Health matters: stopping smoking – what works?
Updated 17 December 2019
Summary
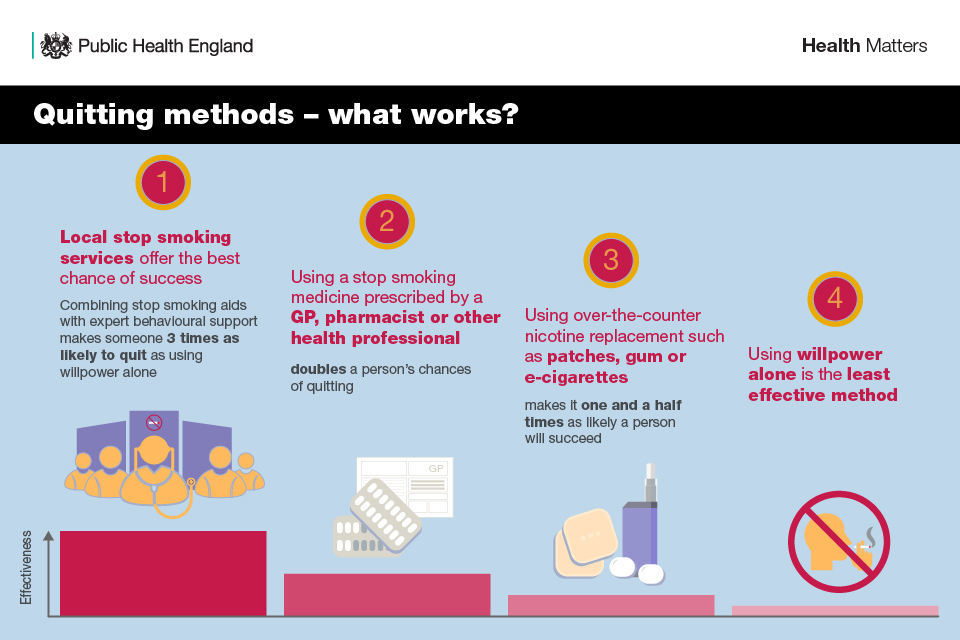
This edition of Health Matters focuses on the range of smoking quitting routes that are available and the evidence for their effectiveness. Two-thirds of smokers say they want to quit, however, most try to do so unaided, which is the least effective method. Smokers who get the right support are 3 times as likely to quit successfully.
Scale of the problem
Smoking is the leading cause of preventable illness and premature death in England, with about half of all lifelong smokers dying prematurely, losing on average around 10 years of life. In 2016 alone, there were around 78,000 deaths attributable to smoking, representing 16% of all deaths across the UK.
The adult smoking rate in England continues to decline year on year and is now at a record low. In 2017, 14.9% of people in England aged 18 years and above smoked, accounting for 6.1 million people. If this trend continues, it will reduce to between 8.5% and 11.7% by 2023. PHE is calling for the NHS long-term plan to commit to achieving a smokefree society by 2030 with an adult prevalence of 5% or less.
