Health matters: preventing cardiovascular disease
Published 14 February 2019
Summary
Too many people are still living with undetected and poorly managed atrial fibrillation (AF), high blood pressure (BP) and raised cholesterol. Working with partners, Public Health England (PHE) and NHS England have agreed ambitions which seek to address the A, B and C of secondary prevention and reduce the health inequalities associated with cardiovascular disease (CVD) over the next 10 years .
Scale of the problem
CVD is the leading cause of death worldwide, accounting for 17.9 million deaths each year, 31% of all global deaths.
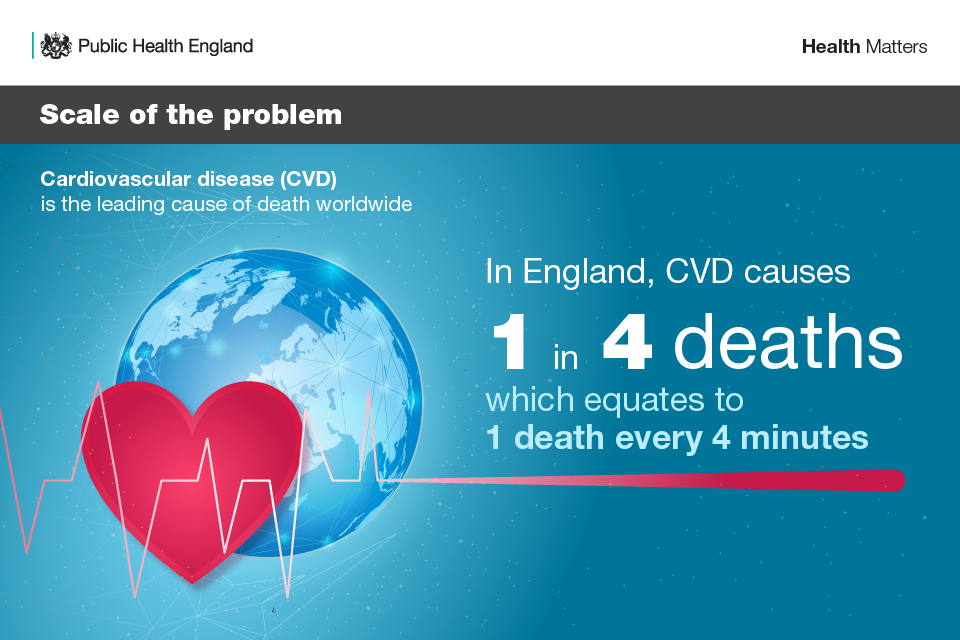
Infographic showwing scale of the problem with cardiovascular disease in England
Poor cardiovascular health can cause heart attacks, strokes, heart failure, chronic kidney disease, peripheral arterial disease and the onset of vascular dementia. Furthermore it disproportionately affects people from the poorest communities.
Falling mortality rates from heart disease were the biggest cause of increases in life expectancy between 2001 and 2016 in England, according to the Health Profile for England.
However, since 2011 the rate of increase in life expectancy has slowed for both sexes as improvements in heart disease mortality have plateaued. This highlights the need for a renewed drive to prevent CVD deaths, which still account for 1 in 4 of all deaths in England - the equivalent to 1 death every 4 minutes. In 2016, heart disease was the leading cause of death for men and the second biggest cause of death for women after dementia.
Although CVD mortality rates have almost halved over recent decades, there is no room for complacency in the efforts required to address the major challenges that CVD continues to play in individual lives, communities and society as a whole.
In 2016, 33,812 people under the age of 75 died from CVD, making this 1 of the largest causes of premature mortality. Morbidity is also a major issue for health and social care, with 6.8 million people living with cardiovascular conditions.
Yearly healthcare costs in England relating to CVD are estimated at £7.4 billion, with an annual cost to the wider economy of £15.8 billion. There is also significant variation in the incidence of CVD. For example, in 2016 to 2017 the premature (under 75 years) death rate for Manchester (140.7 per 100,000) was nearly 4 times higher than that for Mid Suffolk in the East of England (37.0 per 100,000).
