Health and social care integration: joining up care for people, places and populations
Updated 11 February 2022
Applies to England
Foreword: Rt Hon Sajid Javid, Health Secretary and Rt Hon Michael Gove, Secretary of State for Levelling Up, Housing and Communities
The storms we have weathered over the past 2 years have been a great test, but also a great teacher.
We have learned, most notably from our world-leading vaccination programme, that we are stronger when we work together and are united in our purpose and resolve.
We have also seen the moral outrage of persistent health disparities, mirroring other disparities in our society, illuminated as never before in our lifetimes. We have been reminded, once more, of the inextricable link between health services and social care.
So, as we recover and level up, it is right that we draw on our experience of the pandemic to bridge the gaps between health and social care, between health outcomes in different places and within society that are holding us back.
This is what our white paper aims to achieve by bringing together the NHS and local government to jointly deliver for local communities.
It sets out a new approach with citizens and outcomes at its heart instead of endless form-filling, unnavigable processes and a bureaucracy which sees too many people get lost in the system, not receiving the care they need. It is the start, not the end, of a new wave of reform which will both put power and opportunity in the hands of citizens and communities and build a state that is sustainable and just.
Through introducing a single person accountable for delivery of a shared plan at a local level, our proposals will ensure a more joined-up approach between health and social care. It will give health and social care professionals access to the right data and technology to make more informed decisions, and it will also help to create a more agile workforce with care workers and nurses easily moving between roles in the NHS and the care sector.
Moreover, the white paper also delivers on our ambition to level up health outcomes over the long term.
It champions health and well-being as a real priority and places a much greater emphasis on prevention.
To that end, it promotes community-centred care to help people with disabilities, who are suffering from dementia and other mental health issues to live independent and healthy lives.
Crucially, we are proposing measures to help bridge the gap in healthy life expectancy (HLE) between local areas by making sure there is universal access to high-quality treatments and support in all parts of the country.
At every step, this white paper has been shaped by the real-world experience of people as well as nurses, care workers and doctors on the front line, drawing on some of the great examples of collaborative working we have seen at a local level in recent years, not least over the pandemic.
It presents the next component of a bold vision for the future of health and social care in this country with people and patients at its very heart.
Executive summary
The NHS and local government have delivered remarkable things for the public, in the most challenging circumstances, over the last 18 months. From the extraordinary success of the vaccine programme, to meeting the needs of people previously identified as clinically extremely vulnerable and many other examples of reshaping services to continue to deliver care safely. There is a lot for local government and the NHS to be proud of and to learn from as we move into recovery from COVID-19. Through multi-agency community hubs, integrated neighbourhood teams, and other locally developed arrangements, local partners developed a shared understanding of local needs and made flexible use of resources across services to ensure that people got the support they needed. A vast range of other activity has been jointly delivered by various organisations thanks to a combined commitment to go beyond normal organisational boundaries and do whatever has been required to support their local residents. The resilience, commitment to finding a way through for citizens, and the willingness to innovate will all be just as important as we tackle the challenges ahead.
Among the lessons of the pandemic is the need to do more to bring the resources and skills of both the NHS and local government together to better serve the public. So, as well as record investment, NHS and local government reform will be needed to recover from the pandemic and deliver on the government’s priorities, including on its central mission to level up every part of the UK. Our health and care system needs to take this agenda forward with real urgency if the challenges the sectors face – both in the short and long term – are to be met; and this will need to be done with the full involvement of local leaders and the public.
Successful integration is the planning, commissioning and delivery of co-ordinated, joined up and seamless services to support people to live healthy, independent and dignified lives and which improves outcomes for the population as a whole. Everyone should receive the right care, in the right place, at the right time.
We want to go further and faster in building integrated health and care services. People should experience joined up care which makes the best use of public resources and services. While a more integrated approach clearly will not address all of the challenges facing staff, joining up services around users can also improve job satisfaction for the staff delivering them – removing some of the barriers that stop staff delivering care as they would like. This requires change that builds on improvements made across the health and care sectors in recent years.
While progress has been made, our system remains fragmented and too often fails to deliver joined up services that meet people’s needs. The goals of different parts of the system are not always sufficiently aligned to prioritise prevention, early intervention and population health improvement to the extent that is required. That needs to be our focus if we are to continue building better health, tackling unjustifiable disparities in outcomes, and ensuring the sustainability of the NHS and other public services. People too often feel like they have to force services to work together, rather than experiencing joined-up health, public health, social care and other public services.
This paper is part of a wider set of mutually reinforcing reforms: our adult social care reform white paper, People at the Heart of Care; the Health and Care Bill and reforms to the public health system. It sets out our plans to make integrated health and social care a reality for everyone across England and to level up access, experience and outcomes across the country. Specifically, this paper:
- sets out our approach to designing shared outcomes which will place person-centred care, improving population health and reducing health disparities at the centre of our plans for reform, and ensuring that accompanying oversight arrangements and regulatory structures have a clear focus on the planning and delivery of these outcomes
- sets out proposals to strengthen the health and care services in places that feel familiar to the people living in them. While strategic, at-scale planning is carried out at the integrated care system[footnote 1] (ICS) level, places will be the engine for delivery and reform
- introduces an expectation for a single person, of accountable at place level, across health and social care, accountable for delivering shared outcomes and strong, effective leadership
- sets out how we will make progress on the key enablers of integration (workforce, digital and data and financial pooling and alignment) required to further join up services around people and populations
- reinforces the role of robust regulatory mechanisms to support the delivery of integrated care at place level
Joined up care: better for people and better for staff
As people who use health and care services require ever-more joined up care to meet their needs, achieving this will make all the difference both to the quality of care and to the sense of satisfaction for staff. Without a decisive shift to consistently joined up care, we will continue to see fragmentation for people and frustration for staff. For example, closer working between primary and secondary care will improve access to specialist support and advice and enable care to be delivered closer to home, managing risk more effectively and keeping people healthy and independent. And closer working between mental health and social care services can reduce crisis admissions and improve the quality of life for those living with mental illness.
Unlocking the power of data across local authorities and the NHS will provide place-based leaders with the information to put in place new and innovative services to tackle the problems facing their communities. A more joined up approach will bring public health and NHS services much closer together to maximise the chances for health gain at every opportunity.
Shared outcomes which prioritise people and populations
Shared outcomes are a powerful means of bringing organisations together to deliver on a common purpose for the people they serve. We have set out the case for a new approach for designing and measuring progress against these. We will work with stakeholders to develop and introduce a framework with a focused set of national priorities, and an approach for prioritising shared outcomes at a local level, focused on individual and population health and wellbeing. We will set out a framework which makes space for local leaders to agree shared outcomes that meet the particular needs of their communities, whilst also supporting national priorities. Places will be able to choose health and care priorities that matter most to their citizens, alongside national commitments. Implementation of shared outcomes will begin from April 2023. There will be robust arrangements in place to assure both the planning and delivery of both national and local outcomes.
Ensuring strong leadership and accountability
Effective leadership, accountability and oversight are key to delivering integration. Local leaders – including in local government and the NHS, in partnership with their citizens – have a unique understanding of, and relationships with, their populations. We will make changes that bring together these leaders to deliver on shared outcomes in an accountable and transparent manner, through formal place-based arrangements which provide clarity over the responsibility for health and care services in each area. Several places such as Tameside have already successfully adopted arrangements of this kind.
We will set out criteria for place-level governance and accountability for the delivery of shared outcomes. We have suggested a model which meets those criteria and expect places to adopt either this specific governance model, or an equivalent, by spring 2023. The key characteristics needed in any model will be for it to develop a clear, shared plan and, crucially, to be able to demonstrate a track record of delivery against agreed shared outcomes over time, underpinned by pooled and aligned resources.
Local NHS and local authority leaders will be empowered to deliver against the agreed outcomes and will be accountable for delivery and performance against them. Any governance model should also provide clarity of decision-making, covering contentious issues, practical arrangements for managing risk and resolving disagreements between partners, and agreeing shared outcomes. There should be a single person, accountable for shared outcomes in each place or local area, working with local partners (for example, an individual with a dual role across health and care or an individual who leads a place-based governance arrangement). This person will be agreed by the relevant local authority or authorities and integrated care board (ICB). We would expect place-based arrangements to align with existing ICS boundaries as far as possible. We recognise that in some geographies this can be challenging, and we expect NHS and local authority partners to work together (drawing, where needed, on the flexibilities that the legislation will provide, subject to Parliament) to ensure that all citizens are able to benefit from effective arrangements wherever they live. These proposals will not change the current local democratic accountability or formal accountable officer duties within local authorities or those of the ICB and its chief executive.
Places will be supported by central government, NHS England, ICBs and others to develop arrangements which deliver the best outcomes for their populations.
Finance and integration
Financial frameworks and incentives can play a key role in enabling the integration of services and supporting service innovation.
Local leaders should have the flexibility to deploy resources to meet the health and care needs of their population, as necessary. NHS and local government organisations will be supported and encouraged to do more to align and pool budgets, both to ensure better use of resources to address immediate needs, but also to support long-term investment in population health and wellbeing.
Working within the principles set out in this paper, we will work with partners to develop guidance for local authorities and the NHS to support going further and faster on financial alignment and pooling. We will also review existing pooling arrangements (for example, section 75, NHS Act 2006), with a view to simplifying the regulations for commissioners and providers across the NHS and local government to pool their budgets to achieve shared outcomes. This will continue to be subject to both NHS and local authority partners agreeing what constitutes a fair and appropriate contribution.
Digital and data: maximising transparency and personal choice
A core level of digital capability everywhere will be critical to delivering integrated health and care and enabling transformed models of care. When several organisations are involved in meeting the needs of one person, the data and information required to support them should be available in one place, enabling safe and proactive decision-making and a seamless experience for people.
Digital tools will empower people to look after their health and take greater control of their own care, offering flexibility and support – through the NHS App and NHS.UK, remote monitoring and digital health apps. We will aim to have shared care records for all citizens by 2024 that provide a single, functional health and care record which citizens, caregivers and care teams can all safely access.
We will support digital transformation by formally recognising the digital, data and technology profession within the NHS Agenda for Change and including basic digital, data and technology skills in the training of all health and care staff. We will support all health and care staff to be confident when recommending digital interventions to patients and individuals using services, based on what we know works and what people want to access.
To support place-based organisations, ICSs will develop digital investment plans for bringing all organisations to the same level of digital maturity. These plans will outline how ICSs will ensure data flows seamlessly across all care settings and use tech to transform care so that it is person-centred and proactive at place level.
The digital and data transformations outlined in this document provide an opportunity for greater transparency. We will look to introduce mandatory reporting of outcomes for local places, putting citizens at the heart of what we do.
Delivering integration through our workforce and carers
The health and care workforce are our biggest asset, and they are at the heart of wrapping care and support around individuals. We want to ensure that staff feel confident, motivated and valued in their roles and that they can work together in a person’s interests regardless of who they are employed by. Staff numbers and skills across teams should be planned to meet the needs of their local populations and places. They should also be able to progress their careers across the health and social care family, supporting the skills agenda in their local economy. Our proposals in this paper build on our proposals to support the social care workforce, as outlined in our adult social care reform white paper, People at the Heart of Care.
To achieve this, ICS will support joint health and care workforce planning at place level, working with both national and local organisations. We will improve initial training and ongoing learning and development opportunities for staff, create opportunities for joint continuous development and joint roles across health and social care and increase the number of clinical practice placements in adult social care for health undergraduates.
What this means for people and communities
Taken together, these reforms will support a better joined up health and care system, with people’s wishes and wellbeing at its heart. Citizens with access to more information will be more empowered to make decisions about their care and have more choices about where and how they access care. Working with local places and ICSs, we will remove unnecessary barriers so places will be empowered to do what is best for their citizens. They will be supported to be transparent and accountable for the delivery on the outcomes which matter to communities, and variations in performance between areas will be addressed. The financial frameworks and incentives which support this will be reformed over time so that the way funding is allocated and accounted for does not prevent places and ICSs doing the right thing for the people they serve.
These reforms will help us develop a world-leading health and care system which works for every person, and where people work together to deliver continuous improvement in the delivery of health and care services. This is possible and necessary, and we will start making it a reality now.
1. Introduction: delivering more integrated services for the 21st century
The case for going further and faster on integration
1.1. When health and care organisations have a shared mission, work with their local citizens, and pool their ideas, energy and resources to serve the public, the result is often the delivery of outstanding quality and tailored, joined up care, which improves the experience and outcomes for individuals and populations. In recent years, and in particular during the pandemic, we have seen many examples of the power of collaborative working.
