Health matters: physical activity - prevention and management of long-term conditions
Published 23 January 2020
Summary
This edition of Health Matters focuses on the benefit of physical activity for the prevention and management of long-term conditions in adults.
The government’s prevention green paper highlights that becoming more active is good for our mental and physical health, and reduces our risk of developing a number of health conditions. It also sets out the ambition of getting everybody active in the 2020s, including those of us who are already living with a health condition.
One in 3 adults in England live with a long-term health condition and they are twice as likely to be amongst the least physically active. However, evidence shows that regular physical activity can help prevent or manage many common conditions such as type 2 diabetes, cardiovascular disease and some cancers. It also helps keep symptoms under control, prevent additional conditions from developing, and reduce inequalities.
Health benefits of physical activity
In the new UK Chief Medical Officers’ (CMOs) physical activity guidelines launched in September 2019, the CMOs reiterated a clear message about physical activity:
“If physical activity were a drug, we would refer to it as a miracle cure, due to the great many illnesses it can prevent and help treat.”
Physical activity includes: active living, active travel, active recreation, active sport (informal sport and organised sport)
Regular physical activity provides a range of physical and mental health, and social benefits, many of which are increasing issues for individuals, communities and society. These include:
- reducing the risk of many long-term conditions
- helping manage existing conditions
- ensuring good musculoskeletal health
- developing and maintaining physical and mental function and independence
- supporting social inclusion
- helping maintain a healthy weight
- reducing inequalities for people with long-term conditions
Physical activity guidelines for adults
The updated UK CMOs’ physical activity guidelines refreshed the 2011 guidelines across all age groups. It also draws on new evidence to develop additional guidance on being active during pregnancy and after giving birth, and for disabled adults.
The guidelines state that for good physical and mental health, adults should aim to be physically active every day. Any activity is better than none, and more is better still.
Christopher Whitty - Chief Medical Officer full interview
There are 3 elements of the physical activity guidelines:
- strengthening activity
- cardiovascular activity
- sedentary time

UK Chief Medical Officers' physical activity guidelines: build strength and improve balance, be active, and minimise sedentary time
Strengthening activity
Muscle strength, bone health and the ability to balance underpin physical function. Each attribute contributes independently to overall health and functional ability, and in combination they provide lifelong benefits.
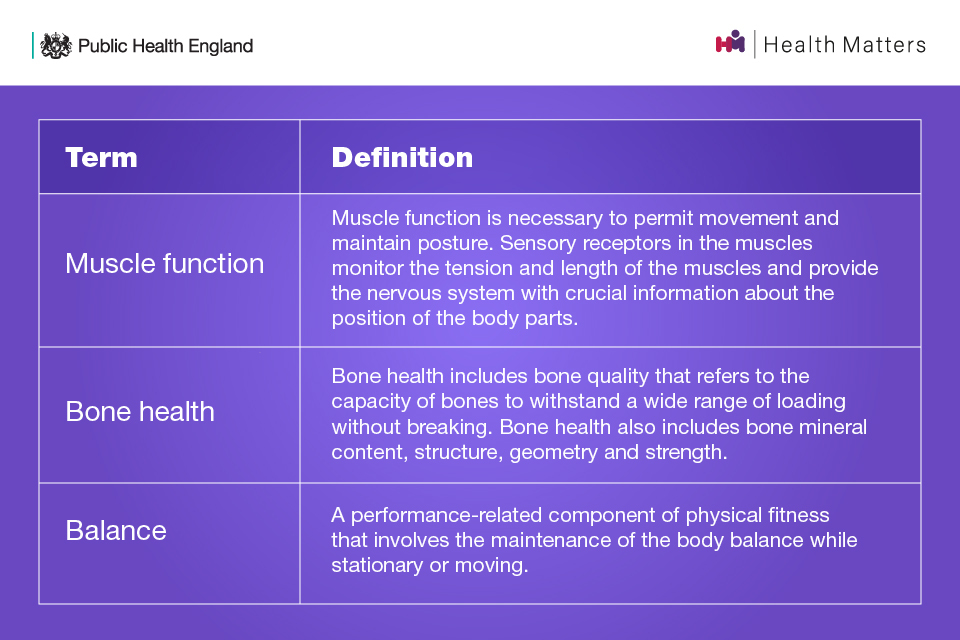
Definitions of muscle function, bone health and balance
There is a challenge faced in physical activity promotion with unequal emphasis on the aerobic, rather than the strength components, of the CMOs’ physical activity guidelines for adults.
Considered the ‘forgotten guidelines’, the CMOs’ strengthening activity guidelines state that: adults should do activities to develop or maintain strength in the major muscle groups. Muscle strengthening activities should be done at least 2 days a week, but any strengthening activity is better than none.

What counts as strengthening and balance activities: going to the gym, yoga, carrying heavy shopping, ball games, racquet sports, aerobic circuit training
The guidelines also highlight the additional benefit of balance and flexibility exercises for older adults. Exercises that improve leg strength, balance and coordination can help people maintain and improve muscle strength and avoid falls as they age. Improving flexibility can improve posture, reduce aches and pains, lower risk of injury, and help with continuing to carry out everyday tasks.
Evidence suggests that muscle strength, bone strength and balance ability increase in childhood and peak in early adulthood, eventually followed by a decline.