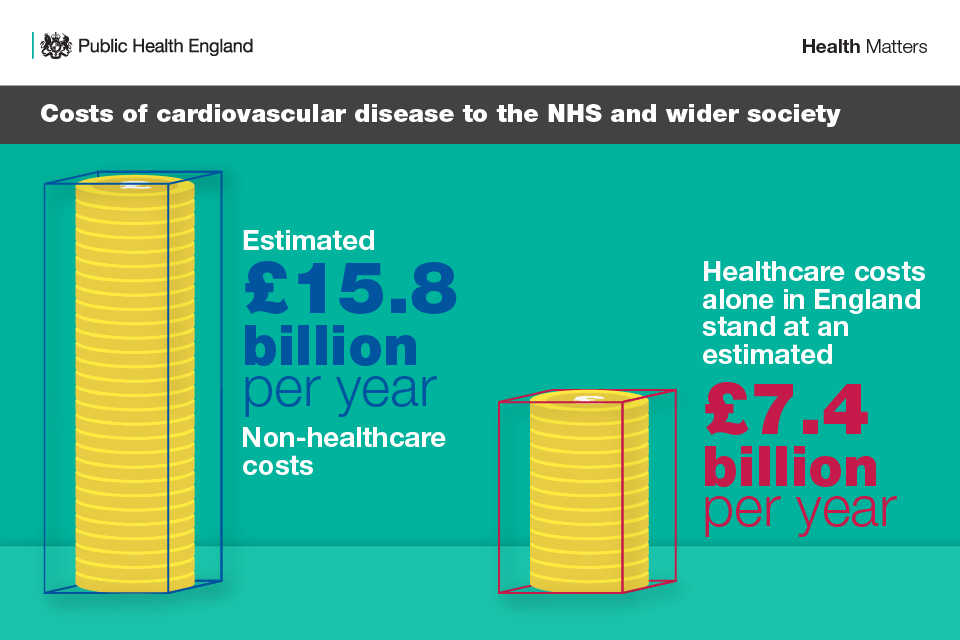
Infographic showing costs of cardiovascular disease to the NHS and wider society
There is a huge opportunity to make a difference in improving CVD outcomes, given that the majority of CVD cases are preventable. Risk factors, such as obesity, physical inactivity, smoking and drinking at unsafe levels, can all be modified to help reduce a person’s risk of developing CVD.
Primary prevention projects form a significant part of NHS England’s and PHE’s ongoing work to tackle CVD. Prevention strategies have already been introduced to help wider determinants of behaviour, such as the government setting salt, sugar and calorie reduction targets.
However, to date, there has been an absence of coordinated action to tackle the secondary prevention of CVD.
CVD ambitions and secondary prevention
The NHS Long Term Plan (NHSLTP) includes a major ambition to prevent 150,000 strokes, heart attacks and dementia cases over the next 10 years. Improving the detection and treatment of the high-risk conditions of AF, hypertension (high BP) and high cholesterol has the potential to unlock considerable health gains.
These common conditions can cause CVD, which includes heart attacks and strokes, and many cases of dementia. Although treatment of these conditions is very effective at preventing cardiovascular events, late diagnosis and under treatment is common.
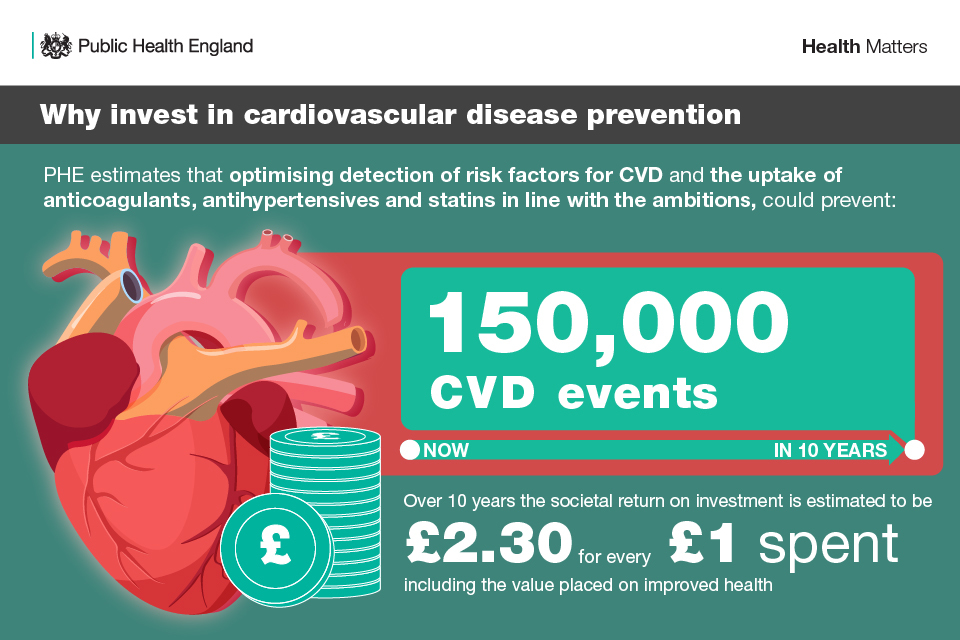
Infographic showing why we should invest in cardiovascular disease prevention
To complement the NHSLTP, the National CVD Prevention System Leadership Forum (CVDSLF) has agreed specific ambitions for the detection and management of the high risk conditions, known as ‘the ABC’:
- atrial fibrillation
- blood pressure
- cholesterol