1.2. This is, however, far from the norm everywhere, and as the challenges of demography, the possibilities of technology and the expectations of citizens all grow, we will need to move beyond a health and care system where organisations and services operate in a compartmentalised way. People have a range of needs which cannot always be addressed neatly by one organisation or another. There is a greater need for holistic care that fits around these needs; our services, processes, institutions, and policies need to catch up. We know that, currently the public often experiences:
- a lack of coordination between the range of services looking after them. Information or actions can be lost between primary and secondary care; where primary care and hospital teams might have to form treatment plans without the crucial insights from a person’s carer; or different specialists might focus only on one or two conditions, without considering the needs of a person holistically
- organisations that are forced or incentivised – by regulation or the financial framework – to focus on their narrow set of organisational outcomes, rather than a health and care service that considers the health needs of the whole community
- duplication in use of resources or patients’ time. People being asked for the same information multiple times, by different organisations, which can lead to delays in diagnosis or treatment; or the use of NHS personal health budgets without considering whether an individual also has a personal budget for social care (and vice versa) and the impact on them of managing both budgets simultaneously
- delays in being discharged as a result of competing budgets and care processes
1.3. Ensuring there is holistic care that fits around people needs includes ensuring that people receive the right care and support, and can maintain healthy independent living, beginning with where they live, and the people they live with. Getting these housing arrangements right for individuals and communities is one example that requires the joining up of not just health and care partners, but a wider set of local government functions and housing providers. Today, too many people with care and support needs live in homes that do not provide a safe or stable environment. People’s homes should allow effective care and support to be delivered regardless of their age, condition or health status. We want people to have choice over their housing arrangements, and we also want to ensure places ‘think housing and community’ when they develop local partnerships and plan and deliver health and care services.
1.4. Over the last few years, there has been a great deal of valuable work to bring about greater integration:
- GP practices are already working together with community health services, mental health, social care, pharmacy, hospital and voluntary services in their local areas in groups of practices known as primary care networks (PCNs). Building on existing primary care services, they are enabling greater provision of proactive, personalised, coordinated and more integrated health and social care for people closer to home NHS Chief Executive, Amanda Pritchard, has asked Dr Claire Fuller (CEO Surrey Heartlands ICS) to lead a stocktake of how systems can enable more integrated primary care at neighbourhood and place, making an even more significant impact on improving the health of their local communities. This will report later in the spring
- the Better Care Fund was introduced to support places to integrate better by pooling budgets and ensuring there is joint planning between NHS commissioners and local authorities to deliver care. Better Care Fund plans have aided integrated work to support people to remain independent for longer, integration of reablement and improved performance on hospital discharge[footnote 2]
- new models of care and sustainability and transformation partnerships (STPs) considered local health priorities, encouraged better joint planning of services and tested innovative models of integrated care. For example, provider collaboratives in mental health have been empowered to reconfigure local services to reduce out of area placements and bring people closer to home to aid their recovery. STPs aimed to develop sustainable services to improve person-centred care in key areas and to improve hospital performance
- devolution, such as that seen in Greater Manchester, allows local places to have more flexibility to integrate care around the needs of their local populations
- local government and the NHS have jointly planned and commissioned some health services, to join up people’s experience of care and address both prevention and treatment
1.5. We know there is more we can do to better integrate health and care services, joining up planning, commissioning and delivery. We must go further, faster. The experience of COVID-19 has shone a spotlight on the health disparities which persist across the country. We need to prioritise prevention decisively and collectively, so that we build health resilience and are well placed to meet the multiple health and care challenges of our changing demographic. Done right, integration will enable concerted, collaborative effort across the whole of the health and care system to reduce the disparity gap and improve population health. In February 2021 we set out our ambitions for the future of health and social care, and for legislative reform to support this, in Integration and innovation: working together to improve health and social care for all. These proposals, including (subject to Parliament) establishing statutory integrated care boards (ICBs) and statutory integrated care partnerships (ICPs), ensure the health and care system will be much better equipped to collaborate across boundaries, make joint decisions and form alliances to tackle shared problems.[footnote 1]
1.6. These proposals were based on the learning from those at the forefront of delivering more integrated care and support locally; in particular how important their partnerships had been when responding to the COVID-19 pandemic. We remain committed to this direction of travel and just as proud of the achievements of our health and care services as they continue to rise to the ongoing operational challenges they face.
1.7. The creation of ICSs as a formal part of our health and care system is a critical opportunity to remove remaining barriers to integrated care and create the conditions for local partnerships to thrive. This paper builds on those ambitions and provides further detail on our plans to empower leaders and strengthen collective working between the NHS and local government at place to work in partnership to achieve the best for those they serve.
Case study: Teesside
Sexual health services across Teesside’s 4 local authorities, 2 CCGs and NHS England are collaboratively commissioned by one prime provider. With a strong focus on prevention, the new service has both improved access and achieved savings, and is highly rated by users, consistently getting a high score on the ‘Friends and Family’ test. It has enabled a greater focus on improving the sexual health of young people, including chlamydia screening, provision of young-people friendly services, access to contraception and outreach, and the prioritisation of HIV prevention. Using equity measures they monitor progress, not just at borough level but using universally shared outcomes.
Our vision for integrated health and care services
1.8. Integration is not an end in itself, but a way of improving health and care outcomes. Successful integration is the planning, commissioning and delivery of co-ordinated, joined up and seamless services to support people to live healthy, independent and dignified lives and which improves outcomes for the population as a whole. Everyone should receive the right care, in the right place, at the right time. Our vision is that integration makes a significant positive impact on population health through services that shift to prevention and address people’s needs promptly and effectively; but it is also about the details and the experience of care – the things that often matter most to people, carers and families. This is captured in the ‘Think Local Act Personal’ statement below:
Everyone should be able to say: ‘I can plan my care with people who work together, to understand me and my carer(s), who allow me control, and bring together services to achieve the outcomes important to me.’
National Voices, TLAP 2013
1.9. This paper seeks to deliver this vision, through the introduction of shared outcomes, agreed by all local health and care organisations, and the delivery of which all local leaders will be held to account for. To facilitate this, we outline the place level accountability arrangements to underpin delivery and the arrangements for aligning and pooling of resources, digital transformation and changes to regulation that will enable change.
1.10. Integration needs to be delivered at every level:
- individuals: for people wanting to live lives which are as healthy and independent as possible, their communities, for carers and families
- neighbourhood and communities: areas covered by, for example, primary care and their community partners
- place: a geographic area that is defined locally, but often covers around 250,000 to 500,000 people, for example at borough or county level
- system: usually larger geographies of about one million people which often (but not always) cover multiple places
- national: in this case, the whole of England
1.11. Our focus in this document is at place level. It is where local government and the NHS face a shared set of challenges at a scale that often works well for joint action. Strong places are also important for effective working at both system level (with many ICSs investing a great deal of effort into developing places within their geography) and at neighbourhood and community level (where the support of places in making improvements happen is critical to success). Our responsibility in central government to facilitate and support improvements at place level, ensuring the right structures, accountability and leadership are in place to enable effective integration locally.
1.12. Whilst children’s social care is not directly within scope of this paper, places are encouraged to consider the integration between and within children and adult health and care services wherever possible. The transition to ICSs represents a huge opportunity to improve the planning and provision of services to make sure they are more joined up and better meet the needs of babies, children, young people and families. The Independent Review of Children’s Social Care is taking a fundamental look at the needs, experiences and outcomes of the children supported by children’s social care. We will consider and respond to the recommendations and final report of the care review once it is published. Government is championing the continued join up of services, expanding family hubs to more areas across the country, and funding key programmes such as Supporting Families and supporting the implementation of the Early Years Healthy Development Review. At the recent Budget, we announced a £500 million package for these services, to provide more support for families so that they can access the help and care that they need. Ensuring that every area has joined up, efficient local services, that are able to identify families in need and provide the right support at the right time, will enable children and young people who rely on multiple public services to thrive.
1.13. This paper sets out our ambition for better integration across primary care, community health, adult social care, acute, mental health, public health and housing services which relate to health and social care.
1.14 Our plans will support the development of a health and care system which:
- is levelled-up in terms of outcomes and reduced disparities
- ensures people have access to health and care services which meet their needs, and experience outstanding quality care
- transforms where care is delivered, according to people’s preferences (including at home and in the community). This includes ensuring that people are discharged in a timely, safe and efficient way from hospital
- enables people to access personalised information about their health and care – to give them more control over their own health and care journey – informed by excellent, timely data and integrated care records
- enables data and information sharing to support joined up and informed decisions around an individual’s care, and better understanding of the needs and priorities of local populations
- is delivered by a capable, confident, multidisciplinary workforce which wraps services around individuals and their families and carers
- allows and encourages innovation and digitisation to ensure that we have the right tools which enable people to have their needs met in the right place
- has joined up, workforce planning at the system level to ensure the right people, with the right skills and training to deliver collaborative, person-centred care
- incentivises organisations to prioritise the same shared outcomes and goals, so rather than a narrow focus on their own organisational targets, they can think about health and care journeys and outcomes, to ensure people don’t fall through gaps between services or settings, or bounce around the system
- incentivises organisations to collectively prioritise upstream interventions for individuals and communities, and increasingly allocate resource to improve population health and address disparities
- is driven forward by decisive leadership, who listen to and understand the needs of their local people and have clear accountability for delivering those outcomes
1.15. There is a widespread commitment to this agenda – we know health and care professionals and leaders want to do more to join up services. People want the services they use to be better joined up around their needs. Better integration can facilitate better care for people now, as well as in the long-term, as the importance of prevention grows.
1.16. Change is needed, and the potential reward – in better outcomes and value for citizens – is significant. Integration does not, of itself, guarantee improved outcomes – doing it well is what is required.
Our policies, interventions and the support we provide will therefore continue to promote the benefits of flexibility, local learning and the evolution of ways of working at place and system. The truly radical possibilities in this agenda are much more likely to be identified and realised by local organisations than through central prescription.
Case studies
Tom and Maureen
Tom is 85 years old and has mild undiagnosed dementia, he is currently living at home with his wife of 60 years, Maureen, who has been his constant support. The couple have lived in their home for 55 years. Maureen, who is of similar age to her husband, suffers with pain in her heart from angina and has high blood pressure. It is of increasing concern to their children, Dan and Sarah – who do not live locally, that the couple do not receive support from local services. Tom and Maureen are unaware of where to seek help as they are both unfamiliar with and lack confidence when using digital technology and feel like they are able to support themselves. Tom suffered from a fall down the stairs and fractured his hip.
Bunmi
Bunmi is a woman with chronic obstructive pulmonary disease (COPD), osteoarthritis and early dementia. She lives in sheltered accommodation and is moving around less than she usually would. Bunmi still tries to attend church every Sunday, however over the past few weeks she has been struggling to get out because of her worsening health and it is affecting her mood.
Kwame
Kwame is from the North East of England and has just celebrated his 18th birthday. Kwame loves to be outdoors and is a big fan of Star Wars. He also has a learning disability, autism and when anxious, he can display behaviour that can be particularly challenging to services.
Kwame has spent several years in an out of area residential, educational placement arranged by the local authority. This caused considerable increase in his anxiety and behaviours, placing himself, staff and other children at risk. This led to him spending more time in self-imposed seclusion. He was admitted for treatment at a specialist children’s hospital where he seriously assaulted a member of staff. To make the situation safer for people around him, Kwame’s interaction with family and staff was done through a glass pane and intercom system.
Madeleine
Madeleine is 65 years old and lives alone with her guide dog. She has been visually impaired since birth. She has 2 grown-up children and one grandchild all of whom live abroad. Good technology means that she is in contact with them on a daily basis but gets practical support from being involved in her local community. In common with most visually impaired people, Madeleine does not have any statutory support but relies on the services provided by Guide Dogs for the Blind Association.
Mandeep
Mandeep is a 24-year-old who struggles to maintain a job due to issues with his mental health. He had learning difficulties which were undiagnosed, resulting in his inability to gain a formal qualification. This affected Mandeep’s relationship with his family who did not understand why he was not achieving. Mandeep left home at 16 and stayed with friends or in supported accommodation when he could. He has type 2 diabetes and is often tired which has caused issues for him in the workplace. Mandeep is at risk of homelessness as he does not have a steady income and is unsure of where to go for help.