Therefore, muscle and bone strengthening and balance activities (MBSBA) are important across the lifecourse for different reasons:
- to develop strength and build healthy bones during childhood and young adulthood
- to maintain strength in adulthood
- to delay the natural decline in muscle mass and bone density that occurs from around 50 years of age, maintaining function in later life
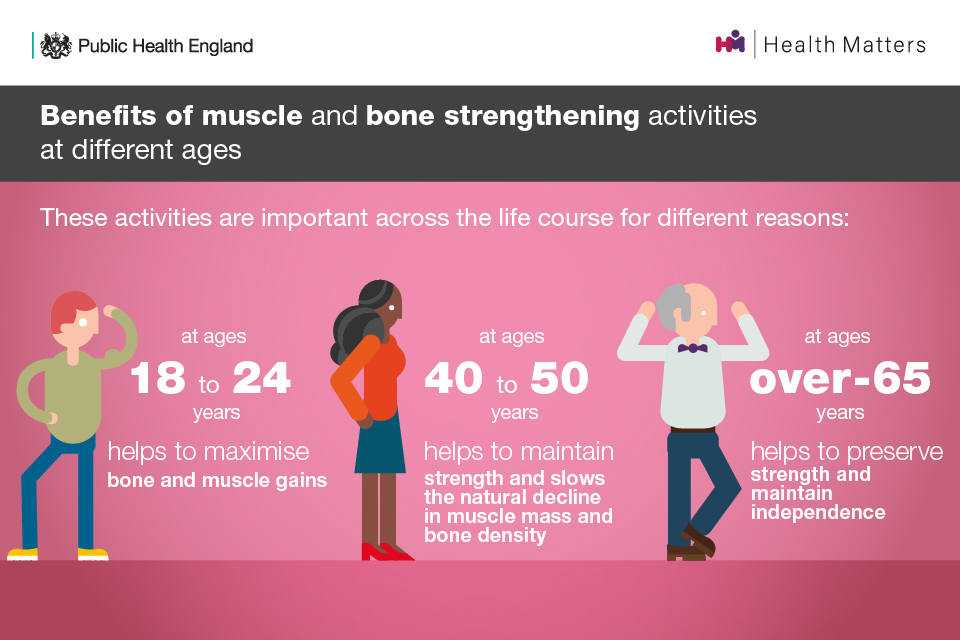
Benefits of muscle and bone strengthening activities at different ages
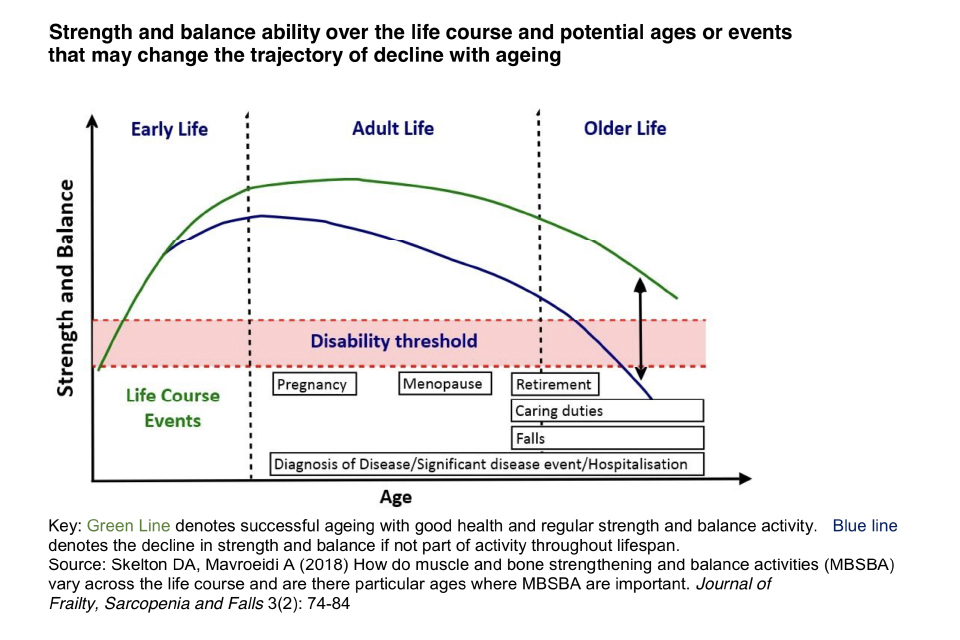
Strength and balance ability over the life course and potential ages or events that may change the trajectory of decline with ageing
Cardiovascular activity
For cardiovascular activity, the guidelines state that: each week, adults should accumulate:
- at least 150 minutes of moderate intensity activity (such as brisk walking or cycling), or
- 75 minutes of vigorous intensity activity (such as running), or
- even shorter durations of very vigorous intensity activity (such as sprinting or stair climbing), or
- a combination of moderate, vigorous and very vigorous intensity activity
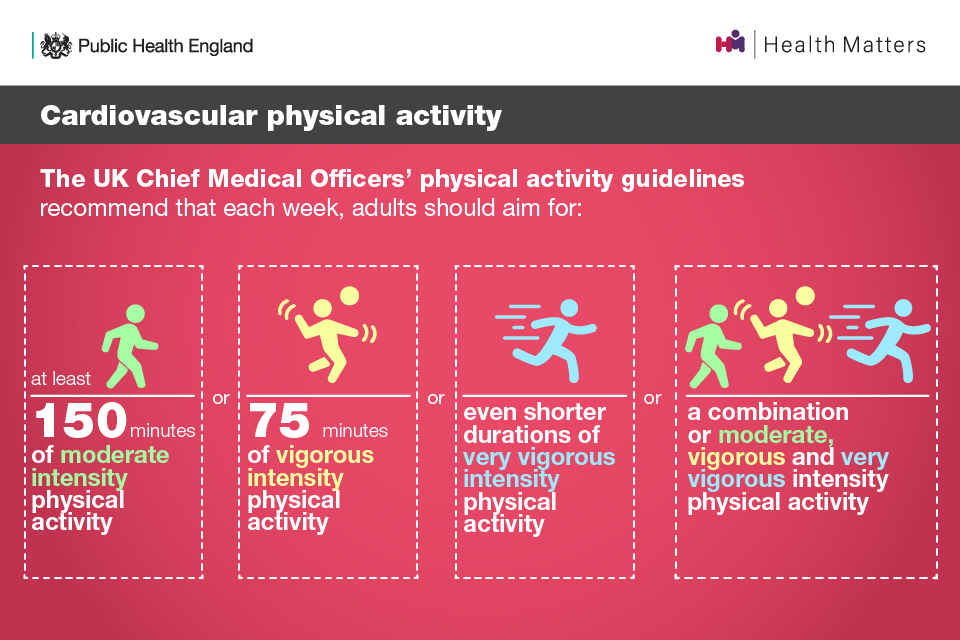
Cardiovascular physical activity: the UK CMOs' physical activity guidelines recommendations
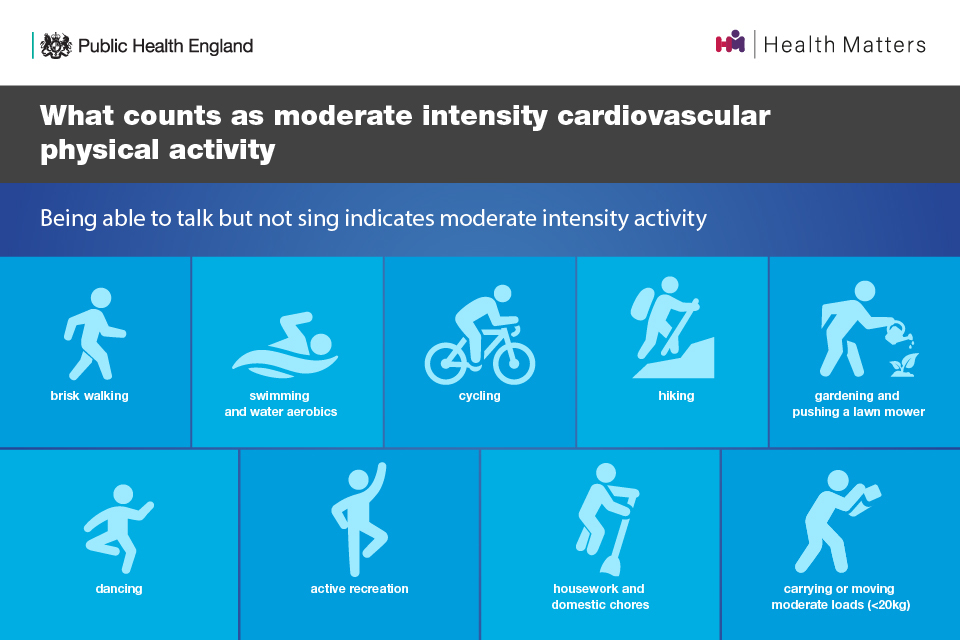
What counts as moderate intensity cardiovascular physical activity
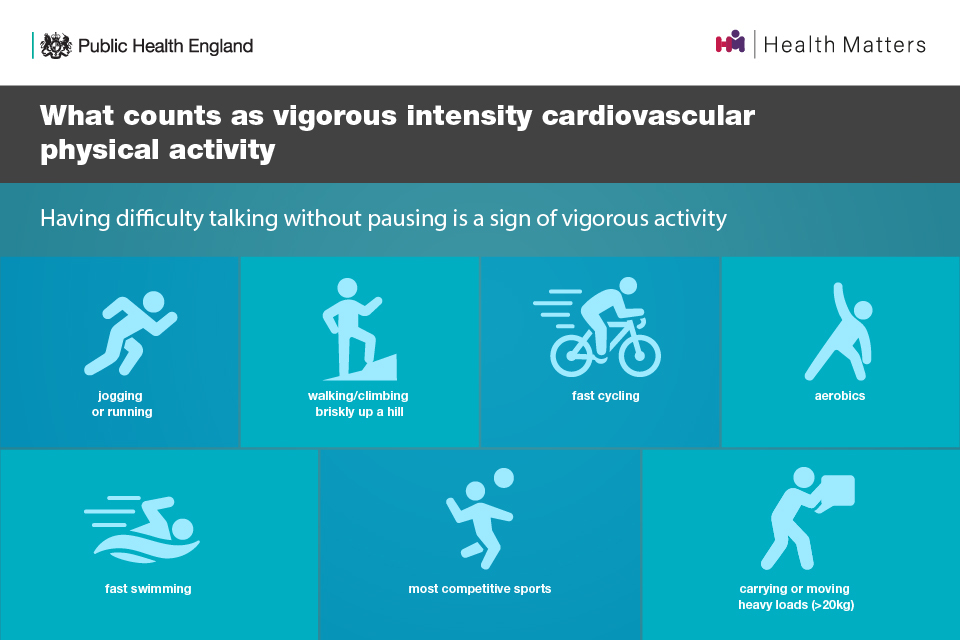
What counts as vigorous intensity cardiovascular physical activity: jogging or running, walking/climbing briskly up a hill, fast cycling, aerobics, fast swimming, most competitive sports, carrying or moving heavy loads
Sedentary time
For sedentary time, the guidelines state that: adults should aim to minimise the amount of time spent being sedentary, and when physically possible should break up long periods of inactivity with at least light physical activity.