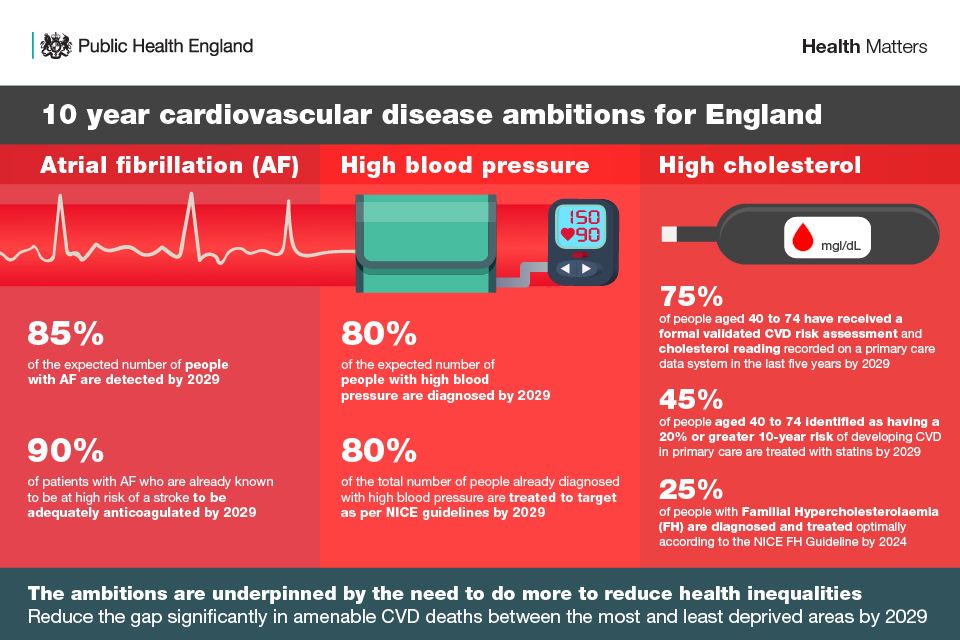
Infographic showing the overall cardiovascular disease ambitions for England
We know that Canada took just over 10 years to reach its CVD ambitions, but is now the world leader for detection and optimal management of high BP. The CVDSLF believes England has the potential to do the same if we all work together to achieve these ambitions.
Return on investment
The NHSLTP sets out a goal of saving 150,000 heart attacks, strokes and dementia cases over 10 years.
Independent PHE estimates show that if the ambitions were achieved within 3 years, at least 49,000 strokes and 32,000 heart attacks could be prevented. Other events averted include heart failure, transient ischaemic attacks, vascular dementia and angina.
The reduction in these events is predicted to achieve 81,000 life years gained and will avoid 9,000 premature mortality cases. These estimates are based on PHE’s CVD Return on Investment Tool. The tool predicted the effects of reaching targets over 3 years, the maximum allowed by the tool. As achieving the Long Term Plan ambitions is expected to take 10 years, these results will be overestimates.
PHE’s independent modelling shows these policies are good value for money. Over 10 years the societal return on investment is estimated to be £2.30 for every £1 spent, including the value placed on improved health.
Though considered separately for the purpose of the ambitions, these conditions are not mutually exclusive and the greatest impact in improving CVD outcomes can be achieved by targeting all 3.
Health inequalities
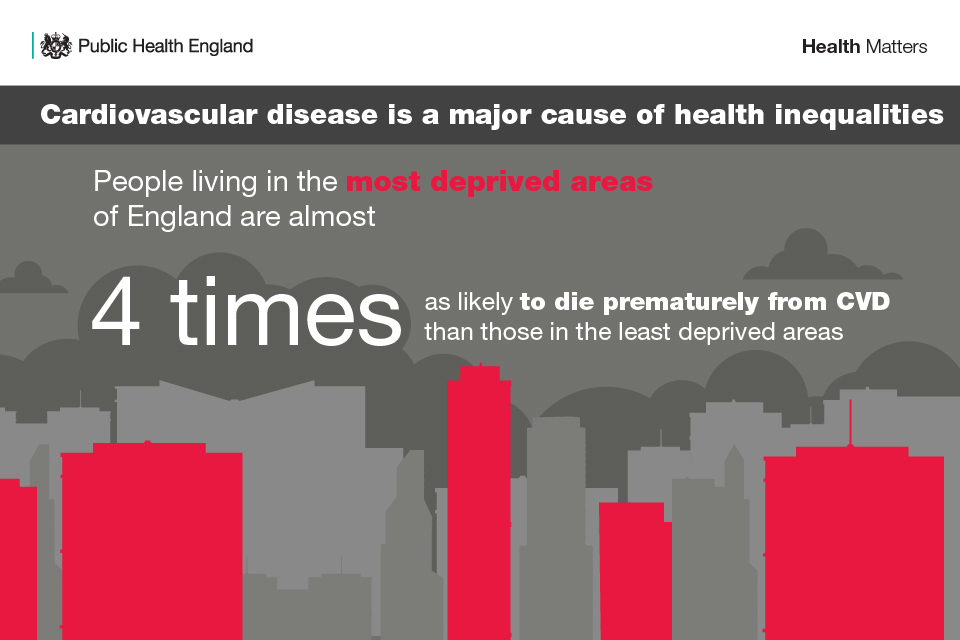
Fundamental to achieving these ambitions is the need to achieve reductions in the gap in avoidable CVD mortality and morbidity between the most and least deprived.
