Healthy ageing: applying All Our Health
Published 20 April 2022
Applies to England
Please note that the Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities on 1 October 2021.
Introduction
This guide is part of All Our Health, a resource which helps health and care professionals prevent ill health and promote wellbeing as part of their everyday practice. The information below will help front-line health and care staff use their trusted relationships with patients, families and communities to promote the benefits of healthy ageing. We also recommend important actions that managers and staff holding strategic roles can take.
Why promote healthy ageing in your professional practice
There has been a steady increase in average life expectancy in recent decades and there are now half a million people in their 90s in the UK, more than two and a half times the number in 1985. By 2035, over half of adults in the UK are expected to be 50 or over. However, these increases have not been matched by an increase in healthy life expectancy.
The gap in life expectancy between the most and least deprived areas of England has significantly widened in recent years. For males it increased from 9.0 years in 2011 to 2013 to 9.4 years in 2017 to 2019. For females during this period, the gap increased from 6.9 to 7.6 years. This means that a boy born in Blackpool can expect to live to the age of 74.5. Whereas a boy born in Westminster can expect to live to the age of 83.9.
People in the most deprived areas were 4 times more likely to die prematurely from cardiovascular diseases and 2.2 times more likely to die from cancer than people living in the least deprived areas in 2017 to 2019.
Many older adults have experienced physical deconditioning as a result of the pandemic and lockdown. This impacts on their physical, mental and social health, and could increase the prevalence of falls. In the first lockdown, 39.3% of people aged 55 to 64 and 36.4% of those aged 65+ were doing less physical activity than usual. By November 2020, over a quarter (26.7%) of people aged 55 to 64 and nearly a third (31.8%) of those aged 65+ had not undertaken at least 30 minutes of physical activity in the past week.
Regional differences in health are large and growing
Male healthy life expectancy from birth
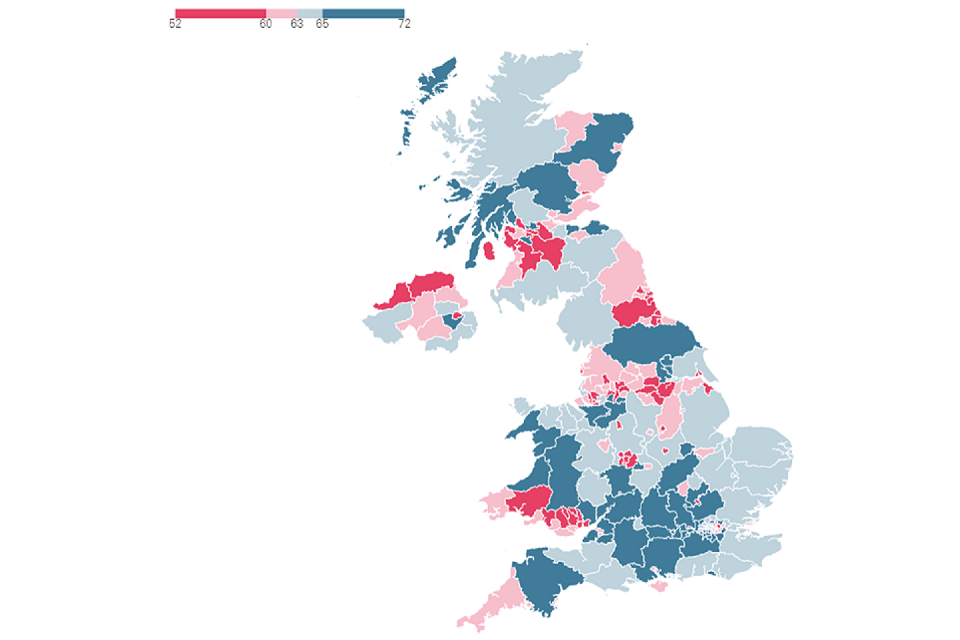
Number of health years expected, by local authority 2016-2018. Category size dependent on number of local authorities in quartile.
Healthy life expectancy varies depending on where you live. The map shows that local areas of low healthy life expectancy tend to be clustered: seen in South Wales, Eastern Scotland, Northern Ireland and parts of the north of England.
As well as a widening gap in life expectancy, too many people spend a large proportion of their later life in poor health or managing multiple long-term conditions which could have been prevented or the impact lessened through reducing behavioural risk factors, and healthy choices and lifestyles, particularly those in more deprived parts of the country. Those in the wealthiest parts of England have almost twice as many years of disability-free life ahead of them at the age of 65 as those in the poorest.