There have been notable developments in the evidence base for the health effects of sedentary time in adults, with research suggesting sitting time is associated with increased all-cause and cardiovascular mortality, and cancer risk and post-treatment outcomes (including quality of life and prognosis).
Adults with long-term conditions
In England, 15 million people are living with one or more long-term health conditions. One in 3 of the working age population have at least one long term condition and 1 in 7 have more than one.
Since the 2011 physical activity guidelines were published, the evidence to support the health benefits of regular physical activity for all groups has become increasingly compelling.
The 2019 guidelines utilised the latest evidence from systematic reviews, meta-analyses, and pooled analyses comprising hundreds of epidemiological studies with several million study participants comparing active and low activity people. Figures for different health risks cannot be compared as they come from different studies.
Dr. Zoe Williams - NHS GP and PHE Physical Activity Clinical Champion Full Interview
Regular physical activity is associated with a reduced risk of a range of diseases including some cancers and dementia. There is also evidence that it can help to prevent some and manage many common chronic conditions and diseases, many of which are on the rise and affecting people at an earlier age, such as:
- some cancers
- obesity
- type 2 diabetes
- cardiovascular diseases (CVD) including coronary heart disease and stroke
- hypertension
- osteoarthritis and lower back pain
- mental health conditions including depression and anxiety
- dementia
- chronic obstructive pulmonary disease (COPD) and asthma
- musculoskeletal (MSK) conditions
Physical activity is as good or better than treatment with drugs for many conditions, such as type 2 diabetes and lower back pain, and has a much lower risk of any harm.