CVD is 1 of the conditions most strongly associated with health inequalities. If you live in England’s most deprived areas, you are almost 4 times more likely to die prematurely than someone in the least deprived. Furthermore, CVD is more common where a person is male, older, has a severe mental illness or ethnicity is South Asian or African Caribbean.
Infographic showing that cardiovascular disease is a major cause of health inequalities
Those in the most deprived communities are 30% more likely to have high BP, the biggest single known risk factor for heart attack and stroke.
PHE analysis shows that 40% of amenable CVD deaths occur in the 3 most deprived deciles. To prevent the gap from widening further, over 40% of action on all ambitions should be delivered to the 3 most deprived deciles in England.
As there is an absence of data to enable England to monitor progress on tackling health inequality within each ambition, the CVDSLF is committed to:
- obtaining and publishing health inequality data on each of the high risk conditions by deprivation decile by 2021
- setting quantitative ambitions for reducing CVD health inequalities in diagnostic and treatment goals by 2021
Atrial fibrillation
Infographic showing the ambition for the detection and management of atrial fibrillation
The ambition
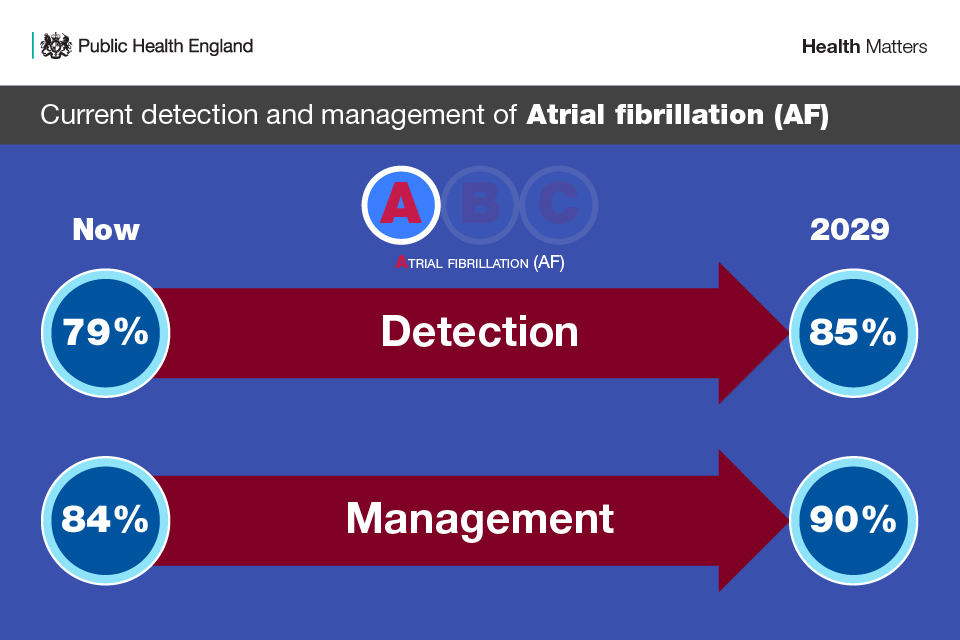
The AF ambitions of the CVDSLF are:
- 85% of the expected number of people with AF are detected by 2029
- 90% of people with AF who are known to be at high risk of a stroke to be adequately anticoagulated by 2029
Why atrial fibrillation?
AF is characterised by a rapid, irregular heartbeat and is the most common heart rhythm irregularity. The irregular beating commonly causes the formation of blood clots, which increases the risk of stroke by 5 times. There are, on average, 40 AF-related strokes every day in England.
The causes of AF are not fully understood but its prevalence increases with age. It is also more prevalent in men than in women. Certain ethnicities and existing CVD conditions are also likely to increase the chance of someone developing AF.
There is huge geographic variation in prevalence across the country depending on the demographic profile. At a GP level, this can mean prevalence ranges anywhere from 0.009% to 27.5%.
Anticoagulation is an effective therapy for managing people with AF who are at risk of stroke, and can reduce the risk of stroke by up to 66%. However, many people with AF are not on anticoagulants, meaning they are getting no treatment at all or are on ineffective treatment, such as aspirin, for AF.
