Falls: applying All Our Health
Updated 25 February 2022
The Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
Introduction
Falls and fractures in older people are often preventable. Reducing falls and fractures is important for maintaining the health, wellbeing and independence of older people.
A fall is defined as an event which causes a person to, unintentionally, rest on the ground or lower level, and is not a result of a major intrinsic event (such as a stroke) or overwhelming hazard. Having a fall can happen to anyone; it is an unfortunate but normal result of human anatomy. However, as people get older, they are more likely to fall over. Falls can become recurrent and result in injuries including head injuries and hip fractures.
The causes of having a fall are multifactorial – a fall is the result of the interplay of multiple risk factors. These include:
- muscle weakness
- poor balance
- visual impairment
- polypharmacy – and the use of certain medicines
- environmental hazards
- some specific medical conditions, which might make a person more likely to fall
Falls are events resulting from the presence of risk factors. The likelihood and severity of injury resulting from an event is related to a number of possible factors including bone health, risk of falls, frailty and low weight. Strong bones are important for your health. People with low bone mineral density are more likely to experience a fracture following a fall. Osteoporosis is one of the reasons why people have low bone mineral density.
Over 3 million people in the UK have osteoporosis and they are at much greater risk of fragility fractures. Fragility fractures are fractures that result from mechanical forces that would not ordinarily result in fracture, known as low-level (or ‘low energy’) trauma. The World Health Organization (WHO) has quantified this as ‘forces equivalent to a fall from a standing height or less’. Hip fractures alone account for 1.8 million hospital bed days and £1.1 billion in hospital costs every year, excluding the high cost of social care.
Fragility fractures are most common in bones of the spine, wrists and hips. The risk of osteoporosis starts to increase in women after the menopause because their ovaries no longer produce oestrogen, which helps to protect the bones. People may also be at increased risk of osteoporosis because it runs in their family or because of the side effects of some medications such as steroid tablets or injections. Therapies and treatments are available to help prevent fractures in people with osteoporosis. Other factors can also put a person at risk of fractures: low body weight (BMI <19), diet lacking in calcium and vitamin D, poor mobility, smoking, alcohol, diabetes, certain long term medications, especially corticosteroids.
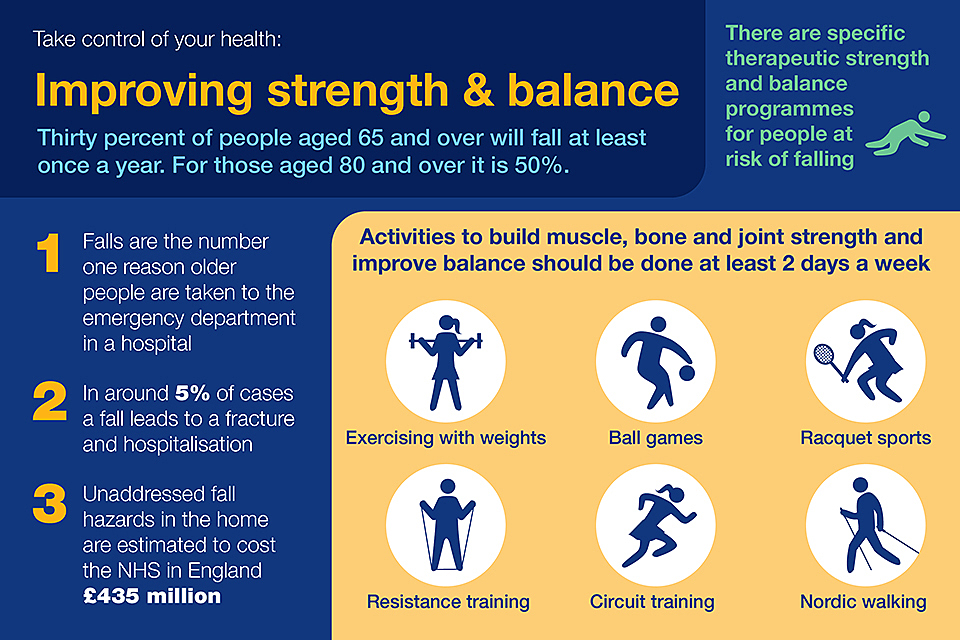
Graphic showing ways to improve strength and balance.
Focusing on falls in your professional practice
Falls and fractures are a common and serious health issue faced by older people in England. People aged 65 and older have the highest risk of falling; around a third of people aged 65 and over, and around half of people aged 80 and over, fall at least once a year. Falling is a cause of distress, pain, injury, loss of confidence, loss of independence and mortality.
For health services, they are both high volume and costly.