Richard
Richard has long-term schizophrenia. He has spent many years constantly bouncing in and out of long stay psychiatric inpatient admissions, but he wanted to live at home independently. After a recent relapse and hospital admission, the ward team identified that part of the reason for his psychotic relapse was that he was falling behind with rent payments and his house had damp and heating problems that he couldn’t fix. While the clinical team on the ward worked to stabilise Richard, including taking his medication, they also sought early input from local authority housing workers who work into the ward and could start on the paperwork to maintain Richard’s tenancy and arrange work to get the damp sorted.
2. Shared outcomes
Summary
Collaboration is essential to delivering joined-up care. Our frameworks should support organisations and systems to work together in pursuit of the same goals, which focus on individuals and population health and wellbeing.
It is right that the national government sets some delivery standards for organisations, to ensure that the public receive a consistent standard of care. But if we are to allow local leaders to work together to make the most of their shared resources on behalf of local people, we need to better support organisations to pull in the same direction.
Some outcomes and goals are appropriately set nationally, but we also need to make space for local leaders to agree shared outcomes that meet the particular needs of their communities. We need a new approach to setting shared priorities which is integrated and focuses on key outcomes which matter for people’s health and wellbeing and improve population health. Some local organisations will be focused on the delivery of outcomes relatively independently of other organisations; but to respond to increasing complexity and multi-morbidity, services should be free to support partner organisations, even when they are not the main delivery agent. For example, hospitals should be incentivised to support public health outcomes, and primary care should be incentivised to support social care outcomes.
Following further work with stakeholders, we will set out a framework with a focused set of national priorities and an approach from which places can develop additional local priorities.
Implementation of shared outcomes will begin from April 2023. In parallel, we will ensure that accompanying oversight arrangements and regulatory structures have a clear focus on the planning and delivery of these outcomes.
As part of the shared outcome setting process, we will review alignment with other priority setting exercises and outcomes frameworks across the health and social care system and those related to local government delivery.
Why shared outcomes matter
2.1. Shared outcomes bring organisations and the people they serve together, and shared outcomes with clear plans for delivery make impactful change happen. We have seen this in both the ICSs that have made the most progress in recent years and in the collaborative working during the pandemic. Priorities tend to be most effective when they are outcome-focused (rather than focusing on output or inputs), when they are specific, and when they reflect clearly the most important issues for local people. The right outcomes will encourage local innovation and positive change.
2.2. Currently, we have many and varied priorities and outcomes for the health and care system, used by different organisations for different purposes, albeit with some areas of overlap and alignment. There are outcomes frameworks for each of public health, the NHS and adult social care, as well as outcomes for local government more broadly. In parallel, priorities have been set in the NHS Long Term Plan and in the government’s mandate to NHS England. Organisational priorities are also shaped by the broader regulatory framework and by statutory duties.
2.3. In recent years we have seen systems and local partnerships working together to deliver shared outcomes and we need our national frameworks to reflect the increasing importance of collaboration in pursuit of joined-up care for local people. Whilst acknowledging the varying roles the current outcomes do serve across the system, it is important that they do not pull local leaders away from collaboration, but rather enable partner organisations to work together to deliver against outcomes that truly matter to the people they serve.
2.4. As we increase our expectations of integrated working at system and place, it is right that we revisit how outcomes are articulated and prioritised- nationally and locally – to ensure that we are doing all we can to support the achievement of greater integration. This will be vital if we are to achieve a decisive shift to a model focused on population health and delivered through a shared understanding of population need and what can be done to improve services. Outcome frameworks, prioritisation exercises and associated processes designed for one or more organisation- or sector-specific purposes will need greater alignment if we want to go further and faster on integration.
2.5. What counts as a good outcome will, in many cases, require much closer working with people who use health and care services. This should result in people having more control in decision-making about what matters in their individual lives. This is perhaps more developed in social care than in health care, and it is becoming an increasingly important element of effective support for people with multiple conditions. In defining shared outcomes, success will therefore be reflective of what individuals want for their own care and what will maximise their wellbeing, focused not only on an individual organisation’s services but also the connections between organisations and services they provide.
2.6. A new approach to shared outcomes will ensure that organisations can work together, focusing on shared goals which improve outcomes for people and populations, and underpinned by measures which support this aim. Following publication, we will work with stakeholders to set out national priorities and a broader framework for local outcome prioritisation for implementation from April 2023.
Design principles for a shared outcomes framework
2.7. Generally, places are best placed to prioritise the outcomes for local people that matter the most.
2.8. Shared outcomes will need to be designed by partners across the system and with citizens, grounded in shared insight and understanding of the needs of the population.
2.9. Integration of services and ambition in improving outcomes go hand in hand. Where there is strong alignment, trust and common purpose between partner organisations, accompanied by a strong local role in identifying priorities, we expect to see high levels of ambition in the outcomes which places identify.
2.10. An approach for agreeing local outcomes will be an essential part of the shared outcomes framework. Some national priorities will, of course, always be needed to secure the improvements in care and outcomes that the public expect – such as those to support elective recovery and hospital discharge to ensure people receive the right care in the right place at the right time. To this end, the government will continue to set a mandate for NHS England. We intend to set out a small and focused set of national priorities, which all places will be expected to deliver alongside their own local priorities. Local and national prioritisation and goal-setting processes should therefore be complementary and realistic. Central government will need to ensure that the priorities set at national level allow sufficient space for local prioritisation in pursuit of the needs of their local populations.
2.11. Outcomes will sit alongside – and complement – systems’ and organisations’ statutory responsibilities and wider regulatory frameworks, and our intention is to address the problem of organisations being pulled in different directions by competing outcomes and targets.
2.12. There is also an important national role in ensuring that national and local outcomes work and sit together coherently such that there is clarity and consistency, and so that local organisations and partnerships are able to consider their own progress in comparison with others.
2.13. We do not intend that shared outcomes should add to the overall burden of national requirements. In defining national outcomes, we will consider what can be aligned or replaced from our current priority and outcome setting exercises and frameworks.
2.14. We want to focus on outcomes rather than outputs. Although outcomes are harder to measure and can take longer to deliver, they offer the best prospect of decisions and services which are both person-centred and improve population health over time. When outcomes are long term, we will need to identify interim or proxy metrics which demonstrate that organisations are collectively making progress towards them.
2.15. Our outcomes-centred approach must therefore be focused on the end goals of better person-centred health and care, improving population health and addressing disparities rather than on the process of integration per se. So, for example, outcomes should focus on areas such as people’s experience of care, wellbeing, and independence, not on organisational processes or decision-making. Further illustrative examples of outcomes are provided below.
2.16. National bodies with a regulatory or oversight role will consider the setting and delivery of outcomes in discharging their regulatory duties.
Illustrative examples of shared outcomes
Mental health
A shared outcome for mental health could mean people with mental illness living well in the community. A shared set of patient reported outcome measures (PROMs), could help align NHS clinical support with local authority support through social care, housing, and other services to improve recovery rates and quality of life for people living with mental illness.
Maternal smoking
Greater Manchester (GM) have taken a whole system approach to addressing smoking in pregnancy. Working collaboratively with foundation trusts, clinical commissioning groups, maternity services and across 10 local authorities. GM have implemented a financial incentives scheme, which enables women to access shopping vouchers at certain timepoints during pregnancy and beyond, conditional on them remaining smoke free. Outcomes from this integrated approach include an increase in the number of women successfully stopping smoking, higher average birth weight of babies and reductions in the number of babies requiring neonatal care.
Enhanced heath in care homes
Enhanced Health in Care Homes (EHCH) provides proactive care for care home residents and is delivered through a whole-system collaborative approach across health and care providers. Primary Care Networks must ensure that every care home has a named clinical lead, receives a weekly home round, and is supported by a multi-disciplinary team, and that every care home resident has a personalised care and support plan within 7 working days of admittance or readmittance. It involves a range of partners, including those from health (both primary and community care services), social care, voluntary, community, and social enterprise (VCSE) sector, as well as care homes, who are expected to work collaboratively with care homes to improve their local models over time.
As part of the care model, there are various shared outcomes which these providers are trying to achieve including:
a. high-quality personalised care within care homes
b. access to the right care and the right health services in the place of their choosing
c. reducing unnecessary conveyances to hospitals, hospital admissions, and bed days while ensuring the best care for people living in care home
Hospital discharge
Discharging people from hospital is an activity that needs acute, community, primary care and adult social care to work together. A shared outcome around discharge could bring together a group of outcomes in various existing frameworks to look beyond discharge to ‘right care, right place’.
What we will do
2.17 The government will undertake further engagement with partners and stakeholders and use these discussions to set a focused set of national outcomes alongside a broader framework for local outcome priorities. Initially, outcomes will focus on health services, the public’s health and adult social care. National and regional partners will play a key role in setting coordinated and consistent strategies to enable all organisations within the wider health and care landscape to align their activity to these national and local outcomes.
2.18 Places, working with local people and communities, will then identify and agree their local outcome priorities with reference to the broad framework. Places will agree action required to meet national and locally identified priorities.
2.19 ICSs will provide support and challenge to each local area as to the assessment of need and local outcome selection and plans to meet both national and local outcomes. Plans should be in place for implementation from April 2023.
2.20 We expect local arrangements, and the ICSs they are within, to take the lead on identifying issues and barriers to delivery and bring about real change for citizens. The Care Quality Commission (CQC) will consider outcomes agreed at place level as part of its assessment of ICSs. The CQC will also continue to develop its assessment of individual providers, to ensure their contribution to plans that improve outcomes at place and ICS level are assessed as part of the overall oversight framework.
2.21 These will build on existing oversight arrangements, some of which we are aiming to strengthen through the Health and Care Bill. The CQC will play a critical role. In addition to its current role in regulating and inspecting health and care providers, the CQC will review ICSs including NHS care, public health, and adult social care and assess local authorities’ delivery of their adult social care duties.
2.22 Working with partners, the CQC will consider both the starting position for each ICB and local authority, and the local and national priorities each area needs to manage, to help understand how all those responsible for health and care services are working together to deliver safe, high quality and integrated care for the public. Further work is underway to develop the detail and methodology of the CQC reviews, in line with existing oversight and support processes.
We will engage with partners and stakeholders to effectively design and implement shared outcomes. We will invite views on the following questions:
- Are there examples where shared outcomes have successfully created or strengthened common purpose between partners within a place or system?
- How can we get the balance right between local and national in setting outcomes and priorities?
- How can we most effectively balance the need for information about progress (often addressed through process indicators) with a focus on achieving outcomes (which are usually measured and demonstrated over a longer timeframe)?
- How should outcomes be best articulated to encourage closer working between the NHS and local government?
- How can partners most effectively balance shared goals or outcomes with those that are specific to one or the other partner – are there examples, and how can those who are setting national and local goals be most helpful?
3. Leadership, accountability and finance
Summary
Leaders are essential for bringing partners together to deliver outcomes that really matter to people and populations.
We will empower effective leaders at place level to deliver the shared outcomes that matter for their populations by setting an expectation that by spring 2023, all places within an ICS should adopt a model of accountability, with a clearly identified person responsible for delivering outcomes, working to ensure agreement between partners and providing clarity over decision making.
We will also work with the CQC and others to ensure there is effective regulation and oversight and that these new models achieve their purposes. CQC reviews will consider both how services deliver safe, high quality and integrated care to the public and the strength of integration within an ICS.
We will develop a national leadership programme, addressing the skills required to deliver effective system transformation and local partnerships, subject to the outcomes of the upcoming leadership review.
We want to build on progress in recent years to go further and faster in pooling and aligning funding to enable delivery at place level. Our expectation is that aligned financial arrangements and pooled budgets will become more widespread and grow to support more integrated models of service delivery, eventually covering much of funding for health and social care services at place level. These should be supported by robust frameworks to manage risk and deliver value for money.
To support this, we are reviewing section 75 of the NHS Act 2006 (which allows partners such as NHS bodies and councils to pool and align budgets) to simplify and update the underlying regulations.
Finally, we are reaffirming our commitment to personal health budgets, personal budgets, and integrated personal budgets as a means for supporting integration around individual patients and people who draw on care services.
3.1 Leaders are essential for bringing partners together to deliver outcomes that really matter to people and populations.
3.2 There are many great leaders in health and care across places in England who have made incredible progress to integrate health and care services and to join up care to improve outcomes for their populations.
3.3 At place level, this is especially important. Local leaders – including clinical and professional leaders – are well placed to understand the health and care needs of their local populations and to deliver the right change to level up health and care outcomes.
3.4 Effective local leaders are responsible – and seen to be responsible – for delivering the right outcomes and value for money, tackling health disparities, and for how well they have brought together the relevant partners to do so. We need to create the conditions to make this the norm in all places.