Physical activity can also benefit those who have MSK conditions. However, many people with MSK conditions often mistakenly believe that physical activity will make their conditions worse. The more conditions you have, the more you need to improve the core aspects of fitness:
- strength
- stamina
- balance
You can read more about this in this previous edition of Health Matters on productive healthy ageing and MSK conditions and healthy ageing consensus statement developed by PHE and the Centre for Better Ageing.
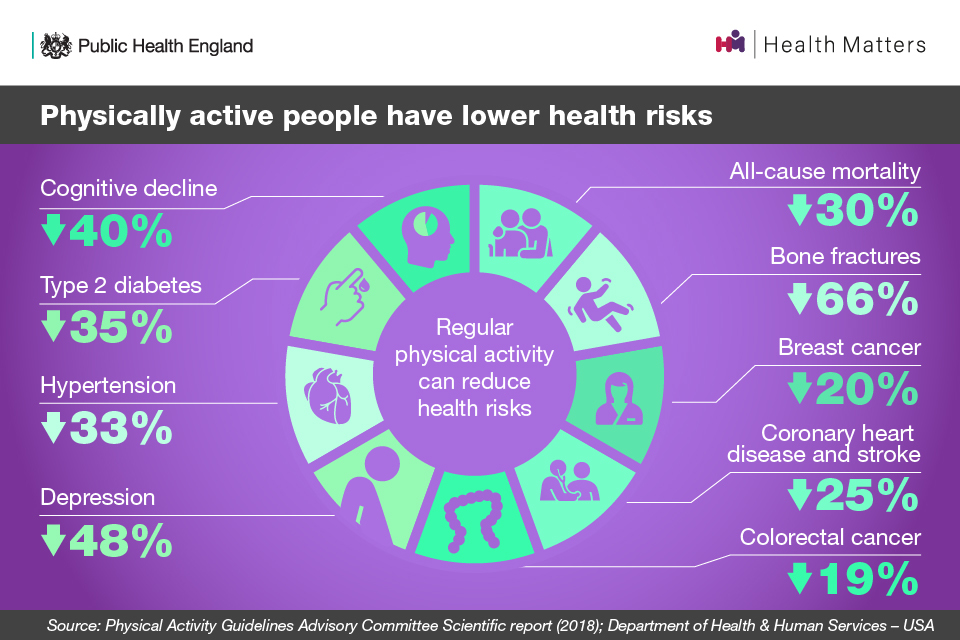
Physically active people have lower health risks
The role of physical activity for preventing and managing illness is included within many National Institute for Health and Care Excellence (NICE) guidelines, and the promotion of physical activity helps to support their implementation.
Adults with disabilities
PHE commissioned an evidence review for the UK CMOs’ guidelines, specifically focusing on the scientific evidence of the health benefits of physical activity for disabled adults. Evidence shows a relationship between engaging in physical activity and positive health outcomes for disabled adults.
It concluded that for substantial health gains, disabled adults should:
- do 150 minutes of physical activity at a moderate to vigorous intensity
- do 2 sets of challenging strength and balance exercises 2 times per week
- minimise sedentary time as per whole population guidelines
Little evidence was found to show that physical activity is unsafe for disabled adults when it is performed at an appropriate level for their current level of activity and health conditions.
Individuals with uncontrolled symptoms for cardiac, metabolic, renal and some musculoskeletal conditions should seek advice before greatly increasing physical activity.
Physical activity during pregnancy and postpartum
The benefits of physical activity during pregnancy include:
- reduction in hypertensive disorders
- improved cardiorespiratory fitness
- lower gestational weight gain
- reduction in risk of gestational diabetes
The benefits of physical activity in the postpartum period (up to one year) include:
- reduction in depression
- improved emotional wellbeing
- improved physical conditioning
- reduction in postpartum weight gain and a faster return to pre-pregnancy weight
Physical activity can safely be recommended to women during and after pregnancy and has not been found to have any negative impacts on breastfeeding postpartum.
Wider role and benefits of physical activity
In addition to supporting good physical and mental health and functioning, regular physical activity also contributes to a range of wider social, environmental and economic benefits for individuals, communities and wider society. Addressing physical activity can also benefit a broad range of wider priorities at a local level, such as reducing air pollution and increasing social cohesion.
Wider benefits come primarily from physical activities undertaken in a community setting such as walking, cycling, active recreation, sport and play. They include:
- improved learning and attainment
- increasing productivity in the workplace
- managing stress
- self-efficacy
- improved sleep
- the development of social skills
- better social interaction
The relevance and importance of these benefits vary according to life stage and other factors.

The wider physical wellbeing, mental wellbeing and individual development benefits of physical activity
Social prescribing enables individuals presenting through primary health care to be signposted and connected to local organisations, groups and activities. There are social prescribing schemes that focus on physical activity and staff with knowledge of the resources available in the local community match individuals to opportunities and support them to engage in activities. In some social prescribing schemes, health trainers and health champions signpost and support clients to become involved in community activities.
Social and community development
Sport England’s Sport Outcomes Evidence Review sets out how sport and physical activity can contribute to the government’s Sporting Future strategy outcomes. One of the outcomes is social and community development, which is described as being about “helping to build stronger communities by bringing people together, often from different backgrounds, to make them feel better about where they live, improve community links and cohesion, and build social capital.”
The evidence review found that sport and physical activity can lead to social and community development through:
- building stronger communities by bringing people from different backgrounds together via participating, volunteering and spectating
- improving community links, levels of cohesion and social capital
- improving residents’ sense of belonging in an area
- feeling more connected to your neighbourhood or community
- increasing levels of social trust
It is of increasing importance to take a whole systems approach to addressing public health challenges, including physical inactivity and obesity. Local government plays an important leadership role in bringing together statutory, voluntary and private sectors and engaging their populations to build confident and connected communities as part of efforts to improve health and reduce health inequalities.
Community-centred approaches seek to mobilise the assets within communities, increase people’s control over their health and promote equity. There is a diverse range of practice, evidence-based approaches that can be used by local leaders, commissioners and service providers to work with communities.
PHE has developed a guide that outlines evidence-based community-centred approaches to health and wellbeing and this previous edition of Health Matters details a whole systems approach to obesity and PHE’s professional guide to support local approaches to promoting a healthy weight.