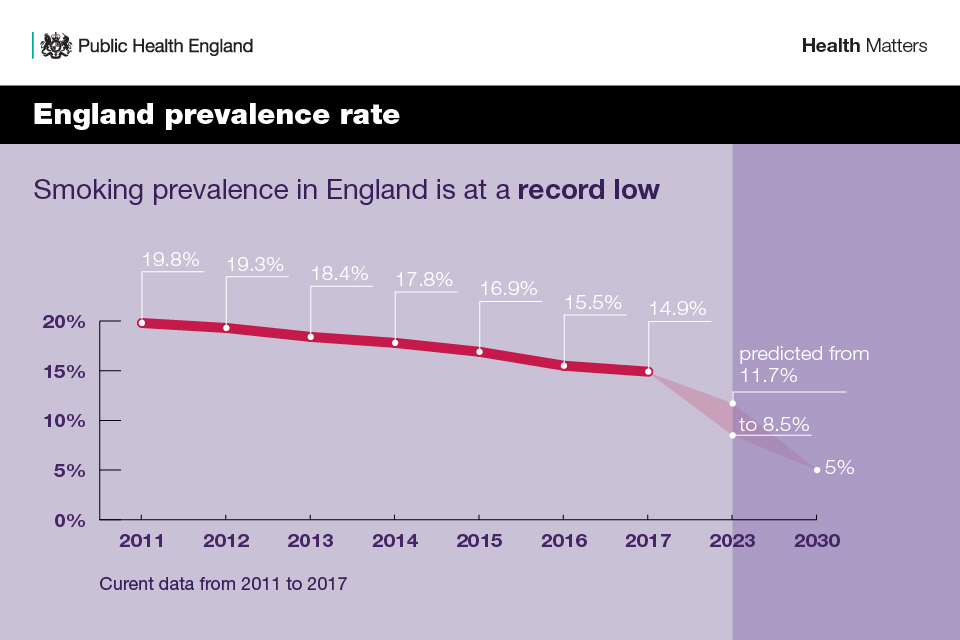
Infographic showing smoking prevalence in England
The largest reduction in smoking prevalence has been among 18 to 24-year-olds – 17.8% of this group smoked in 2017 compared with 25.7% in 2011. Those aged 25 to 34 years continue to have the highest proportion of current smokers at 19.7%, which equates to around 1.6 million people. Those aged 65 years and above continue to have the lowest prevalence rates at 8.1%, equating to around 914,000 people.
The evidence on nicotine
Perhaps the greatest obstacle we face is the widespread misconception amongst smokers and health professionals that most of the harm of smoking comes from the nicotine.
While nicotine is the addictive substance in cigarettes, it is relatively harmless. In fact, almost all of the harm from smoking comes from the thousands of other chemicals in tobacco smoke, many of which are toxic.
Nicotine replacement therapy is a safe form of treatment and licensed for use even in pregnancy and for people with cardiovascular disease. Nicotine increases heart rate and blood pressure, and has a range of local irritant effects, but is not a carcinogen. It is the tar and carbon monoxide in cigarette smoke, along with more than 400 other toxins, that causes almost all of the harm of smoking.
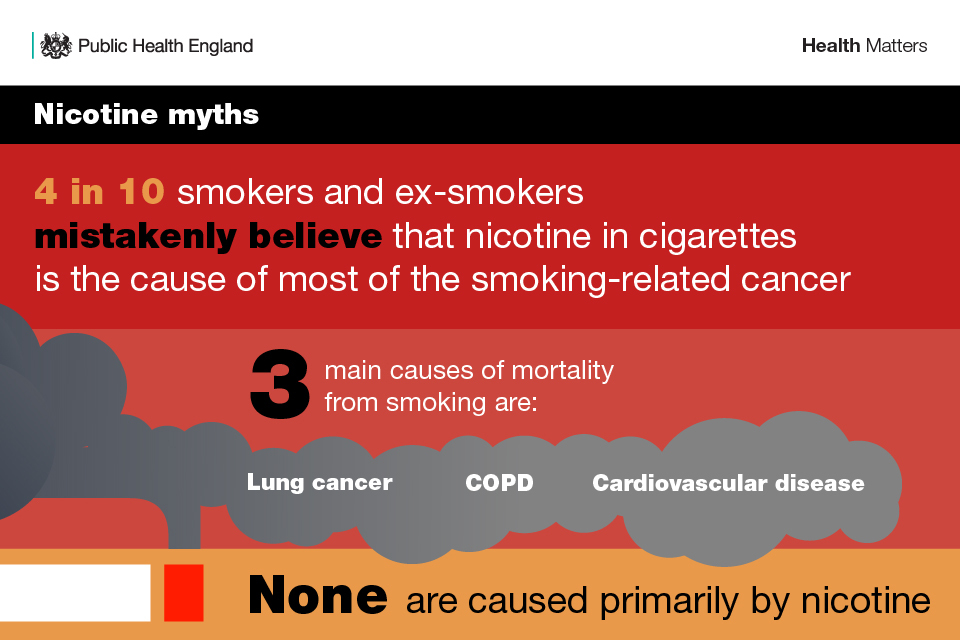
Infographic illustrating myths about nicotine
Smoking and health inequalities
As smoking prevalence has declined, it has become increasingly concentrated among more disadvantaged communities and groups:
- around 1 in 4 people in routine and manual occupations smoked, compared with 1 in 10 people in managerial and professional occupations
- people who are unemployed are almost twice as likely to smoke as those in work
- smoking prevalence among adults with a serious mental illness is over two and a half times the national average
The Tobacco Control Plan for England (2017) sets out the ambition to “reduce the inequality gap in smoking prevalence, between those in routine and manual occupations and the general population”.