3.5 Many leaders, however, find that significant effort, persistence and resources are required to achieve the levels of collaboration and integration that match their ambitions and commitment. In particular:
- financial flows, priorities set nationally, and regulations can pull organisations away from shared goals
- managing complexity and a multitude of relevant actors can make partnership working difficult to do
- a reliance on relationships and ‘soft’ levers can work well in areas where there are strong relationships built over time, but lacks resilience as it is vulnerable to change in leadership, and is not universal
- support and incentives for leaders often focus on developing effective leaders for individual organisations within their siloes, rather than effective leadership of partnerships
Developing effective leadership for integration
3.6 The Health and Social Care Leadership Review will look to improve processes and strengthen the leadership of health and social care in England. It will consider how to foster and replicate the best examples of leadership and will aim to reduce regional disparities in efficiency and health outcomes. The review will report to the Secretary of State for Health and Social Care in early 2022 and will be followed by a delivery plan with clear timelines on implementing agreed recommendations.
3.7 Without pre-empting that review, we believe effective local leaders for health and care should:
- bring their partners together around a common agenda with decisive action in the interest of local people, even when it runs counter to organisational interests
- be able to judge when it is right to remove or challenge organisational boundaries and when it is better to make connections between distinct organisations
- be responsible for delivering outcomes, ensuring data is used and shared safely and effectively, to provide shared insight and a holistic understanding of the health and care needs of their local population
- focus decisions both on what happens at the point of care, and on what is of most benefit from a population perspective – taking a strong interest in what delivers value for money over time
- listen to the voices of people who draw – or may need to draw – on services when designing and improving those services and in defining which outcomes matter to individuals and populations
- support and enable clinical and adult social care leadership in the development and delivery of services
3.8 Again, subject to the recommendations of the leadership review, we will also look to develop a national leadership programme, addressing the skills required to deliver effective system transformation and local partnerships. This programme will also help to build locally the relationships and shared mission that we know is so important to successful integration.
Clear accountability
3.9 Effective integration and local prioritisation require both a strong, shared sense of purpose and clarity of accountability at place level, so everyone is clear who is responsible for delivering what, with which levers and what budgets. This has been demonstrated time and again in local places and wider health and care systems with a strong track record on integration.
3.10 All areas should ensure there is excellent value, good outcomes and improved experience for people. However, the specific areas for action will differ from place to place, as will the accountability arrangements that work best; as is already the case in the most successful places and systems. We therefore have not prescribed either. We do, however, want to ensure the benefits of integrated care are experienced in all places and as soon as possible, and to that end will set out criteria for local governance and accountability for the delivery of shared outcomes. We have suggested a model which meets those criteria.
3.11 Success will depend on making rapid progress towards clarity of governance and clarity of scope in place-based arrangements. We are therefore setting the expectation that, by spring 2023, all places within an ICS should adopt either a governance model as outlined below, or an equivalent model which achieves the same aims. The characteristics we would expect a governance model to have are:
- a clear, shared, resourced plan across the partner organisations for delivery of services within scope and for improving shared local outcomes
- over time, a track record of delivery against agreed or shared outcomes
- a significant and, in many cases, growing proportion of health and care activity and spend within that place, overseen by and funded through, resources held by the place-based arrangement
3.12 We would also expect a governance model to provide clarity of decision-making covering:
- contentious issues such as reshaping services within the place (and contributions to wider decisions such as reconfigurations across a wider geography)
- clear, practical arrangements for managing risk, resolving disagreements between local partners, and for agreeing the outcomes to be pursued locally in addition to any set nationally, with strong involvement for the health and care provider organisations for that place
- a single person, accountable for the delivery of the shared plan and outcomes for the place, working with local partners (for example, an individual with a dual role across health and care or an individual lead for a ‘place board’ as outlined from paragraph 3.18). The single person will be agreed by the relevant local authority or authorities and ICB. This proposal will not change the current local democratic accountability or formal accountable officer duties within local authorities, those of the ICB Chief Executive or relevant national bodies, such as the ability of NHS England to exercise its functions and duties
3.13 These arrangements should, as a starting point, make use of existing structures and processes including Health and Wellbeing Boards and the Better Care Fund. They should also provide clarity about what is done at place and at system levels.
An accountability model and local innovation
3.14 We expect all local areas to put in place-based arrangements to bring together NHS and local authority leadership. This will include responsibility for effective commissioning and delivery of health and care services. Local health and care leaders set and agree the shared outcomes and will be held accountable for delivery of these outcomes.
3.15 Places will be able to decide which model they adopt, and we have outlined one illustrative model (the place board model) that is a good basis for delivering the characteristics described above.
3.16 This will build on ‘Thriving Places’, the joint Local Government Association (LGA)- NHS England (NHSE) guidance published in September 2021.
3.17 Places will be supported in this work by their ICSs and by an NHS England or local government support offer.
The place board model
3.18 In this arrangement, a ‘place board’ brings together partner organisations to pool resources, make decisions and plan jointly – with a single person accountable for the delivery of shared outcomes and plans, working with local partners. In this system the council and ICB would delegate their functions and budgets to the board. Integration of decision-making would be achieved through formal governance arrangements (likely to include definition of membership; responsibility for outcome-setting; responsibility for delivery of functions or programmes delegated; financial arrangements including pooling; and dispute resolution and decision-making). The place board lead would be agreed by the ICB and the local authority (or authorities) for the place.
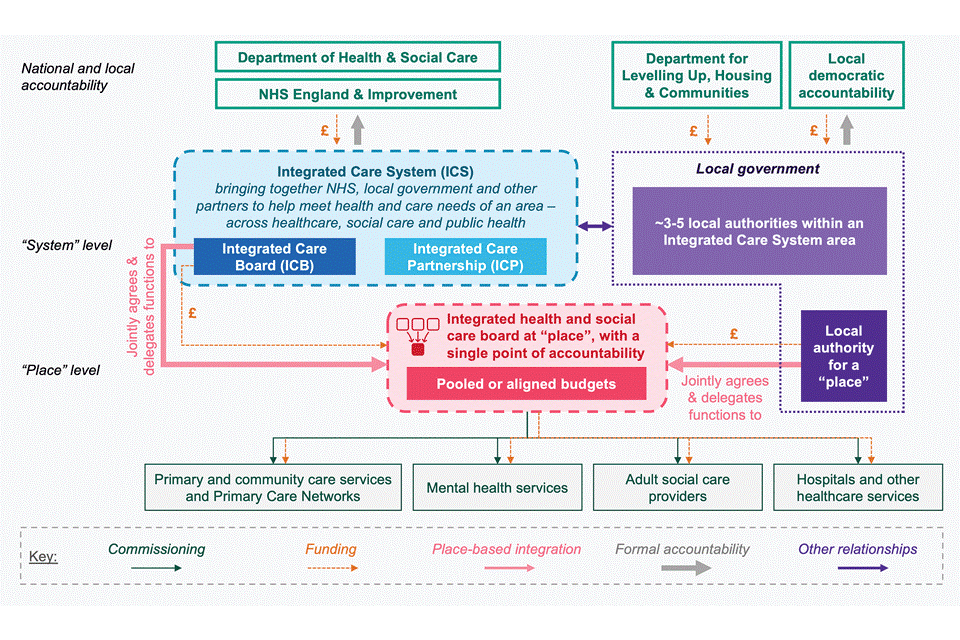
Note: This diagram this is a simplified example of potential governance arrangements and not a full representation of the richness, complexity and range of partnership working across the organisations within systems.
3.19 As the development of ICSs has shown, there is enormous potential within the health and care system to find innovative ways of managing and improving care, and we want to bring that same spirit to the development of places. We are likely to secure more value through setting challenges than through setting limits on that innovative potential. We would therefore stress that the model described here is simply a model, and not the only one. We believe it meets the criteria we have set out above, and so serves as a helpful illustration of what is needed; but the criteria are what really matter. Both places and ICSs vary in size, with some ICSs covering nearly 3 million people and others scaled to the same size as places within other systems. Strong systems and strong places complement and support each other; and this means that it will be important for all relevant partners to work together to agree suitable, proportionate, complementary governance arrangements at place and at system level. In the small number of cases where systems and places are effectively the same geography, we would not expect both place-based and ICS arrangements to be set up as that would be bureaucratic and unhelpful. There are no national plans for further changes to ICS boundaries.
3.20 In addition to clarity of governance, all places will need to develop ambitious plans for the scope of services and spend to be overseen by ‘place-based’ arrangements. From April 2023, arrangements for national and local shared outcomes will go live.
3.21 Those able to go further should do so by putting in place extensive inclusion of services and spend at a local level.
3.22 All local areas should work towards inclusion of services and spend by 2026. Of course, local partners would need to agree fairness in pooling arrangements set out at para 3.24 in working towards this goal.
Financial frameworks and incentives
3.23 Financial frameworks, like other critical enablers of integration such as leadership, workforce and digital are essential to realising our vision of integrated care. However, financial frameworks cannot and do not operate in isolation. They must align with and reinforce our wider strategic objectives and delivery approach, including regulatory, accountability, behavioural and organisational frameworks.
3.24 However, in practice, over the last decade, financial frameworks have often been cited as a barrier to the development and delivery of integrated approaches. There is no one-size-fits-all approach, given how different local systems are in terms of the populations they serve and the existing organisations they contain. However, this complexity is challenging to navigate, often requiring complex workarounds which make it hard to plan and share risk – this being critical to delivering integrated approaches. There are mechanisms that places can use to overcome this (for example, pooled budgets underpinned by legislation through section 75 of NHS Act 2006), but there is scope to simplify and update these mechanisms. In this document, we refer to both ‘pooling’ and ‘aligning’ of resources. Pooling requires a more formal agreement while aligning resources – which can include significant resource and collaboration – is less formal. We want to ensure there is flexibility to enable as much collaboration and integration as possible. In some cases, particularly as arrangements at place mature, it may well make sense to put in place more formal pooling arrangements, and we would expect the overall level of pooling to increase in the years ahead. Pooling agreements will remain subject to both NHS and local authority leadership and NHS system and place leaders agreeing what constitutes a fair and appropriate contribution. A clear sense of fairness for all partners is an important basis for integration and, as we have seen in the most effective systems and partnerships in recent years, a strong culture of trust and mutual accountability allows partners to then focus on the pursuit of shared outcomes.
3.25 We have recognised these challenges. Within the NHS, through the Health and Care Bill (subject to bill passage) we are seeking to enable different parts of the health and care system to work together as part of a move towards a whole population-based approach. This will be underpinned by a collective approach to managing resources, with ICSs as the primary unit for NHS financial planning and accountability, operating with a single system funding envelope across acute, ambulance, community, mental health and primary care (starting with general practice).
3.26 Subject to bill passage, these changes will be complemented by other measures such as Joint Committees, as well as a holistic set of statutory duties and oversight. For example, there is the Triple Aim duty which covers the health and wellbeing of people in England, the quality of services provided or arranged by both themselves and other relevant bodies (NHS England, trusts and foundation trusts, and ICBs), and the sustainable and efficient use of resources by both themselves and other relevant bodies. There are strengthened duties to cooperate, as well as clauses on system collaboration and financial management agreement in NHS standard contracts. We are also joining up services for individuals through expanding the use of personal health budgets (PHBs). The NHS Long Term Plan sets out the commitment to grant individuals more control over their own health, and more personalised care when they need it, through initiatives such as the national roll-out of the NHS’s comprehensive model for personalised care across the country and accelerating the roll-out of personal health budgets to give people greater choice and control over how care is planned and delivered (with up to 200,000 people benefiting from a PHB by 2023 to 2024).
3.27 Pooling of funding to support joint delivery of services is not new and we have established mechanisms for doing this (such as the Better Care Fund (BCF) and section 75 of the 2006 Act). Many areas already use these mechanisms to ensure that the right funding is in the right place to support the delivery of shared objectives with pragmatic mechanisms to manage financial risk. There are examples of systems using these to enable ambitious models of integration which involve pooling a significant proportion of their funding. However, there are also examples of bureaucracy and conflict which prevent pragmatic attempts to improve services. This is not in the interests of those receiving or providing care – local organisations have a shared responsibility to maximise the outcomes of patients, service users and value for the taxpayer.
3.28 Our proposals in the Health and Social Care Bill seek to simplify the governance mechanisms around these arrangements, making it easier for local organisations to collaborate. However, as set out above, we want to go further to drive progress. Our vision for integration, centred around individuals and local populations requires shared objectives, dynamic and collaborative leadership; alongside mechanisms to enable joint working (such as pooled or aligned budgets). When set up effectively, framed around people and service delivery, these are an important way of putting the public pound towards a shared purpose.