Wider economic benefits
In terms of wider economic benefits, physical activity can lead to cost savings for the health and social care system. This is because in some cases, long term conditions can lead to greater dependency on home, residential and ultimately nursing care. However, physical activity supports greater independence and reduced requirement of support, including these statutory services, therefore leading to financial cost savings.
The benefits of active travel
PHE conducted an evidence review – intended for health and social care policy makers, decision makers and commissioners – which looks at the impact of walking and/or cycling on different health outcomes. The review found that walking and cycling benefit health in a number of ways, including:
- improving metabolic health and reducing the risk of premature mortality
- reducing risk factors for various long term conditions, including cardiovascular disease, respiratory disease, some cancers and type 2 diabetes
- providing mental health and neurological benefits, including reduced risk of dementia, improved sleep quality, and a greater sense of wellbeing
Active travel also reduces road congestion and air pollution, which provides both environmental benefits and greater health benefits for the general population.
PHE has an active travel briefing for local authorities – including transport planners and public health practitioners – which sets out a range of actions from overall policy to practical implementation.
The scale of physical inactivity
In England:
- 1 in 3 (34%) men are not active enough for good health
- almost 1 in 2 (42%) women are not active enough for good health
- 1 in 5 (21%) men are classed as physically inactive
- 1 in 4 (25%) women are classed as physically inactive
- 44% of disabled adults are physically inactive
- only 34% of men and 24% of women undertake muscle-strengthening activities at least twice a week
‘Not active enough for good health’ means not achieving the CMOs’ guideline of 150 minutes of moderate intensity physical activity per week.
‘Physically inactive’ is defined as doing less than 30 minutes of moderate intensity physical activity per week.
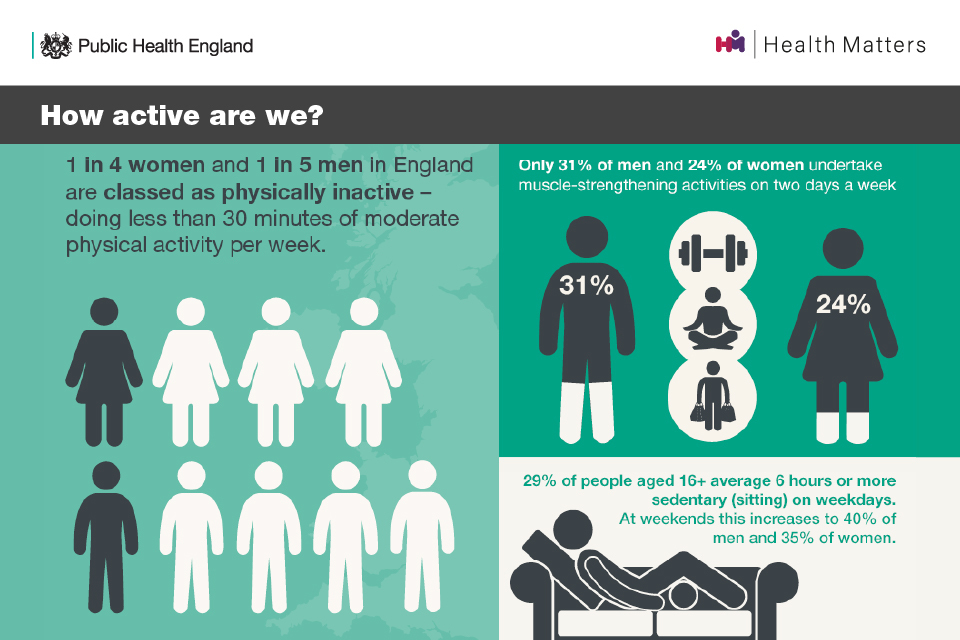
How active are we?
Insufficient physical activity is associated with:
- 1 in 6 deaths in the UK
- up to 40% of many long-term conditions, including preventable conditions such as type 2 diabetes, cardiovascular disease and some cancers
- around 30% of later life functional limitation and falls
This is not a new issue. Over the last few decades, trends such as increased car ownership and use, reduced manual element of jobs, and increased home-based entertainment has designed physical activity out of people’s lives. This has made us the first generation that needs to make a proactive choice to be physically active.
According to the World Health Organisation (WHO), physical inactivity is in the top 5 non-communicable disease (NCD) risk factors for mortality in high income countries. The WHO Global Non-Communicable Disease Action Plan 2013 to 2020 sets targets for improvements in the prevalence of NCD risk factors, including physical inactivity. The Richmond Group of Charities commissioned the BHF Centre on Population Approaches for Non-Communicable Disease Prevention to run a research project, which translates these WHO targets into a UK health context.
This was conducted in a 2-stage process: a modelling project to estimate the NCD burden in England between 2010 and 2025 if the WHO 25 by 25 targets are met, and a policy review of the potential prevention-based population-level interventions that are available, including those for reducing physical inactivity.
Read the UK PROMISE study to find out more about the potential of these interventions.
Physical activity and health inequalities
There are inequalities in physical activity across socioeconomic status and the protected characteristics, including:
- age
- gender
- disability
- race
- sexual orientation and gender identity
These compound or exacerbate other inequalities and lead to physical inactivity being more prevalent in certain groups.
Data on local inequalities in physical activity are available from the PHE physical activity data tool.