Years spent with and without disability at age 65 for men in the poorest and wealthiest area, England, 2016 to 2018
| - | Poorest | Wealthiest |
|---|---|---|
| Years with disability | 9.6 | 8.8 |
| Years without disability | 6.2 | 12.2 |
We have an opportunity to tackle ageism, challenge stereotypes and enable more people in later life to be happy, healthy and active. We need to address these inequalities and we can do this by promoting the concept of productive healthy ageing.
What we mean by productive healthy ageing is that in later life, we want everyone to be able to experience:
- financial security and independence
- a sense of meaning and purpose, including through high quality work, caring or volunteering
- good social connections, friendships and support
- better physical health and mental wellbeing
- resilience – both physical and cognitive reserve
Further information about these individual concepts are described below.
Financial security can be improved through:
- financial planning for the future in midlife
- opportunities to undertake meaningful and rewarding work
- flexible working practices to support carers and those living with long term conditions
Meaning and purpose can be improved through:
- support for unpaid carers
- inclusive approaches that encourage older people to volunteer
- opportunities for older people to provide mentoring and peer support
- remaining engaged with creative, learning and cultural activities as we age
Connectedness can be improved through:
- maintaining friendships and family networks
- community participation among people of all ages
- removing barriers to participation, for example through providing accessible transport and use of technology
- adaptable public engagement approaches that consider cultural issue, needs and differences
Physical health can be improved through:
- education, raising awareness and empowerment to control our own health
- regular physical activity in line with CMO guidelines, particularly increasing strength and balance activity
- maintaining a healthy diet and staying hydrated
- stopping smoking
- reducing alcohol consumption in line with the CMO’s low risk drinking advice
- taking up immunisation and health screening opportunities when offered
- reducing exposure to air pollution
Resilience can be improved through:
- understand the protective factors that help people develop and maintain resilience throughout their lives – good education, good work, financial security, a decent home and the ability to develop and maintain connections to family, friends and a supportive wider community
- build physical and cognitive reserve
- take up lifelong learning opportunities
Since many older adults interact with health and care professionals more frequently than younger populations, you have a unique opportunity to make a lasting impact and support everyone to have a longer, happier, healthier and more active life.
The main principles of public health prevention to improve your general population’s health and wellbeing are covered in detail across the other All Our Health modules. However, there are particular needs and inequalities that exist within the older adult population that need to be taken into account to ensure that all adults have the best chance of being healthy, happy and active into later life.
Core principals for health and care professionals
This All Our Health healthy ageing information has been created to help all health and care professionals:
-
understand specific activities and interventions that can support healthy ageing and provide holistic care
-
think about the resources and services available in your area that can help people to be happy, healthy and active into later life
Taking action
Front-line health and care professionals
Health and care professionals should provide support to those in mid-life onwards to educate and empower individuals to make positive choices about their own health and wellbeing. Supporting positive lifestyle changes can lead to an increase in years spent disability free in later life.
Health and care professionals can have an impact at an individual level by promoting healthy behaviour messages to support the health and wellbeing of individuals and their carers as part of making every contact count (MECC), in particular:
-
the importance of a healthy diet and staying hydrated
-
encouragement of regular physical activity following the Chief Medical Officer’s guidelines, stressing that it’s never too late to start, any activity is better than none and recognising the social benefits that group activities can provide
-
being aware of falls prevention and support services in your local area and signposting to local strength and balance services in your local community to promote good musculoskeletal health
-
support to stop smoking and reduce alcohol consumption in line with the Chief Medical Officers’ low risk drinking advice (particularly important for the over 50s who are most likely to have been accumulating alcohol related risk over decades)
-
supporting the uptake of immunisations and screening programmes when offered
-
advising individuals to reduce their exposure to air pollution, which has been identified as a risk factor for dementia, and that individual contributions such as walking and cycling where possible, instead of driving, improve an individual’s health as well as reducing air pollution
-
being aware of age related visual impairment and hearing impairment, which has been identified as a risk factor for dementia, and signposting to relevant services and support
-
knowing how to identify frailty and signposting to appropriate interventions and support services
-
understanding that older people, particularly those over 65 years, are at increased risk of harm from cold weather – ask about living in a cold home and support vulnerable individuals to access existing resources to keep warm
-
using opportunities to have brief conversations with people about making positive changes to improve their mental health and wellbeing
-
identifying risk factors and symptoms of mental health problems, avoiding age discrimination and the assumption that it is normal to be unhappy and depressed in later life – signposting and referring appropriately, including referral to talking therapies where appropriate
-