Smoking during pregnancy is also a major health inequality, with prevalence varying significantly across communities and social groups:
- smoking prevalence among pregnant women in more disadvantaged groups and those aged under 20 remains considerably higher than in older and more affluent groups
- mothers in routine and manual occupations are 5 times more likely to have smoked throughout pregnancy compared to women in managerial and professional occupations
The decline in the prevalence of smoking during pregnancy has stalled in recent years, with more than 1 in 10 babies in England born to a mother who smoked throughout her pregnancy. Latest figures from NHS Digital found that 10.4% of pregnant women were known to be smokers at the time of delivery.
In some areas, this is as high as 1 in 4. Reducing smoking during pregnancy is one of the three national ambitions in the Tobacco Control Plan: “reducing smoking amongst pregnant women (measured at the time of giving birth) to 6% by the end of 2022”.Just 33 out of 195 Clinical Commissioning Groups (CCGs) in England met the national ambition of 6% or less.

Infographic on smoking in pregnancy
To find out what your local smoking rate is, how it compares with the rest of your region and the impact it has on local health and services, visit the Local Tobacco Profiles for England website where all the latest data is available.
The impact of smoking on health
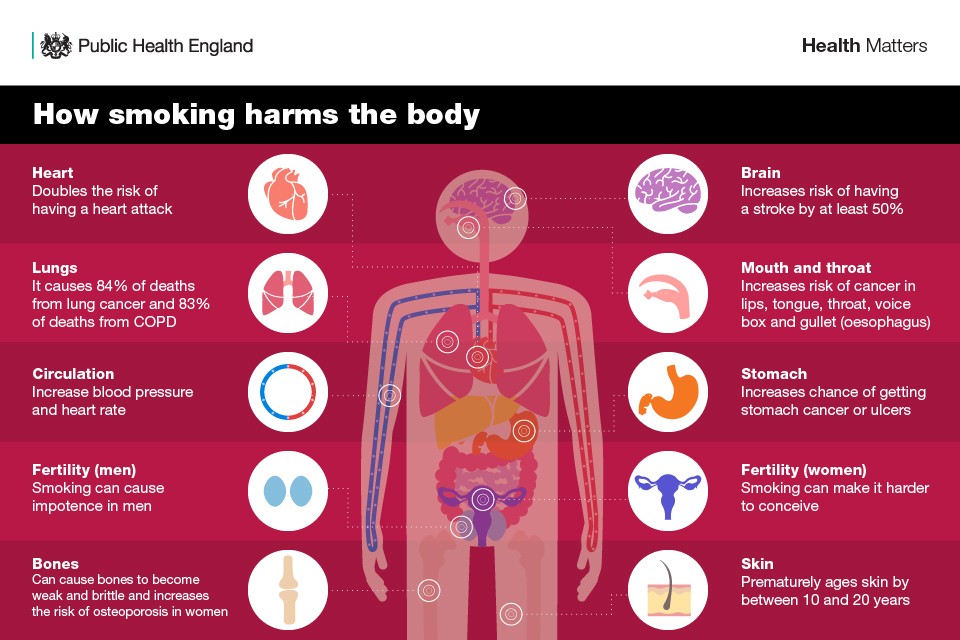
Infographic showing how smoking harms the body
The cost of smoking to society
Smoking places a considerable burden not only on individuals, but also on the NHS and the wider economy and society.