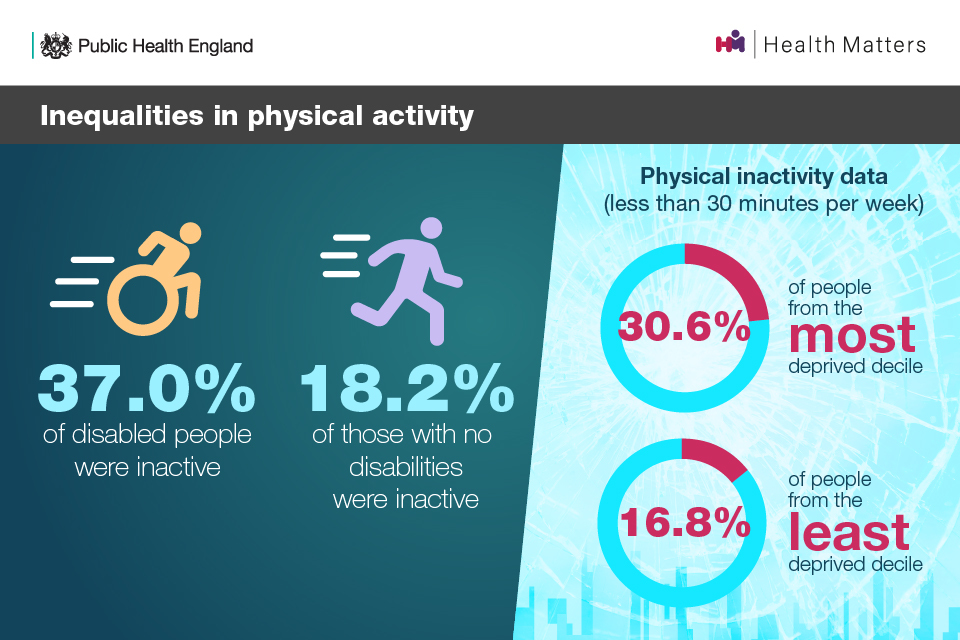
Inequalities in physical activity
Inactive people from economically disadvantaged backgrounds are also more likely to undertake unhealthy behaviours such as smoking, alcohol consumption, and have a poor diet.
A rapid review of the evidence base on physical activity for general health benefits for disabled adults found that no evidence exists that suggests appropriate physical activity is a risk. It also found analogous health benefits for disabled people of engaging in physical activity as for the rest of the adult population.
The UK CMOs’ guidelines say that for both adults with and without disabilities, the risk of adverse events from physical activity is relatively low and the health benefits accrued outweigh the risks.
For people with mental health conditions, inequalities in physical activity is associated with inequalities in physical health. Amongst people with severe mental disorders, there is a high prevalence of low physical activity and 12 hours on average is spent on sedentary activities everyday. This can, in part, lead to crucial physical health disparities and premature mortality, reducing their life span by 10 to 20 years.
The World Health Organisation (WHO) has guidelines that provide evidence-based recommendations to practitioners on how to recognise and manage physical health conditions in adults with severe mental disorders.
Everybody active, every day
Everybody active, every day is the national physical activity framework co-produced with over 1,000 local and national stakeholders, for national and local action to address the physical inactivity epidemic. It is based on international evidence of ‘what works’ to increase population activity.
The framework sets out that if we want everyone to be active every day, physical activity needs to be made easy, fun and affordable. Physcial activity and active recreation must be available to all, in every community across England.
Creating this vision requires actions across 4 domains at both a national and local level:
- Active society: creating a social movement
- Moving professionals: activating networks of expertise
- Active environments: creating the right spaces
- Moving at scale: interventions that make us active
These 4 domains of action are supported by the WHO Global Action Plan on Physical Activity 2018 to 2030.
Everybody active, every day: 2 years on reviewed the progress of these 4 domains of action 2 years on from the framework’s implementation. This ICF report published in 2018 also review the implementation of the framework at a national and local level. A ‘5 years on’ review will be published in early 2020.
The barriers to physical activity for those with long-term conditions
Insight work has found that 61% of people with long-term conditions and 68% of people with multimorbidities are not content with their physical activity levels and wish to be more active.
The Richmond Group of Charities’ Sport and Physical Activity project identified a need for insight into physical activity and long-term conditions. It commissioned research with individuals with long-term conditions and people close to these individuals, to understand the barriers that prevent those with long-term conditions from engaging in physical activity, as well as other factors.
The research found that people with long-term conditions experience both internal and external barriers to exercise. Internal barriers come from within those with long-term conditions themselves, and external barriers are factors external to those with long-term conditions, which make it harder for them to exercise. The latter are often practical or logistical.
Internal barriers are perceived to be greater than external barriers and include:
- pain before, during or after physical activity
- feeling tired before, during or after physical activity
- breathlessness before, during or after physical activity
- lack of motivation
- not knowing what types of activity are right for them or their condition
- fear of hurting themselves
- feeling embarrassed
- feeling unsafe in public spaces
Within this, there is agreement that barriers arising from the symptoms of long-term conditions are greatest, such as pain, feeling tired and breathlessness.
Both exercise and physical activity are seen as “not for people like me” amongst inactive participants with multiple long-term conditions. However, the research found that the majority of people with a long-term health condition want to be active.
Almost all qualitative participants from this research found it much easier to cite barriers to physical activity than benefits. The benefits cited most commonly were psychological, including increased self-esteem and confidence, and improved mood and motivation. Social benefits are also important for many, such as getting out of the house and seeing people, which was seen to support the psychological benefits.
Physical activity resources, programmes and campaigns for the public
OneYou resources: Active 10 and Couch to 5K
PHE and the NHS’ OneYou resource exists to help the public make small changes that fit their life, so that they feel better and healthier everyday. As part of OneYou, Active 10 and Couch to 5K are resources that support the important physical activity message that ‘some is good, more is better’ and that you can start small and build your activity up. A rapid evidence review found that a reduced level of health benefits can be achieved through activity at less than the optimum 150 minutes, with some benefits shown even at levels of 10 minutes or more of at least moderate intensity activity per day.
Active 10 is a free walking tracker app that can be used to monitor brisk walking, set daily goals, and find out how to increase physical activity. It has been downloaded over 800,000 times and since its launch it has remained popular with a rating of 4.3 and 3.3 out of 5 on the iOS and Google Play App stores, respectively.
Brisk walking is a moderate intensity physical activity and evidence-based intervention for promoting physical activity. For currently inactive individuals, evidence shows the following health benefits could be achieved from 10 minutes of brisk walking per day for 7 days:
- increased physical fitness
- greater ease of performance of everyday physical activities
- improved mood
- improved quality of life
- increased body leanness and healthier weight
- 15% reduction in risk of early death
The Couch to 5K app guides people through a 9-week programme by encouraging them to run 3 times a week. The app was designed to support people who have never run before, regardless of age.
It helps people to increase the distance they run incrementally, so that by the time they arrive at week 9 they are encouraged to run for half an hour, which is approximately 5K. Over 3 million people have downloaded the app, and its rating on the app store continues to stay high at 4.5 out of 5.
