Health matters: reducing the burden of tuberculosis
Published 20 October 2016
Summary
Reducing the burden of tuberculosis (TB) in England is a priority for Public Health England (PHE). This professional resource outlines the actions that can be taken to further reduce TB incidence and health inequalities associated with TB.
The scale of the problem
TB explained
TB is a curable and preventable infectious disease caused by bacteria that are spread through the air in small droplets when a person with infectious TB coughs, talks, sings, or sneezes.
When someone breathes in the bacteria they may become infected with TB and could develop active TB disease or latent TB.
The symptoms of active TB are varied and can include:
- a cough for over 3 weeks
- high temperature or fever
- night sweats
- loss of appetite
- weight loss
- extreme tiredness or lack of energy
- coughing up blood
Active TB disease usually affects the lungs and this is known as pulmonary TB. It can also develop in other organs in the body including the bones and joints, reproductive or urinary tract organs, and the brain. This is known as extra-pulmonary TB.
TB is curable with antibiotics and the sooner the illness is diagnosed and treated the better. It is a life-threatening illness if left untreated; about 1 in 20 patients with TB die each year in England.
TB rates remain high
The number of cases of TB in England has shown a steady decline over the last 4 years, down by a third from the peak seen in 2011. There were 5,758 confirmed cases in England in 2015 compared to 8,280 in 2011. However, England has one of the highest rates of TB in Western Europe, according to estimates from the World Health Organisation.

Infographic of TB rates in Western Europe 2015
TB is more common in people born abroad. The rate in the non UK-born population is 15 times higher than in the UK-born population, and 73% of all cases notified in 2015 (4,087) were born abroad.
The decline in the number of cases in the non UK-born population has occurred particularly among new migrants, and 60% of non UK-born TB cases now appear among those who have lived in the UK for more than 6 years.
There has been a continued reduction in the number and proportion of TB cases co-infected with HIV, down from 1 in 12 in 2005 to 1 in 30 in 2014. The majority of TB-HIV co-infected cases were born abroad in countries with high rates of both TB and HIV.
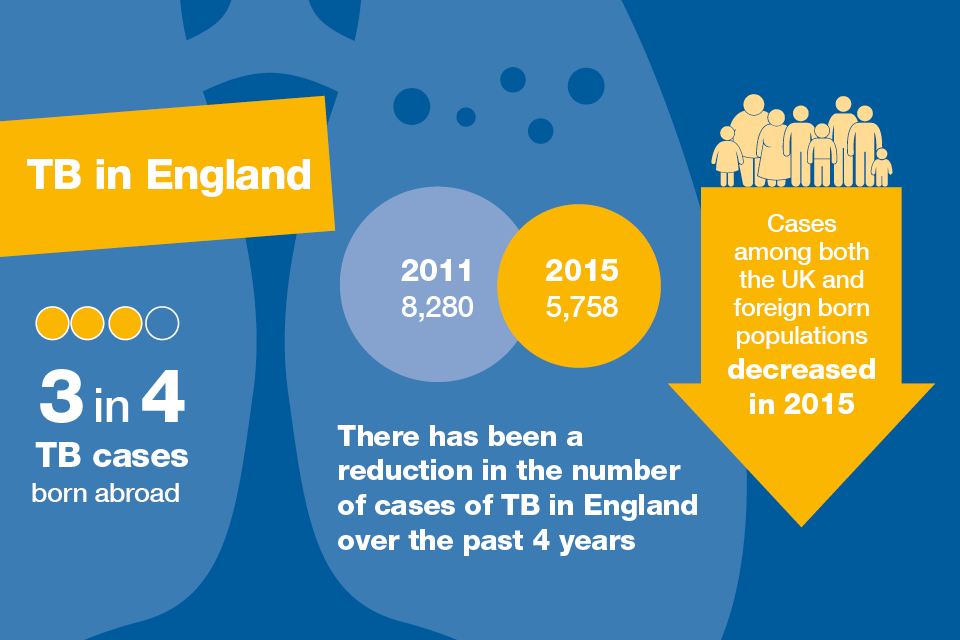
Infographic showing reduction in the number of TB cases between 2011 and 2015
TB and health inequalities
TB can be seen as a barometer of health inequalities. The Chief Medical Officer for England has identified the inequalities associated with TB as an important priority for England. Reducing health inequalities is 1 of 3 aims in the PHE and NHS England Collaborative TB Strategy for England, 2015 to 2020.
Tackling TB will play a role in enabling local authorities and the NHS to reduce health inequalities across England.