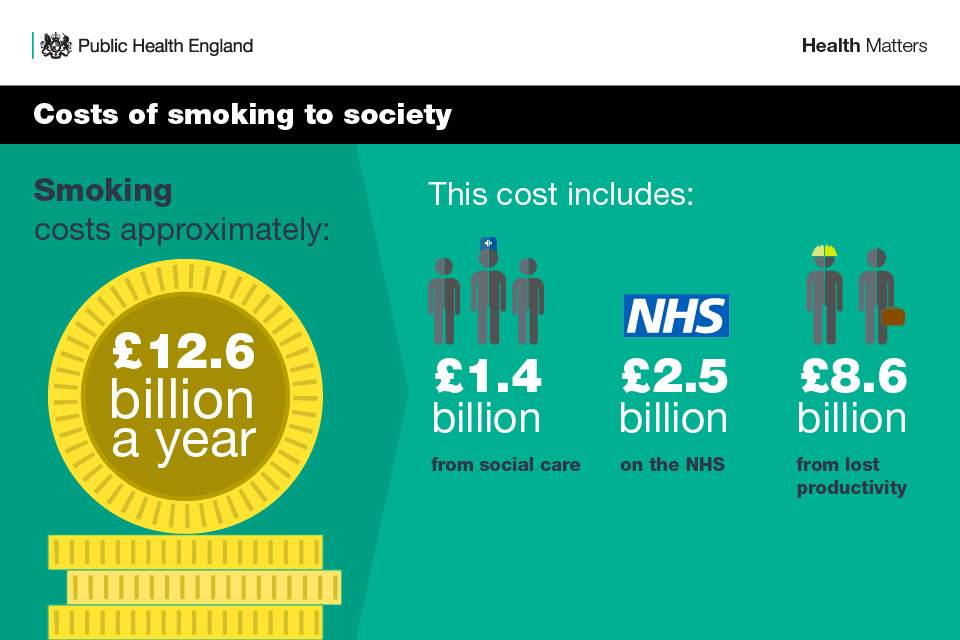
Infographic showing the costs of smoking to society
According to the ONS, in 2016 to 2017 there were an estimated 485,000 smoking-related admissions to hospital, equating to over 1,300 per day. Smokers also see their GP 35% more than non-smokers, and these costs add a great burden to a system already dealing with growing demand.
There are also increased costs for the adult social care system. The All Party Parliamentary Group on Smoking and Health has estimated that as a result of smoking-related health conditions, local councils face a demand pressure of £760 million a year on domiciliary care services.
Creating a smokefree society: the role of the NHS
Although there are now 1 million fewer smokers than in 2014, 6.1 million adults in England are still subject to the devastating harm tobacco causes. Therefore, reducing smoking remains one of PHE’s key priorities.
PHE is calling for the NHS long-term plan to commit to achieving a smokefree society by 2030 with an adult prevalence of 5% or less.
Smoking is not a lifestyle choice but a long-term relapsing condition. Every patient or staff member who smokes must be offered the support they need to quit and PHE wants to see NHS trusts stepping up their efforts in establishing a smokefree NHS by 2020.
Reducing smoking rates is the single biggest thing we can do to improve the nation’s health. It will reduce cardiovascular disease, respiratory conditions and cancer, meaning people can live longer in better health and, according to the Royal College of Physicians (RCGP), it will save the NHS up to £890 million a year.
Stop smoking support options and their effectiveness
In England, around 60% of smokers want to quit, 10% of whom intend to do so within 3 months.
Currently, around half of all smokers in England try to quit unaided using willpower alone, despite this being the least effective method. Getting support can greatly increase a person’s chances of quitting successfully:
- using nicotine replacement therapies (NRT) or e-cigarettes makes it one and a half times as likely a person will succeed
- a person’s chances of quitting are doubled if they use a stop smoking medicine prescribed by a GP, pharmacist or other health professionals
- combining stop smoking aids with expert support from local stop smoking services makes someone 3 times as likely to stop smoking successfully
The following section details the range of quitting methods and their effectiveness.
Quitting aids - what works
Expert face-to-face support
There is clear evidence that the most effective way to quit smoking is with expert behavioural support from local stop smoking services combined with stop smoking aids. These include the prescription tablets Varenicline and Bupropion, nicotine replacement therapies and e-cigarettes. Smokers who get this package of support are 3 times as likely to quit successfully as those who try to quit unaided or with over the counter nicotine replacement therapy.
Prompts by healthcare professionals are the second most common reason for someone to make a quit attempt. Effective referral routes from both primary and secondary healthcare are important to ensure that all smokers who need it get this specialist support. GPs are normally the first point of contact for patients.