Just over 1 in 4 people (26%) with an AF stroke who were not anticoagulated in 2017 to 2018, died. Others are on a suboptimal dosage of the anticoagulant warfarin, meaning that they remain at significant risk of stroke.
The challenge
It is estimated that 1.4 million people in England have AF, which equates to 2.45% of the population.
Recorded AF prevalence in 2017 to 2018 was 1,113,553, which is just 79% of the expected number of people estimated to have AF.
The Menu of Preventative Interventions published by PHE in 2016, communicated an ambition to increase optimal management of people with AF from 74% to 89% over 5 years (by 2021).
Progress has already been made (as 84% was achieved in 2017 to 2018), and it has therefore been agreed that the ambition for optimally managing AF should be 90%. There is clinical consensus that a treatment ambition of 90% is appropriate and achievable.
Read case study: Pharmacist-led virtual clinics to optimise anticoagulation in AF
High blood pressure
Infographic showing the ambition for the detection and management of high blood pressure
The ambition
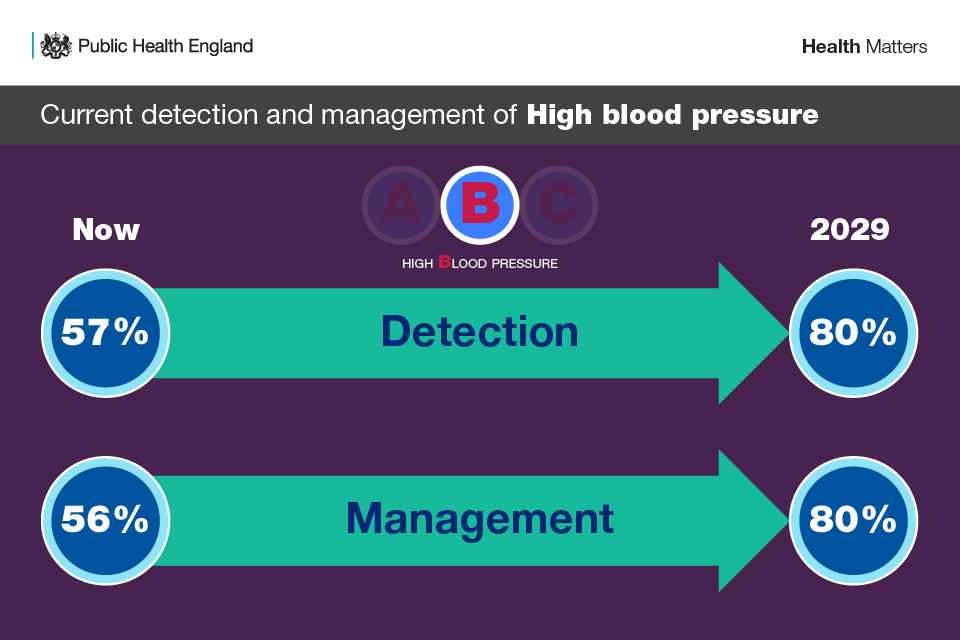
The high BP ambitions of the CVDSLF are:
- 80% of the expected number of people with high BP are diagnosed by 2029
- 80% of the total number of people diagnosed with high BP are treated to target as per NICE guidelines by 2029
Why blood pressure?
High BP is the second largest known global risk factor for disease and disability (after poor diet). It accounts for approximately half of all strokes and ischemic heart disease events globally.
In England, high BP is the number 1 risk factor for CVD mortality and morbidity. It affects more than 1 in 4 adults and was responsible for around 64,000 deaths in 2015. The Global Burden of Disease (GBD) shows that, in England, high BP causes over 1 million disability-adjusted life years and 179,857 years of life lost.
High BP also places a considerable burden on the NHS, where it is responsible for 12% of all visits to GPs with an estimated annual cost to the NHS of over £2 billion. There are over 5 million more people expected to have undetected high BP.
There are also significant inequalities attached to high BP, where prevalence is 30% more likely in the most deprived areas of England compared to the least deprived.
The challenge
Currently in England, only 57% of the estimated number of adults (16+) with hypertension have been detected, and only 56% of people under 80 who have been diagnosed with high BP have achieved the NICE recommended target clinic BP of 140/90 mmHg.
Internationally, the Canadian high BP programme is leading the way on high BP outcomes aspiring to meet an ambition of achieving control in 78% of people with high BP. In their work so far, they have successfully increased detection with 68.1% of people with high BP treated to target in 2012 to 2013.
As Canada has a similar expected prevalence of high BP as England, if we take action now, we can achieve similar ambitions over the next 10 years.