NHS Health Check
The NHS Health Check is a health check-up for adults aged 40 to 74 in England, which plays an important role in the prevention and early detection of CVD. According to the WHO, CVD is the leading cause of death globally, but an estimated 50% to 80% are preventable as they are caused by modifiable risk factors. One of these risk factors is low physical activity (less than 150 minutes of moderate intensity physical activity).
Everyone having an NHS Health Check should receive tailored lifestyle advice and access to local services, including physical activity services and the NHS Diabetes Prevention Programme (NHS DPP).
Find out more about the role of the NHS Health Check in promoting physical activity in this previous edition of Health Matters.
NHS Diabetes Prevention Programme
Type 2 diabetes is a major cause of premature mortality, with around 22,000 people with diabetes dying early each year in England. Being overweight and obesity, driven by the obesogenic environment and physical inactivity, are significant risk factors in the development of type 2 diabetes.
The NHS DPP is a joint commitment from PHE, NHS England and Diabetes UK. The programme provides evidence-based behavioural interventions at scale for individuals identified – for some through the NHS Health Check – as being at high risk of developing type 2 diabetes.
One of the 3 core goals that underpins the NHS DPP behavioural intervention is achievement of the CMOs’ physical activity recommendations. This may be through recommending the use of apps such as Active 10 and Couch to 5K to start adding small amounts of physical activity into your life.
Find out more about the role of the NHS DPP in increasing physical activity to reduce the risk of type 2 diabetes in this previous edition of Health Matters.
We Are Undefeatable campaign
The We Are Undefeatable campaign – led by a collaboration of 15 leading health and social care charities and supported by PHE and Sport England – is designed to inspire and motivate people living with long-term conditions to get active in a way that’s right for them.
It is designed with the perspective and lived experience of people with health conditions, and provides an opportunity to stimulate positive discussion and action, and identify and address barriers to engaging this audience.
The main audience for the campaign is:
- people who are doing little physical activity and those who are doing almost none at all
- male and female, 30 to 64 years old and beyond
- broad range of health conditions
The campaign drives sustainable attitude and behaviour changes, therefore addressing some of the factors that people with long-term conditions identify as barriers to physical activity.
Physical activity initiatives and training for healthcare professionals
More than 1 in 10 people visit their GP every 2 weeks and there are 1.2 million health-related visits to a community pharmacy every year. In most cases, those who are regularly engaging with healthcare professionals have, or are at risk of, developing health conditions and are more likely to be inactive. In addition, 1 in 4 people would be more active if advised by a healthcare professional, so healthcare professionals play a unique role in supporting people to be more physically active.
However, a 2017 survey of 1,000 GPs found that:
- 80% of GPs in England are unfamiliar with the national physical activity guidelines
- less than half (44%) are confident in raising physical activity with patients
- over half (55%) had done no specific training on physical activity
A 2017 survey of 552 physiotherapists found that:
- the activity status of patients is not routinely assessed
- 60% knew the 150 minutes recommendation, but only 16% knew all 3 elements of the guidelines
- they did not routinely signpost to further sources of physical activity support

Support healthcare professionals to discuss physical activity with patients
This is, in part, due to a system issue around providing adequate training for healthcare professionals on the guidelines and physical activity for people newly diagnosed with a long-term condition or in treatment.
Healthcare professionals may also feel that they cannot speak to patients about physical activity when they are seeing them about certain symptoms they are experiencing due to their long-term condition, such as fatigue and pain. They may also face time difficulties with regards to fitting a conversation about physical activity into a 10-minute appointment.
Moving Healthcare Professionals Programme
The Moving Healthcare Professionals Programme (MHPP) is a national partnership programme led by Sport England and PHE. It is a whole-system educational approach to embed prevention and physical activity promotion into clinical practice, helping to address the barrier of healthcare professionals not speaking to their patients about the benefits of physical activity due to either lack of knowledge, skills or confidence.
The programme provides peer-led training and is developing practical resources to support healthcare professionals implement the NICE guidance on physical activity, and guidance for treatment of a breadth of conditions that recommend physical activity.
There are multiple strands to the programme:
- training existing healthcare professionals
- development of resources, such as Moving Medicine (outlined below)
- upskilling the next generation
- testing innovative ideas
Further information on each of these strands can be found on Sport England’s website.
Upskilling NHS workforces through the MHPP provides the opportunity to:
- address a recognised knowledge and skills gap across healthcare professionals and their capability to implement physical activity guidelines
- provide the workforce with access to evidence-based training and resources proven to increase their knowledge and confidence, and support their practice
- improve management of patients with over 30 long-term conditions that physical activity is known to improve
- help reduce service demand and costs to the NHS
Recognised by the WHO as good practice, a second, 3-year programme was launched in the government’s prevention green paper. It will continue to provide free, evidence-based training and resources to healthcare professionals across their careers.
Read this edition’s case study on the Oxford University Hospitals NHS Trust’s Active Hospitals pilot, which aimed to explore integrating physical activity interventions in a secondary care setting.
Moving Medicine
Moving Medicine is an initiative led by the Faculty of Sport and Exercise Medicine UK, in partnership with PHE and Sport England. It is a digital toolkit for clinicians and allied health professionals that is part of the Moving Healthcare Professionals programme, and has been developed in collaboration with experts, professional bodies and charities representing patients and healthcare professionals in each disease area.
The toolkit provides accessible, evidence-based and condition-specific information to help give advice on physical activity at all stages of a patient’s treatment pathway for 10 common conditions:
- cancer
- COPD
- dementia
- depression
- falls and frailty
- inflammatory rheumatic disease
- ischaemic heart disease
- MSK pain
- primary prevention
- type 2 diabetes
The toolkit provides what is needed for a 1 minute, 5 minute and longer conversation, complete with step-by-step guides, behavioural change insights, and all the evidence to back it up. This helps to alleviate the barrier of time constraints that healthcare professionals face when speaking to their patients, allowing them to incorporate physical activity into their conversation.
Through the work of the Moving Healthcare Professionals programme and others, we are seeing changes in the awareness and knowledge of healthcare professionals. We are seeing them becoming empowered to embed physical activity into the care of disabled people and people with long-term health conditions, to improve their health and quality of life.