Certain groups are disproportionately affected by TB and this under-served population includes:
- ethnic minority groups
- refugees and asylum seekers
- migrants
- those with a history of or current homelessness
- those with a history of or current imprisonment
- those with a history of or current drug or alcohol misuse
- people who are immunocompromised
People with a past or current social risk factor (including homelessness, alcohol or drug misuse or imprisonment) are at increased risk of TB and in 2015 there was an increase in the number of cases with these social risk factors.
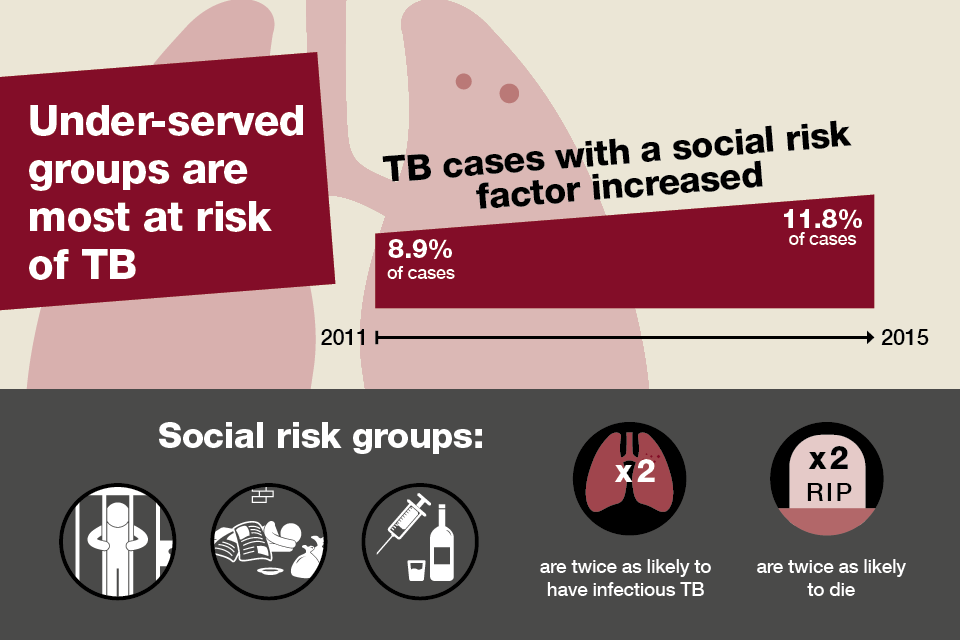
Infographic showing that under-served social risk groups are most at risk of TB
TB patients with social risk factors have a greater potential for infecting others, have poorer treatment completion as well as a greater risk of having drug resistance.
There is significant regional and local variation in rates of TB in England, depending on population characteristics, socioeconomic factors and level of local risk.
There is a clear trend of an increasing rate of TB with increasing deprivation. In 2015, the rate was 20.5 per 100,000 in the 10% of the population living in the most deprived areas compared with only 3.6 per 100,000 in the 10% of the population living in the least deprived areas.
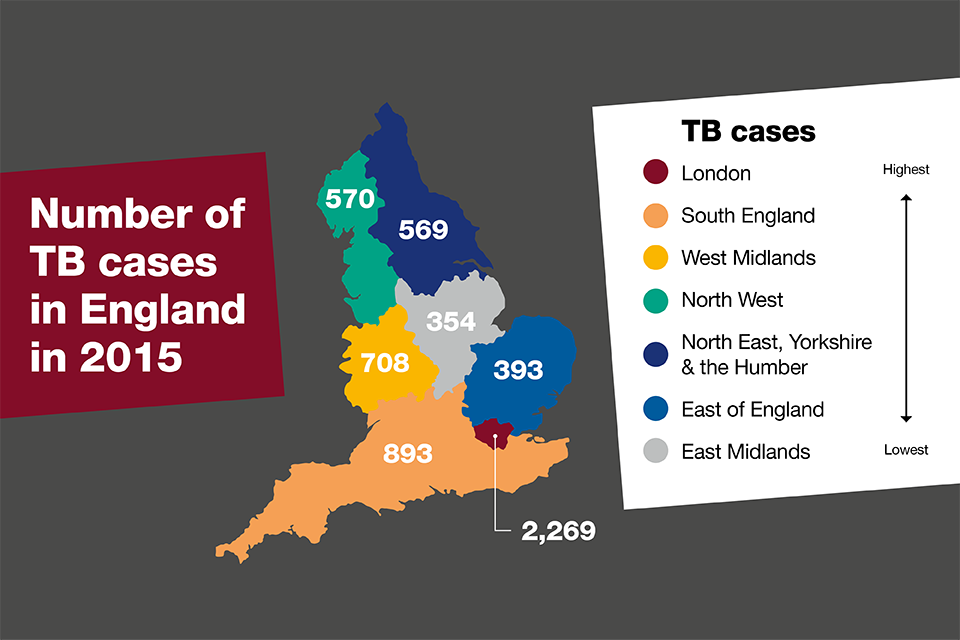
Infographic showing number of TB cases in the 7 major regions of England in 2015
40% of TB cases in England are found in London which has one of the highest rates in a capital city in Western Europe. Latest figures show that in 2015, London had a rate of 26.2 cases per 100,000. Around 6 people develop symptoms of TB every day in London.