Read case studies: High blood pressure quality improvement in Cheshire & Merseyside and Virtual clinics to improve BP in poorly controlled patients
Raised cholesterol
Infographic showing the ambition for the detection and management of high cholesterol and familial hypercholesterolaemia
The ambition
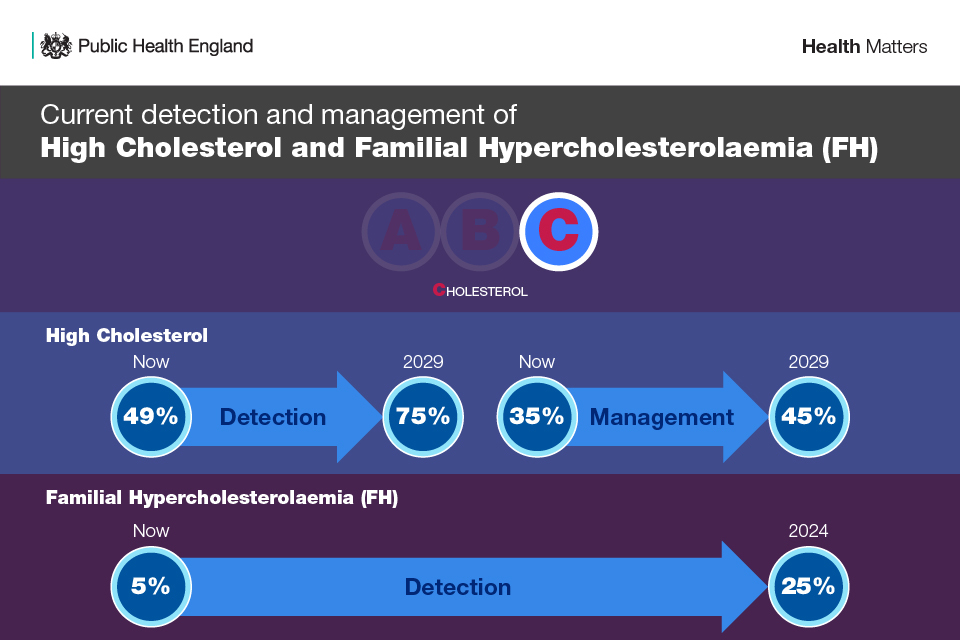
The cholesterol ambitions of the CVDSLF are:
- 75% of eligible people aged 40 to 74 without established CVD, such as a previous heart attack or stroke, have received a formal validated CVD risk assessment and cholesterol reading recorded on a primary care data system in the last 5 years by 2029
- 45% of people aged 40 to 74 without established CVD, such as a previous heart attack or stroke, identified as having a 20% or greater 10-year risk of developing CVD in primary care are treated with statins by 2029
- 25% of people with Familial Hypercholesterolaemia (FH) are diagnosed and treated optimally according to the NICE FH Guideline by 2024
Why cholesterol?
High cholesterol is 1 of the most significant risk factors for CVD. Globally, a third of ischaemic heart disease is attributable to high cholesterol. It is estimated to account for 7.1% of deaths and 3.7% of disability-adjusted life years (DALYS) in England.
High cholesterol is characterised by the build-up of fatty deposits in arteries, so tends to increase as we age.
Raised cholesterol can also be caused by genetic conditions, where cholesterol is elevated from birth, such as Familial Hypercholesterolaemia (FH). FH affects approximately between 1 in 250 to 1 in 500 people in the UK, which is about 130,000 to 260,000 people, including children. If untreated, about 50% of men and 30% of women with FH will develop coronary heart disease by the time they are 55.
Encouraging healthy changes such as improving your diet, stopping smoking or reducing your weight can help to lower cholesterol levels and reduce the risk of CVD and should be considered before initiating treatment with a statin. However, some people with high cholesterol will need to go straight onto a statin.
Due to the lack of a standard method of data collection and reporting, there is currently an absence of accurate data on the number of people with high cholesterol in England. Ambitions have therefore been agreed on the data that is currently available and there is a clear call for improved data on cholesterol in the future, including prevalence and management with statins.
The NHSLTP highlighted plans for a new primary care audit called CVDPREVENT, which will provide this data.
The challenge
High CVD risk
Data is not currently collected on the number of people who have had a CVD risk assessment and cholesterol reading. The percentage of people who have had these measurements done is therefore estimated, based on the number of people who have had an NHS Health Check in the latest 5-year cycle of the NHS Health Check (Quarter 1 2013 to Quarter 4 2018).
The NHS Health Check is a check-up for eligible adults in England aged 40 to 74 designed to assess a person’s risk of developing CVD and their chance of having a stroke or heart attack. In England, the percentage of people aged 40 to 74 who have had a cholesterol reading and CVD risk assessment is therefore estimated at 49%.
However, this is likely to be a conservative estimate as these measurements are also done outside of an NHS Health Check, England therefore has the potential to reach an ambition of 75% in the next 10 years.
