteristics
- your local authority public health team will also be able to access annual school feedback letters with information on the 3-year average of overweight or obesity prevalence level (except where class sizes are very small)
At a population level, the following outcome measures can help build a picture of the obesity-related risk factors in the population:
- Department of Health and Social Care, and Local Government Association’s guide for school readiness
- the Early Years High Impact Area 4 which sets out the main components on healthy weight and nutrition for professionals and commissioners
- breastfeeding initiation: percentage of mothers who have initiated breastfeeding within the first 48 hours
- breastfeeding prevalence at 6 to 8 weeks: percentage of all infants who are partially or totally breastfed at the 6- to 8-week check
- child health profiles: these provide a snapshot of child health and wellbeing for each local authority in England using the main health indicators, which enables comparison locally, regionally and nationally
The Obesity Intelligence Knowledge hub website provides wide-ranging authoritative information on data, evaluation and evidence related to weight status and its determinants.
You can also find out more by visiting data and analysis tools related to obesity.
Further reading, resources and good practice
Advice for patients and the public
NHS weight loss plan is a free 12-week diet and exercise plan for adults.
NHS.UK website offers tips for healthy eating.
The Eatwell Guide shows the proportions in which different types of foods are needed to have a well-balanced and healthy diet.
5-a-day gives advice and recommendations about the benefits of eating 5 portions of fruits and vegetables a day.
These physical activity guidelines infographics explain the physical activity needed for general health benefits for all age groups, disabled adults, pregnant women and women after childbirth.
Use the healthy weight calculator to check your BMI and find out if you are a healthy weight.
Start4Life offers help and advice during pregnancy, birth and parenthood.
Change4Life is an England and Wales campaign offering advice on making healthy choices and reducing sugar.
Better Health provides tools, support and encouragement across the breadth of lifestyle factors to help adults aged 40 to 60 years improve their health, every step of the way.
Professional resources and tools to promote healthier weight
These resources for promoting healthier weight are intended to support health and care professionals to be consistent and provide a core set of evidence-based healthier weight, nutrition and physical activity messages throughout the life course. They consist of a set of infographics for use in practice, a set of slides to be used as a training tool and a child obesity animation.
The Our Healthy Year resources help school nursing teams to explain NCMP and engage parents using classroom activities, practical tips and educational tools.
The Let’s Talk About Weight for adults and Let’s talk about weight resource for children and families support health and care professionals to have conversations about weight, and refer patients into weight management services.
The NCMP operational guidance advises local commissioners and providers on running the NCMP.
A series of 5 audio recordings is available to support school nurses, their teams and other professionals delivering the NCMP to have supportive and constructive conversations with parents about their child’s weight.
Guidance on healthier and more sustainable catering.
UK physical activity guidelines – advice from Chief Medical Officers on how much physical activity people should be doing.
Health Education England e-learning programme for practitioners in the NHS and local authorities working in weight management. Healthcare professionals and the wider workforce can strengthen their knowledge by accessing a range of e-learning modules for free. Some examples include:
- Health Promotion in Pregnancy: Obesity
- Obesity Prevention in Children
- Obese Toddlers and Infants
- Key Child Public Health and Mental Health Issues for 5 to 12 years – Understanding and Tackling Obesity
Promoting healthy weight in children, young people and families is a resource to support local authorities, NHS commissioners and providers, voluntary and community sector organisations to take action to reduce obesity.
Made up of briefings and practice examples to promote healthy weight for children, young people and families as part of a whole systems approach, it helps to:
- make the case for taking action to reduce obesity
- provide examples of actions that can be taken
- provide important documents that form the evidence base and other useful resources
World obesity image bank provides non-stigmatising images that could be used to represent childhood obesity.