As a matter of routine, they should make every contact count and identify smokers and offer smoking cessation interventions. It is, therefore concerning that the number of smokers receiving an offer of support from in primary care has been falling steadily for a number of years.
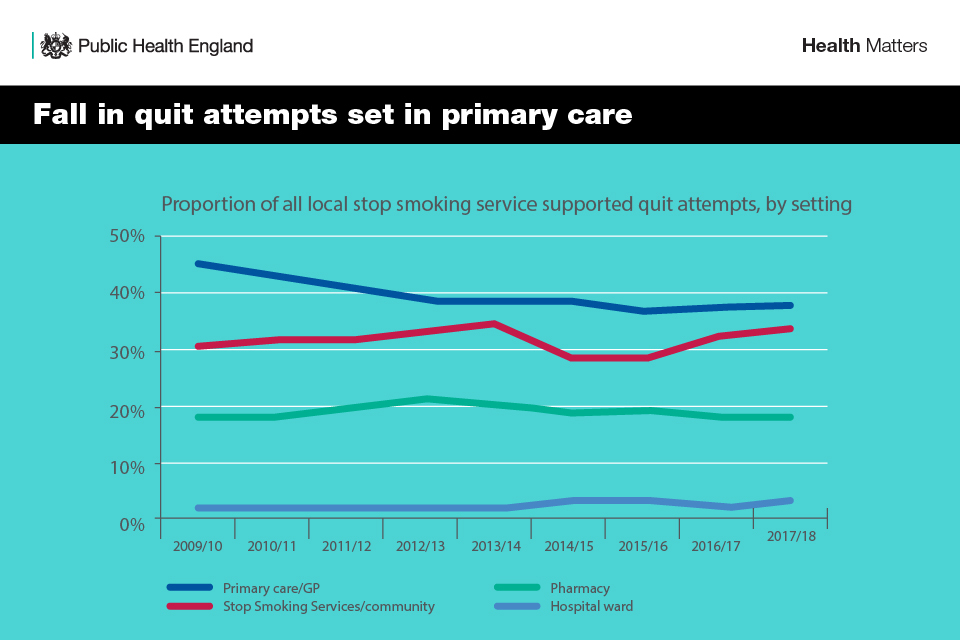
Infographic showing the fall in quit attempts set in primary care
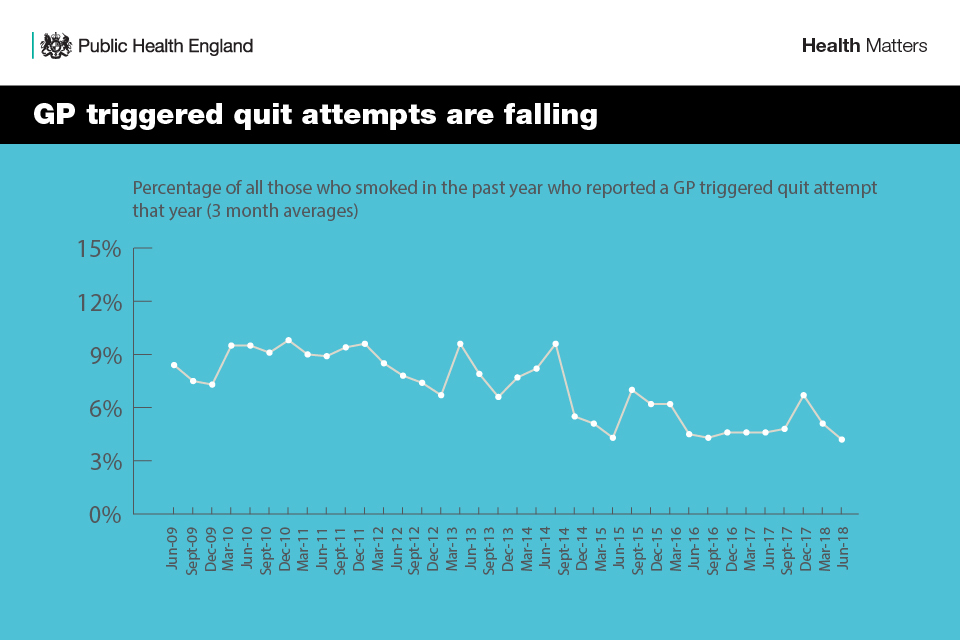
Infographic showing that GP triggered quit attempts are falling
Around 16 in 100 people remain non-smokers a year later when they choose to quit with support from a trained stop smoking advisor and use a stop smoking aid.