Once a CVD risk assessment has been completed, NICE guidance suggests discussing the benefits of lifestyle modification before offering statins to people who have a 10% or greater 10-year risk of developing CVD. For some people, it may be necessary to start statin therapy straight away. This recommendation has proved to be controversial, which means that the public may be reluctant to take them.
The current achievement at both 10% and 20% risk thresholds is suboptimal. Of patients aged over 40 who were recorded on The Health Improvement Network (THIN) research database with a CVD risk score of ≥20% from 2012 to 2015, only 35% were initiated on a statin.
The ambition for optimal management of high CVD risk will therefore initially focus on increasing statin treatment to those who have a 20% or greater risk of developing CVD.
When good progress has been made, this ambition will be reviewed and an ambition for treating people who have a 10% or greater risk of developing CVD will be set, as per NICE guidelines.
Familial hypercholesterolemia (FH)
FH is an inherited condition that results in high levels of blood cholesterol and a high risk of heart disease at an early age. Management of FH with lipid-lowering therapy, such as statins, is highly effective but most people with FH are undetected and therefore not managed.
Identifying FH can either be done genetically, or non-genetically through confirmed family history and measured high cholesterol levels. There is little data on FH, but PHE analysis estimates that only 5% of FH patients have been genetically diagnosed in England.
In England there are 7,500 General Practices (GPs). If 25% of GPs each found 3 possible FH cases per year, 1 FH mutation positive patient would be diagnosed, leading to 19.1% being diagnosed. If 50% of GPs were to participate, the system could reach an ambition of 28% in 5 years.
An ambition for 25% of the expected number of people with FH to be genetically identified and optimally managed according to the NICE FH Guideline has therefore been agreed for England in the NHSLTP. The NHS has committed to deliver this in partnership with the wider system in the next 5 years. This ambition will then be reviewed.
Read case study: Identifying familial hypercholesterolaemia (FH) in primary care
Achieving the ambitions
Collaborative action
Cardiovascular disease prevention
Professor Jamie Waterall of Public Health England discusses how the CVD ambitions can be achieved with members of the National CVD Prevention Leadership Forum.
Achieving the ambitions requires a whole system effort. In the past, primary care has been thought of as responsible for identifying risk factors for CVD. Although it does have a vital role to play, primary care is overstretched and there are many other ways of finding the people most at risk so that they can get the help they need.
The NHS Health Check is mostly provided in primary care settings, but can also be delivered by pharmacies and local outreach programmes in workplaces and communities.
Pharmacies can also deliver opportunistic pulse and blood pressure testing, as well as providing healthy lifestyle advice. There are also new opportunistic ways of identifying high-risk factors, such as podiatrists performing pulse checks.
Read case study: Blood pressure testing outside of general practice
National policy influencers and local authorities can also raise awareness of CVD risk factors to help reduce prevalence of risk factors in the first place and promote both prevention and management via healthy lifestyle behaviours. This can help to reduce the burden on primary care.
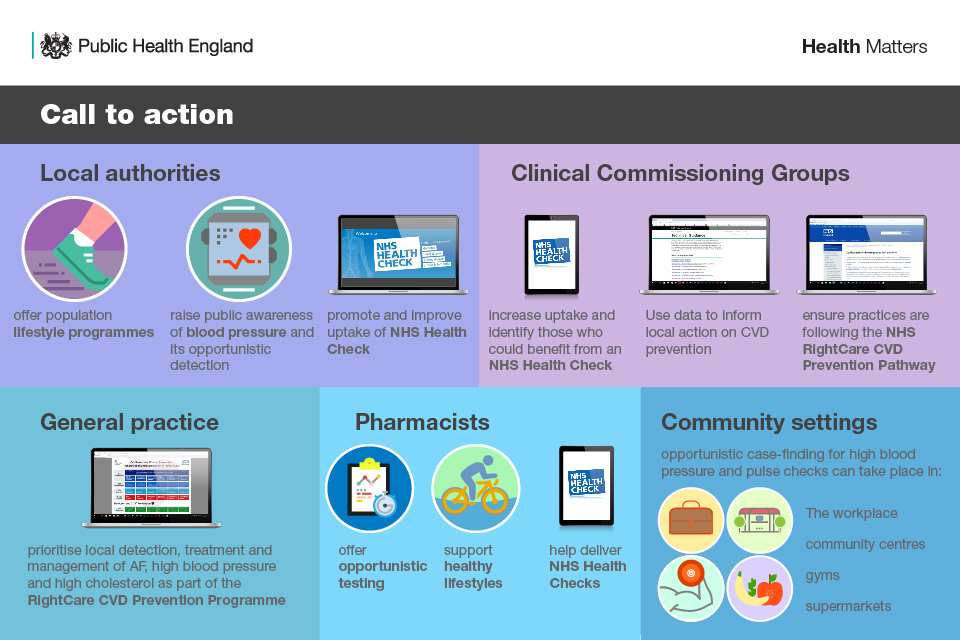
Infographic showing calls to action for local authorities, CCGs, general practice, pharmacists, community
Use the NHS Health Check to support early diagnosis and management
The NHS Health Check offers an opportunity to assess the top 7 risk factors driving premature death and disability in England among 15 million people in midlife. This includes pulse rhythm, BP and cholesterol. They are also supported to understand their risk of CVD and make positive behavioural changes that can prevent and delay the onset of CVD.