being aware of social prescribing services in your local area and how people’s social and emotional needs are affecting their health, for example, their relationships, social networks, and support in their neighbourhood
-
promoting the importance of taking up the NHS Health Check
-
being mindful of medication interactions and compliance
-
considering the needs of carers and knowing where to direct them for further support
-
where appropriate, advising people that their risk of developing dementia can be reduced by making behaviour changes to reduce personal risk, communicating the message to ‘love your heart, stay sharp, keep connected’
Team leaders and managers
If you’re a team leader or manager you should:
-
identify staff learning and development needs in relation to healthy ageing and provide access to appropriate training
-
promote a culture of tackling ageism and negative stereotypes relating to age
-
engage with communities to make links to behavioural risk reduction and support services, encourage their take up and reinforce the support that they offer
-
work with local public health teams to support initiatives working with local businesses, housing, transport networks, leisure services, green spaces, workplaces, care homes and voluntary community services to promote healthy lifestyles and healthy ageing
-
build prevention and promotion of healthy ageing into day-to-day work
-
work with other local services to meet people’s social needs for example, housing, employment, welfare and addressing air pollution
-
support the uptake of community based interventions to address wellbeing, social isolation, volunteering, lifelong learning and loneliness
-
support the uptake of vaccinations, screening and health checks to reduce complications and avoidable hospital admissions
-
sign up to cold weather alerts and ensure staff are aware of resources available to provide support in extreme weathers
Senior and strategic leaders
If you’re a senior or strategic lead you should:
-
adapt the built environment towards being age friendly, to make healthier choices easier
-
understand the health and wellbeing needs of your local older adult population and matching the workforce to the needs of your local population
-
consider how services are operating for those with multiple long-term conditions who do not fit into condition specific siloes
-
implement the NHSE anticipatory care model and developing integrated systems to identify and support people with long-term conditions and reduce premature mortality
-
sign up to cold weather alerts and enable roll out of key messages to local residents/ patients
-
sign your local area up to the Healthy ageing consensus statement
-
consider the unique health needs and inequalities of any coastal and rural communities within your area, as outlined in the Chief Medical Officer’s annual report: health in coastal communities and Age UK and OHID’s Ageing in rural and coastal areas report
-
maximise local signposting opportunities, such as the NHS Health Check, to provide information on what’s available locally on relevant websites
Understanding local needs
The Productive Healthy Ageing Profile tool provides local, regional and national data and signposts to further resources on a wide range of topics relevant to healthy ageing.
The Dementia Profiling tool brings together a wide range of publicly available data on dementia. It can be used to understand the prevalence of dementia and how it is prevented and diagnosed locally. It also shows data on the care that is provided to people with dementia, including end of life care.
Measuring impact
As a health and care professional there are a range of reasons why it makes sense to measure your impact and demonstrate the value of your contribution. This could be about sharing what has worked well in order to benefit your colleagues and local people or help you with your professional development.
The Everyday Interactions Measuring Impact Toolkit provides a quick, straightforward and easy way for health and care professionals to record and measure their public health impact in a uniform and comparable way.
Further reading, resources and good practice
Below is a list of further reading, resources and good practice on Healthy ageing:
Advice for patients and the public
The NHS has a practical guide to healthy ageing for those aged 70 and over.
Information on the types of physical exercises and activities is available on the NHS website. There is guidance for those aged 19 – 64 and guidance for those aged 65 and over. The NHS’ Better Health site offers lots of free tools and support to help make healthy lifestyle changes.
The NHS’ Every Mind Matters site has expert advice and practical tips to help everyone look after mental health and wellbeing.
Professional resources and tools
The Office for Health Improvement and Disparities’ (OHID) Health matters: midlife approaches to reduce dementia risk provides a resource for public health professionals, which brings together important facts, figures and evidence of effective interventions to tackle major public health problems.
The UN Decade of Healthy Ageing: Baseline Report looks at the issue of healthy ageing, enablers and how to accelerate impact.
OHID’s report on interventions for productive healthy ageing: for pharmacy teams working in different settings.
The Royal College of Psychiatrists report on age inequality in older people’s mental health care.
The following All Our Health modules are also relevant to promoting healthy ageing:
There will also be a module focussing on health inequalities being launched soon which will be very relevant to the older adult population.
NICE guidelines
Disability, dementia and frailty in later life – mid-life approaches to delay or prevent onset (NG16) aims to increase the amount of time that people can be independent, healthy and active in later life.
Multimorbidity: clinical assessment and management (NG56) covers optimising care for adults with multimorbidity by reducing treatment burden and unplanned care.
Good practice examples
The British Geriatrics Society report Healthier for longer: How healthcare professionals can support older people looks at actions health and care professionals can take to support healthy ageing and also contains practical case studies.
This content was created with the support of the British Geriatric Society.