Physical Activity Clinical Champions training
PHE and Sport England’s Physical Activity Clinical Champions training involves a national network of 50 healthcare professionals providing a free, peer-to-peer, standardised training package to over 22,000 other healthcare professionals. Clinical champions are paid on a sessional basis to provide the training, which PHE has peer-reviewed, sponsored and updated to match the new CMO guidelines.
An independent evaluation has showed that this training:
- increased knowledge – 1 in 4 (25%) of those who did not know the guidelines recalled them correctly at 4 and 12 weeks
- increased confidence – those ‘extremely confident’ increased from 16% to 30% at 4 weeks
- increased regularity of discussions – 40% had more physical activity conversations with patients
E-learning courses
There are several other digital resources that PHE, in collaboration with partners, has developed to support healthcare professionals in championing the benefits of physical activity with their patients.
PHE, Health Education England and Sport England have developed a physical activity and health e-learning course, which is hosted on the e-Learning for Healthcare hub. The course will familiarise the learner with:
- the UK CMOs’ physical activity guidelines
- the underpinning evidence base
- how to incorporate the guidelines into their daily clinical care
PHE’s All Our Health e-learning session on physical activity gives health and care professionals an overview of the topic and provides evidence, data and resources to help professionals in embedding physical activity into daily life. This supports system-wide priorities on prevention, including those within the NHS Long Term Plan and prevention green paper.
Royal College of General Practitioners 3-year priority
PHE is working with the Royal College of General Practitioners (RCGP) on their 3-year priority on physical activity. This includes their Physical Activity and Lifestyle Toolkit and Active Practice Charter, both developed in partnership with Sport England. The toolkit can be downloaded to help healthcare professionals embed physical activity within the conversations they’re having with patients. The charter inspires and celebrates GP practices that are taking steps to increase activity in their patients and staff, and aims to support around 8,000 GP practices in the UK.
More resources and condition-specific resources for healthcare professionals can be found on the RCGP website.
The RCGP and parkrun UK also launched the parkrun practice initiative in June 2018, which asks GPs to affiliate themselves with their local parkrun and become parkrun practices. Involvement in this initiative will help practices:
- improve the health and wellbeing of practice staff
- improve the health and wellbeing of patients and carers, particularly those who are inactive or living with long-term conditions, reducing the need for lifelong medication
- raise awareness amongst the parkrun community of services that practices provide
- contribute to the development of a local community and environment that is centred around wellness generation
- support the UK-wide movement to scale up social prescribing activities
More than 16% of GP practices in the UK have registered to become a parkrun practice to date.
Read this edition’s case study on the parkrun practice initiative to find out more.
Call to action
The role for healthcare professionals
As discussed above, healthcare professionals play a unique role in supporting people living with, or at risk of developing, long-term health conditions to get more physically active.
With this in mind, healthcare professionals should:
- increase their knowledge of individuals’, communities’ and populations’ needs related to physical activity
- use the resources and the services available in the health and wellbeing system to promote physical activity, including those outlined in the section above
- incorporate physical activity conversations and brief advice into routine care
- understand specific activities or interventions that can prevent physical inactivity and signpost to their local offers
- help create a culture and process of physical activity within their workplaces, for example using the Active Practice Charter
They can have an impact on the individual level by:
- providing high-quality brief interventions for physical activity behaviour changes
- being familiar with the important messages
- being familiar with local physical activity options
- becoming a physical activity role model
Caroline Abrahams - Charity Director at Age UK Full Interview
Healthcare professionals also play an important role in using the NHS Health Check as an opportunity to assess physical activity levels using the general practice physical activity questionnaire (GPPAQ). They can subsequently provide brief advice or behaviour change support.
Social prescribing is another important area that GPs and other healthcare professionals should focus on, referring people to ‘activities’ or services in their community instead of offering only medical solutions.
The NHS Long Term Plan sets out that through social prescribing, the range of support available to people will widen, diversify and become accessible across the country. Over 1,000 social prescribing link workers will be in place by 2020 to 2021, so that over 900,000 people can benefit from social prescribing by 2023 to 2024. This is reiterated in the prevention green paper.
The role for local authorities
Local authorities are the main investors in physical activity in local areas, and should adopt a whole systems approach to ensure that physical activity is embedded across their relevant functions.
A local whole systems approach enables local stakeholders, including communities, to come together, share an understanding of the reality of the challenge, consider how the local system is operating and where there are the greatest opportunities for change. Stakeholders agree actions and decide as a network how to work together in an integrated way to bring about sustainable, long term systems change.
However, leading on taking a whole systems approach to physical activity is just one part of local authorities’ role, as they also have a wider role to play in:
- understanding local physical activity levels and inequalities
- providing and leading action to create physical activity opportunities
- linking the whole systems approach to other local authority agendas
You can find out more about the local whole systems approach to obesity programme in this previous edition of Health Matters.
Building on this work, PHE is working with Sport England to support their Local Delivery Pilots.
Local authorities should work with multiple organisations and groups, for example:
- local enterprise partnerships to invest in cycling and walking infrastructure to support local businesses with active travel and active retail
- leisure, fitness and sport providers to maximise the potential of local physical activity assets
- community groups to activate and maximise the potential of parks and green spaces
PHE has produced a briefing for local authorities on working together to promote active travel.
Use PHE’s Public health and outcomes framework and Physical Activity Fingertip tool to identify the percentage of physically active and inactive adults in your local area.
The role for NHS organisations
NHS organisations have an important role to play in the management and prevention of long-term conditions in adults through physical activity. Their role involves:
- identifying a senior lead for physical activity in line with NICE guidance
- sharing and encouraging training leads to include Clinical Champions training sessions within the staff training sessions
- promoting the use of the e-learning and Moving Medicine resources
- creating a culture that promotes physical activity, including supporting national and local campaigns such as One You, We Are Undefeatable and parkrun practices
- creating links with local physical activity providers (for example, local Active Partnership, Walking for Health)
The Physical activity: encouraging activity in the community and Physical activity: for NHS staff, patients and carers quality standards should be followed.