For example, everyone having an NHS Health Check should benefit from personalised support and access to local services, such as:
- stop smoking services
- weight management services
- physical activity services
- alcohol reduction services
- NHS diabetes prevention programme
Evaluations show that the NHS Health Check is also an effective mechanism for diagnosing disease earlier but that more could be made of the opportunity to ensure that people at high risk of CVD are offered appropriate clinical management. The NHS Health Check can also be delivered in a way that ensures people at the greatest risk of disease are prioritised, helping to narrow the gap in health inequalities.
Read the Health Matters edition on the NHS Health Check to find out more about how the programme is playing an important role in the prevention and early detection of CVD in England, as well as ways to increase the coverage and uptake of the programme.
Implement NHS England’s RightCare CVD prevention pathway
Optimally managing people with already identified CVD risk factors is the initial priority when focusing efforts on secondary prevention. Many people with known AF, high BP or high cholesterol are not currently taking treatment for their risk factor.
Prioritising efforts should therefore initially focus on optimally managing those already known to be at high risk of a CVD event, followed by identifying more people with high risk. Though detection of these ‘silent’ risk factors is extremely important, this will ensure that detection does not just increase on its own, leaving even more people sub-optimally managed for their condition.
NHS RightCare’s CVD prevention pathway, which is underpinned by NICE guidance, is an evidence-based optimal value pathway which provides information on:
- a high-level overarching national case for change
- a best practice pathway for individual conditions including AF, blood pressure and cholesterol
- best practice case studies for elements of the pathway demonstrating what to change, how to change and a scale of improvement
Using this pathway can help health professionals improve the detection and management of AF, BP and cholesterol.
| CVD interventions | ||
| Risk Factor | NICE Guidelines | NHS RightCare |
| Atrial fibrillation | CG180 | AF High Value Interventions |
| High Blood Pressure | CG127 | Blood Pressure High Value Interventions |
| High CVD Risk | CG181 | Cholesterol High Value Interventions |

Infographic showing what health professionals can do to improve cardiovascular disease management
Use existing data to make the case for action
There are a number of existing sources that can provide locally tailored information that will help to make the case for action to support the delivery of these ambitions.
PHE’s CVD primary care intelligence packs provide data and analysis on the prevalence, variation, treatment and CVD outcomes in clinical commissioning group (CCG) areas.
The size of the prize summarises the burden and the size of the opportunity that tackling AF, high BP and CVD risk can offer for each sustainability and transformation partnership (STP) in England.
The cost-benefit of taking action, for example, to increase statin prescribing, can be estimated at a CCG or STP level using the CVD return on investment tool.
Positive behavioural changes for preventing CVD

Infographic illustrating positive behaviour change for preventing cardiovascular disease
There are a number of behavioural risk factors that are associated with AF, high BP and high cholesterol.
Health professionals and local authorities should raise awareness of these factors and encourage people to make positive changes, which include:
- eating a healthier diet, including more fruit and vegetables (at least 5 portions of a variety of fruit and vegetables a day), fibre (including higher fibre and starchy carbohydrates) and oily fish, choosing lower salt, saturated fat and sugar options in line with the Eatwell Guide
- reducing the amount of salt in the diet which can lead to high BP
- cutting down on excess alcohol consumption, which is a causal factor for conditions including high BP
- being physically active including at least 150 minutes of moderate intensity activity each week, in bouts of 10 minutes or more, or 75 minutes of vigorous activity across a week or a mixture of moderate and vigorous activity
The National CVD Prevention System Leadership Forum
The CVDSLF will continue to work together to deliver the ambitions, including publishing their commitments and highlighting how the whole system can get involved.
Resources
These resources can be used in presentations of your own or to share with colleagues:
- supporting references
- Health matters infographics
- read the Health matters blog
Health matters case studies highlight projects and approaches that have been put in place to improve public health:
- Virtual clinics to improve BP in poorly controlled patients
- Blood pressure testing outside of general practice
- High blood pressure quality improvement in Cheshire & Merseyside
- Pharmacist-led virtual clinics to optimise anticoagulation in AF
- Identifying familial hypercholesterolaemia (FH) in primary care