The patient journey
Awareness
TB Alert, the UK’s national TB charity, has highlighted that in some communities, it is a stigmatising disease that can affect prospects for marriage, work and social inclusion. It does not only affect the poor. Although it is more common in more deprived populations, anyone can get TB.
Stigmatisation of TB means that many people are fearful of seeking a diagnosis even when they become very unwell. Late diagnosis increases the chances of onward transmission within the community and poorer outcomes for the person.
A survey conducted by the London Assembly found that many people in London know very little about TB and how it spreads. Almost 1 in 5 Londoners surveyed could not name a single symptom of infectious TB.
The Truth about TB website, from TB Alert, has a number of patient resources, public awareness and health promotion resources that health professionals can share with patients to:
- increase awareness and understanding of TB
- highlight the symptoms of TB
- advise on the treatment and management of TB
Raising awareness among health professionals
Raising awareness of TB isn’t just an issue for at risk groups. The Collaborative TB Strategy for England also encourages awareness raising among healthcare professionals. This can be achieved through:
- continuing professional development courses for healthcare professionals in primary and secondary care
- raising awareness among GPs and other health and social care professionals in high-incidence areas about:
- the incidence of TB
- the local epidemiology of TB
- how TB presents and is diagnosed
- where to refer for treatment of TB
The Royal College of General Practitioners (RCGP), in collaboration with PHE and TB Alert, has produced a free e-learning course on TB in general practice. This course (open to all) enables healthcare professionals and others to increase their understanding of the disease, its diagnosis and treatment.
The Think Suspect Refer’ desk card from TB Alert is available to assist GPs with identifying TB symptoms in general practice.
TB Alert has produced a TB nurse slideset to support TB nurses run information and awareness raising sessions.
Diagnosis
The earlier TB is diagnosed the better. Late diagnosis results in:
- more advanced and complex disease resulting in more illness and death
- higher rates of onward transmission
- increased health and social inequalities, which affect under-served populations to a greater degree
- greater costs to the NHS
Treatment for drug-sensitive TB can be under £1,000 per patient.
Treatment for medically complex TB or patients who have drug resistant TB can require lengthy hospital stays and require more expensive drugs. This treatment can exceed £15,000 per patient.
Treatment and follow-up care for exceptional cases, which may require extensive inpatient stay, can cost upwards of £100,000.
Although the delay between symptom onset and treatment start date for pulmonary TB cases has shown a slight improvement in the past year, delays are still unacceptably long, with 28% of patients waiting more than 4 months from first symptom to treatment start.