3.29 The current system allows a lot of ambition using pooled budgets, but it largely relies on local leadership to drive this. Since 2015, through the BCF, local NHS commissioners (CCGs) have pooled a proportion of their allocations, alongside funding from local government to enable the delivery of joint plans to support person-centred integrated care. The 2019 review of the BCF concluded that it had been effective in incentivising areas to work more effectively, with over 90% of areas saying that the BCF had improved joint working in their locality consistently since 2017,[footnote 3] and that any attempt to remove or dismantle a pooled budget scheme would be a clear backward step on integration. Moreover, places have voluntarily pooled increasing amounts of money into the BCF year-on-year. In 2020 to 2021, voluntary contributions totalled £3 billion above the nationally mandated minimum, double the figure in 2015 to 2016. This represents significant progress and demonstrates what can be achieved through a framework with an element of national requirements and scope for local partners to go further. Later this year we will set out the policy framework for the BCF from 2023, including how the programme will support implementation of the new approach to integration at place level.
3.30 Despite this, we know that local systems say the arrangements to pool budgets can be complex and there are limitations which prevent the most ambitious models of integration. To address this, we will review the legislation covering pooled budgets (section 75a of the 2006 Act) and publish revised guidance. As indicated above, this will continue to be subject to both NHS and local authority partners agreeing locally what constitutes fair.
3.31 Local organisations must, of course, demonstrate careful consideration of value for money and use available funding in line with their respective accountabilities and delegations. Our vision is that this can, and should, also serve shared objectives and secure wider value. Wherever possible, pooled or aligned budgets should be routine and grow to support more integrated models of service delivery, eventually covering much of funding for health and social care services at place level.
3.32 Some systems are already doing this, and it needs to become the norm along with shared objectives and shared delivery plans to improve outcomes for patients and those who use care services. In line with our wider approach, we will not at this point mandate how this is achieved, but our expectation is that funding should be pooled and aligned around pathways where the case for joined up care is most pressing. As progress accelerates, we will need to carefully consider the implications for existing mechanisms, including the BCF.
3.33 We will also build on the roll-out of personal budgets and personal health budgets across health and social care. The overarching aim is an outcomes-based approach to provide patients and people who draw on social care and support with greater flexibility, choice and control over their care that enables services to be tailored to their particular health and care needs.
3.34 Integrated budgets support integration at an individual level by ensuring support is holistic and can improve a range of health, social care, work and education outcomes for people. Alongside reaffirming our commitment to personal health budgets and personal budgets we will continue to identify opportunities to promote the roll-out by supporting places with guidance and sharing best practice.
Oversight and support
3.35 The Health and Care Bill, if passed into law, places a new duty on the CQC to review ICSs as a whole. This will help inform the public about the quality of health and care in their area and review progress against our aspirations for delivering better, more joined up care across ICSs. These reviews are required to look at how system partners are working together to deliver care. The use of resources will be a running theme in the different reviews and assessments, along with delivery against shared outcomes. The CQC will consider outcomes agreed at place level as part of its assessment of ICSs. CQC will also continue to develop its assessment of individual providers, to ensure their contribution to plans that improve outcomes at Place and ICS level are assessed as part of the overall oversight framework.
3.36 Working with partners, the CQC will consider both the starting position for each ICS and local authority, and the local and national priorities each area needs to manage to help understand how all those responsible for health and care services are working together to deliver safe, high quality and integrated care to the public. Further work is underway to develop the detail and methodology of the CQC reviews. This work will be complementary to existing oversight and support processes (including those used by NHS England to support ICSs, and sector led improvement in local government).
3.37 We will also work with others to ensure that local authorities also receive appropriate support to play their part in place-based arrangements.
To ensure these proposals on accountability, financial frameworks and oversight will be implemented effectively, we will engage with stakeholders and partners, inviting views on the following questions:
- How can the approach to accountability set out in this paper be most effectively implemented? Are there current models in use that meet the criteria set out that could be helpfully shared?
- What will be the key challenges in implementing the approach to accountability set out in the paper? How can they be most effectively met?
- How can we improve sharing of best practice regarding pooled or aligned budgets?
- What guidance would be helpful in enabling local partners to develop simplified and proportionate pooled or aligned budgets?
- What examples are there of effective pooling or alignment of resources to integrate care or work to improve outcomes? What were the critical success factors?
- What features of the current pooling regime (section 75) could be improved and how? Are there any barriers, regulatory or bureaucratic, that would need to be addressed?
4. Digital and data
Summary
Joining up data and information is central to integrating services. All citizens should expect to have access to their own shared care record and for it to cover their health and care journey, with full access, where appropriate, for all the staff they come into contact with.
Health and adult social care providers within an ICS must reach a minimum level of digital maturity, and these providers should be connected to a shared care record. This will ensure each ICS has a functional and single health and adult social care record for each citizen by 2024, with work underway to enable full access for the person, their approved caregivers and care team to view and contribute to. A suite of standards for adult social care, co-designed with the sector, will enable providers across the NHS and adult social care sector to share information. This will begin with the consolidation of existing terminology standards by December 2022. Data to support an understanding of population health, including unmet need and disparities, should be fully shared across NHS and local authority organisations, to allow ‘place boards’ or equivalents, and ICSs to plan, commission and deliver shared outcomes, including public health and prevention services.
Each ICS will implement a population health platform with care coordination functionality that uses joined up data to support planning, proactive population health management and precision public health by 2025.
Digital integration will open up new ways for individuals to access health and adult social care services. There has been rapid expansion of digital channels in primary and secondary care services, but there is more we can do to ensure individuals can choose how they interact with services. By 2022, one million people will be supported by digitally enabled care pathways at home.
4.1 The effective use of data and technology to record and share information, is key to the integration of health and care. It will support citizens to take more control of their health and care. The joined up, real-time data that comes from an integrated health and care system will enable continuous improvement, as well as research into new treatments and support developers and innovators to build solutions that improve health and care.
4.2 Better integrated data and technology systems enable people to take greater control of their own health and care needs and preferences using digital tools to manage their appointments, accessing additional support when they need it and contributing to their record at a time that is convenient to them.
4.3 People will move seamlessly between health and care settings because people and those supporting their health and care, including both professionals and unpaid carers, will be able to see and contribute to their care record and care plans.
4.4 They can be assured that they will not become lost in the gaps between services, either experiencing long delays or with risk factors that should be proactively managed, because data is joined up and everyone who needs it can access it.
4.5 Individuals will use technology to access information and services in more flexible ways, to keep themselves well, and support independence when living with a physical or learning disability, helping to reduce health disparities. They will be confident that health and care staff have their up-to-date information and preferences, regardless of the care setting and won’t have to repeat details unnecessarily and understand, with increased transparency, how the health and care system protects and uses their data.
Using digital and data to integrate care
Digitising: records of health and care delivery to be digital, not paper, everywhere
4.6 While more than 60% of NHS trusts have made good progress into digitisation with 21% now digitally mature (as set out in the What Good Looks Like Framework), and only 10% continuing to rely heavily on paper, the picture is often much more challenging in social care. Only 40% of social care providers have electronic care records, with the rest largely paper based – and this is only improving slowly, at around 3% per year.
4.7 In our adult social care reform white paper, People at the Heart of Care, we committed to at least £150 million of new funding to deliver a programme of digital transformation over the next 3 years. Digitalisation will not only drive up the safety and quality of care, but also has the potential to increase productivity benefits for social care providers, with digital social care records expected to reduce the administrative burden placed on staff.
4.8 While we are making good progress, there is still work to be done to bring all organisations up to the minimum level of maturity as outlined in the What Good Looks Like Framework. This framework will be extended to cover community health services and social care, and a tailored framework will be developed for nurses. We will provide support to enable every health and adult social care provider within ICSs to reach a minimum level of digital maturity.
Connecting: different systems to exchange information
4.9 Data saves lives, the draft data strategy for health and care, sets out a vision for data that moves seamlessly across health and care and has transparency at its core, giving people access to high quality, timely data to help them make choices about their care and improve outcomes. The data strategy sets out when and how information can be accessed and used by individuals, those caring for them and those planning services. A final version of the strategy will be published in early 2022.
4.10 Basic shared care records are now in place in all but one ICS. However, we must ensure that shared care records cover the entirety of a person’s life and include both health and care, which they currently do not. For adult social care, we will ensure that within 6 months of providers having an operational digital social care record in place, they are able to connect to their local Shared Care Record, enabling staff to appropriately access and contribute to the record. We will also reinforce the use of the NHS number universally across social care to support this. Work is also underway to enable citizens to be able to access and contribute to their shared care records, building on successes to date.
4.11 Standards will be key to delivering integrated care. We will establish a suite of standards for adult social care, co-designed with the sector, to enable providers across the NHS and adult social care sector to share information. This will begin by developing a process to consolidate existing social care terminology standards by December 2022. We will develop a roadmap for standards development (April 2022), which will be underpinned by a new end to end process for development).
4.12 We will put in place systems to link and combine data to enable improved direct care and better analytics for population health management. This includes connecting data from every health and adult social care provider to provide a near real-time picture of NHS care, sharing consistent data at ICS, region and national levels to enable transformation of care pathways, and providing insight to all users through user led product design and supporting deployment functions.
4.13 The digital and data transformations outlined in this document provide an opportunity for greater transparency. We will look to introduce mandatory reporting of outcomes, for local places, for citizens at the heart of what we do.
Information governance
4.14 The Health and Social Care Information Governance (IG) Portal provides simplified advice and guidance on information sharing to health and social care providers. This includes an IG Framework for Shared Care Records to support the workforce to have the confidence to share information where appropriate and enable joined up care. This guidance recognises certain roles within the adult social care sector such as registered managers to be ‘health and care professionals’, which ensures that information can be more easily shared across health and social care settings.
4.15 Forthcoming proposals in the Health and Care Bill, if passed into law, will support integration introducing a power to mandate standards for how information is collected and stored, so that information flows through the system in a usable way. This will make sure that when it is accessed or provided (for whatever purpose), it is in a standard form, both readable by and consistently meaningful to the user or recipient). The bill also proposes to create a statutory duty for organisations within the health and care system to share anonymous data.
Transforming: digitally enabled transformation and the funding, skills and time needed to do it well
4.16 In social care we are driving rapid adoption of proven technologies, such as risk stratification tools, and will scale technology such as acoustic monitoring to prevent falls. By March 2024, over 20% of care homes will have acoustic monitoring solutions or equivalent care tech in place.
4.17 Tech has been demonstrated to have a positive impact on the quality and safety of care, including medications management and hydration monitoring to prevent urinary tract infections (UTIs) and benefits to people’s wellbeing such as improved quality of sleep, through enabling more proactive and responsive models of care.
4.18 We continue to improve citizen access to information and services directly through NHS.uk and the NHS App. These products provide access to advice and guidance, individuals with access to their records, the ability to book appointments with their GP, order prescriptions, set preferences for data usage and organ donation, and access their COVID Pass.
Skills and workforce
4.19 NHSX has supported Health Education England to build the next cadre of digital leaders through the NHS Digital Academy. We are addressing the specialist tech skills gap through professionalising the digital profession, bringing in talented tech graduates, increasing the number of apprenticeships offered and harnessing talented entrepreneurial and analytical clinicians through the Clinical Entrepreneur scheme and new fellowships.
4.20 NHS England and NHSX, with partners, have created a 16,000 strong online community of practice (AnalystX) for data professionals and analysts to share knowledge, learning and development, supporting the development of analytical skills for transformation.
4.21 Ipsos MORI, the Institute of Public Care and Skills for Care have supported us with a review of the social care workforce’s current digital skills and future skills needs, as well as the barriers and enablers to the use and effectiveness of digital technology in social care. We will use these insights to develop a comprehensive digital learning offer, as well as targeted leadership support, to build the capability and confidence of social care staff to drive change in their organisations. This offer will complement the wider workforce investment package outlined in our adult social care reform white paper, People at the Heart of Care.
4.22 Well-evidenced digital health technologies can empower patients to manage their own health and help frontline staff to provide high quality care and make best use of their time. The Digital Technology Assessment Criteria for health and social care (DTAC) gives staff, patients and citizens confidence that the digital health tools they use meet our clinical safety, data protection, technical security, interoperability and usability and accessibility standards.
Integrated care systems
4.23 An integrated health and care system requires data to flow seamlessly between staff, citizens and their carers. The insights generated will be used to make decisions more quickly, responsively and safely, proactively tailor services to the needs of populations, enable more personalised care and reduce unnecessary interventions. People will have the tools to stay healthy and independent and drive their own care when they need it and will be able to navigate the system and make the decisions that are best for them.