All healthcare professionals should identify and refer smokers using the method known as Very Brief Advice (VBA) which has 3 components, Ask, Advise and Act:
- ASK and record smoking status; is the patient a smoker, ex-smoker or non-smoker?
- ADVISE on the best way of quitting; the best way of stopping smoking is with a combination of stop smoking aids and specialist support
- ACT on patient response; build confidence, give information, refer, and prescribe
PHE has published ‘Stop smoking options: guidance for conversations with patients’ to support conversations between clinicians and people who want to quit smoking, on what method to choose.
Stop smoking aids
There is good evidence to show that using stop smoking aids increases people’s chance of quitting success, particularly when combined with expert face-to-face support from a local stop smoking service. There are 3 types:
- Prescription tablets (Varenicline and Bupropion)
- Nicotine replacement therapy products such as patches, inhalers and gum
- E-cigarettes or vapes
1. Prescription tablets
There are 2 prescription-only stop smoking medicines – Varenicline (Champix) and Bupropion (Zyban). Neither medicine is licensed for use during pregnancy, by people with certain pre-existing conditions or by under-18s.
Varenicline
Varenicline reduces cravings for nicotine by blocking the rewarding and reinforcing effects of smoking which take place in the brain. It increases the chances of long-term quitting success between 2 and 3 times compared to a quit attempt without the use of a stop smoking aid.
Bupropion
Bupropion reduces urges to smoke and helps with withdrawal symptoms. The likelihood of staying smokefree using this medication is similar to that for nicotine replacement therapy.
2. Nicotine replacement therapy (NRT)
NRT is a medicine that provides users with nicotine without the tar, carbon monoxide and other poisonous chemicals present in tobacco smoke. It can help to reduce tobacco withdrawal symptoms such as irritability and cravings.
NRT is available over the counter as well as on prescription. It is available as:
- skin patches
- chewing gum
- inhalers
- oral strips
- lozenges
- microtabs
- nasal and mouth sprays
NRT is an effective stop smoking method, increasing chances of stopping smoking for 6 months or more by more than half. There is also good evidence to show that combination NRT is more effective than single product use.
A nicotine patch releases nicotine slowly into the body’s system to help keep it on a constant level, while a fast-acting product such as an inhaler, lozenge or gum helps with immediate cravings. NICE recommends that combination NRT should be considered as a viable option for all smokers wanting to quit. For further information, see the NCSCT briefing ‘Combination nicotine replacement therapy’.
Nicotine is addictive but the level of addictiveness depends on the delivery system. The addictiveness of tobacco cigarettes is enhanced by compounds in the smoke other than nicotine. NRT products are available in different strengths so that nicotine intake can be gradually reduced when the person feels ready. Premature cessation of NRT is associated with relapse to smoking.
3. E-cigarettes
An e-cigarette allows the user to inhale nicotine through a vapour rather than smoke. E-cigarettes come in a variety of models and work by heating solution (e-liquid) that typically contains nicotine, propylene glycol and or vegetable glycerine and flavourings.
At present, there is no medicinally licensed e-cigarette product available on the UK market. However, the UK has some of the strictest regulation for e-cigarettes in the world. Under the Tobacco and Related Products Regulations 2016, e-cigarette products are subject to minimum standards of quality and safety, as well as packaging and labelling requirements to provide consumers with the information they need to make informed choices. All e-cigarette products must be notified by manufacturers to the UK Medicines and Healthcare products Regulatory Agency (MHRA), with detailed information including the listing of all ingredients.
Leading UK health and public health organisations including the RCGP, BMA and Cancer Research UK now agree that although not risk-free, e-cigarettes are far less harmful than smoking. Based on an assessment of the available international peer-reviewed evidence, PHE and the RCGP estimate the risk reduction to be at least 95%. In 2018, 3 major US reports (National Academies of Sciences, Engineering and Medicine, American Cancer Society and the US Annual Review of Public Health) found that e-cigarettes are substantially less harmful than smoking.