In terms of annual activity and cost:
- the Public Health Outcomes Framework (PHOF) reported that in 2017 to 2018 there were around 220,160 emergency hospital admissions related to falls among patients aged 65 and over, with around 146,665 (66.6%) of these patients aged 80 and over
- falls were the ninth highest cause of disability-adjusted life years (DALYs) in England in 2013 and the leading cause of injury
- unaddressed fall hazards in the home are estimated to cost the NHS in England £435 million
- the total annual cost of fragility fractures to the UK has been estimated at £4.4 billion which includes £1.1 billion for social care; hip fractures account for around £2 billion of this sum
- short and long-term outlooks for patients are generally poor following a hip fracture, with an increased one-year mortality of between 18% and 33% and negative effects on daily living activities such as shopping and walking
- a review of long-term disability found that around 20% of hip fracture patients entered long-term care in the first year after fracture
- falls in hospitals are the most commonly reported patient safety incident with more than 240,000 reported in acute hospitals and mental health trusts in England and Wales
Core principles for health and care professionals
In general health and care professionals should:
- make themselves aware of the range of needs of individuals, communities and the population and the services available in the localities in which they work
- think about the variety of resources available in health and wellbeing systems, including people, data, written, and digital
- understand specific activities which can prevent, protect and promote in the areas of falls and fractures
Taking action
The National Falls Prevention Coordination Group’s Falls and fracture consensus statement advocates a whole system approach to prevention, which includes:
- risk factor reduction across the life-course
- case finding and risk assessment
- strength and balance exercise programmes
- healthy homes
- high-risk care environments
- fracture liaison services
- collaborative care for severe injury
Interventions can take place at population, community and individual levels.
If you’re a front-line health and care professional
Health and care professionals can have an impact on an individual level by:
- routinely asking older people about falls
- observing for deficits in gait and balance
- knowing how to recognise the signs of potential risk
- assessing potential risks, including medical conditions which might predispose a person to fall
- understanding the referral pathway to local services, that reduce fall risks
- reassuring individuals and their carers or families, that help is available to reduce the risk of falling
- supporting healthy ageing, including reducing exposure to risk factors such as physical inactivity and visual impairment, making every contact count and signposting eligible patients to NHS health checks
- providing up-to-date patient information on falls, such as Get up and go: a guide to staying steady from the Chartered Society of Physiotherapists
If you’re a team leader or manager
Community health and care professionals, and providers of specialist services can have an impact by:
- considering their role in primary falls prevention and the messages given out about health behaviours
- encouraging people to stay active, get socially connected and get their eyes and ears checked regularly
- eat a healthy balanced diet, reduce alcohol intake and stay well hydrated to reduce the risk of falling – and improve outcomes if a fall happens
- developing links with local community providers
- displaying information in workplaces promoting physical activity benefits for adults and older adults
- promoting the importance of strength and balance exercise
- encouraging people to drink enough water, especially in hot weather to avoid dehydration
- ensuring that inpatient care is in line with national falls and fracture clinical guidelines and quality standards
If you’re a senior or strategic leader
Senior or strategic leaders should be aware of interventions at population level, which can include:
- understanding the local population – considering the proportion of older people, frailty prevalence, and the number of falls in the population
- reviewing the capacity and makeup of falls prevention services
- influencing relevant parties to support the development of local services – ensuring that falls prevention is a local health priority
- encouraging the use of established tools, such as those from Chartered Society of Physiotherapy (CSP)
- considering the training needs of the workforce, and what action is needed to give all health and care professionals the knowledge and skills to identify the risk of falls for older people
- ensuring the promotion of physical activity is prominent within commissioned services
- exploring the intensity of exercise programmes
- promoting the importance and influencing the evaluation of strength and balance exercise programmes
- ensuring alignment of falls and fracture services with related services such as frailty
Get up and go campaign image
Understanding local needs
The Public Health Outcomes Framework (PHOF) focuses on 2 high-level outcomes:
- increased healthy life expectancy
- reduced differences in life expectancy and healthy life expectancy between communities
The PHOF includes indicators on emergency hospital admissions and hip fractures due to falls in people aged 65 and over.
Emergency hospital admissions due to falls:
- C29i – aged 65 and over
- C29ii – aged 65 to 79
- C29iii – aged 80 and over
Indicators on hip fractures in people aged 65 and over include:
- E13i – aged 65 and over
- E13ii – aged 65 to 79
- E13iii – aged 80 and over
Mortality rates from accidental falls can be found in the Health and Social Care Information Centre Indicator Portal.
The Sport England Active Lives Survey includes information on the activity levels of older adults. Between November 2019 and November 2020, including during the COVID-19 pandemic, older adults aged 75 and over became less physically active, especially those with multimorbidity, due to the government requirement to stay at home and to shield.