Population health management
4.24 ICBs are expected to agree a plan for embedding population health management capabilities and ensuring these are supported by the necessary data and digital infrastructure, such as linked data and digital interventions.
4.25 ICSs will use Population Health Management to help deliver personalised and predictive care based on an individual’s risk. The inclusion of wider determinants of health, will be key to identifying and recognising the impact that factors outside of health and social care can have on the outcomes that people achieve. This must include information about people’s living circumstances – for example, homelessness or social isolation. The inclusion and transparency of workforce, operational capacity, and financial data across an ICS can also support better use of scarce resources, and improve productivity.
4.26 Real-time insights from joined-up, aggregated data can support multi-disciplinary working, clinical decision support, waiting list management and make the best use of new diagnostic centres in the community.
4.27 The digital transformation of screening will enable the identification of at-risk groups more accurately and target interventions towards them appropriately.
ICS first
4.28 We will take an ‘ICS first’ approach. This means encouraging organisations within an ICS to use the same digital systems, making it easier for them to interact and share information and providing care teams working across the same individual’s pathway with accurate and timely data. Where necessary, we will intervene with ICSs and vendors – including by setting conditions of funding, producing guidance, providing support, encouraging disruption and leveraging other allies. This will allow ICSs to provide the best possible support to the places they contain, and the leaders of place-based arrangements.
4.29 Every ICS will need to ensure that all constituent organisations have a base level of digital capabilities and are connected to a shared care record by 2024 enabling individuals, their approved caregivers and their care team to view and contribute to the record.
4.30 ICSs have been asked to identify digital priorities to support the delivery of out-of-hospital models of care through the development of system digital investment plans, ensuring community health services providers are supported to develop robust digital strategies to support improvements in care delivery. Where appropriate, digital investment should be purchased and deployed at ICS level.
4.31 To achieve 80% adoption of digital social care records among CQC-registered social care providers by March 2024, ICSs must work with partners to drive adoption.
Rapid adoption
4.32 We will maintain the pace of adoption seen through the pandemic, when – at extraordinary speed – consultations moved online, clinicians and other staff worked from home, people were monitored remotely, including in care homes, and information flowed more effectively between care settings. This has changed the mindset of many staff and citizens about digitally enabled health and care – they do not want to go back to old ways of doing things.
4.33 We have a real opportunity to build on this progress and to truly integrate health and care services. To do this, we need to bring everyone on this journey, one which will ultimately transform how care is delivered, improving both safety and experience. We will do this by building transparency and trust through ongoing dialogue with citizens and developing our approach to Information Governance, giving confidence to the workforce and leveraging the maximum benefit from information. We will ensure we are inclusive, recognising that the use of digital services can create opportunities for people who struggle to access traditional services, as well as barriers for others, but should always be part of a multi-channel offering that reflect the preferences and needs of individuals. Digital investment plans should be finalised by June 2022 which include the steps being taken locally to support digital inclusion.
4.34 For adoption to be rapid, the frontline needs to be confident when recommending digital interventions, and people who use services need to be aware of and be able to access new products. There’s a lot more we can do to increase confidence.
4.35 The NHS App will offer a personalised experience for users and encourage them to engage in tailored preventative activity (screening, immunisations and vaccinations, health checks etc). We will help people, their families, unpaid carers and care providers to understand what technologies are effective for helping maintain independence and quality of life, such as smart home technologies that give medication reminders, or sensor-based tech that provides alerts if someone has had a fall.
4.36 Led by clinicians, and in partnership with NHS England and Improvement, we will develop new pathways for musculoskeletal, dermatology, ophthalmology, perioperative and cardiovascular pathways used by approximately 20 million people
4.37 Clinical decision support tools, within an electronic health record, will improve clinical outcomes and reduce unwarranted variation. Finally, approaches to regulation of health and care technologies must be proportionate and support the needs and priorities of the health and care system – such as virtual wards and reducing health disparities.
5. The health and care workforce and carers
Summary
This chapter sets out proposals to ensure that staff working in health and care settings are supported to provide integrated services focused on the needs of people by:
- strengthening the role of workforce planning at ICS and local levels
- reviewing the regulatory and statutory requirements that prevent the flexible deployment of health and social care staff across sectors
- increasing the number of appropriate clinical interventions that social care workers can safely carry out by developing a national delegation framework of healthcare interventions
- exploring the introduction of an Integrated Skills Passport to enable health and care staff to transfer their skills and knowledge between the NHS, public health and social care
- increasing the number of learning experiences in social care, including health undergraduate degree programmes and for those undertaking apprenticeships
- exploring opportunities for cross-sector training and learning, joint roles for ASC and health staff in both regulated and unregulated roles
- promoting the importance of the roles of link workers, care navigators and care coordinators to ensure consistent access to these roles across the country
Our proposals will strengthen those laid out in the workforce chapter of our adult social care reform white paper, People at the Heart of Care, which are:
- a knowledge and skills framework, careers pathways and linked investment in learning and development to support progression for care workers and registered managers
- funding for Care Certificates, alongside significant work to create a delivery standard recognised across the sector. This will improve portability, so that care workers do not need to repeat the Care Certificate when moving roles
- continuous professional development budgets for registered nurses, nursing associates, occupational therapists and other allied health professionals
- investment in social worker training routes
- Initiatives to provide wellbeing and mental health support, and to improve access to occupational health
- a new digital hub for the workforce to access support, information and advice, and a portable record of learning and development
- new policies to identify and support best recruitment practices locally
- exploration of new national and local policies to ensure consistent implementation of the above, as well as higher standards of employment and care provided
The importance of workforce integration
5.1 It is through the staff delivering health and care that the ambitions of this paper will be delivered. People’s interactions with health and social care services are through the workforce and, often, no single individual or team can provide all the care and support that a person needs. Joined-up services are delivered effectively when staff work together within and across organisations.
5.2 A workforce with a shared ambition for health, wellbeing and independence can improve the delivery of shared outcomes. Integrated services can only be delivered by a capable, confident, collaborative health and care workforce, which works together to wrap care and support around individuals, and which feels valued for the work they do.
An integrated workforce is where:
- staff work as part of a team to plan and deliver services based on the needs and wishes of the individual, and that takes into consideration the individual’s wider family context
- staff numbers and skills across teams and organisations are planned to meet the needs of their local population
- staff feel confident in their roles and work together in the person’s interests wherever they are employed
- staff understand what all organisations contribute, including the value of unpaid carers and wider community, and have clear processes, lines of communication and the technology and data needed for working with others
- if multiple staff are involved in delivery of services to support a person’s care, they collectively have the skills and capacity to deliver the best person-centred care
- staff are empowered to use their skills to progress their careers across the health and care family
5.3 The response to the COVID-19 pandemic has shown what can be achieved when the workforce comes together to safeguard and promote health and wellbeing by breaking down boundaries in the system. We want to celebrate this approach by making it routine rather than something that only happens in a crisis, with barriers to collaboration removed and the workforce equipped to work across sectors.
5.4 Staff across health and social care already strive to provide person-centred care. Too often, however, structural and/or financial barriers get in the way of effective joint working. This is true within the health and social care sectors, as well as between them. The landscape is even more complex when we factor in public health, community health services, education, housing and homelessness provision, the voluntary, and community health services, and unpaid carers, all of which play a key role in providing joined-up care, support and treatment.
5.5 The new structures being put in place at a national and local level provide an opportunity to overcome these barriers. Through the Health and Care Bill, we are creating a legislative framework for partnership working which will bring the NHS, local government and social care closer together to help ensure everyone receives outstanding, person-centred, outcome-focused services they need. The workforce will be a key part of strategies and plans developed by ICBs and ICPs.
5.6 This government is committed to supporting the NHS, public health and social care workforces, with a focus on workforce capacity and capability. For example, we are delivering 50,000 more nurses in the NHS. Our adult social care reform white paper, People at the Heart of Care, sets out an ambitious vision to transform the workforce, with an unprecedented investment of at least £500 million. This will directly address some of the barriers to integration by improving learning and development and providing more opportunities for progression within adult social care.
Tackling the barriers to workforce integration
5.7 At a national level we can further facilitate workforce integration by removing barriers to collaborative planning and working. We will review regulatory and statutory requirements that prevent the flexible deployment of health and social care staff across sectors. To make integration a reality, places must consider integration in a way that meets their local needs. The role of central government is to facilitate and support that, ensuring the right structures, accountability and leadership is in place to enable workforce integration locally.
Workforce planning
5.8 There are currently limited fora to develop shared approaches to workforce planning, and a lack of clarity about which national and local bodies are responsible for what. Planning is often carried out in isolation, meaning that social care providers and local authorities frequently compete with the NHS, or each other, to attract and retain staff. This siloed approach can also result in a lack of alignment with broader health services commissioned by local authorities, those delivering support to children and young people, unpaid carers, housing, and the voluntary sector.
5.9 To improve workforce planning, in July 2021, the Department commissioned Health Education England (HEE) to work with partners to review long-term strategic trends for the workforce. For the first time, regulated adult social care professions will be included in this framework, which will take a 15-year forward view to guide planning, education and training for the workforce. The framework will provide the information needed for ICBs to fulfil their role on shared workforce planning across health and social care services and will support localities to plan and improve services to meet the needs of people now and in the future.
5.10 Workforce planning is kept under close review by DHSC and other bodies. The Health and Care Bill will propose a that report that will set out the role and responsibility of each of the bodies (at national, regional and local level) in the system responsible for workforce planning in the NHS in England for the first time, to increase accountability and transparency and provide assurance that the system is making this issue a priority. This workforce accountability report will cover the whole of the NHS including primary, secondary, and community health services including where sections of the workforce are shared between health, public health and social care – for example, registered nurses.
5.11 Adult social care is a largely private sector market and core responsibilities of workforce planning and market shaping are devolved to local authorities who are accountable to their local populations for management and delivery under the Care Act. As set out in the adult social care reform white paper, People at the Heart of Care, we recognise the ongoing hard work by providers and local authorities – working with system partners including the NHS – to address difficult workforce capacity issues. We will continue to work closely with local authorities and care providers to monitor workforce pressures, including identifying whether further action may be required.
5.12 We will further improve integrated workforce planning at place level by:
- working with local government and NHS England to strengthen guidance for systems and increase co-production with social care stakeholders, for example, by gathering intelligence about the experience and aspirations of people who use care and support services and have clear approaches to using these insights to inform decision-making and quality governance. Government will incorporate this into the development of guidance for ICPs, so that all components of an ICS are clear on the role they can play in integrated workforce planning across the whole health and care system
- encouraging the expansion of local feedback fora, building on good practice in a number of regions that have led to closer collaboration between NHS regional teams, local government, and other stakeholders such as Skills for Care representatives
- working closely with NHSE and system leaders across the comprehensive health and care system to support the development of ICSs’ ‘people operating model’ and to support places develop a ‘one workforce’ approach
- considering what further national action needs to be taken following the publication of the long-term strategic framework later this year, including what more is needed to support workforce planning for the unregulated adult social care workforce
Working within the devolved Greater Manchester Health and Social Care Partnership, Bury have created a strategic commissioning board which has equal representation from members of Bury Council and the borough’s clinical commissioning group (CCG). The board brings together the governance of health and social care, allocation of shared resources including pooled budgets, and strategic commissioning across adult social care and health.
Crucially, the board brings together the whole of Bury’s cabinet with the CCG, including housing, public health, drug and alcohol services, and children’s social care, allowing for joint workforce planning and commissioning of services to meet needs in a holistic way. This is reflected at a neighbourhood level, with integrated teams reporting to a single line manager, improving people’s direct experience of health and social care.
Learning and development
5.13 Initial training and ongoing learning and development opportunities are an excellent opportunity to prepare people for partnership-working with other teams. Although some health and social care dual qualifications are available, there is disparity in access to, and quality of, learning and development opportunities for staff in adult social care compared to the NHS, which can act as a disincentive to enter or stay in the sector and can create barriers to partnership working.