E-cigarettes are currently the most popular stop smoking aid in England, with an estimated 2.5 million users. Over half (51%) have stopped smoking completely and of the 45% who still smoke, half say that they are vaping in order to stop smoking. The number who have quit smoking and vaping has reached 770,000.
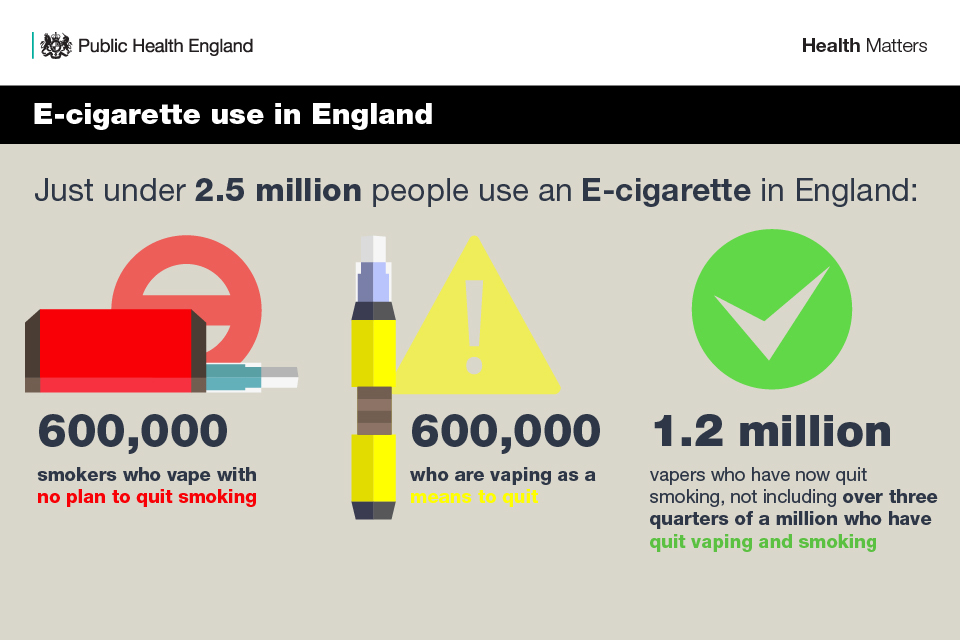
Infographic illustrating e-cigarette use numbers in England
There is growing evidence that e-cigarettes are helping many thousands of smokers in England to quit. The available evidence from research trials suggests that their effectiveness is broadly similar to prescribed stop smoking medicines and better than NRT products if these are used without any professional support. E-cigarettes are particularly effective when combined with expert help from a local stop smoking service. In 2017 to 2018, around two-thirds of smokers who got this support stopped smoking successfully.
Local stop smoking services have an important role to play in supporting smokers who want to use an e-cigarette in their quit attempt. Yet currently, only around 4% of those using stop smoking services are using an e-cigarette in their quit attempt. Clearly, more can be done to combine the popular quitting method with the most effective quitting aid to maximise the number of smokers quitting successfully.
NICE guidance NG92 recommends that health and social care professionals provide the following advice to smokers who are using, or interested in using, an e-cigarette for quitting:
- although these products are not licensed medicines, they are regulated by the Tobacco and Related Products Regulations 2016
- many people have found them helpful to quit smoking cigarettes
- people using e-cigarettes should stop smoking tobacco completely because any smoking is harmful
- the evidence suggests that e-cigarettes are substantially less harmful to health than smoking but are not risk-free
- the evidence in this area is still developing, including evidence on the long-term health impact.
The BMA provides some answers to common questions on e-cigarettes to support doctors when discussing their use with patients. See ‘What should doctors say’ (scroll down the webpage).
The RCGP’s recommendations for primary care clinicians together with a video podcast setting out the evidence to help inform conversations with patients about e-cigarettes, can be found here.
The National Centre for Smoking Cessation and Training (NCSCT) has developed a free online training module on e-cigarettes for healthcare professionals.
PHE’s blog: ‘Clearing up some myths around e-cigarettes’ provides the evidence in response to some of the more commonly reported inaccuracies and misconceptions about e-cigarettes and vaping.