Wider impacts of COVID 19 on physical activity, deconditioning and falls in older adults, published on August 2021, includes an estimation of the impacts of COVID-19 on physical activity and falls in older adults, and recommendations to mitigate these effects.
Measuring impact
As a health and care professional, there are a range of reasons why it makes sense to measure your impact and demonstrate the value of your contribution.
This could be about sharing what has worked well in order to benefit your colleagues and local people, or help you with your professional development.
The Everyday Interactions measuring public health impact toolkit provides a quick, straightforward and easy way for health and care professionals to record and measure their public health impact in a uniform and comparable way.
The falls impact pathway is recommended for health and care professionals to record and measure actions undertaken as part of routine care which impact on falls prevention.
Further reading, resources and good practice
Advice for patients and the public
The NHS website has information and advice on falls prevention.
The CSP’s Get up and go – a guide to staying steady is a 32-page guide for the public and patients on how to prevent falls, produced by Saga in partnership with the CSP and the Office for Health Improvement and Disparities (OHID).
Age UK provides information and advice on falls prevention. RoSPA provides advice on how to make the home a safer environment. NHS Rightcare Falls and Fragility Fractures pathway (2017) NICE Impact Falls and Fractures. Royal Osteoporosis Society Clinical Guidance ‘A Safe Home’ provides information on preventing falls at home developed by NHS 24’s Scottish Centre for Telehealth and Telecare (SCTT). Spot the Hazard is a game about spotting falls hazards in the home.
The Active at Home booklet, updated in August 2021, provides practical guidance to older adults on home-based activities to maintain their strength and balance. It follows concerns that low levels of physical activity in older adults will lead to reduced fitness, resulting in loss of independence and need for care in the future.
The Keeping Well at Home guide, published in 2020, was produced by University of Manchester. It has been recently been updated to Keeping Well this Winter with tips and advice on keeping active and connected, staying safe and well, and managing our money and home.
The ‘Talking about Keeping Well this Winter’ film was made by older adults with tips on opening up a positive conversation on the doorstep or over the phone.
Watch the Talking about Keeping Well this Winter film
Better Health on the NHS website provides advice on healthy changes with free tools and support.
Professional resources and tools
OHID and the National Falls Prevention Coordination Group member organisations have produced a Falls and fracture consensus statement detailing key interventions, approaches to commissioning and the commitment to national support. It is accompanied by a resource pack which details resources relating to the key interventions and contains an additional section on frailty.
Specific guidance includes:
- Occupational therapy in the prevention and management of falls in adults: practice guidelines College of Occupational Therapists 2015
- Clinical guideline for the prevention and treatment of osteoporosis National Osteoporosis Guideline Group 2017
- The management of hip fracture in adults NICE CG124 2014
- Osteoporosis: assessing the risk of fragility fracture NICE CG146 2017
- Falls in older people: assessing risk and prevention NICE CG161 2013
- Midlife approaches to preventing the onset of disability, dementia and frailty NICE NG16 2016
- Multimorbidity: clinical assessment and management NICE NG56 2016
Falls FAQs poster (PDF, 760KB), developed by the National Falls Prevention Coordination Group (NFPCG), is for care and residential homes to support staff to manage a fall that may require an ambulance.
Newcastle University has developed a free online falls prevention training course.
Strength and balance quality markers: supporting improvement (published July 2019) details the 7 quality markers for strength and balance exercise, suitable for use by local areas as criteria to help them carry out self-audits.
Quality standards
- Falls in older people NICE QS86 2017
- Osteoporosis NICE QS149 2017
Cochrane systematic reviews
- Interventions for preventing falls in older people in care facilities and hospitals
- Multifactorial and multiple component interventions for preventing falls in older people living in the community
- Exercise for preventing falls in older people living in the community
The Raising the bar on strength and balance: The importance of community-based provision report from the Centre for Ageing explains the models of delivery, issues and barriers of community ‘strength and balance’ programmes.
Good practice examples
The CSP’s Get up and go – a guide to staying steady is a 32-page guide for the public and patients on how to prevent falls, produced by Saga in partnership with the CSP and OHID.
OHID’s Everybody active, every day: an evidence-based approach to physical activity, published in 2014, is a physical activity strategy co-produced with over 1,000 partners including health and professionals, local authorities, research specialists, educationalists, charities and fitness experts.
The Royal College of Physicians’ National audit of inpatient falls, published in 2021, contains recommendations and resources aimed at reducing inpatient falls
Raising the Bar on Strength and Balance, Centre for Ageing Better, 2019.