5.14 Training and learning together can play a key role in enabling an integrated workforce, with staff from different sectors, and teams within a sector, learning together and gaining an understanding of the roles of others they work with. We will:
- work with national and local partners to identify ways to improve initial training and learning for staff in roles at the interface between health and social care, to ensure they have the skills and knowledge needed to work collaboratively across sectors
- identify opportunities for joint continuous professional development across sectors. This could involve joint training on topics such as mental capacity, frailty, and strengths-based and assets-based practice to help staff develop the understanding needed for team working
- move towards a more collective approach to promoting careers in health and social care: the view of health and social care as an integrated system with equal value should be reinforced as people make decisions around whether to pursue a career in health and social care, including career changers
North Tyneside Clinical Commissioning Group is working in partnership with 4 large care home providers to appoint 7 advanced care practitioners (ACP) nurse trainees as part of the Health Education England ACP apprentice scheme. This is introducing a new way of working with care home providers to enhance the health of residents. It is also supporting apprenticeships with a model that promotes career progression and staff development for care home staff.
Progression and movement within and between sectors
5.15 There are diverse, rewarding opportunities available in all parts of health and social care, but there are barriers to people moving across organisational boundaries. Even where roles have similar skills and responsibilities, there is often not a ‘healthy’ flow of workers between health and social care roles. This is, in part, driven by a lack of cross-sector experience built into training; disparities in career progression, with adult social care in particular viewed as lacking opportunities compared to the NHS, and regulatory barriers.
5.16 We want to make it easier for the workforce to move between health and social care. Within primary care, roles are increasingly being recruited through rotational and joint employment models. We want to build on this approach, to encourage movement of staff within and between sectors, to help build knowledge, relationships, and experience of different settings.
5.17 The adult social care reform white paper, People at the Heart of Care, sets out how we will improve career pathways and progression within adult social care and support local areas to recruit people with the right skills and values to meet care needs now and in the future. We will provide funding to support local authorities to prepare their local markets for reform, including by moving towards paying providers a fair rate for care that reflects local costs, including workforce, where appropriate. In addition to this, we will:
- work with stakeholders to develop and test joint roles in health and social care, for example roles which support integrated care planning, which coordinate across sectors, or which allow people to work flexibly across settings
- consider the introduction of an Integrated Skills Passport to enable staff to transfer skills and knowledge between the NHS, public health and social care. NHSEI and DHSC are developing skills passports to allow health and care workers to demonstrate their knowledge and skills so that employers can easily access this information when a worker moves between organisations
- increase the number of learning experiences in social care to understand perspectives across sectors, enhance future team working and create a sense of a joint health and social care career structure. This will include health undergraduate degree programmes and those undertaking apprenticeships. Our long-term ambition is for all health undergraduates to experience adult social care, to understand perspectives across sectors, enhance future team working, and create a sense of a joint health and social care career structure. To begin with, we will work with the Council of Deans to increase the number of trainee nurses who undertake a placement in adult social care
5.18 We will also remove barriers that prevent particular professions working across settings and make the best use of each person’s skills. We will:
- promote the importance of the roles of link workers, named key worker and care navigator roles[footnote 4] as crucial enablers of integrated care provision. Current care navigator roles exist in multidisciplinary teams, or voluntary services, and are responsible for delivering assessments, advice, signposting, and coordination. Care managing in this way offers ways of sensibly sharing work and responsibility, helping to relieve front-line clinician pressures and improves overall quality of care for patients.[footnote 5] Building on good practice from across the UK and internationally,[footnote 6] the roles support people at the interfaces between health and care and we will ensure that access to these types of roles are consistent across the country
- explore appropriate interventions that can be safely delegated or transferred between the sectors
- consider developing a national delegation framework of appropriate clinical interventions to increase the range of appropriate clinical interventions undertaken in care settings while ensuring safe, appropriate and confident practice and exploring what additional support care workers need. Our adult social care reform white paper, People at the Heart of Care, sets out plans for establishing a foundation for the future registration of social care staff in a way that benefits staff and care providers alike, which we intend to explore further. We want to build confidence in registered professionals delegating these interventions to social care workers
- commission research into how occupational therapists working in community health services and social care can work more effectively to complement one another
- create opportunities for social housing support and homelessness workers, often supporting people with care and support needs, to progress into adult social care, public health and health roles. This will include taking forward recommendations from HEE’s scoping study with the Voluntary, Community and Social Enterprise Health and Wellbeing Alliance
- make the best use of the skills of pharmacy professionals by consulting on regulatory barriers, improving placement opportunities, and delivering the Pharmacy Integration Programme
Volunteering programmes significantly improve the experience of users of care and enable a greater level of support for staff. The pandemic saw excellent examples of the support they can offer, for example, the NHS Volunteer Responders Programme successfully supported thousands of people who were shielding in their communities. Building on the success of this programme, DHSC and NHSEI have been working together on how to build volunteering capacity for local health and social care systems. This type of joint action can strengthen community ties and improve life outcomes for health and social care users. The creation of ‘blended’ enhanced home care roles that take on elements of some interventions previously carried out by district nurses has been piloted in Tameside (Greater Manchester) with plans to scale up in other Greater Manchester localities.
Place-based workforce integration
5.19 To deliver shared outcomes, local leaders will need to consider how the health and care workforce in the area can be deployed in the most effective way. This should prevent duplication across health and care, consider the impacts of one sector on the other, and ensure that citizens contact with members of both workforces is coherent and coordinated.
5.20 While national action can foster the conditions for workforce integration, to make this a reality, places must implement integration in a way that meets their needs. Changes in the Health and Care Bill will embed and speed up integration locally, with flexibility for areas to determine which models of integration will work best at place. For example, ICBs will have the flexibility to determine governance arrangements in their area – including the ability to create committees and delegate functions to them. This would allow systems to create local ‘place’-based committees to plan care where appropriate. Every area should strive to achieve the greatest level of integration possible with appropriate governance arrangements for this at place level.
5.21 For the health, social care and public health workforce, ICSs will be a lynchpin between national organisations and places, providing a key forum for planning and direction setting. But it is at a more local level that the workforce makes integration a reality – and at an individual level where people experience the benefits of an integrated workforce. Local leaders will need to think about what workforce integration looks like in their area, the conditions that are needed, the practical steps required, and who needs to be involved in shaping this.
In The Principles of Workforce Integration, Skills for Care has identified 6 principles to aid areas in their development of workforce plans and workforce development in an integrated way:
- successful workforce integration focuses on better outcomes for people with care and support needs
- workforce integration involves the whole system
- to achieve genuine workforce integration, people need to acknowledge and overcome resistance to change and transition. There needs to be an acknowledgement of how integration will affect people’s roles and professional identities
- a confident, engaged, motivated, knowledgeable and properly skilled workforce supporting active and engaged communities is at the heart of workforce integration
- process matters – it gives messages, creates opportunities, and demonstrates the way in which the workforce is valued
- successful workforce integration creates new relationships, networks and ways of working. Integrated workforce commissioning strategies give each of these attention, creating the circumstances in which all can thrive
5.22 Our proposals in the leadership, shared outcomes and accountability chapters will empower local leaders to embed these principles. Places must build a culture that supports integrated service delivery, sets a shared vision, develops a common language that truly covers the whole workforce, and engenders a culture of partnership. Involving and empowering the workforce directly will be crucial, for example through shared decision councils, as recommended in The Principles of Workforce Integration, adopting local ‘integration champions’ or supporting local communities to build the partnerships and plans to embed housing as part of the local health and care system, as set out in our adult social care reform white paper, People at the Heart of Care.
5.23 There are a variety of models being implemented at place level. The NHS Long Term Plan, for example, includes a commitment to expand community multidisciplinary teams as a means to integrate primary and community health services, and many places have started to use multidisciplinary teams across other parts of the workforce. Other areas have found that physical co-location of staff has had an impact, or that a nominated key worker model is useful to provide a single point of contact for a person receiving care. The family hub model, which emphasises building strong connections between services and families, and on building relationships, is an important way of bringing together.[footnote 7]
Health and care leaders in Portsmouth – including Portsmouth City Council, NHS Portsmouth Clinical Commissioning Group, Solent NHS Trust, Portsmouth Hospitals NHS Trust, Portsmouth GP Alliance and local voluntary sector organisations – developed a blueprint setting out their ambition for integrated services. This Portsmouth Blueprint had at its heart the principle that first comes the person and family being cared for, then comes the team, and only after that comes the organisation. Partners have made extensive use of co-location to bring teams together, with the chief operating officer of Solent NHS Trust (which provides community and mental health services across Portsmouth, Southampton, Isle of Wight and Hampshire) being first to work from within the city council’s headquarters. The civic offices now accommodate community nursing and social care, the learning disability service, health visiting, 0 to 19 young people’s services, and school nursing for the centre and south of the city. As part of this, they will explore the role that family hubs can play in bringing together services in the community to support families.
Greater Manchester – inclusive workforce
Greater Manchester Combined Authority and Greater Manchester Health and Social Care Partnership co-invested in the Working Well Early Help programme, a health-led employment support programme for residents in all 10 local authority areas in Greater Manchester. It supports individuals with a health condition or disability who have recently become unemployed or taken medical leave, to return to sustained employment. The programme is built upon early intervention through personalised and holistic support focused on addressing the barriers to employment and is integrated with local services, including health and skills services. The partnership and governance are set up through key partners including Local leads from local authorities and GP leads in each delivery area. Local leads are designated members of staff from each of the local authorities who have a responsibility to oversee the performance of Working Well contracts at a borough level and are often from the Work and Skills team. Recent qualitative impact assessment indicates that the support has led to 53% positive health and wellbeing outcomes and 39% positive employment outcomes. Working Well Early Help is part of the wider family of Working Well programmes in Greater Manchester. Since its inception in 2014, Working Well has achieved employment outcomes for over 15,200 Greater Manchester residents. Due to its successes, Greater Manchester has also successfully negotiated for the opportunity to co-design, procure and deliver a localised version of the new Work and Health Programme which will support nearly 23,000 individuals across Greater Manchester until 2024.
Cornwall – Healthy Cornwall
Commercial fishing is known to be a physically and mentally straining occupation. The workforce is predominantly male and often less engaging with healthcare services for various reasons such as previous bad experience or working during normal assessment hours. Therefore, Healthy Cornwall (Cornwall Council), together with the GetSeaFit programme, co-ordinated and commissioned healthcare services and brought them to the quayside. The overall aim was to influence the NHS and local authority public health teams at a local level by highlighting the health needs of this vulnerable section of society, with traditionally a history of poor access to health and preventative services, whose work and lifestyle put them at risk of developing chronic and serious health issues later in life. Furthermore, it was envisaged that the wider long-term impact would be social change among fishing communities, with better physical and mental health which would lead to sustained hours at sea, less financial hardship, reduced deprivation and an improved home life through greater financial stability. Activities included conducting quayside health checks, holding health and wellbeing events and having regular informal conversations about health and wellbeing to raise awareness amongst this workforce. The GetSeaFit programme was a joint 2-year initiative, with a time extension of 7 months, run by the Fishermen’s Mission and the Seafarers Hospital Society but also partners such as local GPs, opticians, dentists, health professionals and other charitable organisations. The programme has been successful and representatives from Healthy Cornwall are now trusted members of this community and fishermen and family members who received support are benefitting from better health and are encouraging their peers and fellow crew members to seek advice or treatment. Healthy Cornwall also modernised last September to an operating model that is much more focused on vulnerable groups with increased local initiatives.
Health and social care volunteering
National and local volunteering programmes present great opportunities to build capacity in local systems, with volunteers providing support in a range of settings to assist staff and users of care. The pandemic saw excellent examples of the support they can offer, for example, the NHS Volunteer Responders Programme successfully supported thousands of people who were shielding in their communities. Building on the success of this programme, DHSC and NHSEI have been working together on a scheme to build volunteering capacity for local health and social care systems. This type of joint action can strengthen community ties and improve life outcomes for health and social care users.
Workforce: conclusion
5.24 Integration will be delivered by a workforce equipped with the skills and opportunities to move across the health, public health and social care family, supported by holistic workforce planning to ensure there are the right people to deliver the best outcomes for people and populations. Over the coming years we will work with national and local partners to achieve this vision. Alongside concerted action at a place level, this package of initiatives will improve integration between the health, public health and social care workforce, leading to improved outcomes, and better person-centred care and population health outcomes.
As we begin the implementation of these policies, we are seeking views from stakeholders and partners on the following questions:
- What are the key opportunities and challenges for ensuring that we maximise the role of the health and care workforce in providing integrated care?
- How can we ensure the health and social care workforces are able to work together in different settings and as effectively as possible?
- Are there particular roles in the health or adult social care workforce that you feel would most benefit from increased knowledge of multi-agency working and the roles of other professionals?
- What models of joint continuous professional development across health and social care have you seen work well? What are the barriers you have faced to increasing opportunities for joint training?