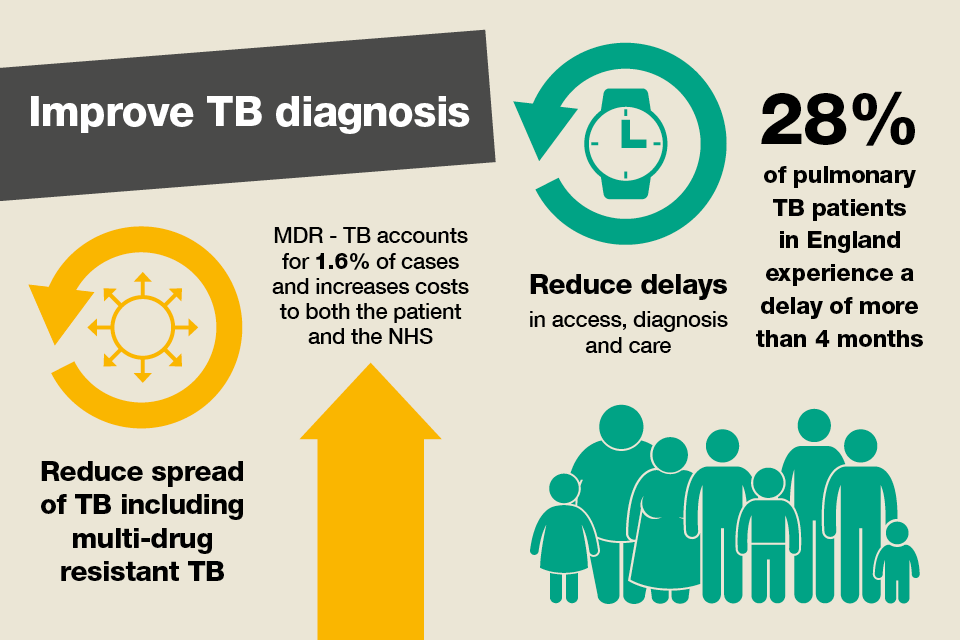
Infographic showing the need to reduce the spread of TB and reduce delays in accessing healthcare
Diagnosing TB in under-served populations
Diagnosing TB among under-served groups is particularly important as rates have risen in those with social risk factors in 2015. Early diagnosis in this group will:
- reduce the potential for onward transmission
- reduce the risk of developing drug resistant TB
- reduce health and social inequalities
The National Institute for Health and Care Excellence (NICE) produced guidance earlier this year for commissioners and service providers on covering the prevention, identification and management of latent and active TB in children, young people and adults. It aims to improve ways of finding people who have TB in the community including under-served populations.
Targeted outreach interventions are recommended for active case finding for pulmonary TB among homeless people and those attending substance misuse services.
In London, the ‘Find and Treat’ model model has involved the use of a mobile X-ray unit for people to have chest X-rays in non-hospital settings, such as homeless hostels and drop-in centres, alongside providing support for those requiring enhanced case management and interventions to encourage patients return to TB services to prevent loss to follow-up.
Treatment of TB

Infographic showing that TB is curable with antibiotics and that patients should complete the 6 month treatment
TB is curable in virtually all cases and can be effectively controlled provided cases are found early and patients complete at least the the 6-months course of antibiotic treatment.
In rare cases, treatment is required for longer than 6 months. Treatment for multidrug resistant TB, for example, can last for up to 24 months. In 2015, 54 of cases in England (1.6%) had initial multidrug resistance/rifampicin resistant TB (MDR/RR-TB). This is a decrease since the peak in 2011 (89 cases or 1.8%)
An individual with the signs and symptoms should be referred directly to the TB service for confirmatory diagnosis and treatment.
The TB Alert toolkit has further advice on supporting treatment regimens and strategies for when people refuse treatment. Some people may be reluctant to take medication for the 6 months or experience side-effects which put them off taking their medication.
NICE guidance offers advice on improving adherence to treatment of ensuring completion and follow‑up. The guidance outlines care for active and latent TB based on multidisciplinary teams and encourages people to follow the treatment plan and prevent them stopping treatment early.
The following techniques are recommended:
- reminder letters, printed information, telephone calls, texts and apps using an appropriate language
- health education counselling and patient‑centred interviews
- tailored health education booklets from quality sources
- home visits
- social and psychological support
- incentives and enablers to help people follow their treatment regimen
Latent TB testing and treatment
The majority of active cases diagnosed in England are a result of reactivation of latent TB. A person with latent TB is well, has no symptoms and cannot pass on the disease. However, there is a risk that they may develop active TB at some point in their life, especially if they were recently infected or are immunocompromised.
Latent TB testing and treatment for new entrants from areas of the world with a high incidence of TB is an effective and cost-effective public health intervention and is recommended in the current TB guidance from NICE.
The Collaborative TB Strategy has estimated that investment in latent TB testing and treatment will yield cost savings to the NHS, by preventing cases.
The national roll-out of a programme testing for latent TB infection and treating eligible new migrants aged 16 to 35 years started in April 2015. Diagnosis is carried out by blood test, and, if positive, the patient is referred to secondary care for treatment.
This programme prioritised the 59 high TB burden clinical commissioning groups (CCGs) across England.
The TB Alert toolkit provides practical guidance and support to those involved in implementing and operating latent TB testing and treatment programmes.
Collaborative action
It is very encouraging that the number of TB cases has declined for the fourth consecutive year in England, and that this decline is now seen in the UK-born, as well as the non UK-born, population, and in every area of the country. This is likely to reflect recent improvements in TB control in England building up to and since the launch of the Collaborative TB Strategy for England 2015 to 2020 in January 2015.
Further work is needed to take forward the Strategy’s 10 areas for action to ensure that we continue to see an ongoing decline in TB in England. A number of recommendations are outlined below for the main stakeholder groups.