E-cigarettes v cigarettes – what’s the difference?:
E-cigarettes v cigarettes – what’s the difference?
The RCGP position statement on e-cigarettes:
RCGP position statement on e-cigarettes
Advising smokers on the relative risks of nicotine-containing products compared to smoked tobacco is an integral part of supporting them to quit. People should be advised to use NRT, or an e-cigarette if they choose, as much they need to help them manage their cravings when they stop smoking. Insufficient nicotine replacement and premature cessation of it are both associated with relapse to smoking.
4. Other options
There are other quitting support options available such as:
- text message support
- websites
- mobile digital apps
- hypnotherapy
- acupuncture
- acupressure
- laser therapy
Some of these options may slightly improve quitting success, but there is evidence that acupuncture, acupressure and laser therapy do not improve chances of quitting smoking. Hypnotherapy is no more effective than counselling.
Unassisted quitting
Unassisted quitting is an attempt to stop smoking with willpower alone, which is sometimes referred to as going ‘cold turkey’. It is the least effective of all stop smoking methods, with only around 3 to 4 in 100 people remaining non-smokers after a year when they choose to make an unassisted quit attempt.
Call to Action
Use the Stoptober resources
Stoptober provides an ideal opportunity to engage with smokers. There’s a range of materials available to support healthcare professionals, including guidance on starting conversations and other campaign material that can be used in GP practices, pharmacies and hospital and community care settings.

Infographic showing Stoptober logo
Pharmacy teams
Pharmacy teams have a variety of opportunities to discuss smoking, such as when people are buying NRT, purchasing cough medicines repeatedly or when dispensing medicines for smoking-related conditions such as high blood pressure, COPD, diabetes and heart disease.
Smokers interested in quitting may also ask about e-cigarettes, so pharmacy staff should update their knowledge on the evidence and products available, by completing the NCSCT online training module.
Primary care
GPs should advise patients who smoke that the most effective way to quit smoking is a combination of behavioural and pharmacological support.
Stop smoking aids (NRT, Champix and Zyban) can be prescribed for smokers who want to quit. While e-cigarettes are not currently available on prescription, GPs should provide advice to patients who are interested and may find them beneficial, in line with NICE guidance.
Secondary care
It is estimated that 1 in 4 patients in acute hospital beds in England are smokers and this presents a unique opportunity to offer stop smoking advice.
Achieving the ambition of a truly smokefree NHS means:
- every front-line healthcare professionals discusses smoking with their patients
- all smokers are offered on-site stop smoking support or referral to local services
- hospital buildings and grounds are completely smokefree
Mental health services
All frontline clinicians should ensure that tobacco dependency is treated among people with mental health problems as part of their clinical care. This includes the provision of a full range of stop smoking support, whether a patient wants to quit for good or temporarily abstain while in a smokefree NHS setting. Tobacco dependence treatment pathways between secondary and primary care are essential to reduce the inequalities gap and ensure continuity of care.
Maternity services
NICE guidance recommends that all pregnant women should be screened for carbon monoxide (CO), with those having elevated levels referred for specialist stop smoking support.
Members of the midwifery team should be trained in the use of the CO monitor and in having a brief meaningful conversation about the harms of smoking and the support available. Robust and effective pathways into specialist support should be in place, with feedback to the referring midwife.
Local authorities
Local authorities should continue to identify local need using PHE’s fingertips tool and provide stop smoking services, particularly for priority populations and those in greatest need.
Local authorities should continue to promote the NHS Health Check which presents an ideal opportunity to offer advice on quitting smoking. All smokers should be offered a referral to their local stop smoking service. Research published in the BMJ has shown that people who attend an NHS Health Check are twice as likely to be referred to smoking cessation clinics.
Read case study: Essex County Council delivers stop smoking support via vape shops
Clinical Commissioning Groups
Commissioners should ensure that Varenicline and Bupropion are included in the local drug formularies and available for GPs to prescribe, in line with NICE guidance.
Local stop smoking services
Local stop smoking services should engage actively with smokers who want to use an e-cigarette to help them quit, and provide the additional support that will give them the best chance of success.
Resources
Download supporting references.
Download the Health matters infographics.
Read the Health matters blog.
Read case study: Essex County Council delivers stop smoking support via vape shops