- What types of role do you feel would most benefit from being more interchangeable across health and social care? What models do you feel already work well?
6. Conclusion: impact on people and next steps
At the beginning of this document, you met Tom and Maureen, Bunmi, Kwame, Madeleine Mandeep and Richard. The policies proposed in this paper will have a material impact on their lives.
Case studies
Tom and Maureen
Tom and Maureen have some digital skills as they use an iPad to keep in touch with their children, grandchildren and great grandchildren. With some support from their children they sign up to the NHS App where they can access their health and care records, book appointments and order repeat medication to be delivered to their door. Tom has given Dan and Sarah access so they can see test results, the outcome of conversations with his care team and can converse with the GP electronically.
To help Tom manage his diabetes more effectively alongside his dementia, he is given a glucose monitoring device so that his blood sugar levels are automatically recorded using a mobile app. This information can help Maureen see if they are high or low and where he might need adjustments to his insulin or diet. This automatically uploads data to his record so that Tom’s clinical team can see how well he is managing his diabetes and offer the right kind of interventions.
These changes mean that Tom’s diabetes is stable again and he and Maureen, as well as their children, have the information they need to empower them to manage his health at home and keep him independent at home for longer.
Tom was admitted to hospital where he received great care, however due to COVID-19 restrictions in the area, Dan and Sarah were not able to visit Tom. They supported their mother and discussed with medical professionals what would be best for their elderly parents going forward. Despite Maureen feeling extremely overwhelmed when a care assessment was carried out, there was much discussion of what could be done locally from their own home.
An assessment for dementia was completed in the hospital and his records were shared with his GP and local care services to ensure that they did not have to be repeated. Tom and his family were offered help with his diagnosis and his community mental health team were involved from the start.
After several weeks in hospital, Tom was discharged, and the detailed package of care was delivered. Dan and Sarah frequently visited and were kept informed by the local care team as to how their parents’ conditions were and how they were being cared for personally.
Tom, Maureen and family are able to hold a meeting with his care worker to discuss the recent trips to A&E and the impact that is having on his dementia and wellbeing.
Care workers and nurses who care for Tom locally have recently taken part in shared learning days so that teams who support Tom at home have good working relationships and open communication. They were able to jointly work on a collaborative care plan with Tom and family to agree how his support needs have changed and develop and implement action plans.
The diabetes team encouraged Tom’s care workers to build their competency in insulin management, and as a result they were able to delegate this intervention using the national framework so the care workers could provide insulin management for Tom. This helped reduce unnecessary interactions with multiple staff so Tom is not distressed due to his dementia.
These improvements in working across specialties mean that Tom is better able to manage his diabetes at home, and the family have a clearer picture of how his overall care is being managed.
Bunmi
A monitoring system is installed in Bunmi’s home, which checks for changes in patterns of use of several connected home devices, including a kettle, a fridge, a bed mat and light switches in her bedroom and bathroom. Bunmi has allowed for this information to be recorded in her longitudinal health and care record.
As Bunmi’s mobility deteriorates the system noticed that she was moving around her home a lot less than usual and sent an alert to the warden to check on Bunmi. On arrival to Bunmi’s home, the warden used his smartphone to record some basic observations. These suggested a worsening of her conditions and were sent to Bunmi’s multidisciplinary primary care team. The duty member of the multidisciplinary team reviewed Bunmi’s longitudinal health and care record and care plan which is stored securely in the cloud. A clinician then visited Bunmi at home to prescribe medication which was delivered to her within 2 hours. The clinician also admitted Bunmi to the ‘hospital at home’ service, which monitors and supports her over the next few days without needing to admit her to hospital. To help Bunmi with her day-to-day life, the social care representative of the multidisciplinary team will use the system to book carer visits to help with shopping and laundry while Bunmi is unwell and recovering.
These changes mean that Bunmi has support for the management of her long-term conditions, allowing her to live well at home for longer. Bunmi and her multidisciplinary team have the means to identify when she needs additional support, and she is now feeling more confident to resume her day-to-day activities that make her happy.
Kwame
The lack of join up between the various services Kwame was using meant that there was no co-ordination from one provider to the other and Kwame was then caught up in a system where he could not receive the appropriate help he required.
A multi-disciplinary team (MDT) identified a new placement for Kwame, with options including segregated living arrangements being replicated in the community. Meeting Kwame’s requirements was challenging for several established providers but as Kwame was transitioning to adult services (16+), the option of adapting a property to become his long-term home was explored. Kwame was referred to a micro provider which runs small supports programmes using innovative individualised care. Placing Kwame at the centre of every decision they made, they invested time to get to know him, gaining his trust before he re-joined his local community.
After 3 months, many physical barriers preventing closer contact began to be removed. Kwame could now take excursions, started contacting his extended family, and his education was reinstated through digital platforms. Kwame applied for funds to buy and adapt a property and moved into his new home in the summer of 2020.
Madeleine
For Madeleine the COVID-19 pandemic has highlighted how important good collaboration between the statutory sector and voluntary sector is as she was unable to get to any vaccination centre or carry out any tests. Once the situation had been explained to her GP surgery, they responded with at home visits. During one of the visits, the staff who had visited Madeleine picked up on how she has been affected by loneliness and how this had taken a toll on her wellbeing. She was recommended to the well-being team who signed her onto an ongoing well-being programme to tackle her loneliness. She was also put in touch with local volunteers who were able to help her with her shopping and other basic services in the community.
This local collaboration meant that Madeleine was able to access various basic services in her community that made her life more comfortable.
Mandeep
After contacting a charity that Mandeep had seen on the side of a bus, Mandeep went to see a GP who referred him to a crisis centre and provided him with self-care techniques to help manage his mental health problems. He was also referred to specialist help that would help Mandeep manage his diabetes.
At the crisis centre, Mandeep was able to work with social workers, care coordinators, community mental health and employment support. It was the first time he felt cared for and listened too. Through this engagement, Mandeep had continuity of support with people he trusted and this opportunity to gain his independence and gain practical life skills that will help Mandeep get and maintain a job. He secured a more suitable housing arrangement.
Mandeep is more engaged than ever before in improving his health. He now has prescriptions to support his nutrition and his mental health has been far more stable. He is actively taking part in conversations about his future and has better understanding of his support needs. As a result, his personal care has improved greatly.
Richard
Richard was able to be discharged earlier than usual because he moved to a ‘step down’ bed where clinical teams and social workers helped him get back on his feet and get used to living life in the local community again. The community psychiatric nurse helped him manage his medicines, and social care and support workers helped him learn how to cook some recipes. The lead social worker supported Richard in applying for PIP payments and getting a new tenancy agreement sorted with the housing officers so he could move back home. While he was in the step down placement the team learned that Richard was a massive Tina Turner fan!
Richard was able to move home eventually, with home adaptations completed and a joint NHS and social care discharge package of support to keep helping him manage daily activities such as shopping and taking his medicines. The package also included a small ‘personalisation fund’ with which Richard chose to buy a few essential items for his kitchen, as well as a cheap last-minute ticket deal to the Tina Turner musical, which was one of his long-standing personal life goals. Richard said that it was an experience he would never forget and going out to the theatre helped him feel valued as a person living in society again – it was something he had never imagined he would be able to do when he spent years living in psychiatric units. While his community health and social care package now costs slightly more than it did before, he has thrived and lived well at home and the costs are negligible compared to the NHS costs of repeat cycle of admissions.
Next steps
6.1 To provide everyone with the person-centred care they need, we will:
- on shared outcomes, consult stakeholders and set out a framework with a concise number of national priorities and approach for developing additional local shared outcomes, by spring 2023
- review alignment with other priority setting exercises and outcomes frameworks across health and social care system and those related to local government delivery
- ensure implementation of shared outcomes will begin from April 2023
- on leadership, accountability and oversight, set an expectation that by spring 2023, all places should adopt a model of accountability and provide clear responsibilities for decision making including over how services should be shaped to best meet the needs of people in their local area
- review section 75 of the 2006 Act which underpins pooled budgets, to simplify and update the regulations
- work with partners to develop guidance for local authorities and the NHS to support going further and faster on financial alignment and pooling.
- publish guidance on the scope of pooled budgets spring 2023
- work with the CQC and others to ensure the inspection and regulation regime supports and promotes the new shared outcomes and accountability arrangements at Place
- develop a national leadership programme, addressing the skills required to deliver effective system transformation and place-based partnerships, subject to the outcomes of the upcoming leadership review
- publish a final version of the Data Strategy for Health and Care will be published (winter 2021 to 2022)
- ensure every health and adult social care provider within an ICS to reaches a minimum level of digital maturity
- ensure all professionals have access to a functionally single health and adult social care record for each citizen (by 2024) with work underway to put these in the hands of citizens to view and contribute to
- ensure each ICS will implement a population health platform with care coordination functionality, that uses joined up data to support planning, proactive population health management and precision public health (by 2025)
- develop a standards roadmap (2022) and co-designed suite of standards for adult social care (autumn 2023)
- ensure 1 million people to be supported by digitally enabled care at home (by 2022)
- on workforce, strengthen the role of workforce planning at ICS and place levels
- review barriers (including regulatory and statutory) to flexible movement and deployment of health and care staff at place level
- develop a national delegation framework of appropriate clinical interventions to be used in care settings
- increase the number of clinical practice placements in social care during training for other health professionals
- improve opportunities for cross-sector training and joint roles for ASC and NHS staff in both regulated and unregulated roles
- appoint a set of front-runner areas in spring 2023. These will trial the outcomes, accountability, regulatory and financial reforms discussed in this document
Questions for implementation
6.2 The policies outlined in this document build on the proposals in the Health and Care Bill and provides further indications of how we expect local organisations to make progress in integrating health and care, while also setting out some of the support we will provide. We are keen to learn and improve our understanding of what works as we begin the effective implementation of these proposals. To that end, we would like to invite views on a number of key issues to support progress towards implementation. As part of the engagement with stakeholders which we intend to start shortly (referred to above). We will therefore engage stakeholders across the sector with a view to answering the following questions:
Outcomes
(i) What role can outcomes play in forging common purpose between partners within a place or system – and can you point to examples of this?
(ii) How can we get the balance right between local and national in setting outcomes and priorities?
(iii) How can we most effectively balance the need for information about progress (often addressed through process indicators) with a resolute focus on achieving outcomes (where data can lag)?
(iv) How should outcomes be best articulated to encourage closer working between the NHS and local government?
(v) How can partners most effectively balance shared goals or outcomes with those that are specific to one or the other partner – are there examples, and how can those who are setting national and local goals be most helpful?
Financial
(vi) How can we improve sharing of best practice regarding pooled or aligned budgets?
(vii) What guidance would be helpful in enabling local partners to develop simplified and proportionate pooled or aligned budgets?
(viii) What examples are there of effective pooling or alignment of resources to integrate care or work to improve outcomes? What were the critical success factors?
(ix) What features of the current pooling regime (section 75) could be improved and how? Are there any barriers, regulatory or bureaucratic that would need to be addressed?
Accountability
(x) How can the approach to accountability set out in this paper be most effectively implemented? Are there current models in use that meet the criteria set out that could be helpfully shared?
(xi) What will be the key challenges in implementing the approach to accountability set out in the paper? How can they be most effectively met?
Workforce
(xii) What are the key opportunities and challenges for ensuring that we maximise the role of the health and care workforce in providing integrated care?
(xiii) How can we ensure the health and social care workforces are able to work together in different settings and as effectively as possible?
(xiv) Are there particular roles in the health or adult social care workforce that you feel would most benefit from increased knowledge of multi-agency working and the roles of other professionals?
(xv) What models of joint continuous professional development across health and social care have you seen work well? What are the barriers you have faced to increasing opportunities for joint training?
(xvi) What types of role do you feel would most benefit from being more interchangeable across health and social care? What models do you feel already work well?
Digital and data
(xvii) What are the key challenges and opportunities in taking forward the policies set out in this paper, and what examples of advanced or good practice are there that could help?
(xviii) How do we best ensure that all individuals and groups can take advantage of improvements in technology and how do we support this?
-
In this document we refer to ‘integrated care systems’ or ICSs – an ICS is made up of both the integrated care board (ICB) and the integrated care partnership (ICP) that are set out in the Health and Care Bill. The term ‘ICS’ is also used to refer to the geographical area covered by the system. ↩ ↩2
-
The health and social care interface (National Audit Office). ↩
-
Care Navigation: A Competency Framework (Health Education England). ↩
-
General Practice Forward View (NHS England). ↩
-
What can England learn from the long-term care system in Japan? (Nuffield Trust). ↩