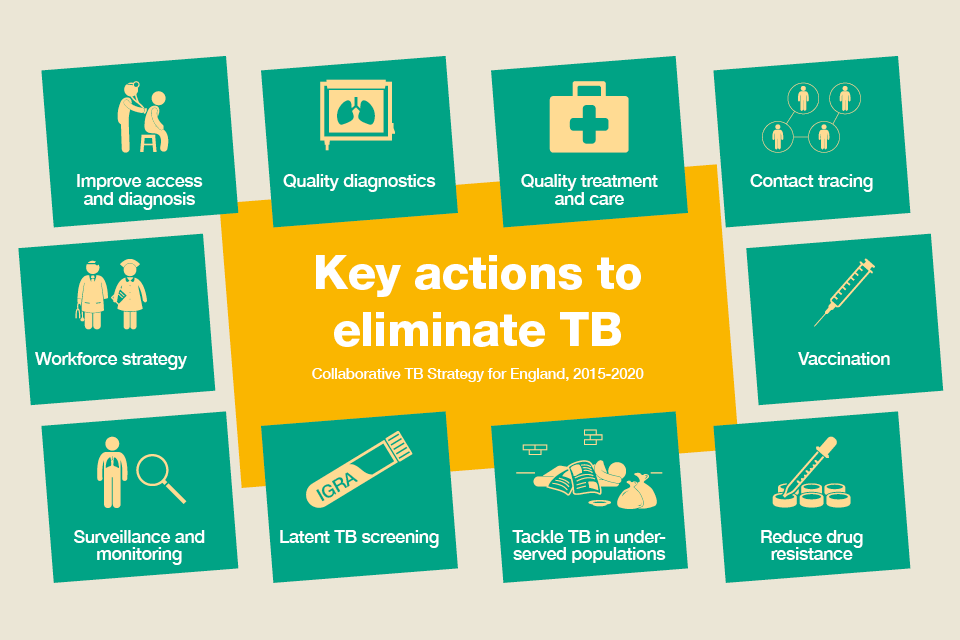
Infographic showing a summary of key actions to eliminate TB
Local Authorities are encouraged to:
- support TB awareness raising in professionals working with under-served populations and in undererved populations themselves
- ensure commissioning of appropriate access to housing and social care support to enable patients to complete treatment
- use the PHE TB Fingertips tool to assess their local TB burden to support JSNA and JHWS development, HWBs and appropriate commissioning and monitoring
Clinical Commissioning Groups (CCGs) are encouraged to:
- support TB awareness raising among healthcare workers by utilising the resources from TB Alert
- raise awareness of the RCGP TB e-learning module in primary care to raise awareness of TB and improve access
- commission and support targeted case finding and prevention activities, which focus on high-risk groups
- commission appropriate access to services, treatment and support to enable patients to complete treatment
- drive forward the roll-out of latent TB programmes in priority CCGs, invite people for testing and encourage those with latent TB to consider treatment
- support healthcare staff to use the recently launched latent TB toolkit to enhance the delivery of LTBI programmes
TB Control Boards are encouraged to:
- continue their work providing over-arching support to local TB control and overseeing local implementation of the TB Strategy’s 10 areas for action
- support and improve local TB clinical networks, and in due course consider the need for regional multidrug resistant TB multidisciplinary teams
- work with CCGs to encourage use of the national TB service specification to commission local TB services
- continue working with CCGs to facilitate the roll-out of the latent TB programmes, facilitate data returns and encourage the use of the recently launched LTBI toolkit to support this work
- complete their gap-analysis of local services against the national TB service specification and use this to prepare local action plans to meet these gaps
- use the soon to be launched under-served populations TB resource to support local action
- work with local laboratories to encourage use of the TB diagnostics standard of best practice, once this has been defined
TB Clinical Teams are encouraged to:
- raise awareness of TB among healthcare workers by utilising resources from TB Alert
- use the TB resources for patients available on TB Alert’s website
- obtain diagnostic samples wherever possible
- continue their excellent case management and support to complex TB patients, and to offer directly observed treatment where indicated
- continue cohort review as a tool to improve local TB control and as a measure of treatment outcomes and contact tracing activity
- discuss each multidrug resistant TB case with the British Thoracic Society MDR-TB Advisory Service
Third Sector organisations are encouraged to:
- represent communities and non-statutory organisations on TB control boards to encourage them to support local action including the commissioning of appropriate support from local non-statutory organisations
- support CCGs, local authorities and TB control boards to raise awareness of TB among affected communities
